Abstract
Background
Birthrates during surgical residency appear to be rising. One assumption is that this is due to changes in the structure of surgical residencies.
Objective
The purpose of our study was to explore whether an increase in birthrates has occurred and the reasons for this.
Methods
We conducted an anonymous survey of current residents and alumni from 1976 to 2009 at a single university-based surgery training program.
Results
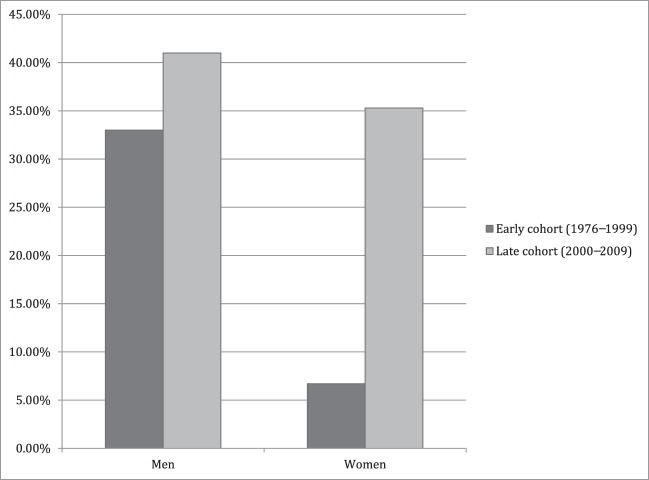
Alumni (46 of 116) and current residents (38 of 51) were surveyed, and our response rate was approximately 50% (84 of 167). Respondents were grouped into cohorts based on their residency start year. The early cohort consisted of residents starting residency between 1976 and 1999, and the late cohort consisted of residents starting residency between 2000 and 2009. The percentage of male residents with children during residency training was similar for the early and late cohorts (34% [10 of 29] versus 41% [9 of 22]). For female residents, there was a substantial increase in childbearing for the late cohort (7% [1 of 15] versus 35% [6 of 18]). Fifty-two percent (44 of 84) of the respondents who had children during residency reported that work hours and schedule had a negative effect on their decision to have children. Most respondents reported that availability or cost of child care, impact on residency, support from the program, increased length of training, or availability of family leave did not factor as concerns.
Conclusions
Childbearing during residency has increased in female residents in our study. Surgical residency programs may need to accommodate this change if they want to continue to recruit and retain talented residents.
What was known
Little is known about the factors related to the decision to have children during residency training.
What is new
A survey of current residents and alumni over a 30-year span at a university-based surgery training program.
Limitations
Single-site, single-specialty administration limits generalizability; the survey instrument is not validated.
Bottom line
Childbearing during residency has increased in female residents in this study. Surgical residency programs may need to accommodate this change if they want to continue to recruit and retain talented residents.
Introduction
Despite an increasing number of women choosing to pursue general surgery training, little is known about the factors related to the decision to have children during the residency years. Although women are still the minority sex in most surgical specialties, this is changing. In 2008, more than 30% of surgical resident and fellow positions were held by women.1 Because of the increasing presence of women in surgical specialties, we sought to determine how training affects the decision to have children for this growing part of the surgical workforce.
To our knowledge, no studies have specifically investigated pregnancy rates or other factors affecting childbearing during general surgery training. Anecdotal reports of increased pregnancy rates in general surgery residencies, and our own observations, motivated us to investigate the childbearing rate before and after duty hour reform.2 We sought to identify whether duty hour reform specifically has contributed to increased pregnancy rates among female general surgery residents. An additional goal of the study was to determine what factors, if any, contributed to the timing of residents having children, either during or after residency training was completed.
Methods
Current residents and alumni from general surgery residency over a span of more than 30 years from a large, university-based training program were sent an electronic survey. Participants were e-mailed a request to participate in the study, a description of the purpose of the study, and an embedded survey link. Two weeks later, they were sent a follow-up e-mail. Responses to the survey were anonymous.
When evaluating birthrates, responses were separated into 2 cohorts based on the initial residency training year of the respondent. July 2000 was chosen as the breakpoint between the 2 cohorts, as this was the first year in which residents completed most of their training within the 80-hour workweek reforms in the program. Although formal Accreditation Council for Graduate Medical Education work hour reforms were implemented in 2003, our institution began work hour reform in 2000. At that time, the 24-hour in-house call was minimized for chief residents, and back-to-back calls without days off began to be eliminated from junior resident call schedules. In the subsequent year, reforms were made to bring work hours to the 80-hour week 2 years before the official reforms in 2003.
Additional survey questions were aimed to identify training program pressures or features that may have influenced the respondent's decisions about childrearing during or after residency. Responses were in the form of a 5-point Likert scale. Analysis was completed in the form of mean with standard deviation. Mean responses were calculated by assigning a numeric value to each response (1 = strong negative, 2 = negative, 3 = no effect, 4 = positive, 5 = strong positive). We did not collect data on respondents' marital status. Internal Review Board approval was obtained before the study began.
Results
Demographics
A total of 167 surgeons were contacted: 116 alumni and 51 current trainees (130 men and 37 women). There were 84 respondents for a survey response rate of 50% (51 men and 33 women). Respondents were separated into early (those who entered training between 1976 and 1999) and late cohorts (those who entered training between 2000 and 2009) based on the year they began training. There were 44 respondents in the early cohort (29 men and 15 women) and 40 respondents in the late cohort (22 men and 18 women). The percentage of men with children during residency was similar for the early and late cohorts (34% [10 of 29] versus 41% [9 of 22], respectively). For female residents, there was a substantial increase in childbearing for the late cohort (7% [1 of 15] for the early cohort versus 33% [6 of 18] for the late cohort; Figure 1). Additional survey answers were grouped by respondents who had children during residency, those who had children after training, and those who do not have children.
FIGURE 1.
Percentage of Cohort Having Children During Residency (Men vs Women)
Childbearing During Training
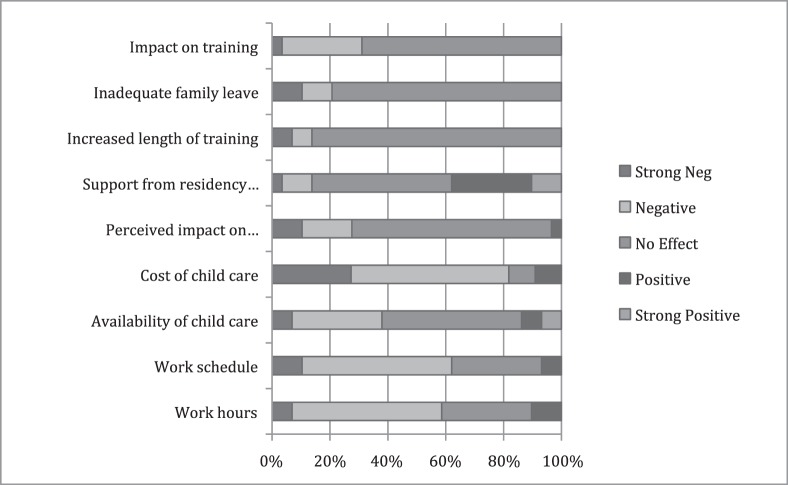
Respondents who had children during residency were asked if factors such as work hours, work schedule, availability of child care, cost of child care, impact on residency, support from the residency program, increased length of training, and adequate family leave affected their decision to have a child. For almost all of these potential considerations, most respondents answered “no effect” on their decision to have children during residency. However, 58% (15 of 26) of respondents reported that work hours had a negative effect on their decision (52% [13 of 26] negative; 8% [2 of 26] strong negative; mean Likert response = 2.44; SD = 0.78). Similarly, 65% (17 of 26) of respondents reported that work schedule had an adverse effect (54% [14 of 26] negative; 12% [3 of 26] strong negative; mean Likert response = 2.34; SD = 0.76) and 81% (21 of 26) of respondents reported that cost of child care had an adverse effect (54% [14 of 26] negative; 27% [7 of 26] strong negative; mean Likert response 2.0; SD = 0.89) on their decision to have children during residency (Figure 2).
FIGURE 2.
Likert Responses for Respondents Who Had Children During Residency
Participants responded to this question: “How did the following affect your decision to have children during residency?”
Other responses that affected the decision to have children during residency were as follows:
• I was much older as a resident and could not put off having children for very long; had my first son during my chief residency year (female respondent)
• [Having children] severely affected sleep off hours, days
• My spouse was able to stay home; military salary allowed me to have financial stability
• Family/spouse support—strong positive
Childbearing After Training
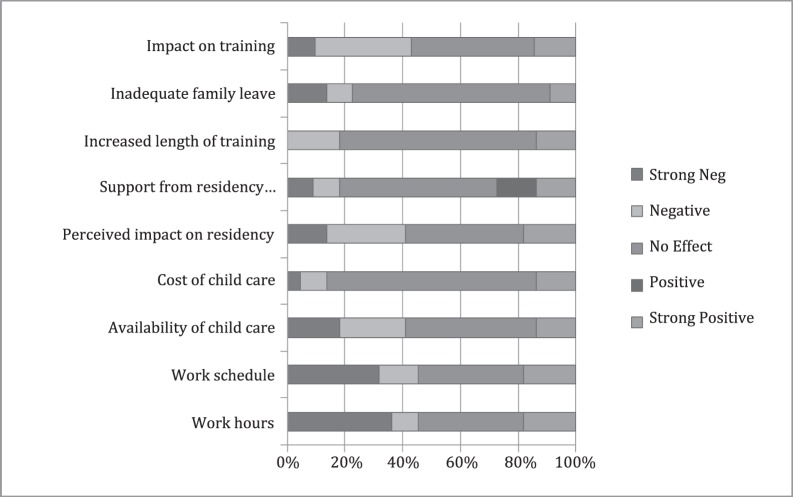
Respondents who had children after residency were similarly queried as to whether these considerations affected their decision to defer childbearing. Most responses indicated that these considerations had no effect on their decision not to have children during training. Although 45% (13 of 29) of respondents said length of work hours was a strong negative in the timing of childbearing, an equal percentage of respondents stated that work hours had no effect on this decision (mean Likert response = 2.55, SD = 1.47). The most commonly reported reason for not having children during residency was lack of a partner (Figure 3).
FIGURE 3.
Likert Responses for Respondents Who Had Children After Residency
Participants responded to this question: “If you did NOT have children during residency, how did the following affect your decision?”
Other responses that affected decision not to have children during residency (in cohort that ultimately had children after residency) were as follows:
• Did not really even think about children; not married at the time
• Not married
• I was single during residency
• No spouse
• Was not married
• Not married
• A professor and a resident having a baby together? Biggest [reason] was probably lack of flexibility
No Children
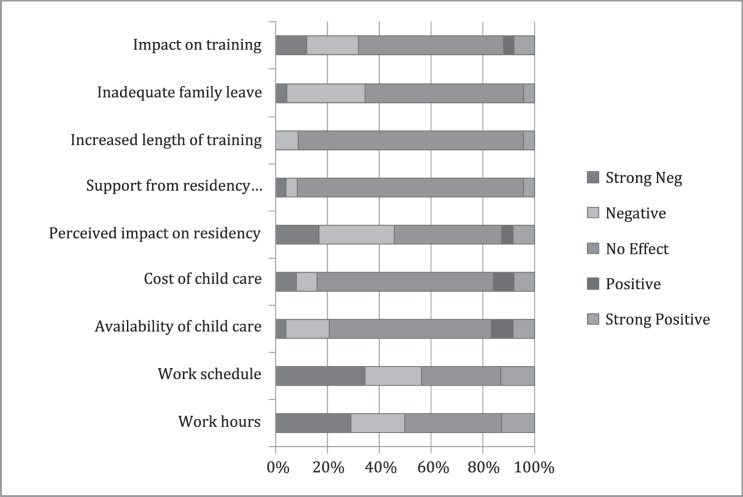
For respondents who did not have children, the considerations examined appeared to have no effect on this decision (Figure 4).
FIGURE 4.
Likert Responses for Respondents Who Did Not Have Children
Participants responded to this question: “If you did NOT have children during or after residency, how did the following affect your decision?”
Other responses that affected decision not to have children during residency (in cohort that never had children) were as follows:
• Residency training didn't impact decision—made decision not to have children prior to entering residency
• I'm not married
• It was the choice of the career itself and not the residency that affected my decision not to have children. Had we decided to have them, I would have done it during residency, however.
• Wasn't married until after residency so never an issue
• Unmarried
Discussion
We attempted to examine the effects of duty hour limits on the timing of childbearing. The overwhelming majority of respondents stated that duty hours had no effect on deciding when to have children. These findings are contrary to the popular belief that a reduction in duty hours is a factor in the prominent increase in childbearing for female surgeons during residency over the past 10 years. Although the reasons for this shift to earlier childbearing in female surgery residents cannot be clearly identified from our survey, several effects of increased childbearing during training on residents and training programs should be considered.
One effect of the increased rate of childbearing during residency years is the scheduling strain that this may place on a training program. Lashbrook and colleagues3 described this situation for obstetrics-gynecology programs, including pregnancy-related accommodations and support provided during training. Their findings showed that 65% of female resident respondents took leave during residency (1994–2002), and the longest leave lasted approximately 15 weeks. Although the impact will be different for each program, it brings to the forefront several issues that program leaders should consider. First, accommodations for leave may be necessary not only after delivery but also during the pregnancy. Second, all residents are entitled to family leave around the birth (or adoption) of a child. The Family and Medical Leave Act states that a person is entitled to 12 weeks of unpaid leave.4 As residents may have varying desire for time off around the birth of a child, the impact on a program may be more or less, depending on what trainees choose. Third, a prolonged break in training may prevent a resident from completing board requirements on schedule and may necessitate an additional year to fulfill these obligations. The American Board of Surgery currently requires a person to have 48 weeks of training per year to be allowed to take the written board examination, but it does allow for 4–6 weeks in 1 year for family leave.5 Accommodating residents may be more difficult in a smaller program where changes in personnel will be more pronounced, but all cases will require program flexibility.6
Our study has several limitations. We did not query for the marital status of respondents as part of the factors contributing to the decision to have children or as demographic information thus and cannot make inferences about how marital status may have influenced the results. However, many respondents cited lack of a partner as a reason they did not have children. Additionally, the survey tool was developed at our institution and was not adapted or based on previously published or validated survey tools. Because the validity of the instrument was not established, the resulting data could be subject to bias.
Despite the increase in childbearing in female residents in the late cohort, the specific reasons for this increase remain unclear. Although respondents who had children during residency reported some negative effects from work hours, work schedule, and cost of child care, they still proceeded with childbearing. In addition, the frequency of negative responses (eg, for work hours and schedule) occurred with similar frequency in both the early and late cohorts, and other considerations that were queried on the survey were considered to have no effect. Explanations other than those discussed here may exist. It is possible that the late cohort places greater emphasis on family development and is accepting of the associated additional work pressures or modifications required; however, these issues were not examined with this survey.7 Future studies should examine this and other potential reasons. Perhaps more specific questions addressing cultural changes and role models in surgical residency would elucidate these factors.
Conclusion
Childbearing for women during surgical residency has increased over time in the single program studied, and schedules, work hours, and program support were not cited as factors female residents considered in their decision to have children. This may represent a national trend. Surgical training programs need to develop clear, fair, and flexible policies to accommodate the multiple effects that childbearing may have on a training program.
Footnotes
All authors are in the Department of Surgery, University of California-Davis. Caitlin Smith, MD, is General Surgery Resident; Joseph M. Galante, MD, is Assistant Professor; Jonathan L. Pierce, MD, is Associate Professor; and Lynette A. Scherer, MD, is Professor, Division of Trauma and Critical Care.
Funding: The authors report no external funding source for this study.
References
- 1.FREIDA Online specialty training search, Surgery–General. https://freida.ama-assn.org/Freida/user/specStatisticsSearch.do?method=viewDetail&spcCd=440&pageNumber=2. Accessed July 31, 2013. [Google Scholar]
- 2.Jones AM, Jones KB. The 88-hour family: effects of the 80-hour work week on marriage and childbirth in a surgical residency. Iowa Orthop J. 2007;27:128–133. [PMC free article] [PubMed] [Google Scholar]
- 3.Lashbrook DL, Frazier LM, Horbelt DV, Stembridge TW, Rall MJ. Pregnancy during obstetrics and gynecology residency: effect on surgical experience. Am J Obstet Gynecol. 2003;189(3):662–665. doi: 10.1067/s0002-9378(03)00877-9. [DOI] [PubMed] [Google Scholar]
- 4.United States Department of Labor. Wage and Hour Division: Family and Medical Leave Act. http://www.dol.gov/whd/fmla/index.htm. Accessed July 31, 2013. [Google Scholar]
- 5.American Board of Surgery. Family leave requirements. In: Booklet of Information: Surgery 2012–2013:13. http://www.absurgery.org/xfer/BookletofInfo-Surgery.pdf. Accessed July 31, 2013. [Google Scholar]
- 6.Finch SJ. Pregnancy during residency: a literature review. Acad Med. 2003;78(4):418–428. doi: 10.1097/00001888-200304000-00021. [DOI] [PubMed] [Google Scholar]
- 7.Mobilos S, Chan M, Brown JB. Women in medicine: the challenge of finding balance. Can Fam Physician. 2008;54(9):1285–1286. [PMC free article] [PubMed] [Google Scholar]