Abstract
Background
Ellis–van Creveld is a dwarfing syndrome transmitted as an autosomal recessive trait. The constant features of the condition include acromelic–micromelic dwarfism, ectodermal dysplasia involving the nails, teeth and gums, postaxial polydactyly of the hands and congenital heart disease. Congenital heart disease affects 50–60 % of all patients and nearly 50 % of patients die by 18 months of age from cardiopulmonary complications. This study is intended to characterise the orthopaedic manifestations of Ellis–van Creveld based on the authors’ unique opportunity to interview and examine the largest group of patients to date in the literature.
Methods
Detailed interviews, physical examinations and/or radiographs were available on 71 cases of Ellis–van Creveld syndrome. Data were collected from physical examinations, radiographs, computed tomography (CT) reconstruction and magnetic resonance imaging (MRI) of the knee. Pathoanatomy of the knee was reinforced by the direct surgical observation of 25 limbs surgically managed during adolescence and puberty.
Results
A number of interesting clinical and radiographic abnormalities were noted in the upper extremities and lower extremities, but by far the most significant orthopaedic finding was a severe and relentlessly progressive valgus deformity of the knee. Although many patients had difficulties making a “fist” with the hand, no patient reported any functional disability. The severe valgus deformity of the knee is the result of a combination of profound contractures of the iliotibial band, lateral quadriceps, lateral hamstrings and lateral collateral ligament, leading to lateral patellar subluxation and dislocation. The lateral portion of the upper tibial plateau presents with cupping and progressive depression of the lateral plateau, along with severe valgus angulation of the proximal tibia and fibula. A proximal medial tibial exostosis is seen in nearly all cases.
Conclusion
This is the largest group of Ellis–van Creveld syndrome patients identified in the literature. An understanding of the orthopaedic pathoanatomy of the knee deformity is critical to determining the appropriate surgical management. This paper characterises the orthopaedic manifestations of Ellis–van Creveld syndrome and especially identifies the pathoanatomy of the severe and progressive valgus knee deformity.
Level of evidence
Level II.
Electronic supplementary material
The online version of this article (doi:10.1007/s11832-013-0541-4) contains supplementary material, which is available to authorized users.
Keywords: Pathoanatomy, Chondroectodermal dysplasia, Ellis–van Creveld syndrome
Introduction
Chondroectodermal dysplasia (Ellis–van Creveld syndrome) is a very rare form of skeletal dysplasia seen most commonly in, but not limited to, the Old Order Amish population. It is estimated that <300 cases have been reported in the English-speaking literature. In 1964, McKusick et al. [1, 2] reported 52 cases in the Old Order Amish (of whom 30 died within the first year of life), the largest single group of affected patients reported at that time, and established the genetic transmission as autosomal recessive [3–6]. Others have suggested the transmission as autosomal recessive [7–9]. The origins of this disorder and its particular pedigree were traced to one Samuel King and his wife, who emigrated from Europe in 1744. Recently, the genes which when mutated produce the condition have been identified [10–14]. The focus of the mutant gene is at 4p16 and represents mutations in two separate EVC genes, EVC and EVC2. The incidence has been estimated at 0.9 cases per 100,000 live births [6]. The genes EVC and EVC2 are highly expressed in bone and heart, two organs predictably affected in individuals with Ellis–van Creveld syndrome. Recent evidence suggests that EVC genes are involved in bone growth mediated at the base of primary cilia [15].
In 1670, Kerckring [16] reported a case of a polydactylous dwarf found drown in a river that might have represented one of the earliest cases ever reported of this condition. The infant had seven fingers and nine toes on one side and seven fingers and seven toes on the other. The drawing from the publication suggests a mesomelic form of dwarfism. Unfortunately, the absence of soft tissue findings renders the case speculative at best. In 1933, McIntosh [17] reported what is currently accepted as the first case reported in the modern literature of Ellis–van Creveld syndrome. In 1940, paediatricians Richard Ellis and Simon van Creveld [18] fully clarified the condition, alluding to the 4.5-year-old case described by McIntosh, and have subsequently received eponymous recognition of the condition. Small numbers of cases of Ellis–van Creveld have been reported in many races and in a multitude of countries throughout the world [19–45]. Currently, the Amish population of eastern Pennsylvania (primarily Lancaster County) still contains the largest concentration of patients with this condition in North America and, likely, outside of North America. Prenatal diagnosis by ultrasound is available [26–49].
The existing literature, albeit assembled from a relatively large number of publications of a small number of patients, paints a picture of a core group of consistent findings that characterise the syndrome across all patients and a larger constellation of findings frequently encountered in many patients but absent or incompletely expressed in others [50–59]. In 1973, Bailey [60] provided a useful overview of the many associated features. A few other clinical findings are only occasionally encountered. The most consistent and typical components of Ellis–van Creveld syndrome include acromelic–micromelic chondrodystrophic dwarfism and ectodermal dysplasia involving the nails, teeth and gums; postaxial polydactyly of the hands and occasionally of the feet; and commonly but not consistent congenital heart disease involving variable defects, most often a single atrium with cleft mitral valves (50–60 % of all patients). The usual average adult height is between 43 and 60 inches (110 and 152 cm.) It has been estimated that nearly a third of the patients die in the first 6 months and up to a half by 18 months of age from cardiac or pulmonary consequences.
A recent, unique opportunity to interview and examine a sizeable group of Amish patients with Ellis–van Creveld syndrome and a few non-Amish cases has prompted an assessment of the orthopaedic manifestations of this condition. Furthermore, an opportunity to directly surgically observe the pathoanatomy of the profound and severe valgus deformity of the knee has provided documentation of the nature of the marked extensive soft tissue contractures and chondro-osseous deformity seen in this condition.
Material—data
General clinical and radiographic characteristics of Ellis–van Creveld syndrome
Approval from our institutional review board was obtained. Detailed interviews, physical examinations and/or radiographs were available on all 71 patients included in this study. All but three of the patients descended from Old Order Amish backgrounds. Radiographic evaluations were available on 47 patients; 80 lower extremities; 31 skeletal surveys, including upper extremities and spine; 13 computed tomography (CT) reconstructions of the knee; and four magnetic resonance imaging (MRI) scans of the knee. Radiographs of the knee were available on all patients, not surprisingly, inasmuch as the knee valgus deformity is the most obvious and functionally impairing deformity routinely seen in Ellis–van Creveld syndrome (Fig. 1a–g). Online Resource 1 depicts a rotating 3-D computer model of Fig. 1 showing severe genu valgum, cupping of the lateral tibial plateau and patellar dislocation of the left knee.
| Typical findings >90 % of patients—non-orthopaedic |
| Acromelic–micromelic dwarfism |
| Ectodermal dysplasia |
| Postaxial polydactyly |
| Congenital heart disease |
Fig. 1.
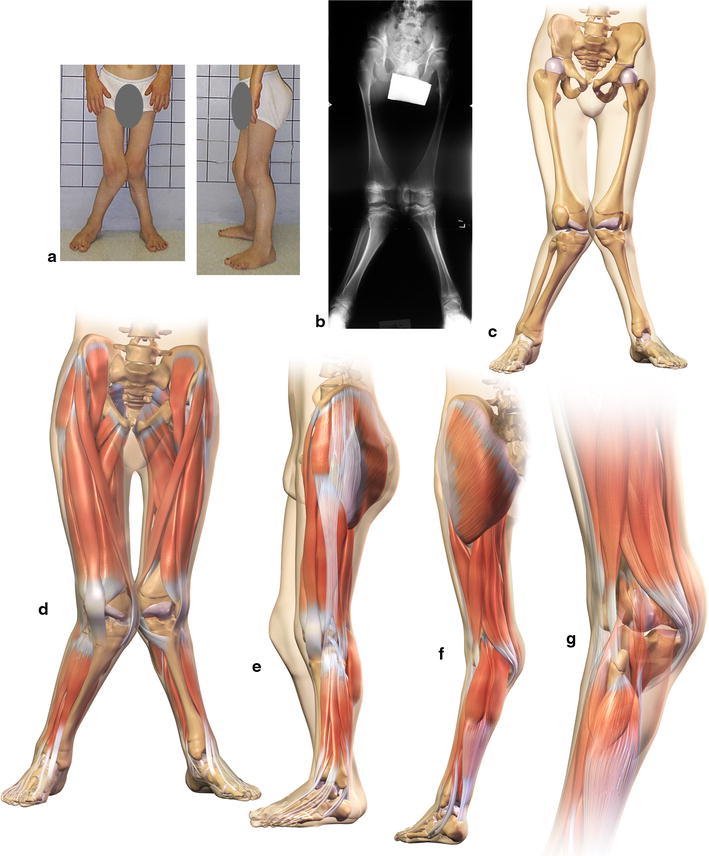
a Front and side clinical views of a 13-year-old adolescent male. b Anteroposterior (AP) standing radiograph waist-to-floor. c Anterior view waist-to-floor illustration of the skeleton showing severe genu valgum. d Anterior view waist-to-floor with musculature showing patellar dislocation. e Lateral view with musculature showing iliotibial band and quadriceps contracture. f Posterior view with musculature. g Posterior detail view with musculature showing biceps tendon contracture
The hair may be sparse or absent or fine and silky. Teeth may be present at birth with wide-spaced, peg-shaped hypoplastic teeth or even absent teeth. The gums are usually serrated and the upper lip is commonly attached to the upper gum in the form of a partial pseudocleft resembling a harelip but clearly different anatomically. Intelligence is generally normal or just slightly below. The nails are usually described as dystrophic, fragile, fluted and bordered by a peculiar brown rim. Dysplastic nails are seen uniformly in all patients.
For the purpose of this paper, we have arbitrarily divided the manifestations into typical (over 90 % of cases), frequent (50 % or more) and occasional (<50 % of cases).
| Orthopaedic manifestations | ||
|---|---|---|
| 71 cases | ||
| Clinical manifestations | ||
| Head and neck | Normal (typical) | |
| Shoulder, arm and elbow | 1.Curvature of the humerus and arm | Typical |
| 2.Increased carrying angle (cubitus valgus) | Typical | |
| 3.Radial head subluxation–dislocation | Frequent | |
| Forearm, wrist and hand | 1.Enlarged distal radius | Typical |
| 2.Stiffness of the PIP joints (thumb and index most frequently, with loss of flexion) | Typical | |
| 3.Marked loss of ability to make “fist” | Typical | |
| Spine and pelvis | 1.Increased lumbar lordosis | Typical |
| 2.Scoliosis | Occasional | |
| Hip and thigh | 1.Full flexion/extension, marked external rotation, markedly limited internal rotation | Typical |
| 2.Overall externally rotated thigh and leg | Typical | |
| 3.Contracted iliotibial band and lateral quadriceps | Typical | |
| Knee and leg | 1.Severe, profound valgus deformity of the knee | Typical |
| 2.Lateral patellar subluxation | Typical | |
| 3.Patellar dislocation | Frequent | |
| 4.Severe contracture iliotibial band, lateral quadriceps, lateral hamstrings and lateral collateral ligament | Typical | |
| 5.Normal knee ligament stability | Typical | |
| 6.Proximal medial tibial exostosis | Frequent | |
| Ankles and feet | 1.Broad foot with pronation | Typical |
| 2.Overriding fifth toe | Frequent | |
| 3.Short third toe and longer fourth toe | Frequent | |
| Radiographic manifestations | ||
|---|---|---|
| Head and neck | 1.Usually normal C-spine | Typical |
| 2.Bone compression upper cervical cord (two cases) | Rare | |
| Shoulder, arm and elbow | 1.Curving of the humerus | Typical |
| 2.Cubitus valgus | Typical | |
| 3.Radial head dysplasia and subluxation. Early ossification humeral head | Frequent | |
| 4.Enlarged proximal ulna | Typical | |
| 5.Enlarged distal radius | Typical | |
| Forearm, wrist and hand | 1.Postaxial polydactyly | Typical |
| 2.Fusion hamates and capitate | ||
| 3.Diminished ossification of the primary centres of ossification in the hand | Typical | |
| 4.Increased ossification of the secondary centres of ossification | Typical | |
| 5.Polymetacarpalia | Typical | |
| 6.Synmetacarpalism | Typical | |
| 7.Epiphyses embedded into the metacarpal | Frequent | |
| 8.Proximal pseudoepiphysis of the second or first metacarpal | Frequent | |
| 9.Small terminal phalanges | Frequent | |
| 10.Diminished sesamoid maturation | Typical | |
| Spine and pelvis | 1.Lumbar lordosis | Typical |
| 2.Spur-like or spike-like downward projection of the medial aspect of the acetabulum in young patients | Frequency unknown | |
| 3. Horizontal sacrum | Frequency unknown | |
| Hip and thigh | 1.Round, smooth femoral head well located in acetabulum | Typical |
| 2.Moderate valgus deformity of the upper femur | Typical | |
| 3.Adducted femur | Typical | |
| Knee and leg | 1.Increased lateral sloping of the lateral tibial plateau region with “cupping” and depression of the lateral plateau | Typical |
| 2.Severe valgus angulation tibia | Typical | |
| 3.Proximal medial tibial exostosis, both clinically and radiographically | Frequent | |
| Ankles and feet | 1.Postaxial polydactyly | Frequent |
| 2.Long fourth metatarsal compared to third | Frequent | |
| 3.Polymetatarsalia | Frequent | |
| 4.Syndactyly | Frequent | |
| 5.Short third metatarsal | Frequent | |
| 6.Ossification of the tarsals at birth | Frequent | |
| 7.Single sesamoid | Frequent | |
| 8.Delayed ossification distal phalanges | Frequent | |
| 9.Overriding third and fifth toes | Frequent | |
| 10.Tarsal fusions | Occasional | |
Surgical observations (14 patients, 25 limbs)
On the basis of direct surgical observation in an attempt to correct the severe valgus deformity of the knee, the following observations were routinely encountered in all cases to varying degrees. In 25 consecutive cases in the 10- to 16-year-old age group of patients, the following findings were typical (Figs. 1, 2 and 3; Online Resource 2 depicts the severe osseous pathoanatomy in a rotating 3-D computer model of Fig. 2, whereas Online Resource 3 includes the accompanying soft tissue abnormalities in a 3-D rotating rendition):
Lateral subluxation or dislocation of the patella.
Severe contracture of the iliotibial band, vastus lateralis and the lateral retinaculum, and capsule of the joint.
Contracture of the lateral hamstrings.
Contracture of the lateral collateral ligament.
Valgus lateralization and insertion of the infrapatellar tendon.
Deep “saucer”-like depression of the lateral tibial plateau.
Severe valgus of the shaft of the tibia, particularly proximally.
Medial proximal tibial exostosis.
Fig. 2.
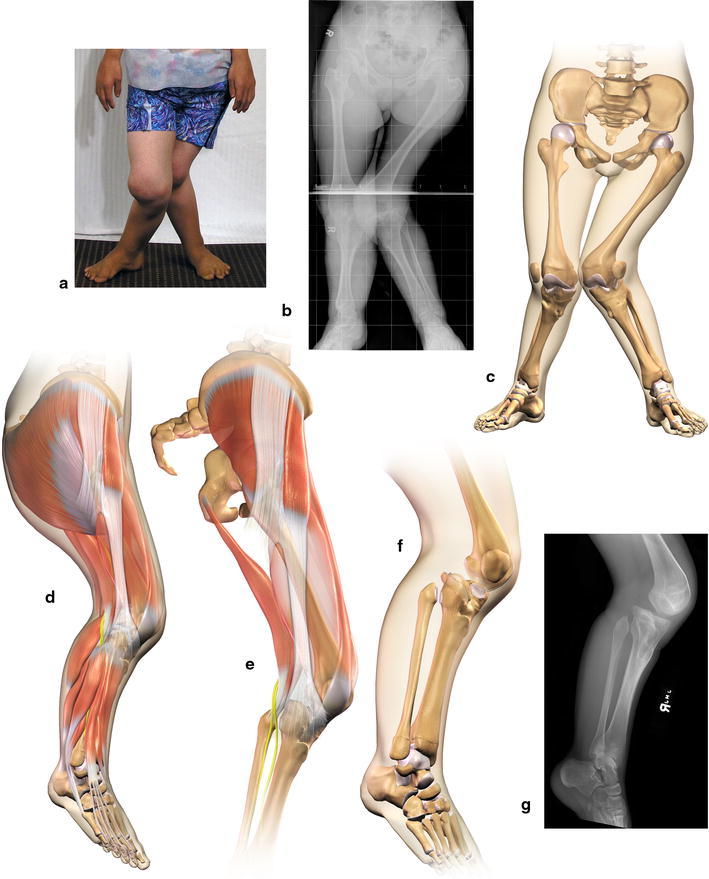
a Front view of a 14-year-old adolescent female. b AP standing radiograph waist-to-floor. c Anterior view waist-to-floor showing severe genu valgum and lateral tibial defect. d Lateral view with musculature. e Lateral view with musculature showing severe iliotibial band and quadriceps contracture. f Lateral view of the knee showing the anterior slope of the tibial plateau. g Lateral radiograph of the knee
Fig. 3.
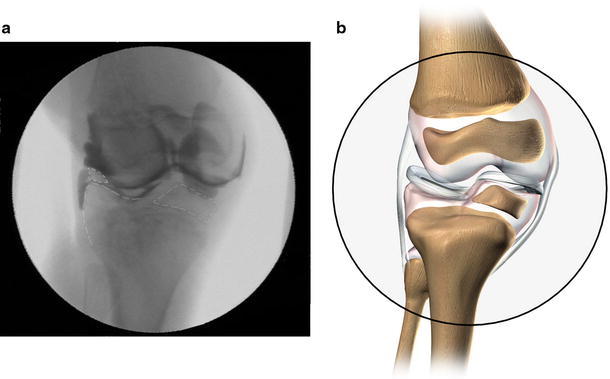
a AP intraoperative arthrogram of the knee of a 7-year-old boy showing tibial defect. b Illustrative reconstruction arthrogram
Although the ankle and foot are in pronation and the metatarsals and toes have frequent angular and rotation deformities, not a single patient had any foot or ankle complaint that led to any surgical correction. An unexplained and interesting observation in this group of patients was the frequency of delayed independent walking. Data were available on 43 of 71 patients who walked independently at an average of >15 months (range 11–35 months). The reason for this finding currently remains unclear.
Discussion
Although clinical and radiographic findings were often interesting and abnormal, the abnormalities surprisingly did not produce any functional limitations in the upper extremity, except the inability to produce a “fist” that was mentioned only rarely by an occasional patient on direct questioning, in spite of routinely encountered stiffness in the interphalangeal joints.
Significant restriction of flexion of the proximal interphalangeal (PIP) joints of the hand, often the thumb and index fingers, was seen very frequently (Fig. 4). One would presume that this restriction would result in the impairment of fine motor skills necessary in many occupations in society. The PIP joint stiffness is likely less impairing in the Amish due to occupational types. In the Amish society, nearly 70 % of males are employed in farming and roughly 30 % in construction and repair trades, such as carpentry, cabinet making, blacksmithing and harness repair or as labourers on farms and construction sites [61]. Unmarried Amish girls often work as store clerks or maids and only rarely work outside the house after marriage [61].
Fig. 4.
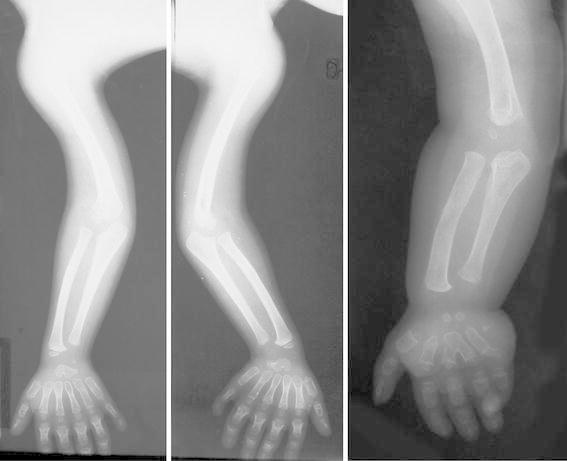
X-rays—upper extremity radiographic changes
Recent identification of two cases of upper cervical bony cord compression is, at the very least, distressing, but it is unclear whether the bony compression is directly related to the EVC syndrome. Routine lateral flexion/extension radiographs or other more detailed radiographic imaging of the upper cervical spine and base of the skull has not been suggested in the past. These cases warrant an increased awareness at least of the possible linkage to the basic condition in rare cases.
The thoracolumbar spine is usually spared deformity, save for an increased lumbar lordosis, which is seen frequently (Fig. 5). Scoliosis is seen only occasionally and kyphosis has not been seen at all in this group of patients or reported to be related to the syndrome. The fascinating radiographic changes in the acetabulum seen early in patients with Ellis–van Creveld (medial spike-like osseous prolongation) [62–65] appear to disappear with progressive osseous maturation, as the changes are not seen in skeletally mature individuals with Ellis–van Creveld syndrome, nor do they result in acetabular dysplasia.
Fig. 5.

X-ray—lateral spine
The femoral head is round, smooth and routinely well positioned in the acetabulum, with the head, neck and proximal shaft positioned in a valgus alignment. The femoral shaft is usually adducted and the overall bony alignment of the head–neck shaft is in moderate valgus. The marked contracture of the iliotibial band and lateral quadriceps, with significant external rotation of the thigh musculature, likely results in the marked clinical external rotation of the hip relative to very limited internal rotation of the hip and was present in nearly all patients. The common peroneal nerve remains adherent to the biceps tendon and is pulled away from its normal course around the neck of the fibula (Fig. 2e), all of which are demonstrated in the rotating 3-D modelling in Online Resource 3.
The soft tissue contractures likely contribute to the bony valgus and external rotation of the femur as well. Flexion/extension ranges of motion of the hip were normal. The severe soft tissue contracture of the iliotibial band and quadriceps is most reflected at the knee level (Figs. 1e and 2e).
Without question, the most striking and functionally impairing orthopaedic deformity affecting patients with Ellis–van Creveld is the severe and relentlessly progressive valgus deformity of the knee. This progressive valgus results in diminished efficiency in ambulation, with increased energy expenditure, and, in some cases, the inability to maintain ambulation. The extent of the valgus angulations far exceeds that seen by the authors in any other known orthopaedic condition. Thigh–leg angulations over 45° were routinely seen, with the lower extremities crossing over each other during ambulation, as shown in Online Resource 4, which is a gait video of a preoperative Ellis–van Creveld patient.
The peculiar lateral sloping and “cupping” and depression of the lateral tibial plateau was present in all cases [1, 7, 60–73], seen before walking age and progressively increased in dimension thereafter. In addition, the proximal lateral tibial plateau slopes in a variable fashion either laterally forward or, to a lesser extent, posteriorly from one patient to another, or even between the right and left knees of the same patient (Figs. 6 and 7). Ironically, the medial aspect of the knee joint remains well formed and intact, forming a pivot point against which the tibia may rotate externally or, in some cases, internally, corresponding with the degree of flexion deformity or recurvatum of the knee. Online Resource 5 demonstrates a computer modelling of Fig. 1, morphing between the right and left knees, depicting the variable slope of the lateral plateau, corresponding with flexion deformity and recurvatum, respectively. The medial aspect of the knee joint remains well formed and intact, forming a pivot point against which the tibia may rotate externally or, in some cases, internally. In severe cases, the lateral tibial plateau may sublux posteriorly, exacerbating the knee valgus (Fig. 2c, f), as demonstrated in Online Resource 3. The defect is believed to be a primary bony dysplasia and an inherent component of Ellis–van Creveld syndrome. Secondary weight-bearing changes likely augment the deformity and increase the valgus (Fig. 3). Online Resource 6 provides a conceptual morphing model between normal to a 13-year-old Ellis–van Creveld patient, depicting secondary weight-bearing changes. A proximal medial tibial exostosis (osteochondroma) is seen in most cases. Although speculative at best, it may occur secondary to “traction” on the physis by the relentlessly progressive valgus deformation of the tibia.
Fig. 6.
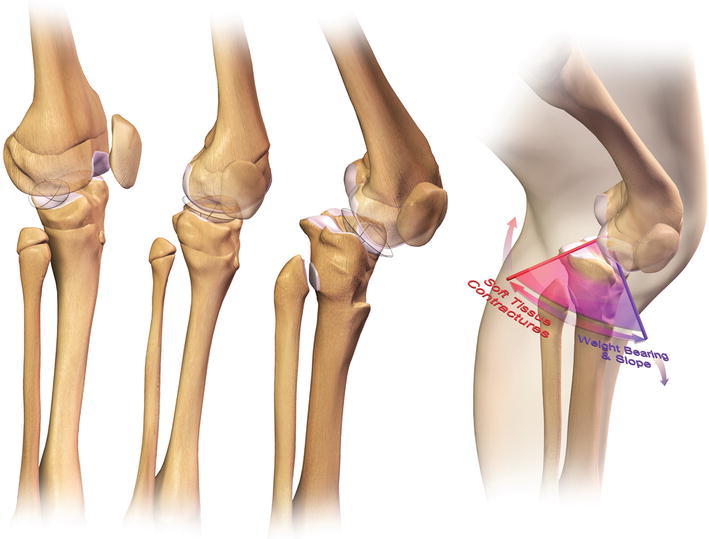
Illustration of the variable lateral tibial plateau defect
Fig. 7.

X-ray—lateral knee and ankle
The profound soft tissue contracture of the iliotibial band, the lateral quadriceps, the lateral hamstrings and the lateral collateral ligament results in progressive lateral displacement of the patella, with eventual subluxation and dislocation. These soft tissue contractures “tether” the tibia and fibula into further valgus (Fig. 2e). The authors believe that the soft tissue contracture is every bit as important in producing the severe overall valgus as the bone deformity. The failure of most isolated bony surgical attempts at correction substantiates the role of the soft tissue contracture aetiologically [74–79]. Currently, the authors have no plausible explanation for the delay in independent walking frequently seen.
Conclusion
Although a myriad of clinical and radiographic orthopaedic abnormalities have been identified in association with the Ellis–van Creveld syndrome, the severe knee valgus deformity is the only one to produce significant orthopaedic impairment and disability. Recognition of the soft tissue and bony pathoanatomy of the knee is essential to avoid fruitless surgical attempts at correction.
Electronic supplementary material
Below are the links to the electronic supplementary material.
Rotating 3-D computer model of a 13-year-old adolescent male (Fig. 1) showing severe genu valgum, cupping of the lateral tibial plateau and patellar dislocation on the left knee (MPG 3292 kb)
Rotating 3-D computer model of a 14-year-old adolescent female (Fig. 2) showing severe genu valgum, cupping of the lateral tibial plateau, patellar dislocation on both knees and severe external rotation of the tibia (MPG 3320 kb)
Rotating 3-D computer model of the right lower limb of a 14-year-old adolescent female (Fig. 2) depicting severe genu valgum of the knee, cupping of the lateral tibial plateau with anterior slope, lateral patellar dislocation, severe external rotation of the tibia, severe iliotibial band and quadriceps contracture. Note the abnormal course of the common peroneal nerve, which is pulled anterolaterally away from the proximal fibular neck (MPG 4566 kb)
Gait of a 23-year-old female: anteroposterior (AP) and lateral views showing extremities crossing during ambulation (MPG 3622 kb)
Computer model of a 13-year-old patient (Fig. 1) morphing between the right and left knees, depicting the variable slope of the lateral tibial plateau, corresponding with flexion deformity and recurvatum, respectively. The medial aspect of the knee joint remains well formed and intact, forming a pivot point against which the tibia may rotate externally or, in some cases, internally (MPG 4062 kb)
Conceptual computer model morphing between normal to a 13-year-old Ellis–van Creveld patient (Fig. 1) depicting secondary weight-bearing changes (MPG 3180 kb)
Acknowledgements
The authors wish to express their appreciation to Richard Pauli, M.D. for providing access to two non-Amish patients’ information and to the Women’s Board of Akron Children’s Hospital for the research funding support.
Conflict of interest
No direct or indirect commercial financial incentive was associated with this publication. This study was supported in part by a grant from the Women’s Board of Akron Children’s Hospital. The authors declare no conflict of interest.
References
- 1.McKusick VA, Hostetler JA, Egeland JA. Genetic studies of the Amish, background and potentialities. Bull Johns Hopkins Hosp. 1964;115:203–222. [PubMed] [Google Scholar]
- 2.McKusick VA, Egeland JA, Eldridge R, Krusen DE. Dwarfism in the Amish I. The Ellis–van Creveld syndrome. Bull Johns Hopkins Hosp. 1964;115:306–336. [PubMed] [Google Scholar]
- 3.McKusick VA, Egeland JA, Eldridge R, Krusen DE. Dwarfism in the Amish. I. The Ellis–van Creveld Syndrome. In: McKusick VA, editor. Medical genetic studies of the Amish: selected papers, assembled with commentary. Baltimore: John Hopkins University Press; 1978. pp. 93–117. [Google Scholar]
- 4.McKusick VA, Hostetler J, Egeland JA, Eldridge R. Genetic studies of the Amish: background and potentialities. In: McKusick VA, editor. Medical genetic studies of the Amish: selected papers, assembled with commentary. Baltimore: John Hopkins University Press; 1978. pp. 1–22. [Google Scholar]
- 5.McKusick VA, Hostetler J, Egeland JA, Eldridge R. The distribution of certain genes in the Old Order Amish. In: McKusick VA, editor. Medical genetic studies of the Amish: selected papers, assembled with commentary. Baltimore: John Hopkins University Press; 1978. pp. 51–66. [Google Scholar]
- 6.McKusick VA. Ellis–van Creveld syndrome and the Amish. Nat Gene. 2000;24:203–204. doi: 10.1038/73389. [DOI] [PubMed] [Google Scholar]
- 7.Metrakos JD, Fraser FC. Evidence for a hereditary factor in chondroectodermal dysplasia (Ellis–van Creveld syndrome) Am J Hum Genet. 1954;6:260–269. [PMC free article] [PubMed] [Google Scholar]
- 8.Zunin C. Observation on the hereditary transmission of the Ellis–van Creveld syndrome. Acta Genet Med Gemellol (Roma) 1963;12:269–275. [PubMed] [Google Scholar]
- 9.Spranger JW, Brill PW, Poznanski AK. Ellis–van Creveld syndrome. In: Spranger JW, Brill PW, Poznanski AK, editors. Bone dysplasia. An atlas of genetic disorders of skeletal development. 2. Oxford: Oxford University Press; 2002. pp. 130–131. [Google Scholar]
- 10.Polymeropoulos MH, Ide SE, Wright M, Goodship J, Weissenbach J, Pyeritz RE, Da Silva EO, Ortiz De Luna RI, Francomano CA. The gene for the Ellis–van Creveld syndrome is located on chromosome 4p16. Genomics. 1996;35:1–5. doi: 10.1006/geno.1996.0315. [DOI] [PubMed] [Google Scholar]
- 11.Ruiz-Perez VL, Ide SE, Strom TM, Lorenz B, Wilson D, Woods K, King L, Francomano C, Freisinger P, Spranger S, Marino B, Dallapiccola B, Wright M, Meitinger T, Polymeropoulos MH, Goodship J. Mutations in a new gene in Ellis–van Creveld syndrome and Weyers acrodental dysostosis. Nat Genet. 2000;24:283–286. doi: 10.1038/73508. [DOI] [PubMed] [Google Scholar]
- 12.Galdzicka M, Patnala S, Hirshman MG, Cai JF, Nitowsky H, Egeland JA, Ginns EI. A new gene, EVC2, is mutated in Ellis–van Creveld syndrome. Mol Genet Metab. 2002;77:291–295. doi: 10.1016/S1096-7192(02)00178-6. [DOI] [PubMed] [Google Scholar]
- 13.Ruiz-Perez VL, Tompson SW, Blair HJ, Espinoza-Valdez C, Lapunzina P, Silva EO, Hamel B, Gibbs JL, Young ID, Wright MJ, Goodship JA. Mutations in two nonhomologous genes in a head-to-head configuration cause Ellis–van Creveld syndrome. Am J Hum Genet. 2003;72:728–732. doi: 10.1086/368063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tompson SW, Ruiz-Perez VL, Blair HJ, Barton S, Navarro V, Robson JL, Wright MJ, Goodship JA. Sequencing EVC and EVC2 identifies mutations in two-thirds of Ellis–van Creveld syndrome patients. Hum Genet. 2007;120:663–670. doi: 10.1007/s00439-006-0237-7. [DOI] [PubMed] [Google Scholar]
- 15.Ruiz-Perez VL, Blair HJ, Rodriguez-Andres ME, Blanco MJ, Wilson A, Liu YN, Miles C, Peters H, Goodship JA. Evc is a positive mediator of Ihh-regulated bone growth that localises at the base of chondrocyte cilia. Development. 2007;134:2903–2912. doi: 10.1242/dev.007542. [DOI] [PubMed] [Google Scholar]
- 16.Kerckring T (1670) Tab. VIII. (Infant skeleton, abnormal; polydactyly). In: Spicilegium anatomicum. Sumptibus Andre, Amstelodami (Amsterdam)
- 17.McIntosh R. In: Holt’s diseases of infancy and childhood. 10. Holt LE, Howland J, editors. New York: Appleton-Century-Crofts; 1933. p. 362. [Google Scholar]
- 18.Ellis RWB, van Creveld S. A syndrome characterized by ectodermal dysplasia, polydactyly, chondro-dysplasia and congenital morbus cordis: report of three cases. Arch Dis Child. 1940;15:65–84. doi: 10.1136/adc.15.82.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lynch JI, Perry LW, Takakuwa T, Scott LP., 3rd Congenital heart disease and chondroectodermal dysplasia. Report of two cases, one in a Negro. Am J Dis Child. 1968;115:80–87. doi: 10.1001/archpedi.1968.02100010082016. [DOI] [PubMed] [Google Scholar]
- 20.Feingold M. Ellis–van Creveld syndrome. Clin Pediatr (Phila) 1966;5:431–436. doi: 10.1177/000992286600500711. [DOI] [PubMed] [Google Scholar]
- 21.Goldblatt J, Minutillo C, Pemberton PJ, Hurst J. Ellis–van Creveld syndrome in a Western Australian aboriginal community. Postaxial polydactyly as a heterozygous manifestation? Med J Aust. 1992;157:271–272. [PubMed] [Google Scholar]
- 22.Douglas WF, Schonholtz GJ, Geppert LJ. Chondroectodermal dysplasia (Ellis–van Creveld syndrome); report of two cases in sibship and review of literature. AMA J Dis Child. 1959;97:473–478. doi: 10.1001/archpedi.1959.02070010475012. [DOI] [PubMed] [Google Scholar]
- 23.Alcalde MM, Castillo JA, García Urruticoechea P, Vilaplana R, Molina E, Ortega J. Ellis–van Creveld syndrome: an easy early diagnosis? Rev Esp Cardiol. 1998;51:407–409. doi: 10.1016/S0300-8932(98)74767-0. [DOI] [PubMed] [Google Scholar]
- 24.Al-Khenaizan S, Al-Sannaa N, Teebi AS. What syndrome is this? Chondroectodermal dysplasia—the Ellis–van Creveld syndrome. Pediatr Dermatol. 2001;18:68–70. doi: 10.1046/j.1525-1470.2001.018001068.x. [DOI] [PubMed] [Google Scholar]
- 25.Prabhu SR, Daftary DK, Dholakia HM. Chondroectodermal dysplasia (Ellis–van Creveld syndrome): report of two cases. J Oral Surg. 1978;36:631–637. [PubMed] [Google Scholar]
- 26.Salvador Amores AM, Grande Baos C, Blanco Caneda ML, Alonso Ortiz T, Moro Serrano M, Arrabal Terán MC. Ellis van Creveld syndrome. An Esp Pediatr. 1990;32:445–550. [PubMed] [Google Scholar]
- 27.Arya L, Mendiratta V, Sharma RC, Solanki RS. Ellis–van Creveld Syndrome: a report of two cases. Pediatr Dermatol. 2001;18:485–489. doi: 10.1046/j.1525-1470.2001.1861994.x. [DOI] [PubMed] [Google Scholar]
- 28.Haque F, Ahmad SA. Ellis–van Crevald syndrome. Indian Pediatr. 2004;41:867–868. [PubMed] [Google Scholar]
- 29.Hill RD. Two cases of Ellis–van Creveld syndrome in a small island population. J Med Genet. 1977;14:33–36. doi: 10.1136/jmg.14.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferrero NA, Pozo OO, Morresi ES. Chondro-ectodermal dysplasia (Ellis–van Creveld syndrome): report of a case and review of the literature. J Bone Joint Surg. 1961;43:1230–1236. [Google Scholar]
- 31.Alvarez-Borja A. Ellis–van Creveld syndrome. Report of two cases. Pediatrics. 1960;26:301–309. [PubMed] [Google Scholar]
- 32.Goor D, Rotem Y, Friedman A, Neufeld HN. Ellis–van Creveld syndrome in identical twins. Br Heart J. 1965;27:797–804. doi: 10.1136/hrt.27.6.797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kurian K, Shanmugam S, Harsh Vardah T, Gupta S. Chondroectodermal dysplasia (Ellis van Creveld syndrome): a report of three cases with review of literature. Indian J Dent Res. 2007;18:31–34. doi: 10.4103/0970-9290.30920. [DOI] [PubMed] [Google Scholar]
- 34.Lichiardopol C, Militaru C. Ellis–van Creveld syndrome. Rom J Morphol Embryol. 2006;47:363–366. [PubMed] [Google Scholar]
- 35.Horák I, Smahel Z. Chondroectodermal dysplasia (Ellis–van Creveld syndrome) report of a case. Acta Chir Plast. 1983;25:161–175. [PubMed] [Google Scholar]
- 36.Akoun E, Bagard M. La maladie d’Ellis–van-Creveld. Algérie Médicale. 1956;60:669–676. [PubMed] [Google Scholar]
- 37.Kunze P. Ellis–van-Creveld syndrome. Kinderarztl Prax. 1980;48:193–198. [PubMed] [Google Scholar]
- 38.Pinelli G, Cottafava F, Senes FM, Becchetti S, Cosso D, Costa M. Ellis–van Creveld syndrome: description of four cases. Orthopaedic aspects. Ital J Orthop Traumatol. 1990;16:113–121. [PubMed] [Google Scholar]
- 39.de Haas WH, de Boer W. Follow-up of one of the first cases of the Ellis–van Creveld syndrome into adulthood. Some developmental aspects. Arch Interam Rheumatol. 1965;8:197–218. [PubMed] [Google Scholar]
- 40.Dayer L (1960) In: Le Syndrome D’Ellis–van Creveld. Une forme de dysplasie chondro-ectodermique. S. Karger, Basel and New York, pp 1–59
- 41.Monnet MP, Monnet F (1967) Le syndrome d’Ellis–van Creveld. Rev. Lyonnaise de Med 5–39 [PubMed]
- 42.Uehlinger E. Pathological anatomy of chondro-ectodermal dysplasia of Ellis van Creveld. Schweiz Z Pathol Bakteriol. 1957;20:754–766. [PubMed] [Google Scholar]
- 43.Weyers H. Knowledge of chondroectodermal dysplasia (Ellis–van Creveld); 2 case reports. Z Kinderheilkd. 1956;78:111–129. doi: 10.1007/BF00438445. [DOI] [PubMed] [Google Scholar]
- 44.Nabrady J. Ellis–van Creveld syndrome and neuroectodermal injury. Ann Paediatr. 1961;196:18–30. [PubMed] [Google Scholar]
- 45.Pachaly L, Martinez C. On congenital aortic sinus aneurysms. Zentralbl Allg Pathol. 1961;102:321–331. [PubMed] [Google Scholar]
- 46.Mahoney MJ, Hobbins JC. Prenatal diagnosis of chondroectodermal dysplasia (Ellis–van Creveld syndrome) with fetoscopy and ultrasound. N Engl J Med. 1977;297:258–260. doi: 10.1056/NEJM197708042970507. [DOI] [PubMed] [Google Scholar]
- 47.Horigome H, Hamada H, Sohda S, Oyake Y, Kurosaki Y. Prenatal ultrasonic diagnosis of a case of Ellis–van Creveld syndrome with a single atrium. Pediatr Radiol. 1997;27:942–944. doi: 10.1007/s002470050277. [DOI] [PubMed] [Google Scholar]
- 48.Tongsong T, Chanprapaph P. Prenatal sonographic diagnosis of Ellis–van Creveld syndrome. J Clin Ultrasound. 2000;28:38–41. doi: 10.1002/(SICI)1097-0096(200001)28:1<38::AID-JCU6>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 49.Dugoff L, Thieme G, Hobbins JC. First trimester prenatal diagnosis of chondroectodermal dysplasia (Ellis–van Creveld syndrome) with ultrasound. Ultrasound Obstet Gynecol. 2001;17:86–88. doi: 10.1046/j.1469-0705.2001.00255.x. [DOI] [PubMed] [Google Scholar]
- 50.McKusick VA, Hostettler A, Egeland JA. Ellis–van Creveld syndrome. In: McKusick VA, editor. Medical genetic studies of the Amish: selected papers, assembled with commentary. Baltimore: John Hopkins University Press; 1978. pp. 125–137. [Google Scholar]
- 51.McKusick VA. Heritable disorders of connective tissue. 4. St. Louis: Mosby; 1972. [Google Scholar]
- 52.Holt LE, Howland J (1936) In: Holt’s diseases of infancy and childhood: a textbook for the use of students and practitioners. Revised by L. E. Holt Jr. and R. McIntosh. 10th edn. Revised. D. Appleton-Century Company, Inc., New York and London, pp 362
- 53.Sarnat H, Amir E, Legum CP. Developmental dental anomalies in chondroectodermal dysplasia (Ellis–van Creveld syndrome) ASDC J Dent Child. 1980;47:28–31. [PubMed] [Google Scholar]
- 54.Winter GB, Geddes M. Oral manifestations of chondroectodermal dysplasia (Ellis–Van Creveld Syndrome). Report of a case. Br Dent J. 1967;122:103–107. [PubMed] [Google Scholar]
- 55.Mitchell FN, Waddell WW., Jr Ellis–van Creveld syndrome; report of two cases in siblings. Acta Paediatr. 1958;47:142–151. doi: 10.1111/j.1651-2227.1958.tb07869.x. [DOI] [PubMed] [Google Scholar]
- 56.Taylor GA, Jordan CE, Dorst SK, Dorst JP. Polycarpaly and other abnormalities of the wrist in chondroectodermal dysplasia: the Ellis–van Creveld syndrome. Radiology. 1984;151:393–396. doi: 10.1148/radiology.151.2.6709909. [DOI] [PubMed] [Google Scholar]
- 57.Biggerstaff RH, Mazaheri M. Oral manifestations of the Ellis–van Creveld syndrome. J Am Dent Assoc. 1968;77:1090–1095. doi: 10.14219/jada.archive.1968.0342. [DOI] [PubMed] [Google Scholar]
- 58.Varela M, Ramos C. Chondroectodermal dysplasia (Ellis–van Creveld syndrome): a case report. Eur J Orthod. 1996;18:313–388. doi: 10.1093/ejo/18.4.313. [DOI] [PubMed] [Google Scholar]
- 59.Gorlin RJ, Cohen MM, Jr, Hennekam RCM. Ellis–van Creveld (chondroectodermal dysplasia) In: Gorlin RJ, Cohen MM Jr, Hennekam RCM, editors. Syndromes of the head and neck. 4. New York: Oxford University Press; 2001. pp. 239–242. [Google Scholar]
- 60.Bailey JA., II . Disproportionate short stature: diagnosis and management. Philadelphia: WB Saunders; 1973. pp. 198–213. [Google Scholar]
- 61.Cross HE, McKusick VA. Amish demography. In: McKusick VA, editor. Medical genetic studies of the Amish: selected papers, assembled with commentary. Baltimore: John Hopkins University Press; 1978. pp. 29–47. [Google Scholar]
- 62.Taybi H, Kane P. Small acetabular and iliac angles and associated diseases. Radiol Clin North Am. 1968;6:215–221. [PubMed] [Google Scholar]
- 63.Gellis SS, Feingold M. Picture of the month. Ellis–van Creveld syndrome. Am J Dis Child. 1967;114:169–170. [PubMed] [Google Scholar]
- 64.Silverman FN. A differential diagnosis of achondroplasia. Radiol Clin North Am. 1968;6:223–237. [PubMed] [Google Scholar]
- 65.Sergi C, Voigtländer T, Zoubaa S, Hentze S, Meyberg-Solomeyer G, Troeger J, Tariverdian G, Otto HF, Schiesser M. Ellis–van Creveld syndrome: a generalized dysplasia of enchondral ossification. Pediatr Radiol. 2001;31:289–293. doi: 10.1007/s002470000421. [DOI] [PubMed] [Google Scholar]
- 66.Murdoch JL, Walker BA (1969) Ellis–van Creveld syndrome. The clinical delineation of birth defects. IV. Skeletal dysplasias. National Foundation—March of Dimes, New York, pp 279–288 (BSOAS V, No. 4)
- 67.Keizer DP, Schilder JH. Ectodermal dysplasia, achondrodysplasia, and congenital morbus cordis. AMA Am J Dis Child. 1951;82:341–344. doi: 10.1001/archpedi.1951.02040040357008. [DOI] [PubMed] [Google Scholar]
- 68.Tubbs FE, Crevasse L, Green JR., Jr Congenital heart disease in an adult with the Ellis–van Creveld syndrome. Ann Intern Med. 1962;57:829–834. doi: 10.7326/0003-4819-57-5-829. [DOI] [PubMed] [Google Scholar]
- 69.Smith HL, Hand AM. Chondroectodermal dysplasia (Ellis–van Creveld syndrome); report of two cases. Pediatrics. 1958;21:298–307. [PubMed] [Google Scholar]
- 70.Ellis RWB, Andrew JD. Chondroectodermal dysplasia. J Bone Joint Surg Br. 1962;44:626–636. [Google Scholar]
- 71.Hirokawa K, Suzuki S. Ellis–van Creveld syndrome: report of an autopsy case. Acta Path Jpn. 1967;17:139–143. [Google Scholar]
- 72.Weiss H, Crosett AD., Jr Chondroectodermal dysplasia; report of a case and review of the literature. J Pediatr. 1955;46:268–275. doi: 10.1016/S0022-3476(55)80280-6. [DOI] [PubMed] [Google Scholar]
- 73.Caffey J. Chondroectodermal dysplasia (Ellis–van Creveld syndrome): report of three cases. AJR Am J Roentgenol. 1952;68:875–886. [PubMed] [Google Scholar]
- 74.Zuege RC, Kempken TG, Blount WP. Epiphyseal stapling for angular deformity at the knee. J Bone Joint Surg Am. 1979;61:320–329. [PubMed] [Google Scholar]
- 75.Steel HH, Sandrow RE, Sullivan PD. Complications of tibial osteotomy in children for genu varum or valgum. Evidence that neurological changes are due to ischemia. J Bone Joint Surg Am. 1971;53:1629–1635. [PubMed] [Google Scholar]
- 76.Shibata T, Kawabata H, Yasui N, Nakahara H, Hirabayashi S, Nakase T, Ochi T. Correction of knee deformity in patients with Ellis–van Creveld syndrome. J Pediatr Orthop B. 1999;8:282–284. [PubMed] [Google Scholar]
- 77.Milgram JW, Bailey JA., 2nd Orthopaedic aspects of the Ellis–van Creveld syndrome. Bull Hosp Joint Dis. 1975;36:11–19. [PubMed] [Google Scholar]
- 78.Pinelli G, Cottafava F, Senes FM, Becchetti S, Cosso D, Costa M. Ellis–van Creveld syndrome: description of four cases. Orthopaedic aspects. Ital J Orthop Traumatol. 1990;16:113–121. [PubMed] [Google Scholar]
- 79.Morsy A, Tsuchiya H, Matsubara H, Kabata T, Tomita K. Ilizarov deformity correction of the lower limbs in Ellis–van Creveld syndrome. J Orthop Sci. 2007;12:505–509. doi: 10.1007/s00776-007-1157-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Rotating 3-D computer model of a 13-year-old adolescent male (Fig. 1) showing severe genu valgum, cupping of the lateral tibial plateau and patellar dislocation on the left knee (MPG 3292 kb)
Rotating 3-D computer model of a 14-year-old adolescent female (Fig. 2) showing severe genu valgum, cupping of the lateral tibial plateau, patellar dislocation on both knees and severe external rotation of the tibia (MPG 3320 kb)
Rotating 3-D computer model of the right lower limb of a 14-year-old adolescent female (Fig. 2) depicting severe genu valgum of the knee, cupping of the lateral tibial plateau with anterior slope, lateral patellar dislocation, severe external rotation of the tibia, severe iliotibial band and quadriceps contracture. Note the abnormal course of the common peroneal nerve, which is pulled anterolaterally away from the proximal fibular neck (MPG 4566 kb)
Gait of a 23-year-old female: anteroposterior (AP) and lateral views showing extremities crossing during ambulation (MPG 3622 kb)
Computer model of a 13-year-old patient (Fig. 1) morphing between the right and left knees, depicting the variable slope of the lateral tibial plateau, corresponding with flexion deformity and recurvatum, respectively. The medial aspect of the knee joint remains well formed and intact, forming a pivot point against which the tibia may rotate externally or, in some cases, internally (MPG 4062 kb)
Conceptual computer model morphing between normal to a 13-year-old Ellis–van Creveld patient (Fig. 1) depicting secondary weight-bearing changes (MPG 3180 kb)


