Abstract
Locking compression plates (LCP) have been developed for paediatric patients, and these provide safe bone fixation and allow for immediate weight-bearing. These plates are becoming increasingly popular and are proving to especially useful for the treatment of proximal and distal (supracondylar) femoral osteotomies. They are thought to provide better grip in osteoporotic bone. The technique has been described in the provider’s manual as well as recently by Joeris et al. (Int Orthop 2012: 36:2299–2306). The LCP system offers optimal stability after the final fixation, but temporary fixation using the originally described method is unstable, and we consider the medialisation instrument unsatisfactory as it has very small contact area with the lateral aspect of the femur and does not provide sound rotational control. For this reason we have developed a technique whereby temporary, stable fixation using fine K-wires can be attained for the proximal, diaphyseal fragment, following sound fixation with locking screws of the distal fragment. This procedure allows for full clinical (including rotation) and radiographic assessment intraoperatively, as well as fine adjustment in all three planes. This modification enables optimal correction before the final fixation and avoids unnecessary, large drill holes which may otherwise act as dangerous tress risers, endangering stability and weight-bearing. Here we describe a refined technique of the supracondylar femoral osteotomy using the paediatric LCP Condylar Plate.
Keywords: Locking compression plate, Femoral osteotomy, Supracondylar osteotomy, Technique
Supracondylar osteotomies have been in use for many years for the correction of deformities in all directions of the distal femur: malalignment in the frontal plane, flexion deformities of the knee and rotational abnormalities and various combinations. Blade plates were traditionally used to fix the bone after the osteotomy, and these allowed for correction in all three planes at once but weight-bearing was restricted for at least 6 weeks. Other implants [nails, standard locking compression plates (LCP)] allowed early weight-bearing but only for rotational correction. The osteotomy also had to be significantly proximal to the growth plate in paediatric patients to allow sufficient fixation distally. The new paediatric hip LCP implants (DepuySynthes© Inc, Zuchwil, Switzerland) have the advantage of allowing for immediate weight-bearing. They also enable an osteotomy to be performed as close as possible to the joint and stable fixation in all three planes; this was only previously available for the proximal femur [1]. For the supracondylar region, however, such a system was lacking. External fixators have also been used, but these tolerated immediate weight-bearing poorly and caused problems with stiffness, infection and pin loosening. For this reason the first author redesigned the 120° LCP hip plate for supracondylar application by changing the direction of the metaphyseal screws to 90°, thereby developing the paediatric Condylar LCP Plate (DepuySynthes© Inc). We have now developed a technique which provides full control of the fragments and stability throughout all steps of fixation after the osteotomy. This is in contrast to the official provider’s manual [2] as well as to the report by Joeris et al. [3], especially in regard to the medialisation component of the procedure. The paediatric Condylar Plate allows for immediate weight-bearing and correction of even severe deformities in all planes.
When a blade plate is used, the principles of the osteotomy follow the same standards: metaphyseal preparation with the seating chisel is the first step before osteotomy. This preparation of the metaphyseal fixation defines the final correction in the sagittal and frontal plane. Only rotation is corrected during the reduction of the proximal fragment to the plate. The same principle is applied to the supracondylar osteotomy technique described here:
Additional instruments for the alternative surgical method in addition to routine osteotomy and AO fixation instruments are:
Supracondylar 90° plate (3.5 or 5.0 mm system)
Equivalent drills
Aiming device (required for correction of valgus deformity only)
2.8-mm-threaded, 2.0-mm long and short and 1.6-mm-long K-wires (not in the provider’s set)
Long screw drivers
LCP-screws and simple lag screws in various lengths
Three drill sleeves (and three reduction sleeves for the 2.8-mm wires for the 5.0-mm plate)
Two reduction sleeves to 1.6 mm (3.5-mm set) or to 2.0 mm (5.0-mm set) (not in the provider’s set, come from the DepuySynthes© Tomofix set)
A reduction clamp which fits in between two drill sleeves if all three are mounted on the diaphyseal part of the plate
The technique for planning the osteotomy for extension was simplified: no measuring of the deficit preoperatively and handling reference angles during the surgery for the correction in the sagittal plane are required. Planning is limited to the frontal angle and rotation. The correction in the frontal plane is planned according to full-length radiographs, whereas rotation is corrected according to clinical assessment or gait analysis. The surgeon, however, must have a clear idea about the corrections required in all dimensions before surgery, especially whether medialisation of the shaft (varisation) or lateralisation (valgisation) is necessary as the centre of correction rotation and angulation in the frontal plane is not at the osteotomy site.
The positioning of the metaphyseal component of the plate defines the final correction (in all planes except rotation) independent of the osteotomy made. For this reason this step is crucial. Only correction of a valgus deformity requires the aiming block. In all other cases it is easier to use the plate with two distally inserted sleeves as a guide. The plate is held against the femur and positioned to fit the contour of the lateral condylar ridge of the distal femur—this will control the angle in the frontal plane (varus/valgus) and result in no change unless the plate is medialised or lateralised proximally. For correction of a varus deformity, the proximal part of the proximal plate is placed flush against the femur while the distal part of the proximal part of the plate is held off the lateral aspect of the femur, thereby producing valgus of the distal fragment to correct the deformity. For the correction of a valgus deformity, the opposite position of the proximal part of the plate can be used. For more severe coronal plane deformities the aiming block can be used to dial in the correction necessary (i.e. the wires are not inserted perpendicular to the shaft of the femur). At the distal femur the first 2.8-mm threaded wire is inserted into the most distal, inferior hole in the plate, and the position is checked using an image intensifier in order to be as close as possible to the distal femoral growth plate (or the physeal scar in adults). The leg and the image intensifier are then rotated to obtain a true lateral view of the plate, which allows for dorsal/ventral positioning of the plate. The knee is extended maximally, and the plate is rotated around the first wire so as to line up parallel to the axis of the tibia. The second threaded K-wire is inserted into the second distal sleeve, and a long, thinner 2.0-mm K-wire is inserted into the small distal hole in the plate. Despite this three-wire fixation, there is still a tendency for the plate to rotate into flexion. For this reason an additional short 2.0-mm K-wire is inserted right at the proximal end of the distal part of the plate, dorsally behind the plate at a slight angle: this wire acts as a shoehorn when the plate is later re-inserted (Fig. 1). This wire is essential to maintain the sagittal plane correction, especially when the plate is reinserted after the osteotomy is completed. Two short 2-mm K-wires are then inserted ventrally on the femur, proximal and distal to the osteotomy site to control the rotational correction. A free long wire is then placed in between the three distal wires, and this wire guides the plane of the distal cut of the osteotomy (Fig. 2). The osteotomy is performed, with the proximal cut being made perpendicular in both the sagittal and coronal planes to the femur. The plate is reinserted over the distal wires. A monocortical compression screw is then placed into the remaining third screw hole of the distal part of the plate to reduce the plate on the distal, metaphyseal fragment. If this screw has a good grip and with the wires left in situ, a careful reduction of the proximal fragment can be done to check the correction in the coronal plane. If further adjustment is required at this time, which will not be achievable with the proximal placement of the plate, the plate can be removed over the wires, bent in the desired direction and re-inserted. In routine cases, the two distal locking screws are inserted in the normal way. We do not recommend using the torque limiter for stainless steel screws as there is usually no danger of over-tightening, and we have witnessed spontaneous screw loosening when the torque limiter is used. The monocortical compression screw is then replaced by a bicortical locking screw. The plate is now secured to the distal, metaphyseal fragment, allowing complete control of this fragment. Threaded guide sleeves are inserted into the three proximal locking holes, and the proximal, diaphyseal fragment is then reduced onto the plate using the standard reduction clamps, thereby controlling the correction angle in all three planes. In the most proximal and most distal guide sleeves of the proximal part of the plate, the internal reduction sleeves for the thinner guide wires (1.6 for 3.5 set, 2.0 for 4.5 set) are inserted, and the guide wires are then inserted when the appropriate correction has been achieved. The reduction is checked under an image intensifier. This preliminary fixation is usually stable enough to assess joint motion clinically and to check the rotation of the femur as well as bony alignment in the frontal and sagittal plane. Further fine adjustment can then still be made in any plane:
Rotation: both proximal K-wires are removed and re-inserted after loosening temporarily the reduction clamp (this is the only adjustment circumstance where control of the bone is poor).
Sagittal plane: for correction in the sagittal plane one proximal K-wire is removed, the reduction clamp is temporarily loosened and the plate is rotated around the remaining wire. This can be done twice (once distally, once proximally) and allows correction depending on the antero-posterior width of the femur, as the plate must still lie against the lateral surface of the femur to ensure that all screws still have a hold in both cortices (Fig. 3).
Frontal plane: correction in the frontal plane does not require removal of the guide wires. The reduction clamp is loosened, and the plate can be proximally or distally lateralised by inserting an instrument (e.g. periosteal elevator) between the plate and bone, distally for correction of varus and proximally for correction of valgus: this is as briefly described above, when considering the initial placement of the plate. The locking screws will then maintain this distance between the plate and bone, controlling the coronal angle (Fig. 4). The correction of severe valgus deformity may even require medialisation of the entire proximal fragment in order to control for the mechanical axis of the limb to the centre of the knee joint centre. This LCP device allows for such fine adjustment of the osteotomy in a much superior manner compared to blade plate devices [3].
Fig. 1.
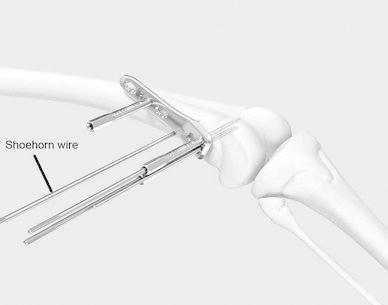
Insertion of the shoehorn wire to control the sagittal plane position of the plate when it is re-inserted
Fig. 2.
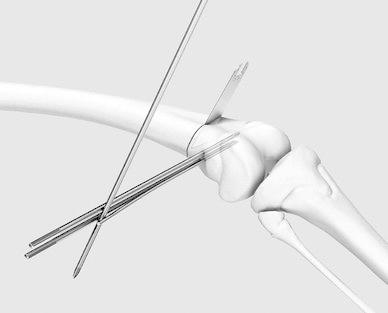
Wire inserted to guide the plane of the distal cut of the osteotomy
Fig. 3.

Fine adjustment in the sagittal plane
Fig. 4.
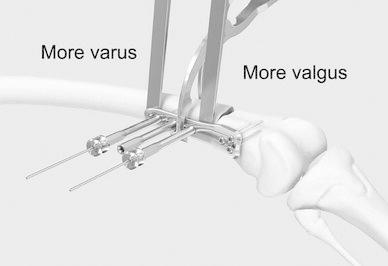
Fine adjustment in the frontal plane
Once the desired reduction is achieved, the middle guide sleeve is removed, and a monocortical compression screw can be used to produce compression at the osteotomy site. The elasticity of the wires allows for this. The proximal and distal wires are then replaced with locking screws, as the middle hole is then also replaced with a locking screw. The fixation is stable.
The technique described here for the diaphyseal fixation of the Condylar LCP Plate can be used in principle for all LCP devices. We recommend using a similar technique for the proximal femur, especially to give accurate rotational corrections. The paediatric Condylar LCP Plate can also be easily used at the proximal and distal tibia, and we have also used it for the distal humerus. The fixation technique as described is very helpful in achieving accurate corrections in sometimes very difficult osteotomies.
The technique described here for the supracondylar osteotomy, in particular the fine adjustments that can be made at the proximal, diaphyseal fragment, is superior to existing procedures as it allows for preliminary fixation without the need for large drill holes in the bone. As such, bone integrity is maintained, and immediate postoperative full weight-bearing is allowed without unnecessary stress-risers. This technique offers the possibility to check the position clinically and radiographically and to readjust the proximal, diaphyseal fragment in all planes to attain the optimal correction.
We have already demonstrated good results using this technique at the distal femur with and as such refer to our previous publications [1, 4].
The technique described here is not officially supported by the manufacturers, and the authors do not any responsibility.
Acknowledgements
We thank the Synthes Inc. for supplying the schematic drawings. There was no funding.
Conflict of interest
None.
References
- 1.Rutz E, Brunner R. The pediatric LCP hip plate for fixation of proximal femoral osteotomy in cerebral palsy and severe osteoporosis. J Pediatr Orthop. 2010;30(7):726–731. doi: 10.1097/BPO.0b013e3181efb86b. [DOI] [PubMed] [Google Scholar]
- 2.Synthes Inc. O, Switzerland . LCP pediatric condylar plate 90°, 3.5 and 5.0. For distal femur osteotomies. Technical guide. Oberdorf: Synthes Inc; 2011. [Google Scholar]
- 3.Joeris A, Audige L, Ziebarth K, Slongo T. The locking compression paediatric hip plate: technical guide and critical analysis. Int Orthop. 2012;36(11):2299–2306. doi: 10.1007/s00264-012-1643-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rutz E, Gaston MS, Camathias C, Brunner R. Distal femoral osteotomy using the LCP pediatric condylar 90-degree plate in patients with neuromuscular disorders. J Pediatr Orthop. 2012;32(3):295–300. doi: 10.1097/BPO.0b013e31824b29d7. [DOI] [PubMed] [Google Scholar]


