Abstract
Purpose
The purpose of the present study was to evaluate the anatomic features of the cervical spine using computed tomography (CT) to select safer screw insertion techniques, particularly emphasizing the location of the transverse foramen.
Methods
Fifty patients who underwent multiplanar CT reconstruction were evaluated. There were 34 males and 16 females with an average age of 67 years. The parameters included the following measurements: foramen width (the size of the transverse foramen FW), foramen height (the size of the transverse foramen FH), pedicle width (PW), foramen angle (FA the position of the transverse foramen), pedicle transverse angle (PTA) and lateral mass angle (LMA).
Results
The mean FW ranged from 6.2 to 6.3 mm (n.s). The mean FH ranged from 5.0 to 5.7 mm, with significant differences between each vertebra, except for the FH between C4 and C5 and the FH between C5 and C6. The mean PW ranged from 5.4 to 6.1 mm. There were significant differences between each vertebra, except for the PW between C3 and C4 and the PW between C3 and C5. The mean FA ranged from 18.8° to 20.5°. There were significant differences between each vertebra, except for the FA between C3 and C6 and the FA between C4 and C5. The mean PTA ranged from 37.1° to 45.4°. There were significant differences between each vertebra, except for the PTA between C3 and C5. The mean LMA ranged from 1.0° to 5.3°. There were significant differences between each vertebra, except for the LMA between C4 and C5. The FW and FH exhibited no correlations with PW, PTA or LMA. FA was found to be positively correlated with both PTA and LMA. There was also a positive correlation between PTA and LMA.
Conclusions
We suggest that in cases in which pedicle screw insertion is difficult, lateral mass screws (LMS) can be inserted safely and longer sizes can be selected. In contrast, in cases in which LMS insertion is difficult, the insertion of pedicle screws can be performed relatively easy.
Keywords: Cervical spine, Lateral mass screw, Pedicle screw
Introduction
Posterior stabilization of the lower cervical spine is most frequently performed using lateral mass screws (LMS) [1–4] and transpedicular screw fixation (CPS) [5–7]. These procedures do not require the lamina to be used for stabilization and are useful in patients undergoing one-stage posterior decompression and stabilization of the cervical spine. However, spinal nerve roots and vertebral arteries lie in close proximity to the lateral masses and are at risk of injury during screw insertion. In particular, vertebral artery injury is a deadly complication. Many authors have reported several potential risks of vertebral artery injury, although with a difference in frequency between pedicle screws and LMS. Abumi et al. [5] reported performing cervical CPS of the middle and lower cervical spine column in patients with traumatic disorders and fractures, describing the technique in 1994 as a preliminary report. Abumi et al. [8] also reported that 45 of 669 (6.7 %) cervical pedicle screws were found on computed tomography (CT) scans have penetrated the pedicle. Cho et al. [9] reported the case of a patient whose vertebral artery injury and brain stem infarction were caused by poor surgical technique of lateral mass plating in the cervical spine. Moreover, Pal et al. [10] noted that an accurate visual estimation of the trajectory angle for LMS is difficult and therefore cannot be consistently achieved. Many cadaveric and radiographic studies of CPS or LMS dimensions such as pedicle diameter, pedicle transverse angle (PTA) and lateral mass length have been reported to improve the safety of screw insertion and avoid injury of the vertebral arteries. However, previous studies evaluated the safety of pedicle or lateral mass screw insertion individually. The purpose of the present study was to evaluate the anatomic features of the cervical spine using CT to select safer screw insertion techniques, particularly emphasizing the location of the transverse foramen.
Materials and methods
Fifty patients who underwent multiplanar CT reconstruction were evaluated. There were 34 males and 16 females with an average age of 67 years. The underlying disorders included 38 patients with cervical spondylotic myelopathy, 2 patients with disc herniation, 5 patients with ossification of the posterior longitudinal ligament (OPLL) and 5 patients with cervical spondylotic amyotrophy. None of the patients exhibited any evidence of infection, neoplasms, traumatic diseases or congenital spinal malformations.
All patients were scanned using axial CT parallel to the upper endplate of the vertebral body (C3–C6) with a helical CT scanner. An algorithm that provided the most detail, a slice thickness of 1 mm and a slice spacing of 1 mm were used. We evaluated the dimensions of the pedicles from C3 to C6. CT images in which each pedicle appeared the largest were selected, and the following dimensions were determined. All parameters were measured three times by the first author (M. N), and the mean was used as the final value.
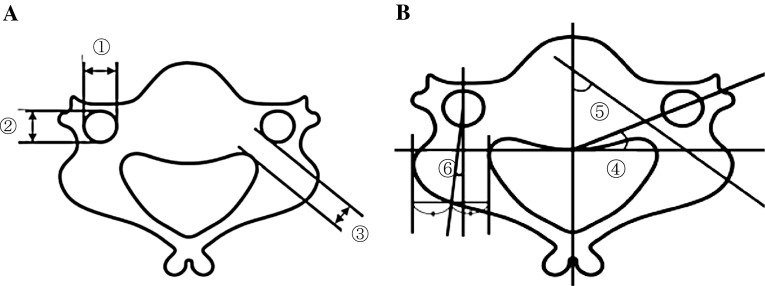
The parameters included the following measurements (Fig. 1a, b).
Foramen width (the size of the transverse foramen FW).
Foramen height (the size of the transverse foramen FH).
Pedicle width (PW).
Foramen angle (FA the position of the transverse foramen).
Pedicle transverse angle (PTA).
Lateral mass angle (LMA).
Fig. 1.
Foramen width (FW). Foramen height (FH). Pedicle width (PW). Foramen angle (FA). Pedicle transverse angle (PTA). Lateral mass angle (LMA)
Moreover, we evaluated the following correlations.
The correlation between the size of the transverse foramen (both FW and FH) and the PW, PTA and LMA.
The correlations between the position of the transverse foramen (FA) and the PW, PTA and LMA.
The correlation between PTA and LMA.
A statistical analysis of all results was performed, and the range values, mean value and standard deviation of each parameter were calculated. Furthermore, the correlations among the linear parameters were calculated using univariate linear regression analyses and expressed as Pearson correlation coefficients. Significant differences were considered to exist at P values of <0.05.
Results
The results of various parameters from C3 to C6 are shown in Table 1. There were no significant differences between the left and right sides for the same vertebra in each subject.
Table 1.
Dimensions of cervical pedicles obtained with CT
| FW (mm) | FH (mm) | PW (mm) | FA (°) | PTA (°) | LMA (°) | |
|---|---|---|---|---|---|---|
| C3 | ||||||
| Mean | 6.2 ± 0.8 | 5.0 ± 0.5 | 5.4 ± 0.8 | 18.8 ± 2.9 | 41.8 ± 0.8 | 3.1 ± 3.0 |
| Female | 6.1 ± 0.8 | 5.0 ± 0.6 | 5.0 ± 0.8 | 17.9 ± 3.0 | 39.8 ± 5.8 | 2.8 ± 3.0 |
| Male | 6.2 ± 0.7 | 5.0 ± 0.5 | 5.6 ± 0.7 | 19.3 ± 2.7 | 42.2 ± 4.8 | 3.3 ± 3.1 |
| C4 | ||||||
| Mean | 6.3 ± 0.9 | 5.4 ± 0.7 | 5.4 ± 0.7 | 20.3 ± 3.3 | 45.4 ± 0.7 | 5.3 ± 3.5 |
| Female | 6.3 ± 0.8 | 5.4 ± 0.6 | 5.3 ± 0.6 | 18.9 ± 2.5 | 43.4 ± 5.0 | 4.4 ± 3.3 |
| Male | 6.4 ± 0.9 | 5.4 ± 0.7 | 5.6 ± 0.6 | 21.0 ± 3.6 | 46.3 ± 6.7 | 5.7 ± 3.5 |
| C5 | ||||||
| Mean | 6.3 ± 0.8 | 5.4 ± 0.7 | 5.7 ± 0.8 | 20.5 ± 3.2 | 42.8 ± 0.8 | 4.9 ± 3.6 |
| Female | 6.1 ± 0.7 | 5.3 ± 0.6 | 5.2 ± 0.7 | 19.6 ± 3.2 | 42.5 ± 5.7 | 4.7 ± 3.6 |
| Male | 6.3 ± 0.8 | 5.5 ± 0.7 | 5.9 ± 0.8 | 21.0 ± 5.5 | 42.9 ± 5.5 | 5.0 ± 3.7 |
| C6 | ||||||
| Mean | 6.3 ± 0.8 | 5.7 ± 1.0 | 6.1 ± 0.8 | 19.2 ± 2.8 | 37.1 ± 0.8 | 1.0 ± 2.4 |
| Female | 6.3 ± 0.8 | 5.7 ± 1.1 | 5.6 ± 0.6 | 18.5 ± 2.5 | 37.6 ± 3.6 | 0.2 ± 2.6 |
| Male | 6.4 ± 0.8 | 5.6 ± 1.0 | 6.4 ± 0.7 | 19.5 ± 2.9 | 37.1 ± 3.3 | 1.3 ± 2.2 |
The values are presented as the mean ± SD
The underlined values indicate significant sex differences, P < 0.01
Foramen width and foramen height (the size of the transverse foramen)
The mean FW ranged from 6.2 to 6.3 mm (Table 1). There were no significant differences among the vertebral levels (Table 2). The mean FH ranged from 5.0 to 5.7 mm (Table 1). The FH values gradually increased on the caudal side. There were significant differences between each vertebra, except for the FH between C4 and C5 and the FH between C5 and C6 (Table 2).
Table 2.
Differences in each parameter between each vertebra
| C3/C4 | C3/C5 | C3/C6 | C4/C5 | C4/C6 | C5/C6 | |
|---|---|---|---|---|---|---|
| FW | n.s | n.s | n.s | n.s | n.s | n.s |
| FH | <0.01 | <0.01 | <0.01 | n.s | <0.05 | n.s |
| PW | n.s | n.s | <0.01 | <0.05 | <0.01 | <0.01 |
| FA | <0.01 | <0.01 | n.s | n.s | <0.05 | <0.01 |
| PTA | <0.01 | n.s | <0.01 | <0.01 | <0.01 | <0.01 |
| LMA | <0.01 | <0.01 | <0.01 | n.s | <0.01 | <0.01 |
n.s not significant
Pedicle width
The mean PW ranged from 5.4 to 6.1 mm. There were significant intersex differences at all the levels (Table 1). The PW values gradually increased from C3 to C6. There were significant differences between each vertebra, except for the PW between C3 and C4 and the PW between C3 and C5 (Table 2).
Foramen angle (the position of the transverse foramen)
The mean FA ranged from 18.8° to 20.5°. There was a significant intersex difference at C4 (Table 1). There were significant differences between each vertebra, except for the FA between C3 and C6 and the FA between C4 and C5 (Table 2).
Pedicle transverse angle
The mean PTA ranged from 37.1° to 45.4° (Table 1). The smallest PTA was found at C6, and the largest PTA was found at C4. There were significant differences between each vertebra, except for the PTA between C3 and C5 (Table 2).
Lateral mass angle
The mean LMA ranged from 1.0° to 5.3° (Table 1). The smallest LMA was found at C6, and the largest LMA was found at C4. There were significant differences between each vertebra, except for the LMA between C4 and C5 (Table 2).
Correlations between parameters
FW and FH exhibited no correlations with PW, PTA or LMA. FA was positively correlated with PTA and LMA. There was also a positive correlation between PTA and LMA (Table 3).
Table 3.
Correlation coefficients between each parameter
| Correlation | Correlation coefficient | Coefficient determination |
|---|---|---|
| PW vs. FW | 0.03 | P = 0.50 |
| PW vs. FH | 0.10 | P = 0.07 |
| PW vs. FA | 0.07 | P = 0.14 |
| PTA vs. FW | 0.02 | P = 0.72 |
| PTA vs. FH | −0.05 | P = 0.25 |
| PTA vs. FA | 0.80 | P < 0.01 |
| LMA vs. FW | −0.01 | P = 0.89 |
| LMA vs. FH | −0.01 | P = 0.65 |
| LMA vs. FA | 0.43 | P < 0.01 |
| PTA vs. LMA | 0.59 | P < 0.01 |
Discussion
Vertebral artery injuries are caused by an inadequate placement and angle of screw insertion. Many authors have published details of regional surgical anatomy and applied the correct surgical techniques to prevent vertebral injury. Morphometric studies using cadavers [11–15] have been reported, which noted the quantitative three-dimensional anatomy of middle cervical regions with measurements of the vertebral bodies, spinal canal, pedicles, lateral masses and transverse foramen. With advances in imaging technology, multiplanar reconstructed CT scans now enable the desired morphology of the cervical spine to be analyzed in three dimensions. Karaikovic et al. [16] and Reinhold et al. [17] reported cervical pedicle morphology and angular measurements to determine the direction of pedicle screw insertion in both the transverse and sagittal planes using CT. Sakamoto et al. [18] also evaluated cervical pedicle morphology using CT and reported that the screw insertion angle should be as close as possible to 50° in the transverse plane and that the entry point of cervical transpedicular screws should be located as laterally as possible on the posterior surface of the lateral mass. The morphology of the transverse foramen in the subaxial cervical spine using CT has been previously reported. Liujun et al. [19] studied the location and size of the vertebral artery in relation to the transverse foramen in the lower cervical spine using CT angiography. They reported that the vertebral artery is located in the medial part of the transverse foramen and that there is a relative abundance space for the vertebral foramen within the transverse foramen. Steven et al. [20] reported the location of the transverse foramen in the subaxial spine to be able to recognize landmarks during anterior surgery. There are a few studies based on the relationship of the vertebral artery to its surrounding structures. Chazono et al. [21] evaluated the linear and angular parameters of the vertebral body required for cervical transpedicular screw insertion using multiplanar CT reconstruction. The farther the transverse foramen extended forward to the anterior region and medially to the lateral edge of the spinal canal, greater the PTA, suggesting that the risk of injury to the VA may be increased when inserting the CPS. In our study, the linear parameters exhibited significant intersex differences in PW at all the levels, similar to the findings of other Asian studies.
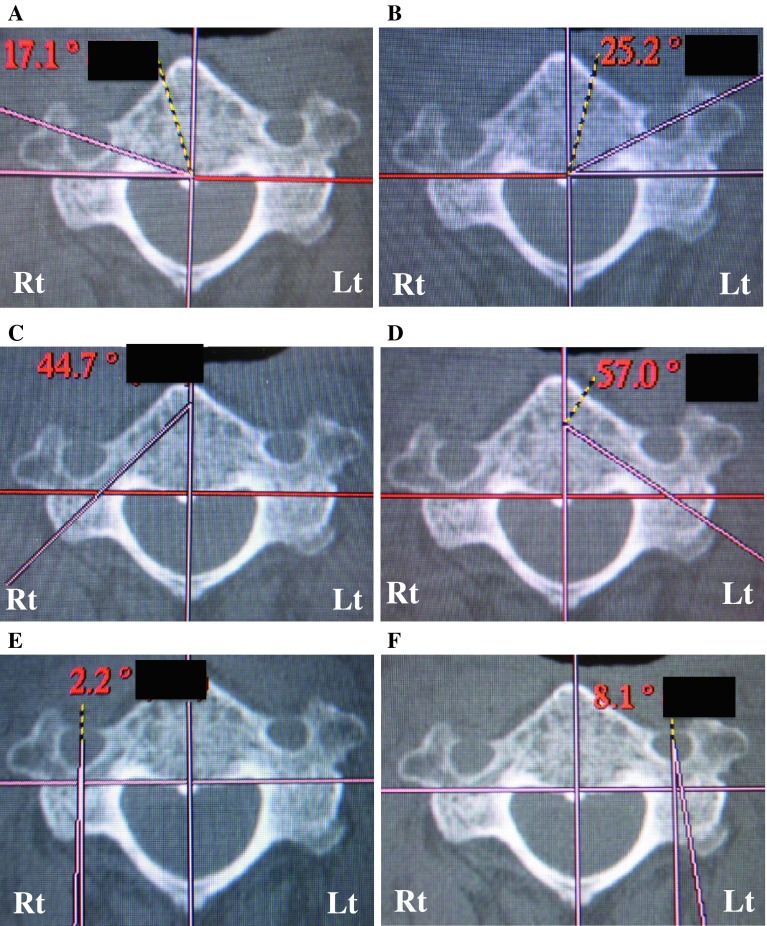
The only significant difference in the angular parameters was in FA at C4. FW and FH exhibited no correlations with PW, PTA or LMA. On the other hand, there were positive correlations between FA and both PTA and LMA. This means that the difficulty of screw insertion changes relatively with the location of the transverse foramen. When the transverse foramen is located more anteriorly and medially (the FA becomes larger), both PTA and LMA are larger. In such cases, insertion of pedicle screws is more difficult, and insertion of LMS should be used to avoid VA injury and bony violation. Furthermore, this allows for the selection of longer screws (Fig. 2b, d, f). In contrast, when the transverse foramen is located more posteriorly and laterally (the FA becomes smaller), both PTA and LMA are smaller. In such cases, insertion of transverse pedicle screws is relatively easy, while insertion of LMS is difficult (Fig. 2a, c, e). However, we should know that the appropriate cervical screw should be selected, length of the screw, and direction of the screw insertion must be determined based on cervical CT for each case.
Fig. 2.
This cervical spine demonstrated opposite characteristics in each transverse foramen. On the left side, FA, PTA and LMA are larger than those of the right side. Therefore, insertion of pedicle screws would be difficult, and lateral mass screws should be selected. Furthermore, longer sizes can be selected. In contrast, when the values of the right side are smaller than those of the left side, insertion of pedicle screws is easier. a FA (Rt). b FA (Lt). c PTA (Rt). d PTA (Lt). e LMA (Rt). f LMA (Lt)
In conclusion, we evaluated the anatomic features of the cervical spine using CT to select safer screw insertion techniques. We suggest that, in cases in which insertion of pedicle screws is difficult, LMS can be inserted safely. In contrast, in cases in which insertion of LMS is difficult, insertion of pedicle screws can be performed relatively easily.
Acknowledgments
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Conflict of interest
None.
References
- 1.Roy-Camille R, Saillant G, Lavile C, Mazel C (1989) Internal fixation of lower cervical spine by a posterior osteosynthesis with plates and screws. In: Lippicott JB (ed) The cervical Spine, 2nd edn. Cervical Spine Research Society, Philadelphia, pp 390–430
- 2.Jeanneret B, Magerl F, Ward EH, Ward J. Posterior stabilization of the cervical spine with hook plates. Spine. 1991;16(suppl):S56–S63. doi: 10.1097/00007632-199103001-00010. [DOI] [PubMed] [Google Scholar]
- 3.An HS, Gordin R, Renner K. Anatomic consideration for plate-screw fixation of the cervical spine. Spine. 1991;16(Suppl):S548–S551. doi: 10.1097/00007632-199110001-00019. [DOI] [PubMed] [Google Scholar]
- 4.Anderson PA, Henley MB, Grady MS, Montesano PX, Winn HR. Posterior cervical arthrodesis with AO reconstruction plate and bone graft. Spine. 1991;16(Suppl):S72–S79. doi: 10.1097/00007632-199103001-00012. [DOI] [PubMed] [Google Scholar]
- 5.Abumi K, Itoh H, Taneichi H, et al. Transpedicular screw fixation for traumatic lesions of the middle and lower cervical spine: description of the techniques and preliminary report. J Spinal Disord. 1994;7:19–28. doi: 10.1097/00002517-199407010-00003. [DOI] [PubMed] [Google Scholar]
- 6.Yukawa Y, Kato F, Ito K, et al. Placement and complications of cervical pedicle screws in 144 cervical trauma patients using pedicle axis view techniques by fluoroscope. Eur Spine J. 2009;18:1293–1299. doi: 10.1007/s00586-009-1032-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schaefer C, Begemann P, Fuhrhop I, et al. Percutaneous instrumentation of the cervical and cervico-thoracic spine using pedicle screws: preliminary clinical results and analysis of accuracy. Eur Spine J. 2011;20:977–985. doi: 10.1007/s00586-011-1775-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abumi K, Shono Y, Taneichi H, et al. Complications of pedicle screw fixation in reconstructive surgery of the cervical spine. Spine. 2000;25:962–969. doi: 10.1097/00007632-200004150-00011. [DOI] [PubMed] [Google Scholar]
- 9.Cho KH, Shin YS, Yoon SH, et al. Poor surgical technique in cervical plating leading to vertebral artery injury and brain stem infarction–case report. Surg Neurol. 2005;64:221–225. doi: 10.1016/j.surneu.2004.09.042. [DOI] [PubMed] [Google Scholar]
- 10.Pal D, Bayley E, Magaji SA, Boszczyk BM. Freehand determination of the trajectory angle for cervical lateral mass screws: how accurate is it? Eur Spine J. 2011;20:972–976. doi: 10.1007/s00586-011-1694-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cagnie B, Barbaix E, Vinck E, et al. Extrinsic risk factors for compromised blood flow in the vertebral artery: anatomical observations of the transverse foramina from C3 to C7. Surg Radiol Anat. 2005;27:312–316. doi: 10.1007/s00276-005-0006-7. [DOI] [PubMed] [Google Scholar]
- 12.Ebraheim NA, Xu R, Yeasting RA. The location of the vertebral artery foramen and its relation to posterior lateral mass screw fixation. Spine. 1996;21:1291–1295. doi: 10.1097/00007632-199606010-00002. [DOI] [PubMed] [Google Scholar]
- 13.Ebraheim NA, Xu R, Knight T, et al. Morphometric evaluation of lower pedicle and its projection. Spine. 1997;22:1–6. doi: 10.1097/00007632-199701010-00001. [DOI] [PubMed] [Google Scholar]
- 14.Jeanneret B, Gebhard JS, Magerl F. Transpedicular screw fixation of articular mass fracture separation: result of an anatomical study and operative technique. J Spinal Disord. 1994;7:222–229. doi: 10.1097/00002517-199407030-00004. [DOI] [PubMed] [Google Scholar]
- 15.Nishinome M, Iizuka H, Iizuka Y, Takagishi K. Anatomy of subaxial cervical foramens, the safety zone for lateral mass screwing. Eur Spine J. 2012;21:309–313. doi: 10.1007/s00586-011-1984-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karaikovic EE, Daubs MD, Madsen RW, et al. Morphologic characteristics of human cervical pedicles. Spine. 1997;22:493–500. doi: 10.1097/00007632-199703010-00005. [DOI] [PubMed] [Google Scholar]
- 17.Reinhold M, Magerl F, Rieger M, Blauth M. Cervical pedicle screw placement: feasibility and accuracy of two new insertion techniques based on morphometric data. Eur Spine J. 2007;16:47–56. doi: 10.1007/s00586-006-0104-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sakamoto T, Neo M, Nakamura T. Transpedicular screw placement evaluated by axial computed tomography of the cervical pedicle. Spine. 2004;29:2510–2515. doi: 10.1097/01.brs.0000144404.68486.85. [DOI] [PubMed] [Google Scholar]
- 19.Zhao L, Xu R, Hu T, et al. Quantitative evaluation of the location of the vertebral artery in relation to the transverse foramen in the lower cervical spine. Spine. 2008;33:373–378. doi: 10.1097/BRS.0b013e318163f349. [DOI] [PubMed] [Google Scholar]
- 20.Ludwig SC, Kramer DL, Balderston RA, et al. Placement of pedicle screws in the human cadaveric cervical spine: comparative accuracy of three techniques. Spine. 2000;25:1655–1667. doi: 10.1097/00007632-200007010-00009. [DOI] [PubMed] [Google Scholar]
- 21.Chazono M, Soshi S, Inoue T, et al. Anatomical considerations for cervical pedicle screw insertion: the use of multiplanar computerized tomography reconstruction measurements. J Neurosurg Spine. 2006;4:472–477. doi: 10.3171/spi.2006.4.6.472. [DOI] [PubMed] [Google Scholar]