Abstract
Background
Closed reduction and percutaneous fixation with Kirschner wires (KWs) is the standard of care of pediatric supra-condylar humerus fractures (SCHFs). Failure modes leading to loss of reduction are not clear and have not been quantified. Multiple factors may weaken the KW–bone interface bonding conditions. To the best of our knowledge, the possible effect of this decrease on different KW configurations and fracture stability has never been studied.
Purpose
To investigate the effect of bone–KW friction conditions on SCHF post-operative mechanical stability and to formulate clinical guidelines for KW configuration under different conditions.
Methods
Finite element-based model of a fixated SCHF was used to simulate structure stability for two lateral divergent versus crossed lateral and medial KW configurations under varying KW–bone friction conditions.
Results
Finite element simulations demonstrated that crossed KWs provide superior stability compared with the divergent configuration when KW–bone bonding is compromised. When KW–bone bonding conditions are adequate, crossed and divergent KW configurations provide similar, sufficient fracture stability.
Conclusions
Under normal bone–implant interface conditions, the two diverging lateral KW configuration offers satisfactory mechanical stability and may be the preferred choice of SCHF fixation. When KW–bone bonding is suboptimal, as when one or more of the lateral KWs are re-drilled, addition of a medial KW should be considered in order to improve stability despite risk to ulnar nerve.
Keywords: Pediatric, Supra-condylar, Finite elements, Kirschner wires
Introduction
Supracondylar humerus fractures (SCHFs) are among the most common fractures requiring surgical stabilization in the pediatric age group [1]. The anatomy of the distal humerus is unique, with marked thinning of the bone just cephalad to the condyles, making this area weaker and more prone to fractures.
Fracture pattern and bone quality are dictated by the patient and injury. However, the configuration of the Kirschner wires (KWs) is determined by the surgeon and has been the subject of much research [5, 7–12]. Placement of a medial KW and the risk of an ulnar nerve injury have been at the center of the debate and remain controversial. Although a medial KW may improve stability, it also increases the risk of iatrogenic ulnar nerve injury, with the reported incidence of post-operative ulnar nerve injury ranging from 0 to 15 % [1, 5, 9, 11]. In their recent review of the literature, Slobogean et al. concluded that when compared with lateral entry KW, the crossed KW configuration is associated with an increased risk of injuring the ulnar nerve [4].
Several laboratory studies have attempted to compare the stability of different KW configurations. Lee et al. [10] compared the crossed medial–lateral KW configuration with the divergent configuration and found comparable stability except under torsional force, in which case the crossed configuration offered better stability. Zionts et al. [13] found that optimal stability was provided by the crossed KW configuration based on experiments on adult human cadaver bone. Using synthetic composite humeri, Feng et al. [14] showed that under most loading conditions two to three lateral KWs were advantageous.
KW configuration has also been analyzed in clinical studies by comparing the outcome of different configurations in large populations. Sankar et al. [15] found that the two-lateral KW configuration was more often associated with a loss of reduction, while no loss of reduction occurred with the crossed KW configuration. Zamzam and Bakarman [11] suggest that a medial KW should often be added, based on intra-operative assessment of fracture stability. Kocher et al. [9] found both configurations to be effective in the treatment of SCHF.
Similarly, KW diameter, relative to bony cortical width, has also been associated with construct stability and a possible loss of alignment [16]. The contact conditions between the KW and the wall of the hole drilled in the bone represent an additional factor necessarily affecting stability of the fixated bone construct. If no friction exists at the interface, significant weakening would occur. Drilling technique may lead to KW loosening due to osteonecrosis from thermal damage. If a KW is redirected through the same entry hole, as is often necessary, hole widening and weakening of the KW–bone interface may occur [11, 17].
Despite multiple studies the failure mechanism of fixated SCHF remains unclear. To the best of our knowledge no study has addressed the possible role of KW–bone interface conditions in SCHF fixation failure. The aim of this study is, therefore, to examine the effect of KW–bone interface conditions on mechanical stability of a SCHF fixated with KW and to compare the stability of the crossed pin configuration to the two lateral diverging configuration. We hypothesized that bone–implant interface grip plays a major role affecting the stability of the fixated bone construct and if so, it should be taken into consideration when choosing KW configuration.
Materials and methods
Model preparation
A fourth-generation composite sawbone (Sawbones®; Vashon, WA) of an adult humerus was used (a pediatric model is not manufactured) as study material. This composite bone model simulates cortical and cancellous bone material and geometry. A complete SCHF was created by cutting this sawbone with a hand saw at the level of the olecranon fossa. A computed tomography (CT) scan was performed on the fractured bone model, with a slice spacing of 0.5 mm and pixel size 0.3 × 0.3 mm (model Brilliance 64ME; Philips, Eindhoven, The Netherlands). The CT data set was imported into AmiraDev (AmiraDev5.3. Visage Imaging, San Diego, CA). A saw bone rather than a cadaveric bone was chosen in order to test an “average” bone that represents human pediatric SCHF shape and bony structure,
A model of the fractured humerus was constructed using the standard AmiraDev built-in tools. This included: (1) manual segmentation, (2) surface generation of each fragment, and (3) automatic volumetric grid generation for each bone fragment. The fracture was then virtually reduced, and KWs were placed at the desired configurations, namely, the crossed KW configuration versus two lateral divergent KW configurations (Fig. 1). For each configuration, a separate model was generated. Material properties were assigned to the bone-model elements according to the manufacturer’s data sheet: Young’s modulus E = 16 GPa and E = 150 MPa for the cortical and cancellous bone, respectively. The KWs were assigned a Young’s modulus of 200 GPa.
Fig. 1.
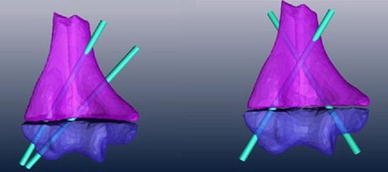
Models of the fixated humerus prior to structural analysis. The fragment models were created by manual segmentation of the computed tomography data set followed by virtual reduction and positioning of the Kirschner wires (KWs)
Finite element simulations
Each of the models created in AmiraDev was imported to a finite element application (Abaqus 6.9, Dassault Systèmes–Simula, Vélizy-Villacoublay, France) for structural analysis [18]. All of the elements used were tetrahedral quadratic elements with an average edge length of 0.625 for the KW and 1.41 for the bone material. For each KW configuration, four different load types were simulated (Fig. 2): (1) a clockwise and counterclockwise torque with a magnitude of 1.5 Newton/meters (NM), (2) a translational force with a magnitude of 30 N in the direction of the humerus shaft, and (3) a shear force with a magnitude of 30 N in the direction parallel to the fracture plane.
Fig. 2.
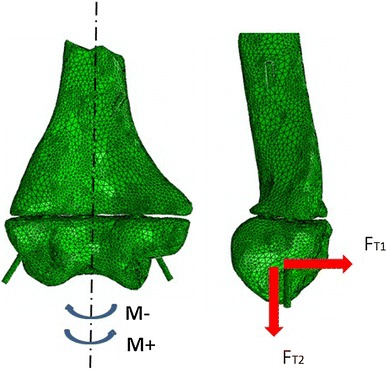
Loading scenarios within the finite element environment. Each KW configuration was subjected to four load cases:left clockwise (CC) and counterclockwise (CCW) torque respectively,right a translation force parallel to the fracture line and a translation force in the humerus axial direction, respectively
The maximal displacements were normalized relatively to the crossed pin configuration. A value of unity was assigned to the displacement of the crossed pin configuration when the coefficient of friction (COF) at the bone–implant interface was set to zero (μ = 0).
For each of the load conditions, the COF at the KW–bone interface ranged from μ = 0 to bonded (μ = ∞). Overall, a total of 20 simulations were carried out for each KW configuration type. The diameter of the KW was set to 1.6 mm for all finite element experiments to avoid the introduction of an additional variable.
The output was the relative displacement between the two fragments, which is inversely related to the fixation’s stability. The relative displacement was defined as the maximum displacement of a point on the distal fragment relative to the proximal fragment. Internal strains and stress within the bone material and KW were not examined.
Results
The results are summarized in Tables 1 and 2.
Table 1.
Normalized displacement for crossed versus diverging Kirschner wire configuration as a result of torque
| KW configuration | μ = 0 | μ > 0.2 | ||
|---|---|---|---|---|
| Torque + | Torque − | Torque + | Torque − | |
| Crossed | 1 | 1 | 0.72 | 0.75 |
| Diverging | 5.2 | 4.1 | 2.51 | 2.51 |
KW Kirschner wire
Table 2.
Normalized displacement for crossed versus diverging KW configuration as a result of translation and pullout forces
| KW configuration | Translation | Pullout | ||
|---|---|---|---|---|
| μ = 0 | μ > 0.2 | μ = 0 | μ > 0.5 | |
| Crossed | 1 | 0.75 | 1 | 0.2 |
| Diverging | 13.5 | 0.75 | 19.2 | 0.2 |
When torque forces were applied (Table 1), both bone constructs showed low sensitivity to bone–implant grip (Fig. 3).
Fig. 3.
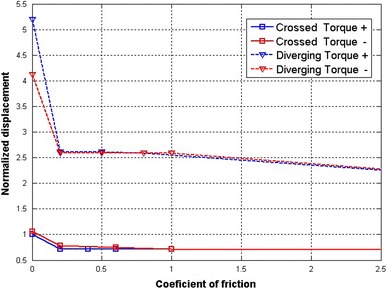
Displacement as a result of torque for both configurations. The displacement was measured for the crossed (squares) and diverging (triangles) configurations for different friction coefficients. The torque was applied in the CC (red) and CCW (blue) directions
For pullout and translation (Table 2), the diverging configuration demonstrated a higher sensitivity to changes in bone–implant grip (Figs. 4, 5). The relative displacement between the humerus and ulna increased substantially when COF values were set below μ < 0.5.
Fig. 4.
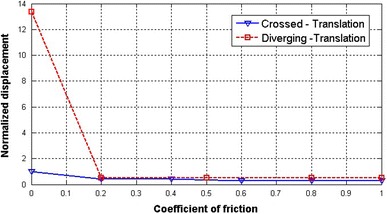
Displacement as a result of translation for both configurations. The displacement was measured for the crossed (solid line) and diverging (dotted line) configurations for different friction coefficients
Fig. 5.
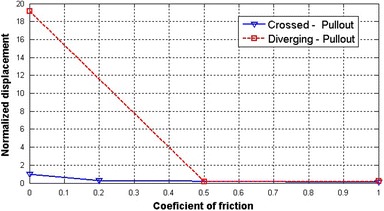
Displacement as a result of pullout for both configurations. The displacement was measured for the crossed (solid line) and diverging (dotted line) configurations for different friction coefficients
In addition the displacement relative to the crossed pin configuration was by far inferior at low COF—13.5 and 19.2 for translation and pullout, respectively, at μ = 0. However, when the COF value surpassed a threshold of μ = 0.2 for translation and μ = 0.5 for pullout, the displacements were similar for both fixation configurations.
Discussion
Multiple studies have addressed the issue of the optimal KW configuration required to stabilize a SCHF, resulting in the crossed KW configuration being considered to be equal or superior to lateral divergent KW configuration [19, 20]. However, the potential for iatrogenic ulnar nerve injury has deterred many surgeons from adding a medial KW. To validate our hypothesis that the effect of bone–KW bonding conditions varies with KW configuration, we performed a simulated biomechanical analysis. The finite element model simulated different friction conditions while checking the stiffness of the fixated bone constructs under rotational, translational, and bending forces.
The main outcomes of the simulations were: (1) bone–implant bonding conditions had a very significant influence on the fixated construct stability, and (2) each configuration was affected differently by these conditions.
We showed that the divergent configuration is much more sensitive to bone–implant grip and demonstrated inferior biomechanical performance, especially for pullout and translational forces.
In this study we did not examine the combination of crossed and divergent KW, as this configuration is necessarily more stable than each of the original configurations separately. Hence, we did not test this configuration under different friction conditions.
Our findings may provide a explanation for the clinical observations [11, 15] of higher incidence of alignment loss with lateral entry KW. Since clinically KW–bone bonding strength is difficult to quantify, the actual bonding conditions at the bone–implant interface is unknown. Many surgeons try rotating the KWs at the end of the procedure to ensure adequate “purchase” in the bone. This manipulation will occasionally reveal a loose KW but cannot truly quantify the bone–KW interface bonding. Once a KW is re-drilled through the same entry hole, as often occurs during surgery when KW re-positioning is necessary, the grip between the KW and the bone may be reduced to very low levels, which can lead in turn to future failure that cannot be recognized at the time of fixation and is explained by the finite element model. Cast immobilization may be helpful in reducing stress and protecting the fixed bone [21]; however, the fracture is not protected from rotational forces that may develop along the humerus shaft.
Our results demonstrate that KW–bone bonding has a profound effect on the stability of the fixated bone construct. This effect was mostly evident when distraction forces were applied (Fig. 5) but also occurred, to a lesser degree, with rotational or translational forces (Figs. 3, 4). Consequently, this effect may be a clinically important variable when KW–bone bonding is compromised after repeat attempts of passing the KW through the same entry hole. Under optimal conditions, when the implant–bone interface is adequate, the stability offered by the diverging configuration may be sufficient to maintain the reduction in the cast.
The outcome of this study suggests that bone–implant holding power is a key factor in the stiffness of a fractured bone fixed with KWs. Consequently, attention should be paid to using insertion techniques that minimize KW re-drilling and completely change the KW path when re-drilling is necessary. However, if appropriate bonding conditions do exist at the bone–implant interface, both fixation configurations provide similar stability. Hence, the diverging configuration may be the preferred choice of fixation as it obviates the risk of ulnar nerve injury associated with a medial KW insertion.
The results are based on a computational analysis and therefore limited in that comparison of the generated modeling results were not validated experimentally with strain gauge measurements. However, the computational methods employed are independently able to assess sensitivity of the fixated bone construct to a range of model input parameters such as COF and KW configuration.
Conclusion
Traditionally, the choice of KW configuration presents the clinician with a dilemma between a more stable construct versus the higher potential of nerve injury. The results of our study suggest that when KW–bone bonding conditions are optimal, the stability of the two diverging lateral KW configuration is similar to that of the crossed KW configuration. When bonding is jeopardized, the relative stability of the crossed configuration is superior. As KW–implant bonding conditions are currently not quantifiable in the clinical setting, further studies are needed to correlate KW insertion techniques and bone–implant bonding conditions. A three lateral KW configuration could be an alternative to a crossed KW configuration, but this option was not tested in this study.
Conflict of interest
None.
Contributor Information
Ron Lamdan, FAX: +972-2-6423074, Email: ronl@hadassah.org.il.
Meir Liebergall, FAX: +972-2-6423074, Email: liebergall@hadassah.org.il.
Amit Gefen, FAX: +972-3-6405845, Email: gefen@eng.tau.ac.il.
Naum Symanovsky, FAX: +972-2-6423074, Email: simanovsky@gmail.com.
Eran Peleg, FAX: +972-2-6423074, Email: eran@hadassah.org.il.
References
- 1.O’Hara LJ, Barlow JW, Clarke NM. Displaced supracondylar fractures of the humerus in children. Audit changes practice. J Bone Joint Surg Br. 2000;82(2):204–210. doi: 10.1302/0301-620X.82B2.9570. [DOI] [PubMed] [Google Scholar]
- 2.Omid R, Choi PD, Skaggs DL. Supracondylar humeral fractures in children. J Bone Joint Surg Am. 2008;90(5):1121–1132. doi: 10.2106/JBJS.G.01354. [DOI] [PubMed] [Google Scholar]
- 3.Bashyal RK, Chu JY, Schoenecker PL, Dobbs MB, Luhmann SJ, Gordon JE. Complications after pinning of supracondylar distal humerus fractures. J Pediatr Orthop. 2009;29(7):704–708. doi: 10.1097/BPO.0b013e3181b768ac. [DOI] [PubMed] [Google Scholar]
- 4.Slobogean BL, Jackman H, Tennant S, Slobogean GP, Mulpuri K. Iatrogenic ulnar nerve injury after the surgical treatment of displaced supracondylar fractures of the humerus: number needed to harm: a systematic review. J Pediatr Orthop. 2010;30(5):430–436. doi: 10.1097/BPO.0b013e3181e00c0d. [DOI] [PubMed] [Google Scholar]
- 5.Skaggs DL, Hale JM, Bassett J, Kaminsky C, Kay RM, Tolo VT. Operative treatment of supracondylar fractures of the humerus in children. The consequences of pin placement. J Bone Joint Surg Am. 2001;83-A(5):735–740. [PubMed] [Google Scholar]
- 6.Skaggs DL, Sankar WN, Albrektson J, Vaishnav S, Choi PD, Kay RM. How safe is the operative treatment of Gartland type 2 supracondylar humerus fractures in children? J Pediatr Orthop. 2008;28(2):139–141. doi: 10.1097/BPO.0b013e3181653ac8. [DOI] [PubMed] [Google Scholar]
- 7.Brauer CA, Lee BM, Bae DS, Waters PM, Kocher MS. A systematic review of medial and lateral entry pinning versus lateral entry pinning for supracondylar fractures of the humerus. J Pediatr Orthop. 2007;27(2):181–186. doi: 10.1097/bpo.0b013e3180316cf1. [DOI] [PubMed] [Google Scholar]
- 8.Eidelman M, Hos N, Katzman A, Bialik V. Prevention of ulnar nerve injury during fixation of supracondylar fractures in children by ‘flexion–extension cross-pinning’ technique. J Pediatr Orthop B. 2007;16(3):221–224. doi: 10.1097/BPB.0b013e328010b684. [DOI] [PubMed] [Google Scholar]
- 9.Kocher MS, Kasser JR, Waters PM, Bae D, Snyder BD, Hresko MT, et al. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children. A randomized clinical trial. J Bone Joint Surg Am. 2007;89(4):706–712. doi: 10.2106/JBJS.F.00379. [DOI] [PubMed] [Google Scholar]
- 10.Lee SS, Mahar AT, Miesen D, Newton PO. Displaced pediatric supracondylar humerus fractures: biomechanical analysis of percutaneous pinning techniques. J Pediatr Orthop. 2002;22(4):440–443. [PubMed] [Google Scholar]
- 11.Zamzam MM, Bakarman KA. Treatment of displaced supracondylar humeral fractures among children: crossed versus lateral pinning. Injury. 2009;40(6):625–630. doi: 10.1016/j.injury.2008.10.029. [DOI] [PubMed] [Google Scholar]
- 12.Foead A, Penafort R, Saw A, Sengupta S. Comparison of two methods of percutaneous pin fixation in displaced supracondylar fractures of the humerus in children. J Orthop Surg (Hong Kong) 2004;12(1):76–82. doi: 10.1177/230949900401200114. [DOI] [PubMed] [Google Scholar]
- 13.Zionts LE, McKellop HA, Hathaway R. Torsional strength of pin configurations used to fix supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 1994;76(2):253–256. doi: 10.2106/00004623-199402000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Feng C, Guo Y, Zhu Z, Zhang J, Wang Y. Biomechanical analysis of supracondylar humerus fracture pinning for fractures with coronal lateral obliquity. J Pediatr Orthop. 2012;32(2):196–200. doi: 10.1097/BPO.0b013e318242a99a. [DOI] [PubMed] [Google Scholar]
- 15.Sankar WN, Hebela NM, Skaggs DL, Flynn JM. Loss of pin fixation in displaced supracondylar humeral fractures in children: causes and prevention. J Bone Joint Surg Am. 2007;89(4):713–717. doi: 10.2106/JBJS.F.00076. [DOI] [PubMed] [Google Scholar]
- 16.Srikumaran U, Tan EW, Erkula G, Leet AI, Ain MC, Sponseller PD. Pin size influences sagittal alignment in percutaneously pinned pediatric supracondylar humerus fractures. J Pediatr Orthop. 2010;30(8):792–798. doi: 10.1097/BPO.0b013e3181f6d3af. [DOI] [PubMed] [Google Scholar]
- 17.Namba RS, Kabo JM, Meals RA. Biomechanical effects of point configuration in Kirschner-wire fixation. Clin Orthop Relat Res. 1987;214:19–22. [PubMed] [Google Scholar]
- 18.Luria S, Hoch S, Liebergall M, Mosheiff R, Peleg E. Optimal fixation of acute scaphoid fractures: finite element analysis. J Hand Surg Am. 2010;35(8):1246–1250. doi: 10.1016/j.jhsa.2010.05.011. [DOI] [PubMed] [Google Scholar]
- 19.Lee KM, Chung CY, Gwon DK, Sung KH, Kim TW, Choi IH, et al. Medial and lateral crossed pinning versus lateral pinning for supracondylar fractures of the humerus in children: decision analysis. J Pediatr Orthop. 2012;32(2):131–138. doi: 10.1097/BPO.0b013e3182471931. [DOI] [PubMed] [Google Scholar]
- 20.Gaston RG, Cates TB, Devito D, Schmitz M, Schrader T, Busch M, et al. Medial and lateral pin versus lateral-entry pin fixation for Type 3 supracondylar fractures in children: a prospective, surgeon-randomized study. J Pediatr Orthop. 2010;30(8):799–806. doi: 10.1097/BPO.0b013e3181f73d59. [DOI] [PubMed] [Google Scholar]
- 21.McKeon KE, O’Donnell JC, Bashyal R, Hou CC, Luhmann SJ, Dobbs MB, et al. Immobilization after pinning of supracondylar distal humerus fractures in children: use of the A-frame cast. J Pediatr Orthop. 2012;32(1):e1–e5. doi: 10.1097/BPO.0b013e31823db1b4. [DOI] [PubMed] [Google Scholar]


