Abstract
Objective:
The objective of this study was to analyse our initial experience using an interdisciplinary angio suite approach to neurosurgical treatment of complex neurovascular lesions and expound technical feasibility and possible applications.
Subjects:
Six out of 451 patients with cranial or spinal neurovascular lesions were surgically treated in the angio suite (biplane angiographic system) during a 28-month observation period. Clinical baseline data, radiological and intraoperative findings as well as clinical and radiological outcome were assessed.
Results:
A ventral spinal perimedullary arteriovenous malformation, a ventral spinal perimedullary fistula, two diffuse frontal dural arteriovenous fistulas, a multifocal temporal arteriovenous malformation and a partially embolized fronto-temporo-basal dural arteriovenous fistula were successfully treated with angiographically confirmed complete occlusion and unimpaired neurological condition of the patients at the 12-month follow up.
Conclusion:
This study demonstrates the feasibility of this approach and points out possible indications, namely ventrally located spinal lesions and diffuse, deep seated cranial lesions.
Keywords: arteriovenous malformation, dural arteriovenous fistula, intraoperative angiography, neurovascular, surgical treatment
Introduction
Digital subtraction angiography (DSA) with three-dimensional reconstruction is still regarded as the gold standard in evaluation and post-treatment control of most cerebral or spinal vascular lesions [Enzmann et al. 1983; Takahashi et al. 1984]. The majority of neurovascular centres are equipped with workstations set up for diagnostic examinations or endovascular treatment procedures, being not available in the operating room (OR) [Schaller et al. 2011]. The oftentimes crucial intraoperative visualization of normal vasculature and the vascular pathology is therefore based on the well-established indocyanine-green angiography (ICG) [Raabe et al. 2003; Snyder and Spetzler, 2011]. However, this technique is limited, providing only information about surgically exposed vascular structures.
Since its first description in the 1960s [Smith, 1977], several studies have reported the value of intraoperative angiography (IOA) in neurosurgery using portable, OR-integrated, ceiling-mounted or robotic-arm-attached hardware [Barrow et al. 1992; Benes et al. 2003; Grams et al. 2011; Murayama et al. 2011; Vitaz et al. 1999]. To date, IOA is most commonly performed using portable fluoroscopic equipment. Although technically improved and meanwhile offering all features of conventional angiography including three-dimensional rotational angiography [Dehdashti et al. 2009], the routine application of IOA in neurosurgical procedures, however, has not yet prevailed. On the one hand this is due to the expensive, resource-demanding technical requirements [Kpodonu, 2010]. On the other hand, a systematic superiority in using IOA compared with the established standard procedures, although being claimed for cerebral aneurysm surgery [Friedman and Kumar, 2009], has not been proven so far. Nevertheless, evidence from single series [Barrow et al. 1992; Martin et al. 1990; Raabe et al. 2006; Vitaz et al. 1999; Yanaka et al. 2003] and our own experience suggest that in some cases of neurovascular lesions, IOA can be regarded as helpful or, moreover, an absolute requirement for a successful surgical treatment. In such cases, we decide to perform surgery using a ‘tailored’ angio suite solution in our institution. The principle set up of this ‘on-demand angio suite’ as well as indications, technical challenges and outcome of the treated patients during a 28-month period in our centre are presented in this study.
Subjects and methods
Subjects
All patients admitted to our department for neurosurgical, interventional or combined treatment of neurovascular lesions between September 2008 and December 2010 were retrospectively analysed. Neurovascular lesions were classified and basic clinical patient data assessed (Table 1). Those patients subjected to angio suite treatment were further analysed regarding indications, technical challenges and clinical and radiological outcome 12 months after treatment.
Table 1.
Neurovascular lesions treated during the observation period. Overall patients and those treated in the angio suite. Concerning intracranial aneurysms (IAs) data, numbers in parentheses represent patient numbers. Combined treatment means initial endovascular treatment and secondary surgical treatment.
| Lesion | Classification | n | Angio suite treatment |
|---|---|---|---|
| Aneurysms | Total | 492 (321) | None |
| Singular | 223 | ||
| Multiple | 269 | ||
| Recurrent | 43 | ||
| SAH | (138) | ||
| Innocent | (183) | ||
| Clipping | (132) | ||
| Coiling | (189) | ||
| AVMs | Total | 88 | 3 (2) |
| Singular | 86 | ||
| Multiple | 2 | 1 | |
| Cerebral | 76 | 2 | |
| Grade1 I | 12 | 1 | |
| Grade II | 23 | 1 | |
| Grade III | 23 | ||
| Grade IV | 10 | ||
| Grade V | 1 | ||
| Spinal | 12 | 1 | |
| Surgery | 25 | ||
| Embolization | 16 | ||
| Combined Treatment | 25 | ||
| dAVFs | Total | 42 | 4 |
| Cerebral | 31 | 3 | |
| Type2 I | 9 | ||
| Type IIa | 1 | ||
| Type IIb | 2 | ||
| Type IIa and IIb | 4 | ||
| Type III | 8 | 2 | |
| Type IV | 7 | 1 | |
| Spinal | 11 | 1 | |
| Surgery | 18 | ||
| Embolization | 17 | ||
| Combined Treatment | 4 | ||
| 439 | 7 (6) |
According to the Spetzler–Martin grading.
According to the Cognard classification.
AVM, arteriovenous malformation; dAVF, dural arteriovenous fistula; subarachnoid hemorrhage (SAH).
Angio suite set up
The angio suite is equipped with a laminar upward air flow system allowing open surgical procedures. A flat panel detector biplane angiographic system (Allura Xper FD20/10, Philips Healthcare, Best, the Netherlands) is installed consisting of a floor-mounted C-arm providing posterior anterior (p.a) projections and excellent patient accessibility to the head. A ceiling mounted C-arm, which can be independently manoeuvred to provide additional lateral projections, can be withdrawn from the patient when not required or during acquisition of rotational angiograms.
The angiography table allows fixation of the head using a radiolucent Mayfield© clamp (Integra, Cincinnati, OH, USA) and positioning in any surgically appropriate position. Multiple display monitors offer the surgeon and the interventional team access to all previous acquired diagnostics of other imaging modalities via the integrated hospital picture archiving network (PACS, Centricity, General Electric, Fairfield, Connecticut, USA). For hybrid neurointerventional and neurosurgical procedures, the angio suite was additionally equipped with an operating microscope capable of ICG (OPMI Pentero, Zeiss, Oberkochen, Germany), a neuronavigation system (Brainlab, Feldkirchen, Germany) and an ultrasound microdoppler system (Aloka Medical, Tokyo, Japan).
Hybrid suite workflow
In our set up, switching between surgery and IOA was possible without turning the patient table or changing the patients’ position, thus, easily allowing intermittent angiographic controls (Figure 1). The operative set up allowed an optimal approach to the cranial or spinal situs while access to perform angiographic series was maintained.
Figure 1.
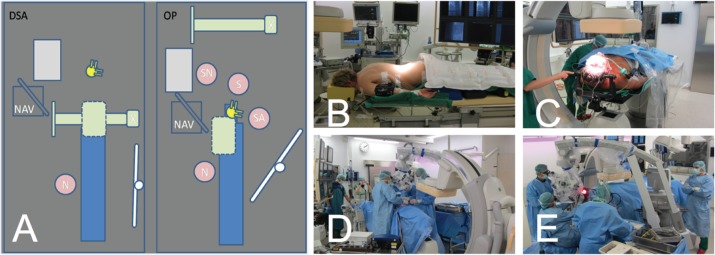
(A) A blueprint of the angio suite setting during initial angiography (DSA), respective cranial surgery (OP). S, surgeon; SA, surgical assistant; SN, surgical nurse; N, neuroradiologist; NAV, neuro-navigation system; green, X-ray arms/detector systems, ceiling mounted arm retracted during surgery; yellow, operative microscope; blue, patient table; white, DSA monitor; grey, surgical table. (B), (D) Images of positioning and the intraoperative situation in the spinal set up with the femoral catheter already in position. (C), (E) Images of positioning and the intraoperative situation in the cranial set up using a radiolucent Mayfield© clamp. In both cases the C-arm is retracted from the situs.
Under general anaesthesia angiography was performed via the routine femoral approach in prone position to place the catheter and illustrate the pathology. After that, the catheter was fixed and the patient positioned for surgery. Details on patient positioning in spinal surgery have been published previously [Grams et al. 2011]. In cranial surgery a radiolucent carbon head clamp was used (Figure 1). Baseline angiography was performed with different routine and individual projections and correlated with the data for neuronavigation. The ceiling-mounted C-arm was retracted from the patient allowing optimal neurosurgical approach. The capability to perform immediate monoplane control angiographies was maintained throughout the entire procedure, whereas three-dimensional rotational angiography was provided on demand. The following neurosurgical procedures were performed in the common manner. In deep-seated cranial lesions the optimal entry point was determined by neuronavigation and additionally correlated with real-time intraoperative tissue surface marking using a small metal clamp whenever necessary as illustrated in Figures 2, 3 and 4. Intraoperative and postoperative angiography were performed in all cases to confirm complete elimination of the neurovascular lesion before wound closure.
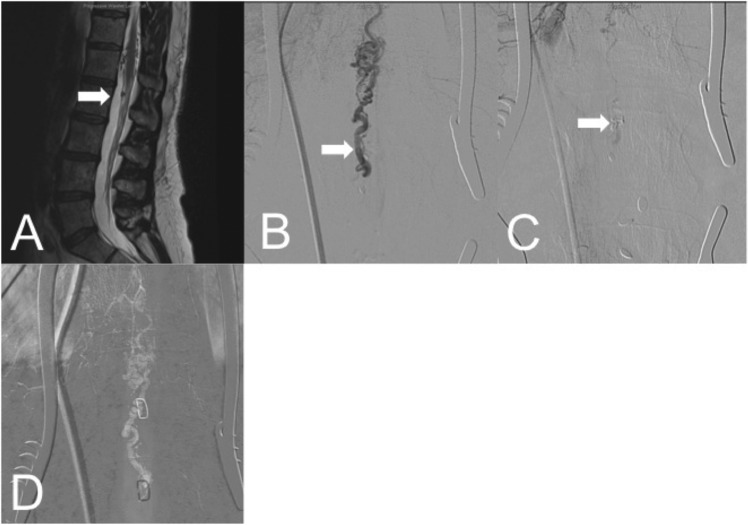
Figure 2.
Exemplary images of a ventral dural arteriovenous fistula (dAVF; case f) with the arteriovenous (AV) shunt located at level L1/2. (A) A sagittal T2-weighted MRI scan with a white arrow indicating the suggested AV shunt. After dorsal approach via laminotomy, anterior posterior intraoperative angiography (IOA; catheter placed in left segment artery Th11) localized the exact fistula point prior to occlusion (B) and confirmed complete occlusion after clipping of the feeding artery (C). (D) A roadmapping image with different metal clamp positions that were used to correlate the fistula point in situ (see also Figure 3).
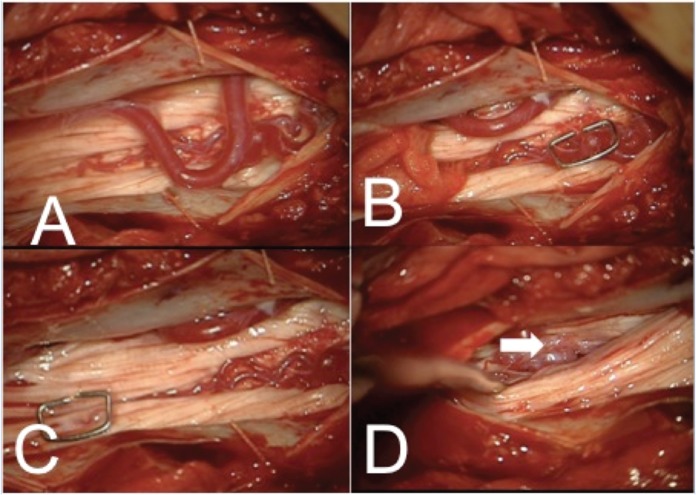
Figure 3.
Intradural situation after laminotomy L1 and L2 (case f) and careful dissection of filum tissue to approach the fistula. (A) may display the unclear vascular situation. Initially a vessel convolute located more cranially was suspected and marked with a metal clamp (B). Intraoperative angiography (IOA) (see Figure 2D), however, located the arteriovenous (AV) shunt more caudally (C) where it could be approached (white arrow (D)) and occluded.
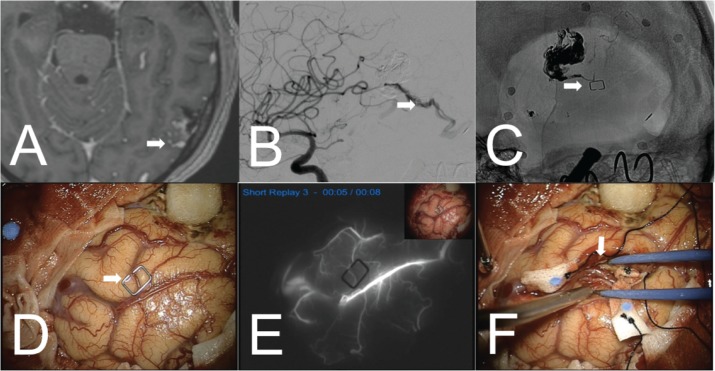
Figure 4.
Initial T1-weighted contrast enhanced MRI scan of the ‘remnant’ fistulous arteriovenous malformation (AVM) left temporo-occipital (A) and initial intraoperative angiography (IOA) displaying early venous drainage (B). Correlation of the deep-seated fistula point via roadmapping using a metal clamp (C), (D). (E) Indocyanine-green angiography (ICG) angiography prior to tissue dissection could not reveal the arteriovenous (AV) shunt located in eloquent temporodorsal area (F).
Results
Subjects
During the 28-month study period a total of 451 patients with neurovascular lesions [321 patients with 492 intracranial aneurysms (IAs) [Mueller et al. 2011], 88 arteriovenous malformations (AVMs) and 42 dural arteriovenous fistulas (dAVFs)] were admitted to our department during the observation period. Clinical and radiological details can be found in Table 1. Six out of these 451 patients (~1.3%) with neurovascular lesions underwent treatment in the angio suite during the observation period: three patients with four AVMs and three patients with three dAVFs.
Indications for hybrid treatment
Each case was routinely discussed in the interdisciplinary neurovascular conference including experienced neurosurgeons and interventionalists. Indication for combined treatment in a hybrid suite with repetitive IOA procedures was based on preoperative neuroimaging and included only cases that were regarded to be at increased risk for incomplete treatment or difficult to localize during surgery. Rather diffuse, noncompact AVMs and dAVFs were selected for angio suite treatment.
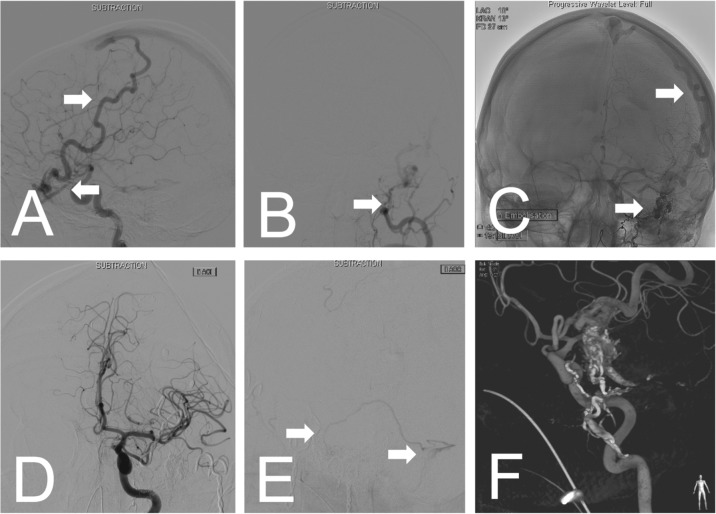
In the following cases angio suite treatment was unanimously decided. (a) Paraparesis due to a mixed pial and intramedullary AVM at level Th 9/10 with small collateral feeders from Th9 and Th10 segmental artery forming a mainly ventrally located nidus. Interventional approach was not possible due to dissection in the feeding segmental artery Th10. (b) Chronic headache caused by frontal dAVF fed by multiple feeders including left ophthalmic artery which was considered not in first line treatable by endovascular approach (Figure 5). (c) Intracerebral haemorrhage by left temporo-occipital AVM (Spetzler-Martin Grade II) in a patient with another left temporal AVM and a small fistulous left temporo-occipital AVM. Prior embolization completely occluded the symptomatic AVM, the left temporal AVM was only partially occluded. During the procedure ‘de novo’ arteriovenous (AV) shunting occurred, revealing the fistulous left temporo-occipital AVM. The latter could not be embolized due to small arterial branches arising on level with the fistula, supplying cortical tissue (Figure 4). (d) Left-sided tinnitus caused by fronto-temporo-basal dAVF (Cognard Type IV) with multiple feeders from ethmoidal branches of the external carotid artery and enlarged ophthalmic artery and a small central vessel convolute. Prior embolization allowed only partial occlusion of the lesion and revealed ‘de novo’ AV shunting during treatment. Further embolization via the ophthalmic artery was considered as too dangerous. (e) ICH caused by very small pial AVF left angular involving a middle cerebral artery branch and the vein of Labbé, not accessible for (super-)selective embolization. Preoperative functional MRI (fMRI) showed localization near the speech area. (f) Mild paraparesis caused by spinal intradural perimedullary AVF with fistula point at level L1/2, caudo-ventrally to the medullary cone, fed by segmental artery Th11 (Figures 2 and 3). For details see Table 2.
Figure 5.
Exemplary images (case (b)) showing a diffuse frontal dural arteriovenous fistula (dAVF). The main feeder is a dilated ophthalmic artery draining via a dilated superficial vein into the superior sagittal sinus (A). Additional multiple feeders come from ethmoidal branches of the external carotid artery (B). Initial embolization was incomplete leaving the main feeder and some small ethmoidal feeders untouched, still showing arteriovenous (AV) shunting (C). During the procedure recruitment of new AV shunts feeding the fistula was observed. Therefore. surgery in the angio suite was planned to assure localization of all feeders and control complete obliteration. After obliteration of the main AV shunts, a new AV shunt draining via a superficial temporal vein into the sigmoid sinus was observed by angiographic control (E). Finally, the fistula was completely occluded. (F) The three-dimensional reconstruction of the control by rotational angiography.
Table 2.
Specifications of vascular target lesions, as well as surgical and angiographical procedures of all treated patients (n = 6).
| Age, Sex | Target Lesion | Target Type | Lesion Type1 | Specifications | Technical Data | |
|---|---|---|---|---|---|---|
| (a) | 37, f | Spinal AVM Th10 | Solitary | Perimedullary AVM | Feeder: segment artery th10 | Clipping: 2 Sugita© Clips |
| Drainage: Ventral perimedullary veins Th 9/10 | Coagulation of feeders | |||||
| Nidus size: 10 mm × 13 mm | Angiographical series: 17 | |||||
| MRI: Medullary oedema th10 | Duration of surgery: 178 min | |||||
| Monitoring: SEP, MEP, ICG | ||||||
| Approach: laminotomy Th 8,9,10 | ||||||
| Position: prone | ||||||
| (b) | 40, m | Frontal dAVF | Solitary | Type III | Feeder: ophthalmic artery, ethmoidal branches and meningeal branches of external carotid artery | Clipping: 3 Sugita© Clips |
| Drainage: via dilated cortical vein to SSSFistula point: multiple, no nidus | Coagulation of feeders | |||||
| Partial obliteration of SSS | ||||||
| Angiographical series: 17 | ||||||
| Duration of surgery: 300 min | ||||||
| Monitoring: SEP, MEP, ICG | ||||||
| Approach: bifrontal | ||||||
| Position: supine | ||||||
| (c) | 41, f | (I) Left temporo-dorsal fistulous AVM, (II) partially occluded left temporal AVM, (III) completely occluded left parieto-occipital AVM | Multiple | Grade II (I) | Feeder: angular artery | Resection of (I) and (II) |
| Grade I (II) | Drainage: via 2 cortical veins into torcula | Angiographical series: 14 | ||||
| Grade III (III) | Nidus size: 10 mm × 15 mm | Duration of surgery: 234 min | ||||
| Endovascular Treatment: Initial complete occlusion (Onyx©) of (III), partial occlusion of (II) | Monitoring: Neuronavigation, Ultrasound, SEP, MEP | |||||
| ‘De novo’ shunting: (I) | Approach: temporo-parietal craniotomy | |||||
| Position: supine | ||||||
| (d) | 42, f | Partially occluded right fronto-temporo-basal dAVF | Solitary | Type IV | Feeder: enlarged ophthalmic artery (3 mm), ethmoidal branches of external carotid artery | Clipping: 3 Sugita© Clips |
| Drainage: via dilated cortical vein (6 mm) to SSS | Angiographical series: 18 | |||||
| Fistula point: central fistulous vessel convolute | Duration of surgery: 175min | |||||
| Endovascular treatment: Initial partial embolization (Onyx©) via ethmoidal branches | Monitoring: Micro-Doppler | |||||
| ‘De novo’ shunting: ethmoidal branches | Approach: pterional | |||||
| Position: supine | ||||||
| (e) | 68, f | Left frontal pial AVF | Solitary | Type III | Feeder: Middle cerebral artery, insular branches | Bipolar coagulation of nidus |
| Drainage: via vein of Labbé and temporal cortical vein to sigmoid sinus | Angiographical series: 9 | |||||
| Fistula point: small vessel convolute | Duration of surgery: 112min | |||||
| Monitoring: ICG, SEP, MEP | ||||||
| Approach: pterional | ||||||
| Position: supine | ||||||
| (f) | 51, f | Spinal dAVF L1 | Solitary | Perimedullary Fistula | Feeder: segment artery Th11, radiculomed. branch | Clipping: 2 Sugita© Clips |
| Fistula point: ventral to cone (L1/2) | Angiographical series: 21 | |||||
| Drainage: small convolute ventral to cone (L1) | Duration of surgery: 195min | |||||
| MRI: significant venous congestion | Monitoring: SEP,MEP | |||||
| Approach: laminotomy L1 and L2 | ||||||
| Position: prone |
According to Spetzler–Martin or Cognard, respectively.
AVF, arteriovenous fistula; AVM, arteriovenous malformation; dAVF, dural arteriovenous fistula; ICG, indocyanine-green angiography; L, lumbar; MEP, motor evoked potentials; SEP, sensory evoked potentials; SSS, superior sagittal sinus; Th, thoracic.
Sugita© Mizuho Medical Inc., Tokyo, Japan; Onyx© ev3 Endovascular Inc., Plymouth, MN, USA.
In all six patients complete occlusion of the neurovascular lesions was confirmed before wound closure in the angio suite set up and in follow-up examination using conventional biplane angiography 12 months after treatment. Overall, Glasgow Outcome Score (GOS) was excellent (GOS=5) in all patients at the 12-month follow up.
Discussion
Indications for AVMs and dAVFs
The impact of IOA findings on treatment procedures for AVMs has been reported in isolated series. In the series from Barrow and colleagues surgery was altered in seven out of 39 cerebral (18%) and two out of three spinal (67%) AVMs [Barrow et al. 1992]. Yanaka and colleagues reported alteration of surgery in one out of 20 (5%) cerebral AVMs [Yanaka et al. 2003], Martin and colleagues reported alteration of surgery in five out of 50 (10%) cerebral AVMs [Martin et al. 1990] and Vitaz and colleagues reported alteration of surgery in 28 out of 98 (29%) cerebral AVMs [Vitaz et al. 1999]. Chalouhi and colleagues reported that IOA revealed residual nidus, respective fistula, in eight out of 97 (8.2%) cerebral AVMs and three out of 18 (18.8%) cerebral dAVFs [Chalouhi et al. 2012]. In all of these studies IOA was performed with portable fluoroscopic equipment, providing single plane images only. A recent study of Dehdashti and colleagues reported treatment of six AVMs using biplanar rotational IOA. Unfortunately, authors did not comment on potential alteration of surgery [Dehdashti et al. 2009].
In all above-named studies IOA was routinely performed in all reported cases. Specific indications for IOA in the treatment of different variants of cerebral or spinal AVMs or dAVFs have therefore not been discussed.
In this study the use of IOA was considered as indicated in the minority of cases, namely in three out of 88 (3%) AVMs and four out of 42 (10%) dAVFs .
In cerebral lesions two main indications for IOA can be assessed: diffuse lesions with multiple deep-seated feeders (cases (b), (c) and (d)) and small deep-seated lesions located in eloquent regions (case (e)). In both cases, IOA was used to locate and approach the lesions causing minimal tissue manipulation. In addition, in two cases preoperative angiography revealed ‘de novo’ shunting during prior partial embolization (cases (c) and (d)). In these cases, such newly recruited feeders might be missed during surgery without IOA control.
In spinal lesions, IOA can be foremost helpful to differ pathological from normal perimedullary or intramedullary vascular structures, especially in ventrally located lesions which are difficult to approach and cannot be displayed by ICG (cases (a) and (f)). Biplane angiography allows three-dimensional visualization of feeders without manipulation or dissection of spinal cord tissue which is often necessary when using ICG angiography or microvessel Doppler control. Barrow and colleagues already reported that dissection and exposition of vessels in these spinal AVM is limited, which may lead to nonidentification of feeders and higher rates of residual lesions [Barrow et al. 1992]. Dorsally located perimedullary AVMs and dural AVMs arising from the radicular artery with the AV shunt located near the root entry zone are naturally much easier to access, visualize and completely occlude. The radiological key features of the cases in which treatment in the angio suite was performed are summarized in Figure 6.
Figure 6.
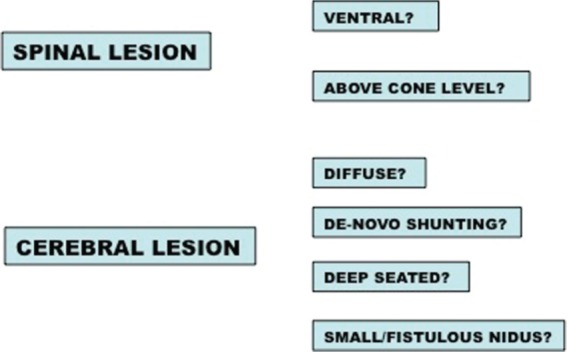
The key features of the neurovascular lesions that were considered for angio suite treatment in this series.
Indications for IAs
None of the IAs that underwent occlusion in our centre was subjected to angio suite treatment. This is remarkable as several studies reported clip placement revisions in aneurysm surgery due to IOA findings in up to 27% of cases, preventing incomplete securing or parent vessel occlusion [Tang et al. 2002; Vitaz et al. 1999]. As 5–7.3% of surgically treated IA are unexpectedly incompletely occluded [Kivisaari et al. 2004] and parent vessel occlusion occurs in 3–9% of cases [Friedman and Kumar, 2009; Kumar and Friedman, 2009; Tang et al. 2002], systematic IOA is expected to decrease these numbers. One group found an IA size exceeding 15 mm in maximum diameter independent predictor for clip revision, respective necessity of IOA [Tang et al. 2002]. The nonuse of this tool as a routine procedure in treatment of IA in our centre is presumably based on well-established neurovascular treatment procedures and individual experience of surgeons and interventionalists. In our opinion, ICG angiography allows the surgeon to control the patency of the parent vessels and branches arising from the lesion. Small perforator vessels, which are foremost at risk of obliteration, however, can usually not be controlled by imaging at all, neither by ICG angiography nor by IOA.
Angiography-related complications
In general, IOA-related complications have been reported to be very low, not exceeding 3% in larger series [Friedman and Kumar, 2009]. In our small series occlusion of a segment artery and the radiculo-medullary branch occurred. We attribute that to the long intra-arterial placement of the catheter, probably causing thrombosis. On the other hand, the observed vessel occlusion might rather have occurred consecutively to dAVF occlusion. Expectedly, due to sufficient collateral blood supply at level Th11, no correlated acute or delayed neurologic deficit occurred. Long-term placement of catheters in segment arteries with known limited collateralization though, such as in upper thoracic level, should be avoided.
Financial matters
Acquisition of a new hybrid operating room is a major investment for hospital owners. Costs are estimated between US$1.2 million and US$5.0 million, and beyond, for imaging systems solely, depending on brand and specifications. In addition, high-tech ORs, suitable for hybrid procedures, cost approximately double the investment and maintenance of conventional ORs [Kpodonu, 2010]. In comparison, for ‘on-demand’ hybrid procedures in our institution we put the additional costs at roughly €1000 per procedure.
Summary
In neurovascular centres where IOA is not performed routinely, IOA can be performed on demand using a ‘tailored’ angio suite solution. This is an alternative to pre-installed hybrid operating rooms. In this study, we present six cases of a large series of neurovascular lesions that were preselected for angio suite treatment during a 28-month period.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: The authors declare that there are no conflicts of interest.
Contributor Information
Philipp Dammann, Department of Neurosurgery, University Hospital Essen, Hufelandstrasse 55, 45122 Essen, Germany.
Tobias Breyer, Institute for Diagnostic and Interventional Radiology and Neuroradiology, University Hospital Essen, Germany.
Karsten H. Wrede, Department of Neurosurgery, University Hospital Essen, Germany
Klaus-Peter Stein, Department of Neurosurgery, University Hospital Essen, Germany.
Isabel Wanke, Institute for Diagnostic and Interventional Radiology and Neuroradiology, University Hospital Essen, Germany Department of Neuroradiology, Hirslanden Clinic, Zurich, Switzerland.
Astrid E. Grams, Department of Neuroradiology, University Hospital Innsbruck, Medical University Innsbruck, Austria
Elke R. Gizewski, Department of Neuroradiology, University Hospital Innsbruck, Medical University Innsbruck, Austria
Marc Schlamann, Institute for Diagnostic and Interventional Radiology and Neuroradiology, University Hospital Essen, Germany.
Michael Forsting, Institute for Diagnostic and Interventional Radiology and Neuroradiology, University Hospital Essen, Germany.
I. Erol Sandalcioglu, Department of Neurosurgery, University Hospital Essen, Germany.
Ulrich Sure, Department of Neurosurgery, University Hospital Essen, Germany.
References
- Barrow D., Boyer K., Joseph G. (1992) Intraoperative angiography in the management of neurovascular disorders. Neurosurgery 30: 153–159 [DOI] [PubMed] [Google Scholar]
- Benes L., Wakat J., Sure U., Bien S., Bertalanffy H. (2003) Intraoperative spinal digital subtraction angiography: technique and results. Neurosurgery 52: 603-609; discussion 608–609. [DOI] [PubMed] [Google Scholar]
- Chalouhi N., Theofanis T., Jabbour P., Dumont A., Gonzalez L., Starke R., et al. (2012) Safety and efficacy of intra-operative angiography in craniotomies for cerebral aneurysms and arteriovenous malformations: a review of 1089 cases. Neurosurgery 71(2): E550–E551 [DOI] [PubMed] [Google Scholar]
- Dehdashti A., Thines L., Da Costa L., terBrugge K., Willinsky R., Wallace M., et al. (2009) Intraoperative biplanar rotational angiography during neurovascular surgery. Technical note. J Neurosurg 111: 188–192 [DOI] [PubMed] [Google Scholar]
- Enzmann D., Brody W., Djang W., Riederer S., Keyes G., Collins W., et al. (1983) Intraarterial digital subtraction spinal angiography. AJNR Am J Neuroradiol 4: 25–26 [PMC free article] [PubMed] [Google Scholar]
- Friedman J., Kumar R. (2009) Intraoperative angiography should be standard in cerebral aneurysm surgery. BMC Surg 9: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grams A., Gizewski E., Sandalcioglu I., Forsting M., Sure U. (2011) Indication, technique and benefit of intraoperative spinal digital subtraction angiography with a new setting in a patient with spinal arteriovenous malformation. Cent Eur Neurosurg 72: 149–151 [DOI] [PubMed] [Google Scholar]
- Kivisaari R., Porras M., Ohman J., Siironen J., Ishii K., Hernesniemi J. (2004) Routine cerebral angiography after surgery for saccular aneurysms: is it worth it? Neurosurgery 55: 1015–1024 [DOI] [PubMed] [Google Scholar]
- Kpodonu J. (2010) Hybrid cardiovascular suite: the operating room of the future. J Card Surg 25: 704-709 [DOI] [PubMed] [Google Scholar]
- Kumar R., Friedman J. (2009) Intraoperative angiography during cerebral aneurysm surgery. Neurocrit Care 11: 299–302 [DOI] [PubMed] [Google Scholar]
- Martin N., Bentson J., Vinuela F., Hieshima G., Reicher M., Black K., et al. (1990) Intraoperative digital subtraction angiography and the surgical treatment of intracranial aneurysms and vascular malformations. J Neurosurg 73: 526–533 [DOI] [PubMed] [Google Scholar]
- Mueller O., Schlamann M., Mueller D., Sandalcioglu I., Forsting M., Sure U. (2011) Intracranial aneurysms: optimized diagnostic tools call for thorough interdisciplinary treatment strategies. Ther Adv Neurol Disord 4: 267–279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murayama Y., Irie K., Saguchi T., Ishibashi T., Ebara M., Nagashima H., et al. (2011) Robotic digital subtraction angiography systems within the hybrid operating room. Neurosurgery 68: 1427–1432; discussion 1433. [DOI] [PubMed] [Google Scholar]
- Raabe A., Beck J., Gerlach R., Zimmermann M., Seifert V. (2003) Near-infrared indocyanine green video angiography: a new method for intraoperative assessment of vascular flow. Neurosurgery 52: 132–139; discussion 139. [DOI] [PubMed] [Google Scholar]
- Raabe A., Beck J., Rohde S., Berkefeld J., Seifert V. (2006) Three-dimensional rotational angiography guidance for aneurysm surgery. J Neurosurg 105: 406–411 [DOI] [PubMed] [Google Scholar]
- Schaller K., Kotowski M., Pereira V., Rufenacht D., Bijlenga P. (2011) From intraoperative angiography to advanced intraoperative imaging: the Geneva experience. Acta Neurochir Suppl 109: 111–115 [DOI] [PubMed] [Google Scholar]
- Smith R. (1977) Intraoperative intracranial angiography. Neurosurgery 1: 107–110 [DOI] [PubMed] [Google Scholar]
- Snyder L., Spetzler R. (2011) Current indications for indocyanine green angiography. World Neurosurg 76: 405–406 [DOI] [PubMed] [Google Scholar]
- Takahashi M., Bussaka H., Nakagawa N. (1984) Evaluation of the cerebral vasculature by intraarterial DSA - with emphasis on in vivo resolution. Neuroradiology 26: 253–259 [DOI] [PubMed] [Google Scholar]
- Tang G., Cawley C., Dion J., Barrow D. (2002) Intraoperative angiography during aneurysm surgery: a prospective evaluation of efficacy. J Neurosurg 96: 993–999 [DOI] [PubMed] [Google Scholar]
- Vitaz T., Gaskill-Shipley M., Tomsick T., Tew J., Jr (1999) Utility, safety, and accuracy of intraoperative angiography in the surgical treatment of aneurysms and arteriovenous malformations. AJNR Am J Neuroradiol 20: 1457–1461 [PMC free article] [PubMed] [Google Scholar]
- Yanaka K., Matsumaru Y., Okazaki M., Noguchi S., Asakawa H., Anno I., et al. (2003) Intraoperative angiography in the surgical treatment of cerebral arteriovenous malformations and fistulas. Acta Neurochir (Wien) 145: 377–382; discussion 382–383. [DOI] [PubMed] [Google Scholar]