Abstract
Background
Pediatrics residents have few opportunities to perform cardiopulmonary resuscitation (CPR). Enhancing the quality of CPR is a key factor to improving outcomes for cardiopulmonary arrest in children and requires effective training strategies.
Objective
To evaluate the effectiveness of a simulation-based intervention to reduce first-year pediatrics residents' time for 3 critical actions in CPR: (1) call for help, (2) initiate bag-mask ventilation, and (3) initiate chest compressions.
Methods
A prospective study involving 31 first-year pediatrics residents at a children's hospital assigned to an early or late (control) intervention group. Residents underwent baseline assessment followed by repeat evaluations at 3 and 6 months. Time to critical actions was scored by video review. A 90-minute educational intervention focused on skill practice was conducted following baseline evaluation for the early-intervention group and following 3-month evaluation for the late-intervention group. Primary outcome was change in time to initiating the 3 critical actions. Change in time was analyzed by comparison of Kaplan-Meier curves, using the log-rank test. A 10% sample was timed by a second rater. Agreement was assessed using intraclass correlation (ICC).
Results
There was a statistically significant reduction in time for all 3 critical actions between baseline and 3-month evaluation in the early intervention group; this was not observed in the late (control) group. Rater agreement was excellent (ICC ≥ 0.99).
Conclusions
A simulation-based educational intervention significantly reduced time to initiation of CPR for first-year pediatrics residents. Simulation training facilitated acquisition of critical CPR skills that have the potential to impact patient outcome.
What was known
Pediatrics residents need to acquire cardiopulmonary resuscitation (CPR) skills, yet opportunities in day-to-day practice are scarce.
What is new
Simulation-based training measured time efficiency gains in 3 critical actions in CPR.
Limitations
Single-site, single-specialty study may limit generalizability. Potential exists for bias in the assignment to the study versus control group. Assessment was focused on time to initiation, not quality of execution of the skills.
Bottom line
Simulation training resulted in time efficiency gains in initiating key components of CPR in first-year pediatrics residents.
Editor's Note: The online version of this article contains instructional content (59.5KB, doc) , the baseline skills survey (40.5KB, doc) , and the experience survey (50.5KB, doc) used in this study.
Introduction
Pediatric cardiopulmonary arrest is a rare event, and timely, high-quality cardiopulmonary resuscitation (CPR) improves outcomes.1–4 Pediatrics residents have a critical role in initiating life-saving interventions yet have little opportunity to develop or maintain their resuscitation skills.5–7
The timely delivery of high-quality CPR is a key dimension of good care, and delays in initiating CPR have a detrimental effect on patient outcome regardless of the quality of resuscitation.8–12 Pediatrics residents have demonstrated good knowledge of CPR and pediatric advanced life support (PALS), as reflected by high scores on written tests. At the same time, many residents show suboptimal clinical skills in mock code performance.7,13 The paucity of opportunity to practice these skills makes the application to actual patient care challenging.
Simulation-based training has demonstrated effectiveness in promoting skill acquisition.14–26 There is growing research in pediatrics evaluating the effect of simulation-based training on the clinical performance of PALS skills during resuscitations.13,20,22,27–31 Most practicing primary care pediatricians or clinic-based subspecialists are unlikely to perform CPR frequently, and residency training should prepare the pediatrician to appropriately initiate CPR until help arrives. Our study uses standardized simulations to assess first-year pediatrics residents in 3 critical actions of CPR: (1) calling for help, (2) initiation of bag-mask ventilation (BMV), and (3) initiation of chest compressions. Our hypothesis was that a simulation-based educational intervention will reduce residents' time to initiation of CPR.
Methods
Thirty-one first-year pediatrics residents from a large, urban, tertiary care children's hospital participated from July 2007 through May 2008. All were certified in basic life support (BLS) and CPR 1 month prior to the beginning of the study. We randomized residents based on their clinical schedule into 2 groups: (1) early-intervention group or (2) late-intervention (control) group. Each resident underwent a baseline evaluation followed by repeat evaluations at 3 and 6 months. Our design was a prospective trial using a wait-list control group with the simulation-based educational intervention immediately following baseline evaluation in the early-intervention group and following the 3-month evaluation in the late-intervention group.32 To capture their increasing clinical exposure, a self-reported experience survey was completed at each evaluation period (provided as online supplemental material).
Our educational intervention consisted of a 90-minute small group (maximum of 9 participants) simulation-based workshop that practiced multiple patient care scenarios with structured feedback focused on CPR and resuscitation skills. The content consisted of assuming the role of first responder and demonstrating appropriate actions, discussing the American Heart Association 2005 Guidelines for CPR and the physiology supporting the recommendations, the importance of timely intervention, skill practice with BMV and ancillary airway equipment, the practice of proper technique for chest compressions, and discussion of basic rhythm management as it pertains to defibrillation and use of epinephrine (provided as online supplemental material).8
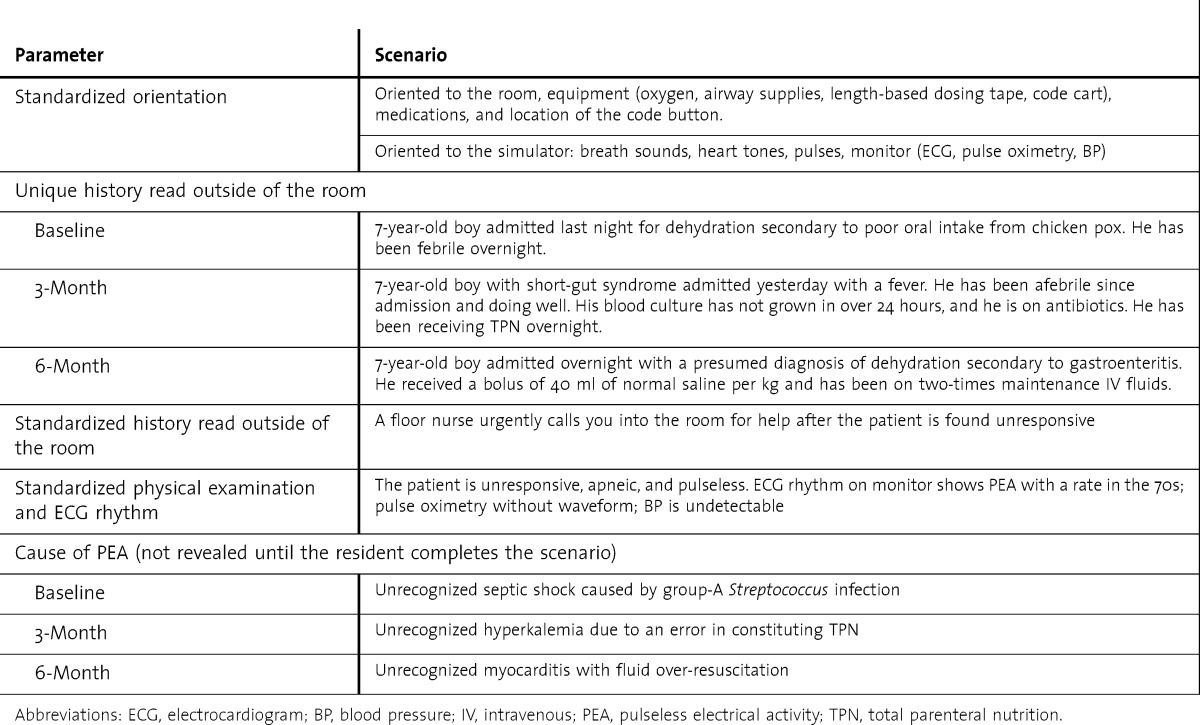
The evaluation consisted of a standardized simulated patient care scenario. Each resident individually participated, with the assistance of a simulated nurse, in 3 different scenarios over the course of 9 months. Prior to each scenario, the resident completed an orientation to the simulator, room, equipment, and medications. The patient history was read outside of the room; the resident then entered the room and intervened as if in a real clinical setting. To help blind the residents to the actions of interest but maintain standardization of examination and management, the scenario at each evaluation period had a unique history, yet in all the scenarios, the patient is found unresponsive in a pulseless electrical activity arrest rhythm (table 1).
TABLE 1.
Standardized Simulation Scenarios
All scenarios were conducted in a standardized simulation laboratory and recorded on video for later review. We used a pulse-generating MegaCode Kid manikin and produced monitor outputs using software provided with the SimBaby manikin (Laerdal Medical, Wappingers Falls, NY). Resident participants were blinded to the timed data collection and actions of interest. In both groups, after all 3 critical actions of CPR were initiated, a single instructor (J.C.R.) facilitated application of the advanced PALS protocols as they relate to pulseless arrest (eg, rhythm, defibrillation versus no defibrillation, medications, continuing CPR, endotracheal intubation skills) until arrival of the “code team.” In order to blind the residents to the outcome of interest, scenarios continued well after BLS was started and the facilitator addressed additional learning goals. This provided an educational opportunity for the nonintervention group so the experience felt worthwhile to them. There was no instruction on BLS and CPR during the scenario. If a resident did not initiate all 3 critical actions of CPR at 5 minutes, the instructor intervened.
Initiation of CPR was defined by 3 critical actions: (1) calling for help, (2) initiation of BMV, and (3) initiation of chest compressions. The time-to-action data were recorded from the moment the resident entered the room by using video review (2 camera views: side and foot of bed). Data were collected that measured each resident's time to initiate the 3 critical actions of CPR. To assess interrater reliability, a 10% sample was reviewed and timed by a second rater.
The primary outcome measure was the change in time to initiate the 3 critical actions of CPR from baseline to the 3-month evaluation in the early-intervention group compared to that in the late-intervention (control) group. The change in time was analyzed by comparing Kaplan-Meier curves, using the log-rank test with a P value ≤ .05. To provide a measure of central tendency, medians with intraquartile ranges were calculated. Because median data will not account for those who never completed the critical actions, we compared Kaplan-Meier curves to determine statistical significance. Interrater reliability was assessed using intraclass correlation (ICC). The clinical experience surveys were compared using the χ2 statistic with a P level ≤ .05. Data were analyzed using Stata version 10.1 software (StataCorp LP, College Station, TX).
The Children’s Memorial Hospital Institutional Review Board approved this study, and all participants signed informed consent agreeing to video recording of sessions.
Results
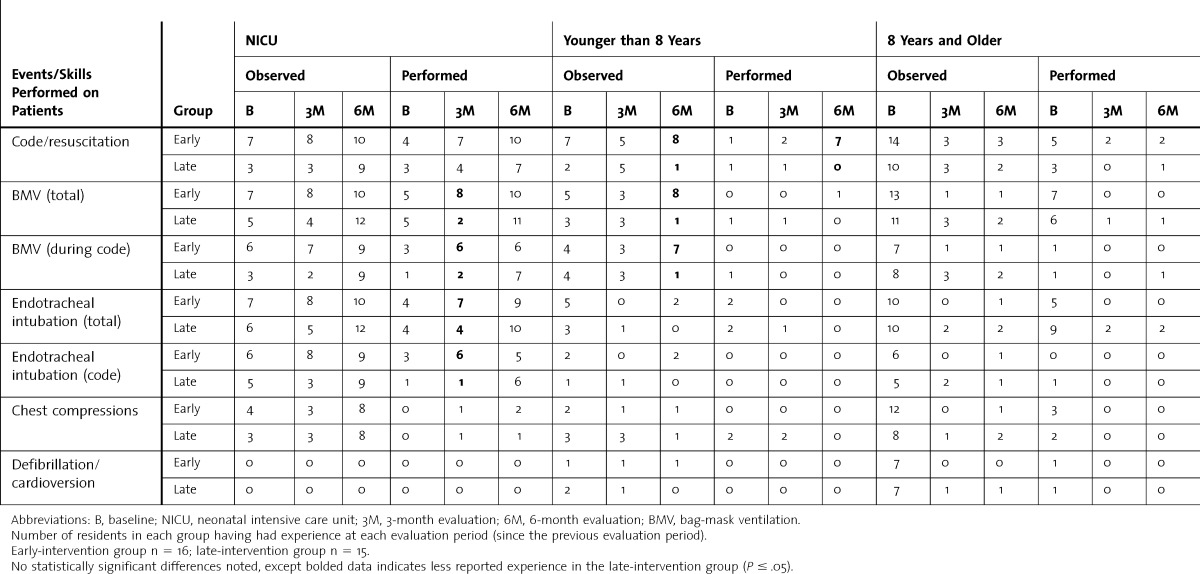
At baseline, there were no significant differences between the groups in medical school and clinical experience, previous simulation training, and participation in mock codes. There also were no significant differences between the groups at all 3 evaluation periods regarding their experience hearing or reading about resuscitation skills. There were some differences between the groups reported in observing and participating in resuscitation skills at the 3- and 6-month evaluations (table 2).
TABLE 2.
Comparison of Clinical Experience Between Early- and Late-Intervention Groups
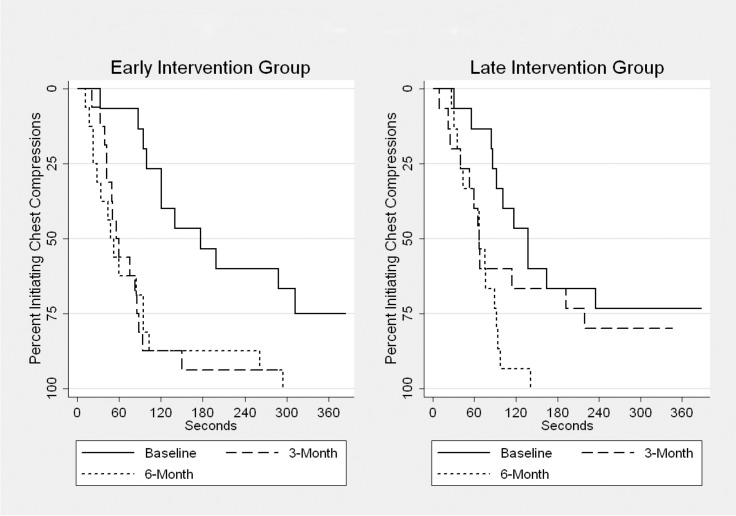
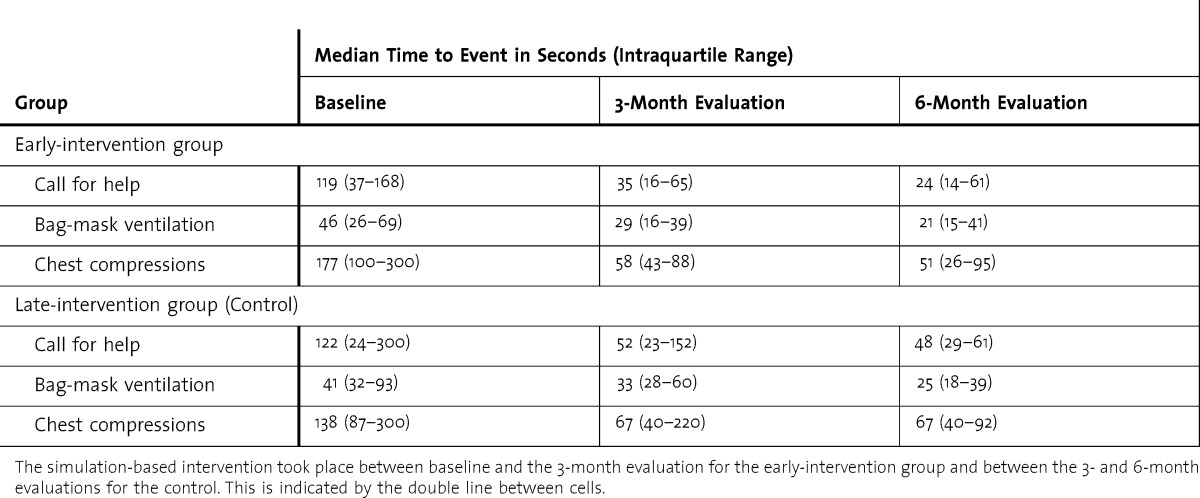
Each resident participated in 3 different individual simulation scenarios, for a total of 93 evaluations. The primary outcome measure (change in time from baseline to the 3-month evaluation) was analyzed separately for all 3 critical actions of CPR. In the early-intervention group there was a statistically significant reduction in the time to call for help (P < .01), initiation of BMV (P < .04), and initiation of chest compressions (P < .01). This was not seen in the call for help (P = .16), BMV (P = .18), and chest compressions (P = .28) in the late-intervention (control) group. The differences between each group's time to initiation of chest compressions at each evaluation period are illustrated in the figure.
FIGURE.
Time to Initiation of Chest Compressions
Median times to the critical actions of CPR are shown in table 3. Rater agreement for each of the 3 critical actions was excellent with an ICC ≥ 0.99.
TABLE 3.
Median Time to Critical Actions of CPR
Discussion
Our study demonstrates the efficacy of simulation training in reducing time to initiation of CPR for first-year pediatrics residents. Using an objective time-based measure to evaluate individual resident's performance with a late-intervention group to control for clinical experience allowed us to evaluate the impact of our educational intervention.
An important finding was the reduction in time to initiation of chest compressions. At baseline, most residents took more than 2 minutes to initiate chest compressions in a pulseless patient, and 25% never initiated compressions. This finding is similar to those in a study of pediatrics residents participating in mock codes in which 66% failed to start compressions within 1 minute of pulselessness, and 33% never started compressions.6 Our study demonstrated that the early-intervention group significantly reduced the time to initiation of compressions, and all members of this group started compressions.
The goal of our intervention was to reduce both the time to initiation of CPR and the variation in performance among the members of the first-year resident cohort. We wanted to improve the performance of the entire group and help poorly performing residents initiate CPR in a timely fashion. We used Kaplan-Meier survival curves to more accurately capture the performance of residents who may never have initiated the action and evaluate the effect of our intervention in reducing performance variation for the entire group (illustrated by more vertical/steeper curve). The intraquartile range of median times also narrowed after the intervention, reflecting this decrease in performance variation. By focusing our study on first-year residents, we were able to understand the effect of our educational intervention on a relatively naïve group of learners with fewer confounding clinical and educational experiences. Furthermore, we felt demonstrating timely initiation of CPR was crucially important for a first-year resident who would be a likely first hospital responder to a critically ill child.
The chance of survival is greater the sooner CPR is initiated in a pulseless patient; few studies have focused on individual performance in terms of time to initiation of CPR.27,30,33–35 Andreatta et al36 showed a positive correlation between increased frequency of resident participation in mock code training sessions and increased survival rates for hospitalized pediatrics patients who experienced a cardiopulmonary arrest. Simulation provides the opportunity to train individuals in the care of rare but life-threatening events in a standardized manner.
All resident participants were certified in BLS and CPR at the same time, 1 month prior to participating in the study, and we believe most would start CPR in a timely fashion. However, when patients are in a more complex hospital environment, trainees may be distracted from the basics of providing high-quality CPR.
Our investigation has several limitations. Both groups had similar baseline clinical and educational experiences; however, the groups reported at the 3-month evaluation some differences in experience, with 81% of the early-intervention group having completed a neonatal intensive care unit rotation by the 3-month evaluation compared to only 47% of the late-intervention group. In addition, our study was conducted in a single institution with a limited number of participants. The assignment of residents to the intervention and control groups was not randomized but based on schedule and availability. Our outcome of interest was the change in time to initiation of the 3 critical actions of CPR, but we did not examine the quality of those interventions. Finally, our study was not able to assess whether the gains in our interventions were sustainable.
Future research should examine the quality of CPR performance, the challenges to providing timely CPR in a complex hospital environment, and the optimal timing for ongoing educational efforts.
Resources needed for this intervention include the cost of 1 instructor and 1 staff member to set up the equipment and run the simulator. Each session ran 90 minutes plus 30 minutes of setup and breakdown, resulting in 2 hours per session times 6 sessions for a total of 12 hours. At $150 an hour, the cost (excluding faculty time) is estimated at $1,800, while faculty time costs vary by specialty and academic role. Residents accepted the simulation training and expressed thanks for the opportunity to practice, improve, and reduce some of their anxiety caring for critically ill children.
Conclusion
A simulation-based educational intervention significantly reduced time to initiation of CPR for first-year pediatrics residents. Residents improved their time to initiation of chest compressions with greatly decreased performance variation. Simulation training facilitated the acquisition of these critical skills that impact patient outcome, and this type of educational strategy is feasible for pediatrics residency programs.
Footnotes
Joshua C. Ross, MD, is Assistant Professor of Pediatrics and Medicine, Division of Emergency Medicine, Department of Pediatrics and Medicine, University of Wisconsin School of Medicine and Public Health, American Family Children’s Hospital; Jennifer L. Trainor, MD, is Associate Professor of Pediatrics, Division of Emergency Medicine, Department of Pediatrics, Northwestern University Feinberg School of Medicine, Ann and Robert H. Lurie Children’s Hospital of Chicago; Walter J. Eppich, MD, MEd, is Assistant Professor of Pediatrics and Medical Education, Division of Emergency Medicine, Department of Pediatrics, Northwestern University Feinberg School of Medicine, Ann and Robert H. Lurie Children’s Hospital of Chicago; and Mark D. Adler, MD, is Associate Professor of Pediatrics and Medical Education, and Director, kidSTAR Medical Education Program, Division of Emergency Medicine, Department of Pediatrics, Northwestern University Feinberg School of Medicine, Ann and Robert H. Lurie Children’s Hospital of Chicago.
Funding: The authors report no external funding source for this study.
The authors would like to thank Dr. Ellen Wald for help with editing the manuscript.
References
- 1.Topjian AA, Berg RA, Nadkarni VM. Pediatric cardiopulmonary resuscitation: advances in science, techniques, and outcomes. Pediatrics. 2008;122(5):1086–1098. doi: 10.1542/peds.2007-3313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meert KL, Donaldson A, Nadkarni V, Tieves KS, Schleien CL, Brilli RJ, et al. Multicenter cohort study of in-hospital pediatric cardiac arrest. Pediatr Crit Care Med. 2009;10(5):544–553. doi: 10.1097/PCC.0b013e3181a7045c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moler FW, Meert K, Donaldson AE, Nadkarni V, Brilli RJ, Dalton HJ, et al. In-hospital versus out-of-hospital pediatric cardiac arrest: a multicenter cohort study. Crit Care Med. 2009;37(7):2259–2267. doi: 10.1097/CCM.0b013e3181a00a6a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peberdy MA, Kaye W, Ornato JP, Larkin GL, Nadkarni V, Mancini ME, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58(3):297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 5.Fiedor ML. Pediatric simulation: a valuable tool for pediatric medical education. Crit Care Med. 2004;32(suppl 2):72–74. doi: 10.1097/01.ccm.0000110732.68981.52. [DOI] [PubMed] [Google Scholar]
- 6.Hunt EA, Vera K, Diener-West M, Haggerty JA, Nelson KL, Shaffner DH, et al. Delays and errors in cardiopulmonary resuscitation and defibrillation by pediatric residents during simulated cardiopulmonary arrests. Resuscitation. 2009;80(7):819–825. doi: 10.1016/j.resuscitation.2009.03.020. [DOI] [PubMed] [Google Scholar]
- 7.Nadel FM, Lavelle JM, Fein JA, Giardino AP, Decker JM, Durbin DR. Assessing pediatric senior residents' training in resuscitation: fund of knowledge, technical skills, and perception of confidence. Pediatr Emerg Care. 2000;16(2):73–76. doi: 10.1097/00006565-200004000-00001. [DOI] [PubMed] [Google Scholar]
- 8.American Heart Association. 2005 American Heart Association (AHA) guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) of pediatric and neonatal patients: pediatric basic life support. Pediatrics. 2006;117(5):e989–e1004. doi: 10.1542/peds.2006-0219. [DOI] [PubMed] [Google Scholar]
- 9.Palmisano JM, Akingbola OA, Moler FW, Custer JR. Simulated pediatric cardiopulmonary resuscitation: initial events and response times of a hospital arrest team. Respir Care. 1994;39(6):725–729. [PubMed] [Google Scholar]
- 10.Hunt EA, Walker AR, Shaffner DH, Miller MR, Pronovost PJ. Simulation of in-hospital pediatric medical emergencies and cardiopulmonary arrests: highlighting the importance of the first minutes. Pediatrics. 2008;121(1):e34–e43. doi: 10.1542/peds.2007-0029. [DOI] [PubMed] [Google Scholar]
- 11.Abella BS, Sandbo N, Vassilatos P, Alvarado JP, O'Hearn N, Wigder HN, et al. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrest. Circulation. 2005;111(4):428–434. doi: 10.1161/01.CIR.0000153811.84257.59. [DOI] [PubMed] [Google Scholar]
- 12.Abella BS, Alvarado JP. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA. 2005;293(3):305–310. doi: 10.1001/jama.293.3.305. [DOI] [PubMed] [Google Scholar]
- 13.White JR, Shugerman R, Brownlee C, Quan L. Performance of advanced resuscitation skills by pediatric housestaff. Arch Pediatr Adolesc Med. 1998;152(12):1232–1235. doi: 10.1001/archpedi.152.12.1232. [DOI] [PubMed] [Google Scholar]
- 14.Satava RM. The revolution in medical education—the role of simulation. J Grad Med Educ. 2009;1(2):172–175. doi: 10.4300/JGME-D-09-00075.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ziv A, Wolpe PR, Small SD, Glick S. Simulation-based medical education: an ethical imperative. Acad Med. 2003;78(8):783–788. doi: 10.1097/00001888-200308000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Beaubien JM, Baker DP. The use of simulation for training teamwork skills in healthcare: how low can you go. Qual Saf Health Care. 2004;13(suppl 1):51–56. doi: 10.1136/qshc.2004.009845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carol JS, Rudolph JW. Design of high reliability organizations in health care. Qual Saf Health Care. 2006;15(suppl 1):4–9. doi: 10.1136/qshc.2005.015867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McGaghie WC, Issenberg SB, Petrusa ER, Scalese RJ. A critical review of simulation-based medical education research: 2003–2009. Med Educ. 2010;44(1):50–63. doi: 10.1111/j.1365-2923.2009.03547.x. [DOI] [PubMed] [Google Scholar]
- 19.Issenberg SB, McGaghie WC, Petrusa ER, Lee Gordon D, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach. 2005;27(1):10–28. doi: 10.1080/01421590500046924. [DOI] [PubMed] [Google Scholar]
- 20.Weinberg ER, Auerbach MA, Shah NB. The use of simulation for pediatric training and assessment. Curr Opin Pediatr. 2009;21(3):282–287. doi: 10.1097/MOP.0b013e32832b32dc. [DOI] [PubMed] [Google Scholar]
- 21.Gordon JA, Vozenilek J. Executive summary of 2008 AEM consensus conference: the science of simulation in healthcare. Acad Emerg Med. 2008;15(11):971–977. [Google Scholar]
- 22.Eppich WJ, Adler MD, McGaghie WC. Emergency and critcal care pediatrics: use of medical simulation for training in acute pediatric emergencies. Curr Opin Pediatr. 2006;18(3):266–271. doi: 10.1097/01.mop.0000193309.22462.c9. [DOI] [PubMed] [Google Scholar]
- 23.Wayne DB, Butter J, Siddall VJ, Fudala MJ, Linguist LA, Feinglass J, et al. Simulation-based training of internal medicine residents in advanced cardiac life support protocols: a randomized trial. Teach Learn Med. 2005;17(3):210–216. doi: 10.1207/s15328015tlm1703_3. [DOI] [PubMed] [Google Scholar]
- 24.Wayne DB, Butter J, Siddall VJ, Fudala MJ, Wade LD, Feinglass J, et al. Mastery learning of advanced cardiac life support skills by internal medicine residents using simulation technology and deliberate practice. J Gen Intern Med. 2006;21(3):251–256. doi: 10.1111/j.1525-1497.2006.00341.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2004;79(suppl 10):70–81. doi: 10.1097/00001888-200410001-00022. [DOI] [PubMed] [Google Scholar]
- 26.Didwania A, McGaghie WC, Cohen ER, Butter J, Barsuk JH, Wade LD, et al. Progress toward improving the quality of cardiac arrest medical team responses at an academic teaching hospital. J Grad Med Educ. 2011;3(2):211–216. doi: 10.4300/JGME-D-10-00144.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nadel FM, Lavelle JM, Fein JA, Giardino AP, Decker JM, Durbin DR. Teaching resuscitation to pediatric residents: the effects of an intervention. Arch Pediatr Adolesc Med. 2000;154(10):1049–1054. doi: 10.1001/archpedi.154.10.1049. [DOI] [PubMed] [Google Scholar]
- 28.Donoghue AJ, Durbin DR, Nadel FM, Stryjewski GR, Kost SI, Nadkarni VM. Effect of high-fidelity simulation on Pediatric Advanced Life Support training in pediatric house staff: a randomized trial. Pediatr Emerg Care. 2009;25(3):139–144. doi: 10.1097/PEC.0b013e31819a7f90. [DOI] [PubMed] [Google Scholar]
- 29.Adler MD, Vozenilek JA, Trainor JL, Eppich WJ, Wang EE, Beaumont JL, et al. Development and evaluation of a simulation-based pediatric emergency medicine curriculum. Acad Med. 2009;84(7):935–941. doi: 10.1097/ACM.0b013e3181a813ca. [DOI] [PubMed] [Google Scholar]
- 30.Gerard JM, Thomas SM, Germino KW, Street MH, Burch W, Scalzo AJ, et al. The effect of simulation training on PALS skills among family medicine residents. Fam Med. 2011;43(6):392–399. [PubMed] [Google Scholar]
- 31.Tofil NM, Benner KW, Zinkan L, Alten J, Varisco BM, White ML. Pediatric intensive care simulation course: a new paradigm in teaching. J Grad Med Educ. 2011;3(1):81–87. doi: 10.4300/JGME-D-10-00070.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Boston: Houghton Mifflin; 2002. [Google Scholar]
- 33.Shilkofski NA, Nelson KL, Hunt EA. Recognition and treatment of unstable supraventricular tachycardia by pediatric residents in a simulation scenario. Simul Healthc. 2008;3(1):4–9. doi: 10.1097/SIH.0b013e31815bfa4e. [DOI] [PubMed] [Google Scholar]
- 34.Herlitz J, Bång A, Alsén B, Aune S. Characteristics and outcome among patients suffering from in hospital cardiac arrest in relation to the interval between collapse and start of CPR. Resuscitation. 2002;53(1):21–27. doi: 10.1016/s0300-9572(01)00485-3. [DOI] [PubMed] [Google Scholar]
- 35.Cooper S, Cade J. Predicting survival, in-hospital cardiac arrests: resuscitation survival variables and training effectiveness. Resuscitation. 1997;35(1):17–22. doi: 10.1016/s0300-9572(97)00020-8. [DOI] [PubMed] [Google Scholar]
- 36.Andreatta P, Saxton E, Thompson M, Annich G. Simulation-based mock codes significantly correlate with improved pediatric patient cardiopulmonary arrest survival rates. Pediatr Crit Care Med. 2011;12(1):33–38. doi: 10.1097/PCC.0b013e3181e89270. [DOI] [PubMed] [Google Scholar]