Abstract
Purpose
The goal of prosthetic fitting is to provide comfort and functionality to the patient. It is thought that incorporating the use of standing anterior–posterior long leg radiographs (LLR) into the fitting of lower extremity prostheses will provide an objective guide when making adjustments, and be a better assessment of alignment. This study compares prosthetic alignment before and after radiography-guided adjustments.
Method
This retrospective study was performed at a multidisciplinary amputee clinic on patients with congenital and/or acquired limb deficiencies. Their prosthetic alignment was evaluated by LLR and adjusted as needed. Satisfactory alignment was defined as a mechanical axis angular deviation of ≤1° and a leg length discrepancy of ≤10 mm.
Results
A total of 45 unique prostheses from 24 subjects (10 female and 14 male) were included. Post-adjustment radiographs were obtained from 29 prostheses. After the initial prosthetic fitting, the probability of a satisfactory fit was 20.0 % (95 % CI 10.9–34.9 %). Following the baseline adjustment, the probability of a satisfactory fit improved to 53.3 % (95 % CI 37.5–70.9 %). After adjustment number 4, the probability of a satisfactory fit further improved to 76.7 % (95 % CI 41.9–98.0 %). There were also significant improvements in distal offset distance (p = 0.0040) and leg length discrepancy (p = 0.0206). The distal offset distance decreased by an average of 10.7 mm (95 % CI 3.6–17.8), and leg length discrepancy decreased by an average of 3.0 mm (95 % CI 00.48–5.5).
Conclusions
The addition of LLRs to existing fitting methods significantly improves prosthetic alignment and length.
Keywords: Long leg radiographs, Prosthetic alignment, Lower extremity, Amputees
Introduction
The prevalence of congenital limb deficiency is estimated at 0.11 per 10,000 live births [1]. The overall incidence of acquired limb loss in children is not known, but among children with limb loss, congenital cases outnumber acquired cases 2:1 [2]. Traffic accidents and tumors are the most common causes of pediatric acquired limb loss [3]. Many of these children are fitted with a prosthesis to enhance the amputee’s ability to perform activities of daily life (ADLs) [4, 5]. A well-fitting prosthesis is highly important for maximizing function during ADLs, and is important for social and school adaptations [3].
Conversely, misaligned prostheses can lead to secondary conditions, including back pain, residual limb irritation, excessive energy expenditure, osteoarthritis, and scoliosis [5–7]. One study of lower-limb amputees indicated that 43 % of subjects develop scoliosis later in life [8]. Moderate-to-severe back pain has also been cited as occurring in over 52 % of subjects that use prosthetic devices during daily activities [9, 10]. It is thought that these conditions result from the increased forces on the intact limb and altered gait pattern when ambulating in a prosthesis that is improperly aligned [7]. Obtaining proper prosthetic alignment diminishes the impact of these stresses, leading to similar forces to those experienced by a non-amputee, and a similar gait, thus delaying the onset of secondary conditions related to prosthetic use [7, 11].
The maintenance of a proper prosthetic fit during childhood is a challenge, primarily due to the rapid growth of the pediatric skeleton. Comfort is one of the most important criteria used to evaluate the quality of a prosthesis [5]. For children, it is recommended that prostheses should be replaced annually until the age of 5, bi-annually from 5 to 12, and then every third year until the age of 21 [12]. In addition to fitting these new prostheses, numerous supplemental adjustments are required to resolve function- and comfort-related issues [4].
Traditionally, prosthetic alignment is established through conventional methods including physical examination and/or gait observation [4, 6]. When using traditional methods, it is estimated that pediatric amputees require adjustments an average of nine times per year [4]. Common reasons for patients requiring adjustments include improper fit, shortening, dysfunction resulting from wear, and related skin problems [4]. Additionally, it has been demonstrated in the literature that minor compensations for improper fit can increase the stress on the intact limb and expose the long-term prosthetic wearer to secondary physical conditions [7, 11]. Given that many patients live in remote regions and face a financial burden due to frequent prosthetic adjustment visits, it is essential to attain a satisfactory fit when the patient initially receives their prosthesis. Therefore, it is important to investigate new methodologies that may improve prosthetic fit and function, potentially decreasing the need for repeated clinic visits and the progression of degenerative conditions.
In an effort to improve this process, our institution has begun utilizing standing anterior–posterior long leg radiographs (LLR) to evaluate the static, frontal plane alignment of prostheses. This methodology allows the clinician to make prosthetic adjustments based on objective measurements of lower extremity alignment. The purpose of the study described in the present paper was to determine whether the use of radiographic parameters improves the lower extremity static frontal plane alignment when compared to alignment achieved through physical examination and observational gait analysis alone. We hypothesized that there would be a significant difference in the chosen “satisfactory” alignment of the lower extremity following radiography-based prosthetic adjustments.
Materials and methods
Prosthetic evaluation technique
A multi-disciplinary amputee clinic was established at our institution for the purpose of addressing the diverse pre- and post-surgical needs of patients affected by congenital and/or acquired limb deficiencies. An orthopedic surgeon, a rehab physician, a physical therapist, one midlevel providers, a dedicated nurse coordinator, and prosthetists attend this monthly clinic. Patients who are potential candidates for limb amputation or other related surgical interventions are referred to this clinic for pre-amputation consultations, surgical planning, and—following appropriate recovery—prosthetic fit evaluations. Prostheses are initially fitted by a community prosthetist based on parameters obtained from a physical exam and observational gait analysis, per standards of care. A trial socket is created from this initial evaluation, which is then used by the healthcare providers to determine a satisfactory fit based on the patient’s individual needs. Adjustments and modifications are measured using a baseline LLR in the trial socket with the patient’s shoes on, and with the patellae facing forward. From this assessment, a permanent socket is developed.
Each LLR is performed using the same methodology. A calibration ball measuring 25.4 mm in diameter is placed around the level of the knee at the level of the bone in the sagittal plane. The distance from the beam to the plate is 102 in. The exposure technique varies based on the patient’s age and size. Ranges for the technique are ~70–85 kVp and 16–50 mAs. Based on the patient’s height, 2–3 digital images are captured on 17″ × 17″ plates and stitched together. The Fujifilm® Pacsweb production interface is used to view and measure the images.
The alignment of the prosthesis is carefully reviewed using principles established in the joint replacement and limb deformity literature [13–17]. There are three important radiographic measurements to consider: mechanical axis angular deviation, distal offset, and leg length discrepancy (LLD) (see Fig. 1). Coronal plane alignment is assessed based on the mechanical axis angular deviation measured between two lines. The first line is drawn from the center of the femoral head through the center of the native/prosthetic knee joint (or in the case of a rotationplasty, the center of the native ankle joint). The second is drawn from the center of the femoral head to the center of the native/prosthetic ankle joint (or point of contact between distal prosthetic segment and the floor). The resulting angle indicates the angular deviation of the mechanical axis from neutral. The distal offset is measured using the horizontal distance (parallel to the floor) between the optimal line and the deviation line. LLD is measured as the difference in distance from the most proximal aspect of the femoral heads to the floor.
Fig. 1.

Radiographic measurements. 1 Mechanical axis angular deviation (°): center of the femoral head through the center of the knee joint and through the center of the ankle joint. 2 Distal offset (mm): distance from the center of the ankle joint to the mechanical axis angular deviation. 3 Leg length discrepancy (mm): top center of the femoral head through the center of the ankle joint and to the floor
In addition to the coronal plane alignment measurements, the radiographs are used to identify other potential indicators of an undesirable fit (see Fig. 2). The presence of a gap between the proximal portion of the prosthetic socket and the patient’s thigh indicates that the prosthesis may not be properly aligned and/or appropriately sized for the patient. Similarly, the presence of a soft-tissue indent may be indicative of excessive pressure between the prosthetic socket and the limb. When pelvic obliquity is present and there is no difference in pelvic size (top of the femoral head to top of the iliac crest), prosthetic length adjustments may be necessary.
Fig. 2.
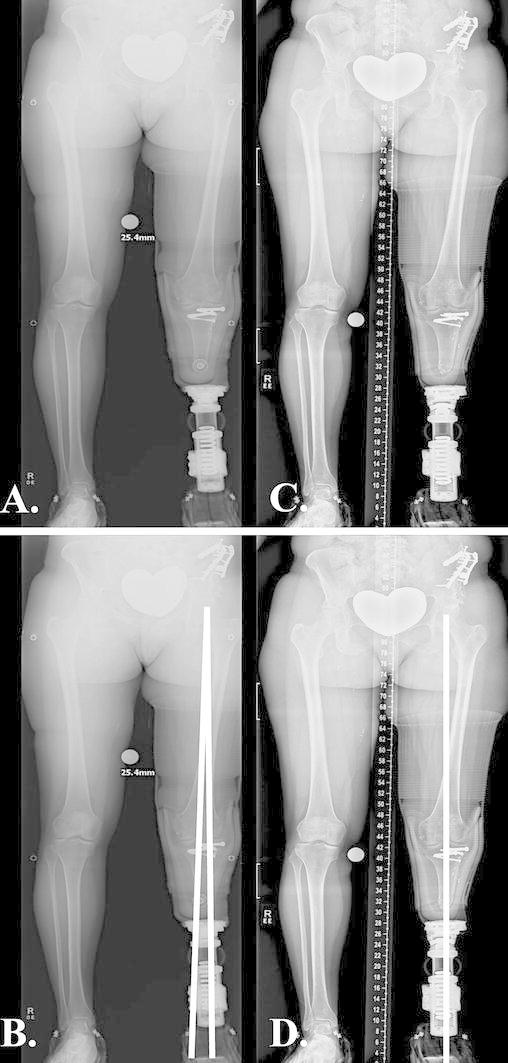
Pre vs. post-adjustment change in static alignment: a pre-adjustment alignment; b pre-adjustment alignment (mechanical axis angular deviation equals 2° of valgus); c post-adjustment alignment; d post-adjustment alignment (neutral mechanical axis)
The clinical evaluation of the patient also includes a thorough physical exam and a qualitative assessment of the patient’s observational gait. The results of these exams are considered when determining whether additional prosthetic adjustments are necessary. Minor adjustments can be made in the clinic, while larger adjustments require a return visit to the prosthetist. Following large adjustments and new prostheses, a repeat LLR is obtained.
Study methods
Institutional Review Board (IRB) approval was obtained prior to any study procedures being performed, and the study was performed in accordance with proper ethical standards. All patients that presented to our institution’s multidisciplinary amputee clinic and received an LLR between September 2009 and September 2011 were included in this retrospective study. The prosthetic alignment in the subjects’ baseline radiograph (before any prosthetic adjustments were made) was compared to the alignment in the subjects’ final post-adjustment radiograph. The following variables were used to assess lower extremity alignment: mechanical axis angular deviation (MAAD, in °), distal offset distance (in mm), LLD (in mm), and overall fit (satisfactory vs. unsatisfactory). Satisfactory overall alignment was defined as a MAAD ≤1° and an LLD of ≤10 mm.
Patients at our institution are instructed to return to the clinic annually for prosthetic maintenance, and more often if they experience pain or other complications with their prosthesis. After a physical evaluation, the patients received a new LLR if it was deemed necessary. LLRs were obtained and radiographic parameters were measured every time the patient returned to the clinic with a new prosthesis.
A total of 24 patients (10 female and 14 male) were identified. Of these patients, 70.83 % (n = 17) were bilateral amputees. Below-knee amputations comprised 41.7 % (n = 10) of the population, above-knee amputations comprised 29.2 % (n = 7) of the population, and rotationplasty comprised 29.2 % (n = 7) of the population. During the 2-year study timeframe, the average number of prostheses a patient received was 1.71 (range 1–4). For the sake of analysis, each new prosthesis was considered a separate subject. Therefore, 45 subjects (unique prostheses) underwent a baseline radiographic analysis. A Kaplan–Meier time to event analysis was used to estimate the probability of a satisfactory fit based on the number of LLRs that were obtained. Among the 45 subjects that underwent a baseline evaluation, follow-up LLRs were obtained from 29 prostheses that underwent radiography-based adjustments (see Fig. 3). Among these 29 prostheses, differences in measures of alignment between the baseline LLR and first post-adjustment LLR were analyzed using a generalized linear mixed model. The correlation between the limbs and the prostheses within a given subject were appropriately controlled for using a multi-level modeling strategy (SAS 9.3).
Fig. 3.
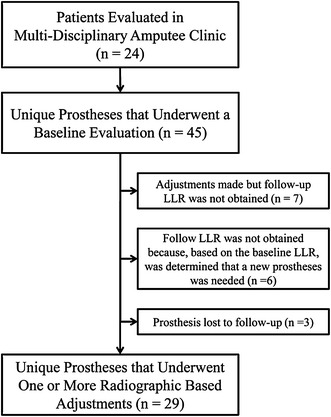
Flowchart of subjects (unique prostheses) included in analysis
Results
The average age of the patients with the 45 unique prostheses included in the analysis was 13.45 years (±6.74 years) at the baseline LLR. Based on the Kaplan–Meier analysis, after the initial prosthetic fitting, the probability of a satisfactory fit was 20.0 % (95 % CI 10.9–34.9 %). Following the baseline adjustment, the probability of a satisfactory fit improved to 53.3 % (95 % CI 37.5–70.9 %), and remained constant during adjustments 1, 2, and 3. After adjustment number 4, the probability of satisfactory fit further improved to 76.7 % (95 % CI 41.9–98.0 %). Four subsequent adjustments (5 total LLRs) represented the maximum number of adjustments that were required to achieve satisfactory alignment. Only one subject required the maximum number of LLR-based adjustments to achieve satisfactory alignment. The probability of obtaining a satisfactory prosthetic fit is further described in Fig. 4.
Fig. 4.
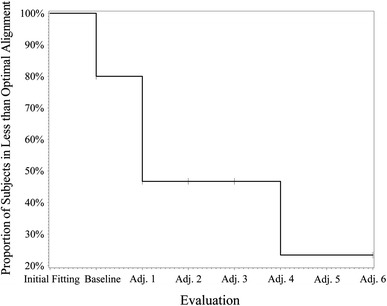
Number of radiographs needed to achieve satisfactory alignment. X-axis: evaluation. Y-axis: probability of being in less than satisfactory alignment
Among the prostheses that underwent multiple radiographic based adjustments (n = 29), a significant improvement in lower extremity alignment was achieved following the first radiography-based adjustment. The odds of a given prosthesis being in satisfactory alignment after a single adjustment were 3.9 (95 % CI 1.2–12.7, p = 0.0248) times the odds of the prosthesis being in satisfactory alignment during the baseline evaluation. For a given prosthesis, the odds of being in satisfactory mechanical axis angular alignment during the post-adjustment evaluation were 3.0 times (95 % CI 1.2–7.2, p = 0.0181) the odds of being in satisfactory alignment during the baseline evaluation. After undergoing the radiography-based prosthetic adjustments, there were also significant improvements in distal offset distance (p = 0.0040) and leg length discrepancy (p = 0.0206). The distal offset distance decreased by an average of 10.7 mm (95 % CI 3.6–17.8) (see Fig. 5), and leg length discrepancy decreased by an average of 3.0 mm (95 % CI 00.48–5.5) (see Fig. 6).
Fig. 5.
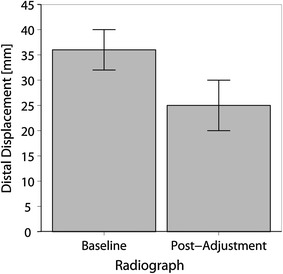
Change in distal offset. X-axis: radiograph. Y-axis: distal offset (mm)
Fig. 6.
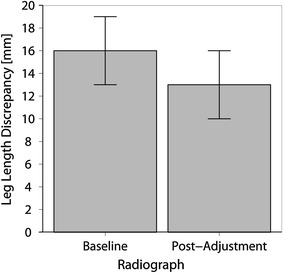
Change in leg length discrepancy. X-axis: radiograph. Y-axis: leg length discrepancy (mm)
Discussion
Attaining proper prosthetic alignment and length is vital to a lower extremity amputee’s quality of life, as it allows for improved gait, more efficient energy expenditure [5, 18, 19], and potentially less discomfort during ambulation. Improved alignment may also increase the longevity of the prosthesis itself. In a retrospective review of implant survival in 6,070 total knee joint replacements, Ritter et al. [20] demonstrated that implant failure was least likely to occur if the proximal and distal components were in neutral alignment (p < 0.0001). Despite the obvious differences between prostheses and total joints, this study highlights the effects that slight alignment issues can have on mechanical systems that are meant to sustain the repetitive loads induced during ambulation.
Numerous studies have demonstrated greater ambulation-related energy expenditure among lower extremity amputees compared to non-amputee controls [21–24]. Herbert et al. [22] reported that oxygen consumption during self-selected walking was 15 % greater for children with below-knee amputations compared to children without amputations. Schmalz et al. [19] demonstrated that even small changes in the alignment of the prosthesis can have a detrimental effect on energy demand. When the prosthetic knee joint was deliberately shifted away from optimal alignment, metabolic demand increased by 1–5 % depending on the walking speed being evaluated [19]. Using LLRs, we were able to significantly improve prosthetic length and alignment (distal offset). However, energy expenditure was not directly measured in this study, so further research is warranted to confirm whether it was also improved.
In the present study, the probability of a satisfactory fit during baseline evaluation was only 20.0 %. Following radiography-based adjustments, the probability of a satisfactory fit improved to 53.3 %. However, several prostheses did not achieve satisfactory alignment following multiple radiography-based adjustments. Among the 12 prostheses that underwent radiography-based adjustments but did not achieve satisfactory alignment, the majority of the patients were affected by residual intrasegmental bony limb deformities such as fibular hemimelia (n = 2), tibial hemimelia (n = 2), or unspecified lower extremity bony deficiency variants (n = 5). Two patients had outgrown their prosthetic sockets at the same time a significant limb length discrepancy was noted. The LLD was too large to adjust in the clinic. As they needed new sockets, the LLD was therefore corrected in their new prosthesis rather than in their current prosthesis. The remaining prosthesis was lost to follow-up.
A few key recurring issues were identified as limiting factors for achieving satisfactory prosthetic fits in these patients. These factors included reaching the limits of the adjustment capabilities of the current socket (deformity is recognized but a new socket is needed to obtain satisfactory alignment), patient currently undergoing guided growth procedures for a limb deformity that is gradually being corrected over time (deformity is recognized and treated but not fully corrected during the study’s time frame), prohibitive cost of prosthetic adjustments (deformity is recognized but the cost of the action necessary to correct it is prohibitive), and date of scheduled deformity correction surgery was outside the study timeframe (deformity is recognized and treatment is planned outside timeframe of the study).
All measurements performed in this study were obtained from digital LLRs. The potential benefits of using digital radiographs over traditional fitting techniques are highlighted by the fact that clinical exams and observational gait analyses are associated with less than ideal reliability [25]. Leg length measurements made during the clinical evaluation are prone to error due to differences in girth, difficulties in locating boney prominences, and angular deformities [26]. In typically developing subjects, the correlation between radiographic and clinical evaluations of leg length is reportedly moderate (ICC 0.683–0.790) [25]. Furthermore, observational analysis of gait deviations caused by orthopedic impairments is reported to be only moderately reliable, as minor gait deviations are difficult to recognize, may be complicated by inconsistent gait patterns, and are dependent upon the experience of the rater (ICC = 0.40, 95 % CI 0.36–0.44 for inexperienced and ICC = 0.54, 95 % CI 0.48–0.60 for experienced raters) [6].
The utilization of LLRs during the prosthetic fitting process raises potential concerns about radiation exposure. Based on a 10-year-old, the radiation dose associated with a single LLR at our institution is approximately 0.0362 mSv. Considering that the natural background radiation in North America is estimated to be 3 mSv per year [27], the radiation dose associated with a single LLR is minimal. The radiation dose associated with a single LLR in a 10-year-old is equivalent to the background radiation an individual naturally receives in <5 days in North America. Although this represents a very low dose, we still recognize the importance of minimizing radiation exposure whenever possible. In our clinic, lower extremity amputees primarily undergo radiography-based prosthetic evaluations for the check and permanent sockets of a new prosthesis. In a skeletally immature patient with a well-fitting socket, leg length adjustments are made based on physical exam rather than radiographs until the patient is due for a new socket. In this way, LLRs are taken at a frequency that is equivalent to their use in other populations of patients, such as those affected by limb alignment and length deformities, for which serial LLRs are the standard of care.
We used very strict criteria to define satisfactory alignment in this study. Among the subjects that achieved satisfactory alignment, the Kaplan–Meier graph of time to satisfactory alignment demonstrated that the proportion of patients in satisfactory alignment improved from 20.0 to 53.3 % after a single round of radiography-based adjustments (2 total LLRs). This change represented the greatest improvement in alignment between any two consecutive evaluations. Thus, there may be a point of diminishing returns at which the minimal improvements achieved with additional radiographs no longer outweigh the risks of additional radiation exposure. Research is needed to better define acceptable static alignment so that prostheses that truly need further adjustments can be better differentiated from those in acceptable alignment. The radiation dose of digital radiographs is adjustable, and research is needed to determine the optimal dose that minimizes radiation exposure without negatively affecting radiograph quality.
Study limitations
Due to the retrospective nature of the study, the data collection was limited to information that was available in the subjects’ charts. Our results indicate that static alignment was improved, but the effects of this on dynamic function or quality of life were not assessed. This study did not account for energy expenditure with prosthesis use, which has been related to greater ambulation and function in other studies [19, 21–24].
Conclusion
The results of this study support the use of LLR as an effective methodology for improving static prosthetic fit. Using LLR to guide adjustments significantly improves length, distal offset, and frontal plane alignment. LLRs should not, however, be used to replace a thorough physical exam and functional evaluation. Instead, this methodology should be utilized in conjunction with traditional methods during the prosthetic fitting process as an additional evaluation tool. The results have also caused us to re-evaluate the importance of considering factors other than just the patient’s primary deformity when developing treatment plans for lower extremity amputees. Limb deformities in residual bony segments that are not aligned properly along the mechanical axis should be addressed to prevent the development of “Z” deformities. The recognition of these deformities at an early age may allow for increased use of smaller guided growth procedures instead of larger osteotomies. The results have also caused us to reevaluate the timing of the LLR in the fitting process. Our preference is now to obtain LLRs in a check socket rather than a permanent prosthesis. This way, adjustments can be made to the position of the pylon attachment site, which allows for optimal placement and alignment prior to completion of the final socket.
Acknowledgments
Supported in part by an NIH/NCRR Colorado CTSI grant, number UL1 RR025780. The authors would like to acknowledge Ishtiaq H. Bercha, M.Sc., for his assistance in calculating the effective radiation dose associated with a long leg radiograph.
References
- 1.Martinez-Frias ML, Bermejo E, Aparicio P, Blanco M, Buron E, Cuevas L, Espinosa MJ, Fondevilla J, Gallo M, Hernandez F, Marco JJ, Martinez S, Morales MC, Mujica I, Paisan L, Valdivia L. Amelia: analysis of its epidemiological and clinical characteristics. Am J Med Genet. 1997;73(2):189–193. doi: 10.1002/(SICI)1096-8628(19971212)73:2<189::AID-AJMG15>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 2.Vannah WM, Davids JR, Drvaric DM, Setoguchi Y, Oxley BJ. A survey of function in children with lower limb deficiencies. Prosthet Orthot Int. 1999;23(3):239–244. doi: 10.3109/03093649909071640. [DOI] [PubMed] [Google Scholar]
- 3.Yigiter K, Ulger O, Sener G, Akdogan S, Erbahceci F, Bayar K. Demography and function of children with limb loss. Prosthet Orthot Int. 2005;29(2):131–138. doi: 10.1080/03093640500199703. [DOI] [PubMed] [Google Scholar]
- 4.Boonstra AM, Rijnders LJ, Groothoff JW, Eisma WH. Children with congenital deficiencies or acquired amputations of the lower limbs: functional aspects. Prosthet Orthot Int. 2000;24(1):19–27. doi: 10.1080/03093640008726518. [DOI] [PubMed] [Google Scholar]
- 5.Jia X, Suo S, Meng F, Wang R. Effects of alignment on interface pressure for transtibial amputee during walking. Disabil Rehabil Assist Technol. 2008;3(6):339–343. doi: 10.1080/17483100802044634. [DOI] [PubMed] [Google Scholar]
- 6.Brunnekreef JJ, van Uden CJ, van Moorsel S, Kooloos JG. Reliability of videotaped observational gait analysis in patients with orthopedic impairments. BMC Musculoskelet Disord. 2005;6:17. doi: 10.1186/1471-2474-6-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gailey R, Allen K, Castles J, Kucharik J, Roeder M. Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use. J Rehabil Res Dev. 2008;45(1):15–29. doi: 10.1682/JRRD.2006.11.0147. [DOI] [PubMed] [Google Scholar]
- 8.Burke MJ, Roman V, Wright V. Bone and joint changes in lower limb amputees. Ann Rheum Dis. 1978;37(3):252–254. doi: 10.1136/ard.37.3.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kulkarni J, Gaine WJ, Buckley JG, Rankine JJ, Adams J. Chronic low back pain in traumatic lower limb amputees. Clin Rehabil. 2005;19(1):81–86. doi: 10.1191/0269215505cr819oa. [DOI] [PubMed] [Google Scholar]
- 10.Ehde DM, Czerniecki JM, Smith DG, Campbell KM, Edwards WT, Jensen MP, Robinson LR. Chronic phantom sensations, phantom pain, residual limb pain, and other regional pain after lower limb amputation. Arch Phys Med Rehabil. 2000;81(8):1039–1044. doi: 10.1053/apmr.2000.7583. [DOI] [PubMed] [Google Scholar]
- 11.Hurley GR, McKenney R, Robinson M, Zadravec M, Pierrynowski MR. The role of the contralateral limb in below-knee amputee gait. Prosthet Orthot Int. 1990;14(1):33–42. doi: 10.3109/03093649009080314. [DOI] [PubMed] [Google Scholar]
- 12.Jain S. Rehabilitation in limb deficiency. 2. The pediatric amputee. Arch Phys Med Rehabil. 1996;77(3 Suppl):S9–S13. doi: 10.1016/S0003-9993(96)90237-3. [DOI] [PubMed] [Google Scholar]
- 13.Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M. Early failures in total knee arthroplasty. Clin Orthop Relat Res. 2001;392:315–318. doi: 10.1097/00003086-200111000-00041. [DOI] [PubMed] [Google Scholar]
- 14.Hungerford DS, Kenna RV. Preliminary experience with a total knee prosthesis with porous coating used without cement. Clin Orthop Relat Res. 1983;176:95–107. [PubMed] [Google Scholar]
- 15.Lotke PA, Ecker ML. Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg Am. 1977;59(1):77–79. [PubMed] [Google Scholar]
- 16.Moreland JR. Mechanisms of failure in total knee arthroplasty. Clin Orthop Relat Res. 1988;226:49–64. [PubMed] [Google Scholar]
- 17.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Fridman A, Ona I, Isakov E. The influence of prosthetic foot alignment on trans-tibial amputee gait. Prosthet Orthot Int. 2003;27(1):17–22. doi: 10.3109/03093640309167973. [DOI] [PubMed] [Google Scholar]
- 19.Schmalz T, Blumentritt S, Jarasch R. Energy expenditure and biomechanical characteristics of lower limb amputee gait: the influence of prosthetic alignment and different prosthetic components. Gait Posture. 2002;16(3):255–263. doi: 10.1016/S0966-6362(02)00008-5. [DOI] [PubMed] [Google Scholar]
- 20.Ritter MA, Davis KE, Meding JB, Pierson JL, Berend ME, Malinzak RA (2011) The effect of alignment and BMI on failure of total knee replacement. J Bone Joint Surg Am 93(17):1588–1596 [DOI] [PubMed]
- 21.Gailey RS, Wenger MA, Raya M, Kirk N, Erbs K, Spyropoulos P, Nash MS. Energy expenditure of trans-tibial amputees during ambulation at self-selected pace. Prosthet Orthot Int. 1994;18(2):84–91. doi: 10.3109/03093649409164389. [DOI] [PubMed] [Google Scholar]
- 22.Herbert LM, Engsberg JR, Tedford KG, Grimston SK. A comparison of oxygen consumption during walking between children with and without below-knee amputations. Phys Ther. 1994;74(10):943–950. doi: 10.1093/ptj/74.10.943. [DOI] [PubMed] [Google Scholar]
- 23.Waters RL, Mulroy S. The energy expenditure of normal and pathologic gait. Gait Posture. 1999;9(3):207–231. doi: 10.1016/S0966-6362(99)00009-0. [DOI] [PubMed] [Google Scholar]
- 24.James U. Oxygen uptake and heart rate during prosthetic walking in healthy male unilateral above-knee amputees. Scand J Rehabil Med. 1973;5(2):71–80. [PubMed] [Google Scholar]
- 25.Beattie P, Isaacson K, Riddle DL, Rothstein JM. Validity of derived measurements of leg-length differences obtained by use of a tape measure. Phys Ther. 1990;70(3):150–157. doi: 10.1093/ptj/70.3.150. [DOI] [PubMed] [Google Scholar]
- 26.Sabharwal S, Kumar A. Methods for assessing leg length discrepancy. Clin Orthop Relat Res. 2008;466(12):2910–2922. doi: 10.1007/s11999-008-0524-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chamberlain CC, Huda W, Hojnowski LS, Perkins A, Scaramuzzino A. Radiation doses to patients undergoing scoliosis radiography. British J Radiol. 2000;73(872):847–853. doi: 10.1259/bjr.73.872.11026860. [DOI] [PubMed] [Google Scholar]


