Abstract
Background
Compliance with the Accreditation Council for Graduate Medical Education duty hour standards may necessitate more frequent transitions of patient responsibility.
Intervention
We created a multidisciplinary Patient Safety and Quality Council with a Task Force on Handoffs (TFH), engaging residents at a large, university-based institution.
Methods
The TFH identified core content of effective handoffs and patterned institutional content on the SIGNOUTT mnemonic. A web-based module highlighting core content was developed for institutional orientation of all trainees beginning summer 2011 to standardize handoff education. The TFH distributed handoff material and catalogued additional program initiatives in teaching and evaluating handoffs. A standard handoff evaluation tool, assessing content, culture, and communication, was developed and “preloaded” into the institution-wide electronic evaluation system to standardize evaluation. The TFH developed questions pertaining to handoffs for an annual institutional survey in 2011 and 2012. Acceptability of efforts was measured by program participation, and feasibility was measured by estimating time and financial costs.
Results
Programs found the TFH's efforts to improve handoffs acceptable; to date, 13 program-specific teaching initiatives have been implemented, and the evaluation tool is being used by 5 programs. Time requirements for TFH participants average 2 to 3 h/mo, and financial costs are minimal. More residents reported having education on handoffs (58% [388 of 668] versus 42% [263 of 625], P < .001) and receiving adequate signouts (69% [469 of 680] versus 61% [384 of 625], P = .004) in the 2012 survey, compared with 2011.
Conclusions
Use of a multispecialty resident leadership group to address content, education, and evaluation of handoffs was feasible and acceptable to most programs at a large, university-based institution.
What was known
Compliance with the Accreditation Council for Graduate Medical Education's duty hour standards may necessitate more frequent transitions of patient responsibility.
What is new
A multidisciplinary Patient Safety and Quality Council with a Task Force on Handoffs, engaging residents at a large, university-based institution.
Limitations
The tool to evaluate resident handoffs was not validated; self-reporting bias may overestimate quality of handoffs.
Bottom line
Use of a multispecialty resident leadership group to address content, education, and evaluation of handoffs was feasible and acceptable to most programs at a large, university-based institution.
Editor's Note: The online version of this article contains the handoff evaluation tool developed in this study as used by the Department of Medicine (paper version (124KB, docx) ) and as adapted by the Department of Pediatrics (web version (100.4KB, docx) ; Page 1 of 2); and 4 handoff-related questions (24KB, doc) that were incorporated into the Duke Graduate Medical Education Designated Institutional Official Housestaff Survey.
Introduction
In July 2011, changes to the Accreditation Council for Graduate Medical Education (ACGME) Common Program Requirements, which included new duty hour standards, resulted in more handoffs at many institutions. Increased handoff frequency can increase errors if information is inaccurate or fails to predict likely patient events.1–5 As a result, transitions of care are increasingly the focus of studies on patient safety and quality initiatives.4,6,7
In the past, handoffs education was rarely standardized.8–10 Studies have shown that a single session on handoffs, emphasizing content, improves self-perception of handoff quality.8,11 In another study, improvements lasted 2 months after educational sessions.12 The optimal timing or strategy for such education is unknown; however, coordinating sessions across an institution may be difficult.
Similarly, the best process for evaluating handoffs remains unclear, although studies reported improved quality perception with attending supervision.13,14 As institutions strive to meet ACGME requirements, institutional examples may provide insight on improving handoff quality. The purpose of our project was to determine whether a multispecialty, resident-led task force could drive standardization of handoff content, improve education on handoffs, and develop evaluation tools acceptable to most individual training programs.
Methods
Setting and Participants
Duke University Hospital (DUH; Durham, NC) sponsors 79 ACGME programs and 60 internal programs that involve approximately 1000 residents. In 2010, a multispecialty group of DUH residents organized an institutional Graduate Medical Education (GME) Patient Safety and Quality Council, incorporated under the institution's GME Committee for Peer Review Protection. The group meets monthly and has faculty participation (Health System Patient Safety Officer, Chief Medical Officer, and Associate Director of GME). Early on, the Council emphasized handoffs as a major focus, creating a Task Force on Handoffs (TFH), composed of residents from 13 DUH departments, to facilitate meeting ACGME requirements and improving handoff quality, as described previously.15
Interventions
Standardizing Handoff Content
The TFH convened during academic year 2010–2011 in preparation for July 2011, when new requirements took effect. The TFH's first goal was to standardize handoff content throughout DUH, as suggested by multiple authors and organizations.9,11,16,17 To standardize handoff content, the TFH identified a review of published mnemonics.18 After considering multiple mnemonics and principles recommended by the Society for Hospital Medicine, the TFH agreed on a set of content based on the SIGNOUTT mnemonic (Sick/not sick, Identifying information, General hospital course, New events of the day, Overall trajectory, Upcoming events, Tasks for overnight, Time for questions) because that mnemonic provided a baseline for inpatient services and flexibility for implementation across departments.8,17
The TFH emphasized the following critical content in an effective handoff: (1) patient demographics; (2) concise medical history and current problems/issues; (3) pending laboratory results, radiography results, and other results; (4) anticipatory guidance; (5) plan or to-do list; and (6) time for questions. Handoffs were encouraged to be performed face to face to create protected environments.10 Departments could add content, such as requiring a code status in medicine or the Foley catheter status in urology. Additionally, programs maintained unique, electronic handoff lists with that information available to oncoming providers.
Identifying Unique Handoffs
Many programs identified “primary” transitions of care. Programs with ward teams focused on inpatient care, whereas those without inpatients identified transitions in care relevant to their practice of medicine.
Resident Education
The TFH identified resident education on handoffs as integral for patient safety. A 22-slide, 20-minute, online module on handoffs was created by the TFH as a required component of Duke's annual Housestaff Orientation. In the module, a video created by Arora et al19 illustrates the pitfalls of poor handoffs. Thereafter, narrated slides identify Duke's standardized handoffs content and the need for defined times and locations for handoffs. Two questions on core content were included in the orientation questions, which all incoming residents must answer with 100% accuracy. The module was revised in 2012 to illustrate evaluation tools and amended in 2013 to show patient lists. The module is available to programs for use in additional educational sessions or for retesting resident knowledge.
To spread awareness, a TFH member made a presentation during a semiannual workshop for program directors, and a video of that presentation was uploaded to the GME office's educational website. The TFH initiated additional program-specific education on handoffs in conversations with program representatives. Many departments identified specialty-specific challenges, leading to the creation of educational sessions that were often timed to coincide with the orientation of new residents. Additionally, many programs wished to provide information regarding handoffs (eg, core content) within printed resident resource materials.
Development of an Evaluation Tool
Residents in the Department of Medicine developed a third-party, “observer” evaluation tool for shift handoffs (provided as online supplemental material) as a quality improvement project. That tool was based on standardized content and contained features important to medicine services (Do Not Attempt Resuscitation status, for example) based on a 4-point competency scale. Components evaluated by the tool included core content, the process of the verbal transition, and the culture or setting of the handoff. An observer of the handoff completed the evaluation tool, which was entered into the institutional electronic evaluation system for facile tracking and electronic documentation. The tool was piloted in the internal medicine services in 2010 and was informally noted by residents to allow constructive feedback. The TFH adapted that evaluation tool and “preloaded” it into the DUH online evaluation system (provided as online supplemental material), so all programs could use or amend the inherent questions for their needs. Attending physicians, program directors, chief residents, and senior residents have used this tool to evaluate interns and junior residents and to provide directed feedback. Those evaluations are typically uploaded into a resident's file for future review and for documentation to meet ACGME requirements. Some programs, such as pediatrics, added or omitted questions within the online evaluation system (provided as online supplemental material).
Institutional Evaluation
The winter survey of the DUH GME designated institutional official was amended in 2011 and 2012 to include 4 questions about handoffs (provided as online supplemental material). Those questions were developed by the TFH and were not piloted or validated before inclusion in the institutional survey.
Outcomes
Outcomes of this work included (1) the acceptability of the TFH efforts at the individual and program levels; (2) the feasibility, as measured in time and financial costs; and (3) the results from an institutional survey. For acceptability, the numbers of incoming trainees who successfully completed the orientation's education module and who answered questions within the institutional survey were compiled. The number of programs providing additional handoff education or using the evaluation tool was measured as well.
To document feasibility, resident and faculty time for participation in the TFH and the associated information technology and GME staff time for module development or dissemination were estimated. Further time estimates were made for program educational sessions. Costs for participation and tools were also estimated.
The results of the questions about handoffs on an annual institutional survey were calculated for 2011 and 2012 to measure resident awareness of educational efforts, to determine self-reported prevalence of receiving poor handoffs, and to rate personal confidence in providing adequate handoffs.
The questions for the institutional survey were reviewed and exempted by the Duke University School of Medicine Institutional Review Board.
Analysis
The data from the annual institutional survey were analyzed using χ2 statistics in Stata version 9.2 (StataCorp LP, College Station, TX). All postshift survey results were calculated as simple proportions.
Results
Acceptability
All incoming DUH residents, beginning in July 2011 (n = 310) and 2012 (n = 312), underwent training on handoffs using the module and passed the required posttest. Institution-wide, 679 of 958 residents (71%) responded to the institutional survey in 2012, compared with 625 of 954 residents (66%) in 2011. Residents rated the module favorably (3.98 on a 5-point scale).
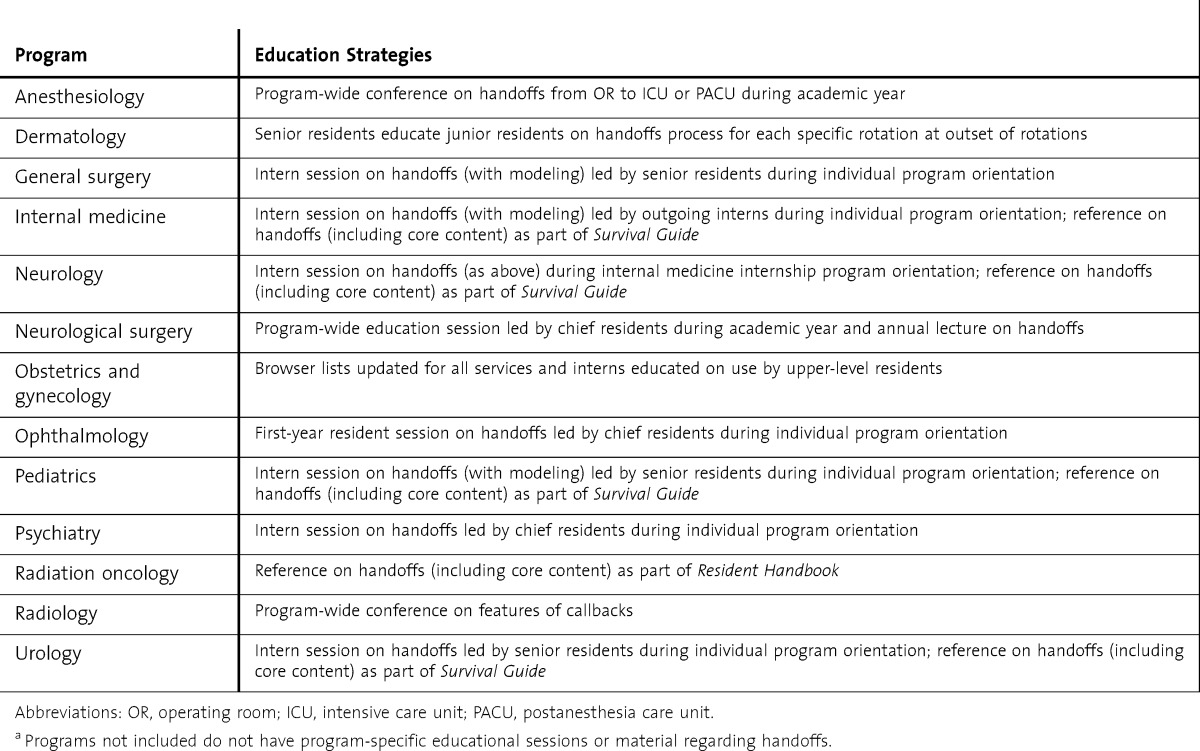
Thirteen programs currently provide additional education on handoffs to their residents as outlined in Table 1. Some sessions, such as the internal medicine orientation, predated the TFH. Examples of specific education approaches include dedicated lectures or conferences, invited GME speakers, and resident-led modeling of handoffs for incoming residents. This latter approach was favored during program-specific orientations to provide practical experience. Radiation oncology, alternatively, provided written information.
TABLE 1.
Education Practices Regarding Transitions of Care, by Programa
Programs also responded on their evaluation practices. Fewer programs adopted the evaluation tools; however, 7 programs evaluated most of their residents by May 2012, with 5 programs (71%) using the tool.
Feasibility
Time involvement for members of the Patient Safety and Quality Council began at 1 h/mo. Members of the Executive Committee met for an additional hour with the main faculty for the project. Additional time required for projects or separate TFH meetings was estimated at 1 to 3 h/mo. One team member kept and distributed minutes for the meetings and forwarded samples of project materials, requiring 3 h/mo. Additional time was required for creation of the orientation module, which was approximately 6 hours of combined resident and information technology support time initially and required 2 hours annually to update. Analysis of the institutional survey was done by GME staff and was supported by GME information technology resources. Programs typically allowed approximately 1 hour for additional training conferences or sessions, with members of the TFH leading sessions. Costs for the committee included 2 presentations at national meetings and were supported directly by the GME department. Faculty members were not compensated financially for the time they devoted to the TFH.
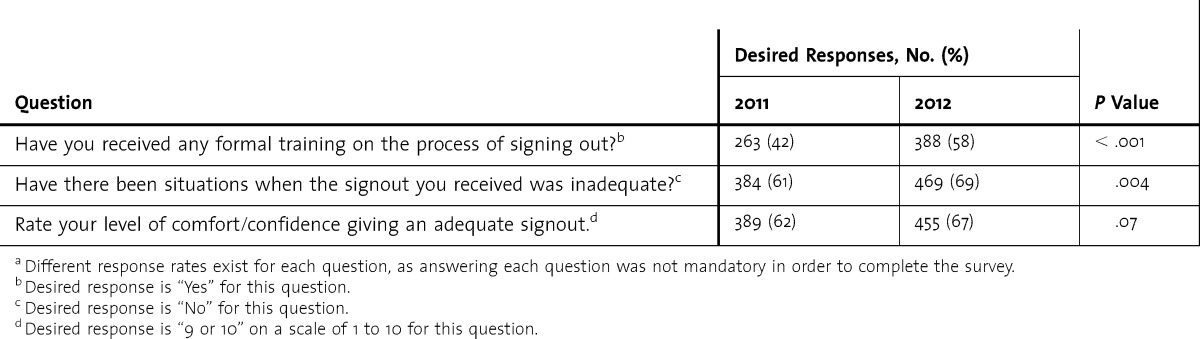
Institutional Survey
Results of the institutional survey are summarized in Table 2 and show increased awareness of handoff education and reception of adequate handoffs.
TABLE 2.
Designated Institutional Official Survey Results for Handoff Questions, 2011 and 2012a
DISCUSSION
At our large, university-based institution, residents led the effort to improve handoffs. Significant findings from this experience were that residents recognized the importance of safe handoffs and were eager to improve them; that programs were willing to accept resident input on this topic and to adopt educational practices to improve resident perception of the quality of handoffs; that programs without traditional inpatient services identified and educated residents on transitions within and across their disciplines; and that tools could be developed for evaluating handoffs, and those tools could be shared among departments with minimal changes. Additionally, those changes could be performed at minimal financial cost.
Most important, GME efforts were structured to give residents across multiple specialties leadership in handoffs. Similar to the approach described by Horwitz et al,20 a committee composed of individuals from different programs directed work on handoff education. Unlike the approach of Horwitz et al,20 residents took the main role in discussing and advancing improvement at DUH. In our experience, standardizing core content across the institution (as Horwitz et al20 did) and developing an orientation module and posttest highlighting that content aimed at giving all first-year, second-year, and future residents a baseline level of competence.8,20 After implementation of the module and increasing program-specific sessions, residents who have taken the designated institutional official survey increasingly identified handoff educational opportunities, and fewer residents reported having received inadequate signouts. We will analyze the results of our institutional survey annually to see whether that trend continues as a higher proportion of residents receive education on handoff procedures.
A second point, as discussed in the literature, is that a flexible approach is required, so the various GME programs accept changes in handoff requirements or standardization.21,22 Providing flexibility encourages maximal resident and program adherence and frees programs from obligations to create novel handoff strategies and tools. After starting with a basic framework of content and institution-wide education, programs can add individual education sessions or materials specific to their field when desired. At DUH, 13 programs currently are providing additional education.
An important part in increasing the acceptance of the program at DUH was identifying unique transitions of care in clinical departments without inpatient services. Although a significant amount of literature exists regarding handoffs in specialties with a large component of inpatient care, little information is available in others, such as radiology or radiation oncology. In our effort, emergency medicine identified communication between residents and inpatient admitting teams as a target for teaching and evaluating handoffs. Radiology focused its efforts on notification of abnormal findings to appropriate providers and developed a structured communication format. Dermatology targeted direct communication of findings with the ordering staff via electronic means. Radiation oncology, in which residents work with attending physicians for several months, focused on handoffs of service patients to oncoming residents at the end of rotations.
Defining handoffs in these fields is vital for meeting ACGME requirements and will hopefully improve care. Educational efforts at other institutions should highlight similar unique handoff situations.
Evaluation of handoffs at Duke is less robust than the educational effort, although 7 programs evaluated most of their residents for handoff competency, and most programs adopted the TFH evaluation tool. As programs work to continue to meet ACGME requirements, we will continue to offer access to this tool with the potential for modifications.
There are some limitations to our intervention. First, the tool to evaluate resident handoffs was not validated, and the residents or faculty evaluating the handoffs have not received formal training on evaluations and, therefore, may not provide consistent or optimal feedback. Second, as previously reported,5 residents overestimated the quality of the handoffs they provide. That was highlighted in our institutional survey, in which two-thirds of residents reported they gave signout information of quality 9 or 10 on a 10-point scale, yet one-third of residents had received inadequate signout during the past year.
There are several areas for future work. They include studies to improve handoff systems, such as automatically abstracting core content or information into written handoff materials to minimize errors related to omission. In addition, information gathered about handoffs must be distributed back to the programs in a constructive format. Finally, metrics for demonstrating improved patient care outcomes related to handoffs are difficult to identify or to attribute to changes in the handoff process.
Conclusion
Our intervention showed that residents can lead the standardization of handoffs across an institution, improve educational practices regarding handoffs, and take a formative role in the evaluation process. Implementing a similar approach at other institutions is feasible and has minimal costs. Time is a valuable commodity for both residents and faculty and is the most significant cost in this process; however, we were able to demonstrate the time commitment required for this intervention was feasible for participants during most months.
Footnotes
All authors are at the Duke University Health System. Joel C. Boggan, MD, MPH, is Chief Resident for Quality and Safety in Medicine at Durham VA Medical Center; Tian Zhang, MD, is a Fellow in Hematology-Oncology in the School of Medicine; Chris DeRienzo, MD, MPP, is a Fellow in Neonatal- Perinatal Medicine in the School of Medicine; Karen Frush, MD, is Professor of Pediatrics in the School of Medicine and Chief Patient Safety Officer in Patient Safety and Clinical Quality; and Kathryn Andolsek, MD, MPH, is Professor of Community and Family Medicine in the School of Medicine and Associate Director of Graduate Medical Education.
Funding: The authors report no external funding source for this study.
The authors wish to acknowledge the contributions of the Handoffs Task Force; this manuscript was made possible through the efforts of Drs Rebecca Sadun, Katherine Westreich, Abhay Singh, Michael Barfield, Kristi Rialon, Brian Griffith, Aimee Zaas, Aubrey Jolly-Graham, David Johnson, and John Weinerth and Ms Judy Milne.
References
- 1.Manjunath A, Srirangam SJ. Risks of working time directive: shorter shifts and more frequent handover. BMJ. 2010;341:c4858. doi: 10.1136/bmj.c4858. doi: 10.1136/bmj.c4858. [DOI] [PubMed] [Google Scholar]
- 2.Pezzolesi C, Schifano F, Pickles J, Randell W, Hussain Z, Muir H, et al. Clinical handover incident reporting in one UK general hospital. Int J Qual Health Care. 2010;22(5):396–401. doi: 10.1093/intqhc/mzq048. [DOI] [PubMed] [Google Scholar]
- 3.McSweeney ME, Lightdale JR, Vinci RJ, Moses J. Patient handoffs: pediatric resident experiences and lessons learned. Clin Pediatr (Phila) 2011;50(1):57–63. doi: 10.1177/0009922810379906. [DOI] [PubMed] [Google Scholar]
- 4.Scoglietti VC, Collier KT, Long EL, Bush GP, Chapman JR, Nakayama DK. After-hours complications: evaluation of the predictive accuracy of resident sign-out. Am Surg. 2010;76(7):682–686. [PubMed] [Google Scholar]
- 5.Chang VY, Arora VM, Lev-Ari S, D'Arcy M, Keysar B. Interns overestimate the effectiveness of their hand-off communication. Pediatrics. 2010;125(3):491–496. doi: 10.1542/peds.2009-0351. [DOI] [PubMed] [Google Scholar]
- 6.Ye K, Mc DTD, Knott JC, Dent A, MacBean CE. Handover in the emergency department: deficiencies and adverse effects. Emerg Med Australas. 2007;19(5):433–441. doi: 10.1111/j.1742-6723.2007.00984.x. [DOI] [PubMed] [Google Scholar]
- 7.Sabir N, Yentis SM, Holdcroft A. A national survey of obstetric anaesthetic handovers. Anaesthesia. 2006;61(4):376–380. doi: 10.1111/j.1365-2044.2006.04541.x. [DOI] [PubMed] [Google Scholar]
- 8.Horwitz LI, Moin T, Green ML. Development and implementation of an oral sign-out skills curriculum. J Gen Intern Med. 2007;22(10):1470–1474. doi: 10.1007/s11606-007-0331-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Solet DJ, Norvell JM, Rutan GH, Frankel RM. Lost in translation: challenges and opportunities in physician-to-physician communication during patient handoffs. Acad Med. 2005;80(12):1094–1099. doi: 10.1097/00001888-200512000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Raduma-Tomas MA, Flin R, Yule S, Williams D. Doctors' handovers in hospitals: a literature review. BMJ Qual Saf. 2011;20(2):128–133. doi: 10.1136/bmjqs.2009.034389. [DOI] [PubMed] [Google Scholar]
- 11.Arora V, Johnson J. A model for building a standardized hand-off protocol. Jt Comm J Qual Patient Saf. 2006;32(11):646–655. doi: 10.1016/s1553-7250(06)32084-3. [DOI] [PubMed] [Google Scholar]
- 12.Gakhar B, Spencer AL. Using direct observation, formal evaluation, and an interactive curriculum to improve the sign-out practices of internal medicine interns. Acad Med. 2010;85(7):1182–1188. doi: 10.1097/ACM.0b013e3181da8370. [DOI] [PubMed] [Google Scholar]
- 13.Chu ES, Reid M, Schulz T, Burden M, Mancini D, Ambardekar AV, et al. A structured handoff program for interns. Acad Med. 2009;84(3):347–352. doi: 10.1097/ACM.0b013e3181970829. [DOI] [PubMed] [Google Scholar]
- 14.Nabors C, Peterson SJ, Lee WN, Mumtaz A, Shah T, Sule S, et al. Experience with faculty supervision of an electronic resident sign-out system. Am J Med. 2010;123(4):376–381. doi: 10.1016/j.amjmed.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 15.DeRienzo CM, Frush K, Barfield ME, Gopwani PR, Griffith BC, Jiang X, et al. Handoffs in the era of duty hours reform: a focused review and strategy to address changes in the Accreditation Council for Graduate Medical Education Common Program Requirements. Acad Med. 2012;87(4):403–410. doi: 10.1097/ACM.0b013e318248e5c2. [DOI] [PubMed] [Google Scholar]
- 16.Vidyarthi AR, Arora V, Schnipper JL, Wall SD, Wachter RM. Managing discontinuity in academic medical centers: strategies for a safe and effective resident sign-out. J Hosp Med. 2006;1(4):257–266. doi: 10.1002/jhm.103. [DOI] [PubMed] [Google Scholar]
- 17.Arora VM, Manjarrez E, Dressler DD, Basaviah P, Halasyamani L, Kripalani S. Hospitalist handoffs: a systematic review and task force recommendations. J Hosp Med. 2009;4(7):433–440. doi: 10.1002/jhm.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Riesenberg LA, Leitzsch J, Little BW. Systematic review of handoff mnemonics literature. Am J Med Qual. 2009;24(3):196–204. doi: 10.1177/1062860609332512. [DOI] [PubMed] [Google Scholar]
- 19.Arora V, Farnan J, Paro J, Vidyarthi A, Johnson J. Teaching video—handoffs: a typical day on the wards. MedEdPORTAL; 2011. www.mededportal.org/publication/8331. Accessed March 9, 2012. [Google Scholar]
- 20.Horwitz LI, Schuster KM, Thung SF, Hersh DC, Fisher RL, Shah N, et al. An institution-wide handoff task force to standardise and improve physician handoffs. BMJ Qual Saf. 2012;21(10):863–871. doi: 10.1136/bmjqs-2011-000658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jorm CM, White S, Kaneen T. Clinical handover: critical communications. Med J Aust. 2009;190((suppl 11)):108–109. doi: 10.5694/j.1326-5377.2009.tb02613.x. [DOI] [PubMed] [Google Scholar]
- 22.Yee KC, Wong MC, Turner P. “HAND ME AN ISOBAR”: a pilot study of an evidence-based approach to improving shift-to-shift clinical handover. Med J Aust. 2009;190((suppl 11)):121–124. doi: 10.5694/j.1326-5377.2009.tb02617.x. [DOI] [PubMed] [Google Scholar]


