Abstract
Introduction
Gunshot wounds are one of the commonest causes of spinal injury. Management of these patients differs from other blunt trauma injuries to the spine. We present a case of a gunshot wound to the lumbar spine that occurred in 1985 which was treated non-operatively.
Methods
In the last 10 years, the patient was admitted multiple times for confusion and lead toxicity with blood levels over 100 μg/dl. Inpatient chelation therapy was implemented. After multiple recommendations for surgery, the patient agreed to have as much of the bullet removed as possible. The patient successfully underwent decompression and fusion from both anterior and posterior approaches. Lead levels subsequently declined.
Conclusion
The purpose of this paper is to show a case of a gunshot wound to the spine that ultimately caused plumbism and required surgery. Technical aspects of the surgery are described as well as pre- and post-procedural imaging. Recommendations for the general management of spine gunshot wounds are also described.
Keywords: Gunshot, Plumbism, Lead toxicity, Antibiotics, Spine

Case presentation
A 39-year-old male presented to our hospital 27 years ago with a gunshot wound to the abdomen with a colonic injury and the bullet lodged in his spine between L5 and S1 without neurologic injury. He was treated with a diverting colostomy, 7 days of broad spectrum intravenous antibiotics and a subsequent reanastamosis at 4 months post injury. The bullet was not removed and he was asymptomatic for 14 years.
Over the last 10 years he was admitted to hospital on multiple occasions (>10) for encephalopathy, bone pain, anemia, and lead levels >100 μg/dl (secondary to lead toxicity), which had been treated with chelation therapy using dimercaprol and calcium EDTA. He had responded to chelation with his lead levels dropping to 20 μg/dl and improvement of symptoms which lasted from 3 to 14 months. The idea of removing the offending bullet had been broached with him but the patient was always reluctant.
This admission, the 63-year-old patient reported dryness in his throat, dizziness, headache, blurred vision, nausea, vomiting, confusion, and new onset paresthesia along his medial left thigh and left lateral four toes. His medical problems included hypertension, gout, diverticulosis, diverticulitis, benign prostatic hypertrophy and alcoholism. Hemoglobin was 9.0 g/dl, electrolytes were normal, and his lead level was 99 μg/dl. This time the patient agreed to have surgery.
Diagnostic imaging section
An X-ray and Computed tomography (CT) scan of the lumbar spine showed a bullet in the L5 vertebral body and the L5–S1 interspace surrounded by multiple smaller bullet fragments in the lumbar and the sacral canal. Facet arthropathy and some evidence of left sided lumbar stenosis were noted (Figs. 1, 2 and 3).
Fig. 1.

AP of lumbar spine showing a retained bullet in the L5–S1 disc space
Fig. 2.

Lateral of lumbar spine showing retained bullet in the L5–S1 disc space
Fig. 3.
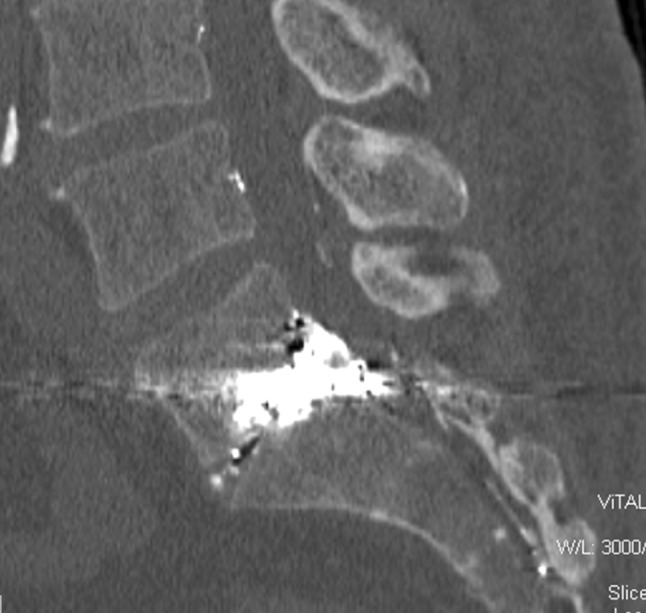
Sagittal reconstruction of Lumbar CT scan of a bullet lodged between L5 and S1. 63-year-old male with 24 year history of gunshot wounds to abdomen and LS spine with anemia, abdominal pain, and lethargy
Historical review
In the United States, gunshot wounds are among one of the common causes of spinal injury. It has been estimated that violent crime caused 13.3 % of spinal injuries prior to 1980, 24.8 % between 1990 and 1999 and 15.1 % since 2005 and the victims are primarily young males of lower socioeconomic status [1].
Computed tomography (CT) scan is useful to assess bone destruction, canal compromise and spinal stability. MRI has a limited role in the acute management of spinal cord injuries caused by gunshot wounds [2] and may be hazardous depending on the composition of the bullet and location of the retained fragments. MRI has been performed in the face of complete spinal cord injury with retained intraspinal bullets at a minimum of 2 months post injury with no movement of the bullet post scanning [3]. MRI is not recommended in the early injury period or in patients with incomplete spinal cord injuries.
The management of civilian gunshot wounds resulting in spinal cord injury is focused on the concomitant thoracic, abdominal and vascular injuries and is generally nonoperative for the spine [4, 5]. Debridement of the missile tract, as done in high velocity injuries have not been shown to result in a better outcome [4]. There is no role for surgical decompression or bullet/fragment removal for complete spinal cord injury from civilian gunshot wounds. Surgical decompression has been shown to be beneficial in patients who sustained incomplete spinal injury with bullet fragments or bony fragments that are impinging on the spinal cord or nerves when neurological decline is apparent [5], not if it is a non-evolving injury.
Civilian gunshot wounds result in spinal instability in less than 10 % of patients [6]. Most injuries are stable because interspinal ligaments which are normally torn apart during blunt injuries are not similarly affected during civilian gunshot wounds. In patients with proven spinal instability, early operative stabilization by short segment posterior spinal instrumentation using pedicle screw and rod constructs is recommended.
The recommendation for patients with gunshot injury to the spine from bullets that first transverse and perforate the bowel is still non-operative plus a 5-day cycle of antibiotics that cover gram positive, gram-negative and anaerobes. These patients need to be followed closely for at least 6 months prior to declaring the patient free of spinal infection [7, 8].
Fewer than 100 cases of lead toxicity in patients with retained bullets have been reported in the medical literature [9], and we found only one case of lead toxicity from a retained spinal bullet [10]. The onset of symptoms is insidious and a high level of suspicion is needed to prompt testing. Symptoms of lead toxicity include microcytic hypochromic anemia, encephalopathy, peripheral paresthesia due to motor axon demyelination, chronic renal failure, fatigue, malaise, abdominal complaints, headache, joint pain; memory loss, attention deficit, and behavior changes. Such cases come to medical attention only because presenting symptoms disable the patient, but even then lead toxicity is not always immediately suspected. We are largely ignorant of the percentage of gunshot victims with retained projectiles whose subclinical and clinical lead intoxication is undiagnosed.
Rational for treatment
McQuirter et al. [9] studied 451 patient suffering from gunshot wounds and determined that blood lead levels should be determined at the time of initial treatment, 2 weeks later, then monthly for the next 3 months, and finally at 1 year after the injury. Acceptable levels of lead due to environmental exposure have been reported to be <40 μg/dl in adults or <10 μg/dl in children; however, others have reported that levels of <10 μg/dl can cause harm in children and levels of >20 μg/dl is abnormal in adults [11]. In cases, where the levels of lead remain elevated, chelation therapy may be of use to acutely decrease the level [12]. In general, chelation therapy should be initiated in patients with blood lead levels >100 μg/dl. Considerations for treatment are given to asymptomatic patients with blood lead levels between 80 to 100 μg/dl and for symptomatic patients with blood lead levels between 50 and 80 μg/dl [13]. The most common chelating agents for lead poisoning are calcium EDTA, dimercaprol, and succimer. In cases where a patient is refractory to chelation therapy alone, removal of the bullet or bullet fragments may be warranted. Bullets are now being made with steel, bismuth, copper and other metals to lessen the burden lead carries with regards to the environment.
Procedure
Our patient underwent an L5–S1 discectomy, partial L5 and S1 vertebrectomy, decompression and removal of bullet fragments using an anterior approach. An interbody fusion at L5–S1 was performed using a femoral ring allograft cage, demineralized bone matrix with anterior instrumentation using a titanium one-third tubular plate and 6.5 screw into the S1 vertebral body. This was followed by a posterior L5–S1 decompression with further posterior removal of bullet fragments and L5 vertebral body, posterior L5–S1 instrumentation, posterior arthrodesis with iliac crest autograft.
Technical details
The anterior retroperitoneal approach was marred by scar in the retroperitoneal space which encapsulated the aortic bifurcation, the left iliac vein and made mobilization for the exposure long and difficult. There was only a small remnant of the L5–S1 disc which we were able to see and fluoroscopic guidance was required to assess the amount of anterior bone which needed to be removed. A Midas Rex was used to remove the anterior inferior body of L5 as the bone was sclerotic and tough. Once the anterior edge of the bullet was located, we circumscribed it with the Midas. The bone surrounding the bullet fragment was infiltrated with metallic fragments. We continued to burr the vertebra until we no longer noted metal fragments in the bone which sparkled with the headlight. Bullets lodged in soft tissue usually become encapsulated and we were hoping for this but the largest fragments abutted directly on the dura. We pulled these off gently for fear of creating a massive dura leak and left a few (Fig. 4) as they seemed to be incorporated directly into the dura. Some of the lead had migrated superiorly and inferiorly which we left as well. The posterior approach was easier as it was virgin tissue. After doing a laminectomy of L5 and laminotomy of S1 and scar excision (which was in the canal), we retracted the dura to remove more lead fragments from the canal with kerrison rongeurs, pituitary rongeurs and curettes. Pedicle screws were placed in L5 and S1 and a posterolateral fusion was accomplished with iliac crest autograft.
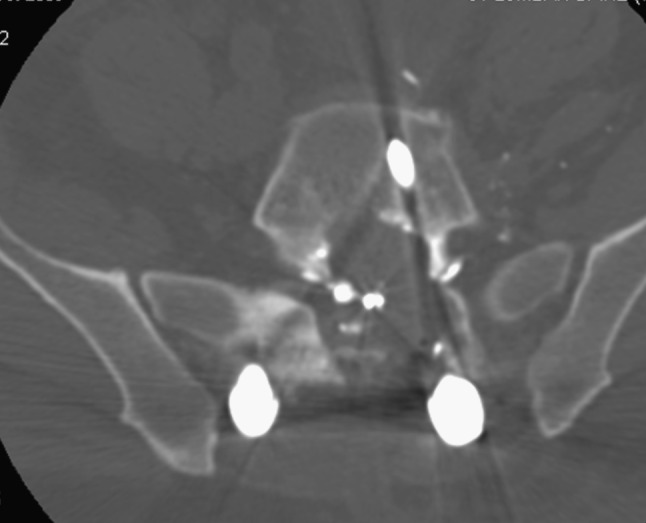
Fig. 4.
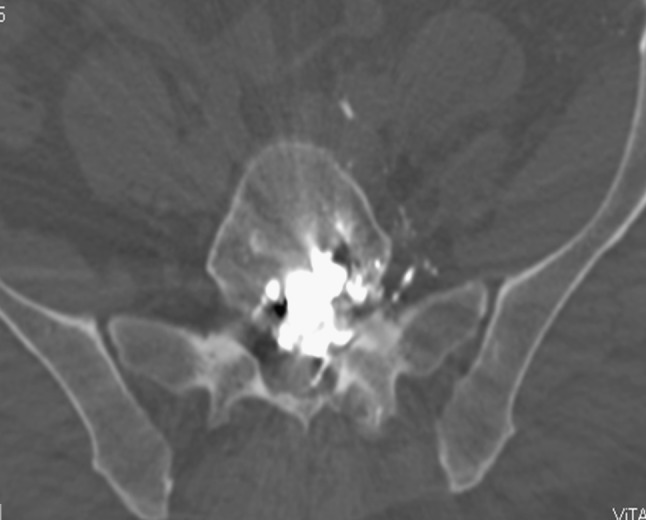
Axial CT scan of L5/S1. The patient has a lead level of 97 μg/dl and failure of chelation therapy with dimercaprol and calcium EDTA on several admissions
Procedure imaging section (Figs. 5, 6, 7 and 8).
Fig. 5.
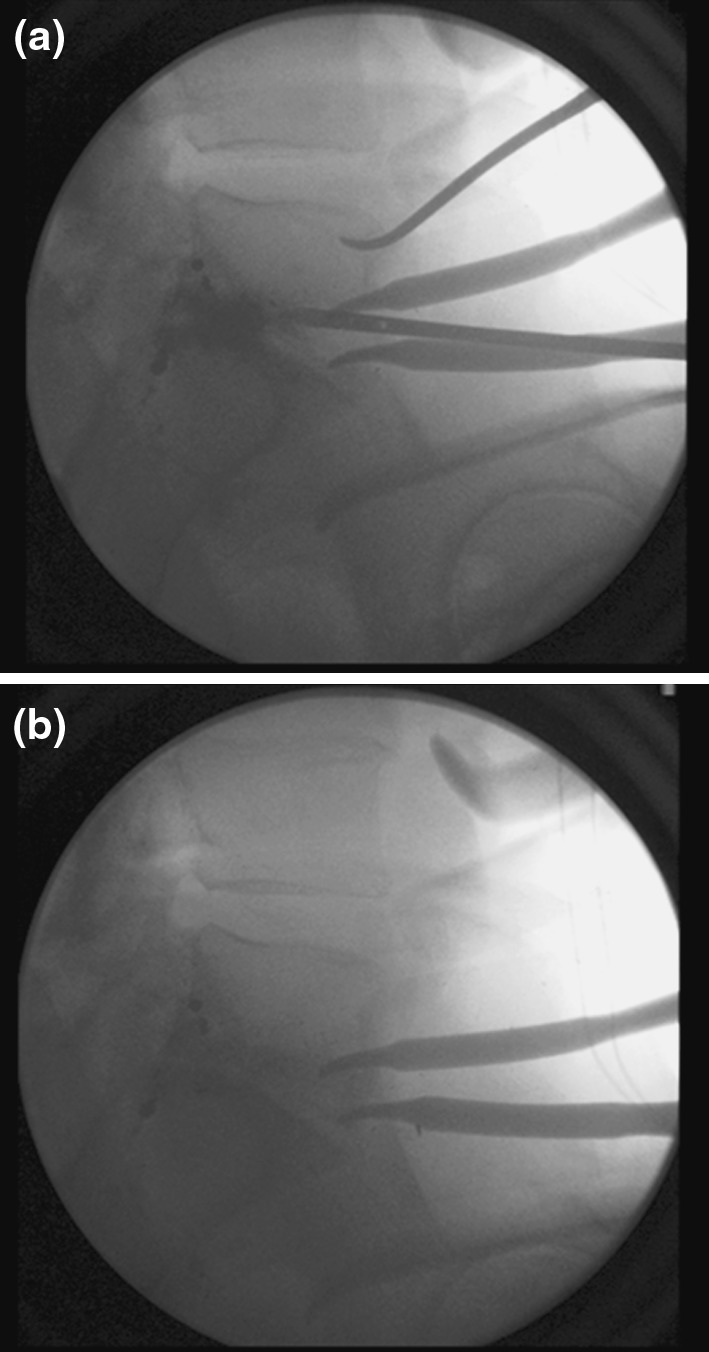
Intraoperative fluoroscopy showing removal of the bullet
Fig. 6.
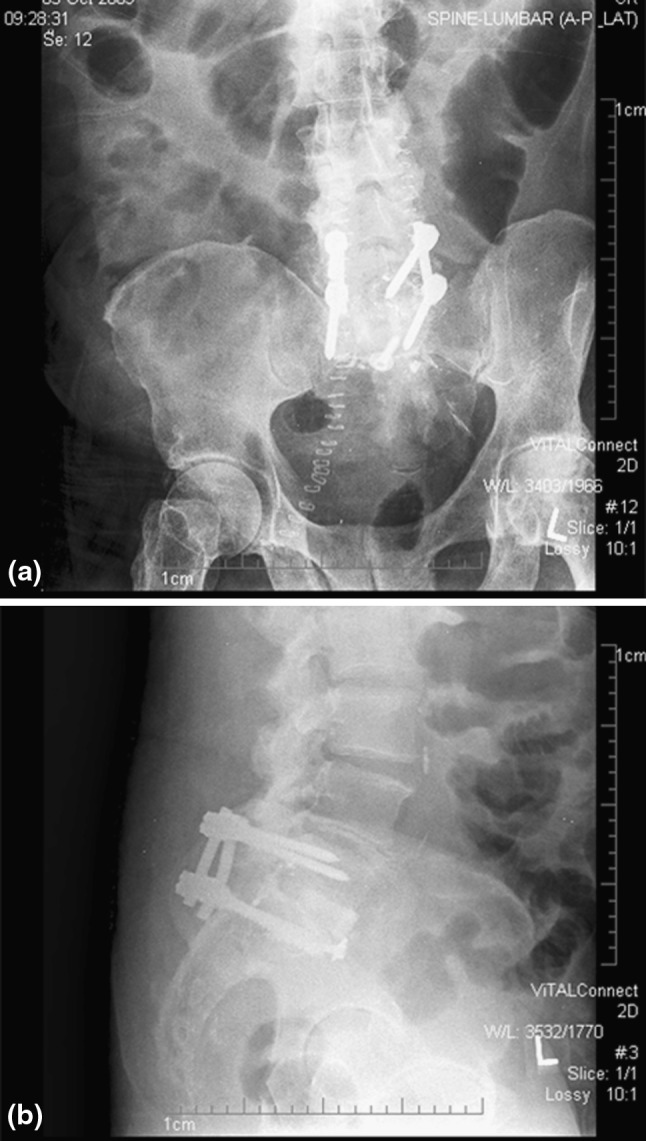
Postoperative radiographs showing removal of bullet, placement of femoral allograft and posterior fusion
Fig. 7.

Sagittal CT scan of lumbar spine after anterior and posterior decompression, partial L5 vertebrectomy interbody graft and fixation with pedicle screws L5–S1
Fig. 8.
Axial CT scan L5/S1 post operation, there is still some remnant lead around the dura. His levels fell to 4 μg/dl but began rising again after 4 months and was 24 μg/dl at 8 months post operation
Outcome and follow-up
The patient tolerated the procedure well and his symptoms improved dramatically. The next day after surgery, the patient’s lead levels were measured to be 4 μg/dl, and 15 μg/dl 1 week and 24 μg/dl 2 weeks after the procedure. At 2 months the level was back to 52 μg/dl but it stayed at 54 μg/dl 1 year after surgery and 57 μg/dl 2 years after surgery. He remains asymptomatic and has not required chelation therapy since the procedure. We continue to be worried about a gentle upward creep of his lead levels and have contemplated a revision surgery from posterior to see if we can remove lower and higher fragments as he continues to be at risk of organ damage.
Conflict of interest
None.
Contributor Information
Ben Rentfrow, Phone: +1-313-9667786, FAX: +1-313-9668400, Email: Brentfro@dmc.org.
Rahul Vaidya, Email: Rvaidya@dmc.org.
Chris Elia, Email: Eliachr1@msu.edu.
Anil Sethi, Email: Asethi3@dmc.org.
References
- 1.National Spinal Cord Injury Statistical Center, Birmingham, Alabama (2009) Spinal Cord Injury Facts and Figures at a Glance April 2009. Available at https://www.nscisc.uab.edu/public_content/pdf/FactsApr09.pdf. Accessed 28th Jan, 2010
- 2.Kitchel SH. Current treatment of gunshot wounds to the spine. Clin orthop Relat Res. 2003;408:115–119. doi: 10.1097/00003086-200303000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Smugar SS, Schweitzer ME, Hume E. MRI in patients with intraspinal bullets. J Magn Reson Imaging. 1999;9(1):151–153. doi: 10.1002/(SICI)1522-2586(199901)9:1<151::AID-JMRI20>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 4.Mirovsky Y, Shalmon E, Blankstein A, Halperin N. Complete paraplegia following gunshot injury without direct trauma to the cord. Spine. 2005;30(21):2436–2438. doi: 10.1097/01.brs.0000184588.54710.61. [DOI] [PubMed] [Google Scholar]
- 5.Waters RL, Sie IH. Spinal cord injuries from gunshot wounds to the spine. Clin Orthop Relat Res. 2003;408:120–125. doi: 10.1097/00003086-200303000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Waters RL, Hu SS. Penetrating injuries of the spinal cord: stab and gunshot injuries. In: Frymoyer JW, editor. The adult spine: principles and practice. New York: Raven Press; 1991. pp. 815–826. [Google Scholar]
- 7.Heary RJ, Vaccaro AR, Mesa JJ, Balderston RA. Thoracolumbar infections in penetrating injuries to the spine. Orthop Clin North Am. 1996;27:69–81. [PubMed] [Google Scholar]
- 8.Romanick PC, Smith TK, Kopanicky DR, Oldfield D. Infection about the spine associated with low-velocity-missile injury to the abdomen. J Bone Joint Surg. 1985;67A:1195–1201. [PubMed] [Google Scholar]
- 9.McQuirter JL, Rothenberg SJ, Dinkins GA, Kondrashov V, Manalo M, Todd AC. Change in blood lead concentration up to 1 year after a gunshot wound with a retained bullet. Am J Epidemiol. 2004;159(7):683–692. doi: 10.1093/aje/kwh074. [DOI] [PubMed] [Google Scholar]
- 10.Scuderi GJ, Vaccaro AR, Fitzhenry LN, Greenberg S, Eismont F. Long-term clinical manifestations of retained bullet fragments within the intervertebral disk space. J Spinal Disord Tech. 2004;17(2):108–111. doi: 10.1097/00024720-200404000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Gracia RC, Snodgrass WR. Lead toxicity and chelation therapy. Am J Health Syst Pharm. 2007;64(1):45–53. doi: 10.2146/ajhp060175. [DOI] [PubMed] [Google Scholar]
- 12.Kosnett MJ (2005) Lead. In: Brent J, Wallace K, Burkhart KB (eds) Critical care toxicology: the diagnosis and management of the acutely poisoned patient. Elsevier, PA, pp 821–836
- 13.Kosnett MJ, Wedeen RP, Rothenberg SJ, Hipkins KL, Materna BL, Schwartz BS, Hu H, Woolf A. Recommendations for medical management of adult lead exposure. Environ Health Perspect. 2007;115(3):463–471. doi: 10.1289/ehp.9784. [DOI] [PMC free article] [PubMed] [Google Scholar]


