Abstract
Purpose
We have evaluated the effect of bracing in scoliosis on coronal alignment in a cohort of patients. Current literature has not described the specific effect of bracing on the 3D shape of the scoliotic curves. The purpose of this study was to analyze the variability of the 3D effect of bracing on idiopathic scoliosis.
Materials and methods
The spines of 30 patients with adolescent idiopathic scoliosis were reconstructed using biplanar stereoradiography with and without the brace. The Cobb angle, sagittal and pelvic parameters and transverse plane parameters were calculated. The variability and the mean values of each parameter, with and without a brace, were analyzed and compared using a student t test.
Results
The Cobb angle improved in 50 % of patients but remained unchanged in 50 % cases. In 90 % of the cases lordosis was decreased. The thoracic kyphosis was decreased in 26 % cases, unchanged in 57 % of cases and increased in 17 % cases. The AVR was improved (>5°) in 26 % cases, worsened in 23 % and unchanged in 50 %. Only the differences of Cobb angle and the lordosis were statistically significant.
Conclusions
Global statistics of this study concur with the literature. The Cobb angle was significantly improved. It also showed a significant hypolordotic effect. However, the results showed a high variability of the brace treatment effect in almost every parameter. Analysis of this variability by means of 3D reconstructions instead of global statistics should help characterize the mechanisms of correction of brace treatment.
Keywords: Scoliosis, Brace, 3D, Variability, Stereoradiography
Introduction
Bracing is the main option in the treatment of scoliosis before skeletal maturity. Many different types of braces have been described in the past decades but principles of correction are very similar. Empirical evidence dictates that a pressure should be below the apex of the curve with opposite pressure near the junctions [1]. An area of relief needs to be preserved so that the trunk may shift. Besides these basics, in reality one must consider the curve topology and severity, the experience of the brace manufacturer and patient compliance.
The effect of bracing in idiopathic scoliosis has been evaluated in our series and essentially in the AP plane by means of global statistics [2–8]. However, the different curve topology and severity, different brace concepts and designs should not be analyzed together as this could lead to controversial conclusions. Compared with the natural history [9] and the prospective study data of Nachemson et al. [5], most braces are effective in preventing progression of adolescent idiopathic scoliosis for curves under 35 degrees. But there is a lack of knowledge of the effect of brace treatment on the sagittal alignment and more particularly on the 3D transverse plane parameters.
Recent development in 3D imaging using biplanar stereoradiography has allowed a novel 3D approach to scoliotic deformity in standing position. These methods of 3D reconstruction of the spine have been validated in asymptomatic and scoliotic patients [10–13]. The purpose of the current study was to analyze the variability of the effect of brace treatment on the 3D shape of idiopathic scoliosis.
Methods
Imaging protocol and 3D modeling
Thirty patients with adolescent idiopathic scoliosis undergoing brace treatment were asked to undergo a radiologic examination with and without a brace in our institution. 23 girls and 7 boys were included. The mean age at radiological examination was 11 [range 8–14]. 10 were classified Risser 0 or 1, 7 were Risser 2, 8 were Risser 3 and 5 were Risser 4. The mean Cobb angle was 28° (15°).
There were 20 thoracic (Apex between T1 and T11), 5 thoracolumbar (Apex between T12 and L1), and 5 lumbar (Apex between L2 and L5) curves.
Braces were Cheneau in 18 cases, Milwaukee in 5 cases, GTB in 3 cases, Lyonnais in 2 cases and Charleston in 2 cases. All patients had been treated for a minimum of 6 months.
The radiological examination was performed with the EOS System which is a tridimensional imaging modality recently developed and validated to improve 3D evaluation of the spine deformity [14]. This low dose imaging system provides simultaneous AP and lateral views in the standing position. Computerized reconstructions based on identifiable anatomic points provide a 3D image of the entire spine which offers a novel approach to the scoliotic deformity giving measurements of vertebral and intervertebral axial rotation [11]. The imaging protocol was approved by our national ethics committee (CCPPRB 6001).
At the day of the radiological examination, all patients were asked to come to our institution without brace. We asked for a minimum of 1 h without brace to perform the primary radiological examination. Each examination was performed in a free standing position. After the first examination the patient was told to put the brace on like usual. A second examination was subsequently performed along with the same instructions.
Both biplanar X-rays, with and without brace, were computed in Stereos software and 3D reconstruction of the spine were performed. 3D shape parameters were automatically computed in Stereos [11]. The parameters computed were as follows:
The Cobb angle.
The sagittal parameters: T1–T12 thoracic kyphosis angle, L1–S1 lumbar lordosis angle.
The pelvic parameters: pelvic incidence, sacral slope and pelvic tilt.
- Specific transverse plane parameters describing a 3D pattern of severe scoliosis [15] were as follows:
- Apical axial vertebral rotation (AVR).
- Intervertebral axial rotation at the lower neutral zone (lower IAR) as described by Perdriolle et al. [16].
- Torsion index: this index, proposed by Steib et al. [17], indicates to what extend vertebrae are continuously rotated one with regard to the other from lower neutral vertebra to the apex, then from the apex to the upper neutral vertebra. The torsion index is the mean of the two sum of intervertebral axial rotation from lower junction to the apex, then from the apex to the upper junction.
Fig. 1.
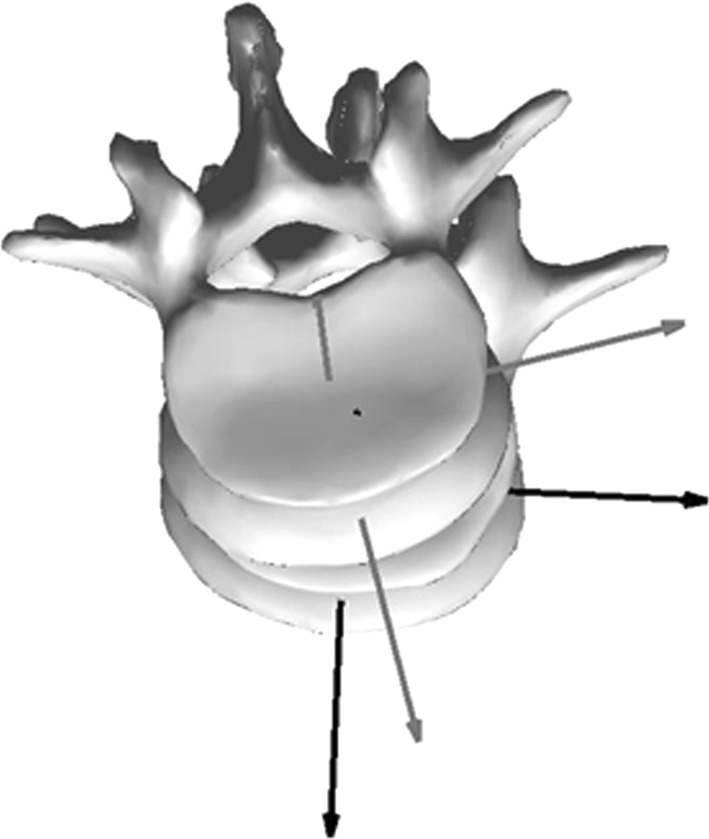
3D drawing showing the measurement of intervertebral axial rotation (IAR)
Analysis of the data
The values of all parameters described above were collected with and without brace for each patient. For each parameter and for each patient, the variations of the values were differentiated as: increase, when the value with the brace increased of more than 5°; unchanged, when the variation of the value with the brace was below 5°; and decreased, when the value with the brace decreased of more than 5°.
A statistical analysis was also performed in the SPSS version 12.0.1 for Windows (SPSS inc., Chicago, IL, USA). Mean values of each parameter were also compared with and without brace using a paired two-side Student t-test. Differences were considered as being statistically significant for p = 0.001.
Results
The variability of the values of each parameter with and without brace is recorded in Table 1.
Table 1.
The table presents the variation of each parameter with and without brace for each patient. The variations of the values were differentiated in: increase, when the value with the brace increased of more than 5°, unchanged, when the variation of the value with the brace was below 5° and decreased, when the value with the brace decreased of more than 5°
| Variation | Cobb angle | Sagittal parameter | Pelvic parameters | Transverse plane parameters | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kyphosis | Lordosis | Pelvic tilt | Incidence | Sacral slope | Torsion | Lower IAR | Upper IAR | AVR | ||||||||||||
| Increase | 0 | (0 %) | 6 | (20 %) | 17 | (57 %) | 1 | (3 %) | 4 | (13 %) | 0 | (0 %) | 2 | (7 %) | 7 | (23 %) | 8 | (27 %) | 7 | (23 %) |
| Unchanged | 15 | (50 %) | 14 | (47 %) | 11 | (37 %) | 20 | (67 %) | 18 | (60 %) | 17 | (57 %) | 22 | (73 %) | 18 | (60 %) | 16 | (53 %) | 15 | (50 %) |
| Decrease | 15 | (50 %) | 10 | (33 %) | 2 | (7 %) | 9 | (30 %) | 8 | (27 %) | 13 | (43 %) | 6 | (20 %) | 5 | (17 %) | 6 | (20 %) | 8 | (27 %) |
The Cobb angle decreased of more than 5° in 15 cases (50 %) and remained unchanged in 15 cases (50 %). Among the 15 cases that decreased, 11 cases (36 %) decreased more than 10°. The L1–L5 lordosis decreased in 17 cases (57 %), remained unchanged in 11 (37 %) cases and increased in 2 (7 %) cases. The AVR was decreased (max 14°) in 8 cases (26 %), remained unchanged in 15 cases (50 %) and increased in 7 cases (23 %). The pelvic incidence decreased in 14 cases (47 %), remained unchanged in 9 (30 %) cases and increased in 7 (23 %) cases.
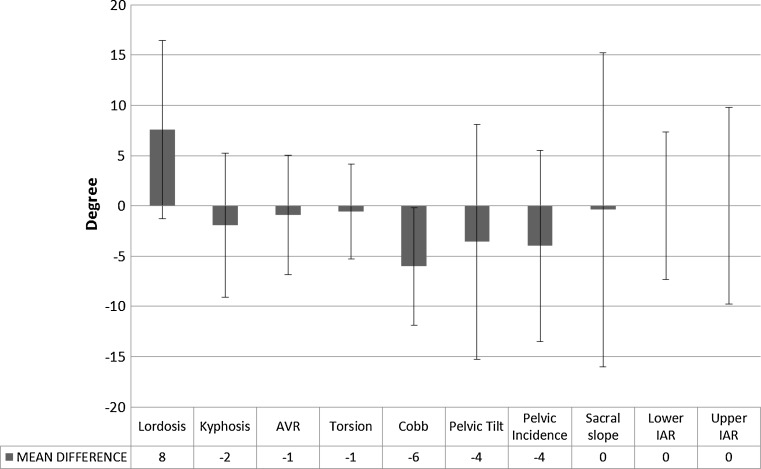
Global statistics are recorded in Fig. 2.
Fig. 2.
The mean difference without and with the brace and the standard deviation is shown. Note the high variability of the values. A statistical difference was observed for the lordosis and the Cobb angle
The mean Cobb angle improved significantly from 28° (SD 15°) to 22° (SD 14°). Lumbar lordosis significantly decreased from −46° (SD 10°) to −39° (SD 12°), but no statistical difference was noted regarding thoracic kyphosis (p = 0.14) and the sacral slope (p = 0.82). The pelvic tilt increased significantly (p = 0.001) from −11° (SD 8°) compared to from −7° (SD 8°) without brace. The pelvic incidence was almost significantly decreased (p = 0.003) from 39° (SD 7°) compared to from 43° (SD 6°) without brace.
There were no statistically significant differences with and without brace when considering transverse plane parameters: AVR (p = 0.4), from 8° (SD 7°) to 7° (SD 7°); upper IAR (p = 0.99), from −3° (SD 6°) to −3° (SD 7°); lower IAR (p = 0.97), from 2° (SD 4°) to 2° (SD 5°); and torsion (p = 0.2), from 8° (SD 5°) to 7° (SD 6°).
Discussion
The purpose of the study was to analyze the variability of the 3D effect of bracing on idiopathic scoliosis using the EOS system. The main finding of this study is the high variability of the effect of bracing on all 3D parameters involved in the analysis, which contrasts with the global statistics that only shows a significant modification of the Cobb angle and the lordosis.
There are several limitations to this study. Different types of braces from different institutions and different types of curves were involved. The purpose of this study was indeed to extract constant or variable effects of brace treatment regardless of the curve types and conception modalities. The small amount of patients in each group of brace types could not allow a comparison between the different braces.
The main objective of brace treatment is to improve and stabilize the shape of the scoliotic spine. Even if modifications of the spine shape are immediately visible on X-Rays once the brace is worn, progressive modifications of the spine may occur during the whole period of treatment. In this study, only the immediate effect of the brace was quantified but not the progressive correction, if this exists.
When considering the global statistics, the results concurred with most of the previous clinical studies [2, 7, 18]. A significant diminution of the Cobb angle was observed, which is the expected effect of brace treatment and the direct application of a force close to the apex of the curve. Diminution of the Cobb angle is indeed expected and was statistically significant but highly variable in this series. The magnitude of correction of the Cobb angle ranged from 0° to 16°. Only 50 % of the patients involved in the study had their Cobb angle improved with the brace. Several factors are involved in the correction like the rigidity and the topography of the scoliosis or the modalities of brace conception, but it was not the purpose of this study to analyze these factors.
Most of the previous clinical studies focused on the Cobb angle. However, the other 3D parameters are of primary importance as it is mandatory to stabilize the Cobb angle without creating adverse effects on the sagittal alignment and the transverse plane parameters.
A significant diminution of the lordosis was observed which is not currently reported in the literature (Fig. 3). It is however expected in the conception of Boston braces [1]. The braces analyzed in the current study were mainly European braces, which were made along with the principles of plaster casts concepts. Traditionally, a global flexion of the spine is required in the conception of European plaster casts, which could explain the diminution of lordosis in most of our cases. The modification of the lordosis was variable: in 37 % of the cases the lordosis remained unchanged and was increased in 7 % of the cases.
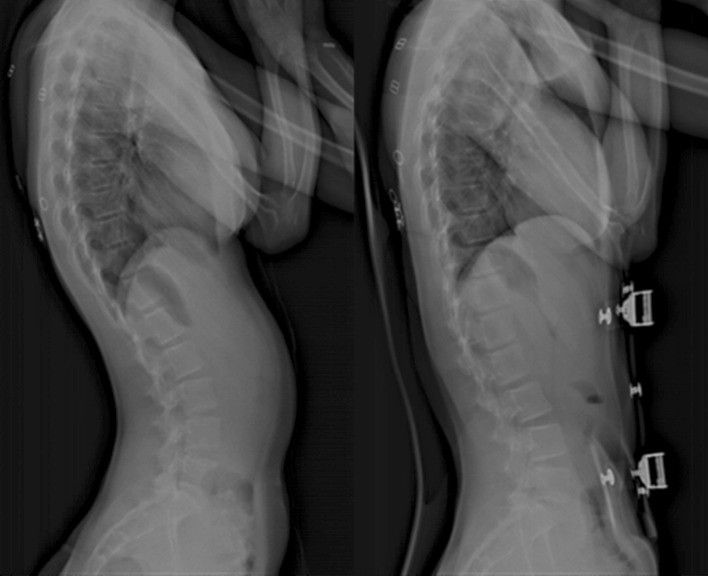
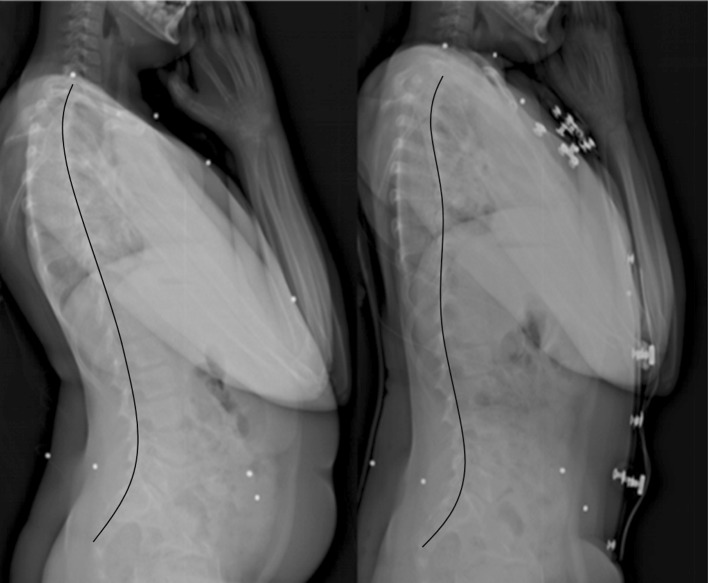
Fig. 3.
EOS standard full spine lateral views without and with the brace showing the hypolordodic effect of the brace
Bracing may artificially modify the sagittal alignment. No evidence is reported in the literature of the benefit of a diminution of the lordosis neither on the ability of correction of the scoliosis nor the sagittal alignment. It is however well reported that brace treatment flattens the thoracic kyphosis. It is usually the consequence of a posterior pressure on the rib hump, which translates the trunk anteriorly (Fig. 4). This occurs particularly in the most severe thoracic scoliosis. This “flat back” effect is a true side effect of brace treatment that is to be avoided. The consequences on the thoracic shape and pulmonary function impairment may be significant. This effect was observed in 27 % cases but in most cases the kyphosis remained unchanged.
Fig. 4.
EOS standard full spine lateral views without and with the brace showing the hypokyphosis effect of the brace
The effect of bracing on the pelvic parameters was also highly variable. Surprisingly, a decrease of the pelvic incidence was observed in 47 % and an increase in 23 % of the cases. This may only occur when there is rotation in the sacroiliac joints. Our hypothesis is that the diminution of the incidence occurs when braces apply a pressure on the caudal aspect of the sacrum and at the anterior aspect of the iliac crest. Augmentation of the incidence occurs when braces applies a pressure on the cranial aspect of the sacrum and at the anterior aspect of the iliac crest. Subsequently, the variations of lordosis may not always be correlated to the sacral slope and the pelvic tilt. These modifications of the incidence may explain the high variability of the sacral slope and pelvic tilt regardless of the modifications of the lordosis. Pelvic incidence is usually considered as an individual constant morphologic parameter, which influences the sagittal alignment of the spine. But variations of the pelvic incidence of more than 5° have been already reported after posterior spinal fusion using CD instrumentation [19]. This previous study underlined the central role of pelvis in balance and motion of the patients before and after surgery. In the current study, the suggested mechanism is not an adaptation of the pelvis to a modification of the sagittal balance but a compression of the pelvis by the brace.
To concur with the previous findings of Aubin et al. [20] and Labelle et al. [21], no statistically significant modification of the transverse plane parameters was noted when considering the mean values. However, a high variability was observed considering all the transverse plane parameters. These parameters involved should be part of a 3D pattern, which would describe potentially severe scoliosis. The rationale in analyzing these parameters is that the improvement of the whole 3D pattern would lead to a better stabilization of the scoliotic curve.
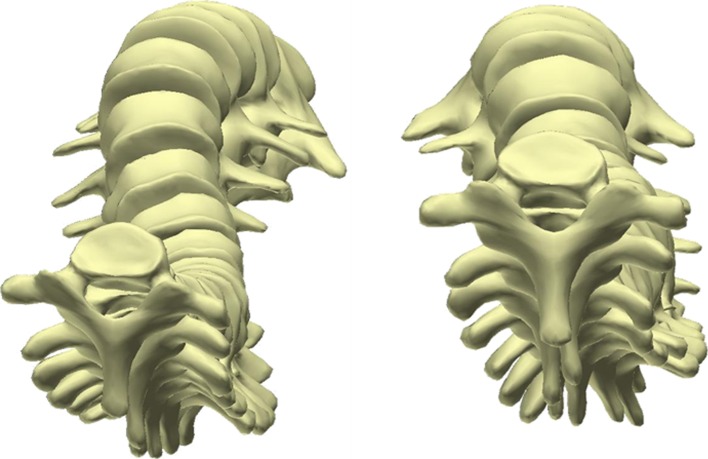
The AVR was improved more than 5° in 26 % of patients (Fig. 5), worsened in 23 % and unchanged in 51 %. But the torsion index remained unchanged in 73 % of the cases. A modification of the AVR without modification of the torsion means that the spine is globally rotated without intervertebral detorsion. The intervertebral rotations at junctions were increased, decreased and unchanged equally. Moreover, in 23 % of the patients, the AVR was worse with a brace than without which reveals the lack of understanding of brace 3D correction mechanisms.
Fig. 5.
Upper views of EOS 3D reconstructions without and with the brace showing the diminution of the AVR with the brace
Conclusion
The main aim of bracing is to provide a 3D correction of the spine without compromising sagittal alignment and pulmonary function. This study reveals the high variability of the effect of brace treatment on the 3D shape of the spine. There is still a lack of knowledge of the mechanisms of correction of brace treatment. There are cases where the whole 3D shape of the scoliosis is improved and others where the sagittal alignment and the transverse plane parameters are worsened. Global statistics reports do not reflect the true potential of brace treatment as they compare different types of braces and conception, different patient morphology (i.e., pelvic parameters, trunk shape), different type of curve topography and reducibility. 3D reconstruction and analysis of each case should help understanding the mechanisms of brace effects to improve the conservative management of scoliosis during growth.
Conflict of interest
None.
References
- 1.srs (2009) bracing manual. http://www.srs.org/professionals/education_materials/SRS_bracing_manual/
- 2.Zeh A, Planert M, Klima S, Hein W, Wohlrab D. The flexible Triac-Brace for conservative treatment of idiopathic scoliosis. An alternative treatment option? Acta Orthop Belg. 2008;74(4):512–521. [PubMed] [Google Scholar]
- 3.Schmitz A, Konig R, Kandyba J, Pennekamp P, Schmitt O, Jaeger UE. Visualisation of the brace effect on the spinal profile in idiopathic scoliosis. Eur Spine J. 2005;14(2):138–143. doi: 10.1007/s00586-004-0788-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spoonamore MJ, Dolan LA, Weinstein SL. Use of the Rosenberger brace in the treatment of progressive adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2004;29(13):1458–1464. doi: 10.1097/01.BRS.0000128756.89367.9E. [DOI] [PubMed] [Google Scholar]
- 5.Nachemson AL, Peterson LE. Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis. A prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J Bone Joint Surg Am. 1995;77(6):815–822. doi: 10.2106/00004623-199506000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Wong MS, Cheng CY, Ng BK, Lam TP, Sin SW, Lee-Shum LF, Chow HK, Tam YP. The effect of rigid versus flexible spinal orthosis on the gait pattern of patients with adolescent idiopathic scoliosis. Gait Posture. 2008;27(2):189–195. doi: 10.1016/j.gaitpost.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Lonstein JE, Winter RB. The Milwaukee brace for the treatment of adolescent idiopathic scoliosis. A review of one thousand and twenty patients. J Bone Joint Surg Am. 1994;76(8):1207–1221. doi: 10.2106/00004623-199408000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Negrini S, Minozzi S, Bettany-Saltikov J, Zaina F, Chockalingam N, Grivas TB, Kotwicki T, Maruyama T, Romano M, Vasiliadis ES. Braces for idiopathic scoliosis in adolescents. Cochrane Database Syst Rev. 2010;1:CD006850. doi: 10.1002/14651858.CD006850.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Duval-Beaupere G, Lamireau T. Scoliosis at less than 30 degrees. Properties of the evolutivity (risk of progression) Spine (Phila Pa 1976) 1985;10(5):421–424. doi: 10.1097/00007632-198506000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Pomero V, Mitton D, Laporte S, de Guise JA, Skalli W. Fast accurate stereoradiographic 3D-reconstruction of the spine using a combined geometric and statistic model. Clin Biomech (Bristol, Avon) 2004;19(3):240–247. doi: 10.1016/j.clinbiomech.2003.11.014. [DOI] [PubMed] [Google Scholar]
- 11.Humbert L, De Guise JA, Aubert B, Godbout B, Skalli W. 3D reconstruction of the spine from biplanar X-rays using parametric models based on transversal and longitudinal inferences. Med Eng Phys. 2009;31(6):681–687. doi: 10.1016/j.medengphy.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 12.Gille O, Champain N, Benchikh-El-Fegoun A, Vital JM, Skalli W. Reliability of 3D reconstruction of the spine of mild scoliotic patients. Spine (Phila Pa 1976) 2007;32(5):568–573. doi: 10.1097/01.brs.0000256866.25747.b3. [DOI] [PubMed] [Google Scholar]
- 13.Humbert L, Carlioz H, Baudoin A, Skalli W, Mitton D. 3D Evaluation of the acetabular coverage assessed by biplanar X-rays or single anteroposterior X-ray compared with CT-scan. Comput Methods Biomech Biomed Engin. 2008;11(3):257–262. doi: 10.1080/10255840701760423. [DOI] [PubMed] [Google Scholar]
- 14.Dubousset J, Charpak G, Skalli W, Kalifa G, Lazennec JY. EOS stereo-radiography system: whole-body simultaneous anteroposterior and lateral radiographs with very low radiation dose. Rev Chir Orthop Reparatrice Appar Mot. 2007;93(6 Suppl):141–143. doi: 10.1016/S0035-1040(07)92729-4. [DOI] [PubMed] [Google Scholar]
- 15.Courvoisier A, Drevelle X, Dubousset J, Skalli W (2013) Transverse plane 3D analysis of mild scoliosis. Eur Spine J. doi:10.1007/s00586-013-2862-x [DOI] [PMC free article] [PubMed]
- 16.Perdriolle R, Vidal J. A study of scoliotic curve. The importance of extension and vertebral rotation (author’s transl) Rev Chir Orthop Reparatrice Appar Mot. 1981;67(1):25–34. [PubMed] [Google Scholar]
- 17.Steib JP, Dumas R, Mitton D, Skalli W. Surgical correction of scoliosis by in situ contouring: a detorsion analysis. Spine (Phila Pa 1976) 2004;29(2):193–199. doi: 10.1097/01.BRS.0000107233.99835.A4. [DOI] [PubMed] [Google Scholar]
- 18.Chase AP, Bader DL, Houghton GR. The biomechanical effectiveness of the Boston brace in the management of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 1989;14(6):636–642. doi: 10.1097/00007632-198906000-00018. [DOI] [PubMed] [Google Scholar]
- 19.Skalli W, Zeller RD, Miladi L, Bourcereau G, Savidan M, Lavaste F, Dubousset J. Importance of pelvic compensation in posture and motion after posterior spinal fusion using CD instrumentation for idiopathic scoliosis. Spine (Phila Pa 1976) 2006;31(12):E359–E366. doi: 10.1097/01.brs.0000219402.01636.87. [DOI] [PubMed] [Google Scholar]
- 20.Aubin CE, Dansereau J, de Guise JA, Labelle H. Rib cage-spine coupling patterns involved in brace treatment of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 1997;22(6):629–635. doi: 10.1097/00007632-199703150-00010. [DOI] [PubMed] [Google Scholar]
- 21.Labelle H, Dansereau J, Bellefleur C, Poitras B. Three-dimensional effect of the Boston brace on the thoracic spine and rib cage. Spine (Phila Pa 1976) 1996;21(1):59–64. doi: 10.1097/00007632-199601010-00013. [DOI] [PubMed] [Google Scholar]