Abstract

Introduction
Osteoblastoma is a rare, benign bone tumor that accounts for approximately 1 % of all primary bone tumors and 5 % of spinal tumors, mostly arising within the posterior elements of the spine within the second and third decades of life. Nonspecific initial symptoms mainly neck or back pain and stiffness of the spine remain often undiagnosed and the destructive nature of the expanding tumor can cause even neurological deficits. CT and MRI scans constitute the basic imaging modalities employed in diagnosis and preoperative planning with the former delineating the location and osseous involvement of the mass and the latter providing appreciation of the effect on soft tissues and neural elements.
Materials and methods
In our case a 23-year-old male presented with persisting head and neck pain, after being involved in a car collision a month ago. Although the initial diagnostic imaging, including plain X-rays and MRI scan failed to reveal any pathological findings, the persistence of the symptoms led to repeating imaging (CT and MRI) that showed the existence of a benign osseous tumor of the C2 lamina that was destructing the surrounding osseous structures and encompassing the right vertebral artery. The suspicion of an osteoblastoma was raised and the decision for surgical removal of the tumor was made for treating the persistent symptoms and preventing a possible neurological deficit or vascular lesion. A marginal tumor resection was performed through a posterior approach, followed by an anterior instrumented fusion. Histological examination confirmed the diagnosis of an osteoblastoma.
Results
The recovery of the patient was uneventful and a significant symptom subsidence was reported following surgery. Eighteen months postoperatively the patient remains pain free without any indications for tumor recurrence.
Conclusion
This case delineates the difficulties in diagnosing this tumor, as well as the challenges and problems encountered in its surgical management, and also the favorable prognosis when adequately treated.
Keywords: Osteoblastoma, Cervical spine, Vertebral artery, Primary bone tumor
Case presentation
A 23-year-old male presented with persisting head and neck pain, refractory to oral pain medication, after being involved in a car collision about a month ago. The initial diagnostic imaging, including plain X-rays and MRI scan that was performed immediately after the accident, failed to reveal any pathological findings and the patient was treated conservatively with oral analgesics and physiotherapy.
Since there was no improvement of the symptoms within 6 weeks following the initial injury, a neurological examination including neurophysiology tests and a new MRI scan of the cervical spine were performed.
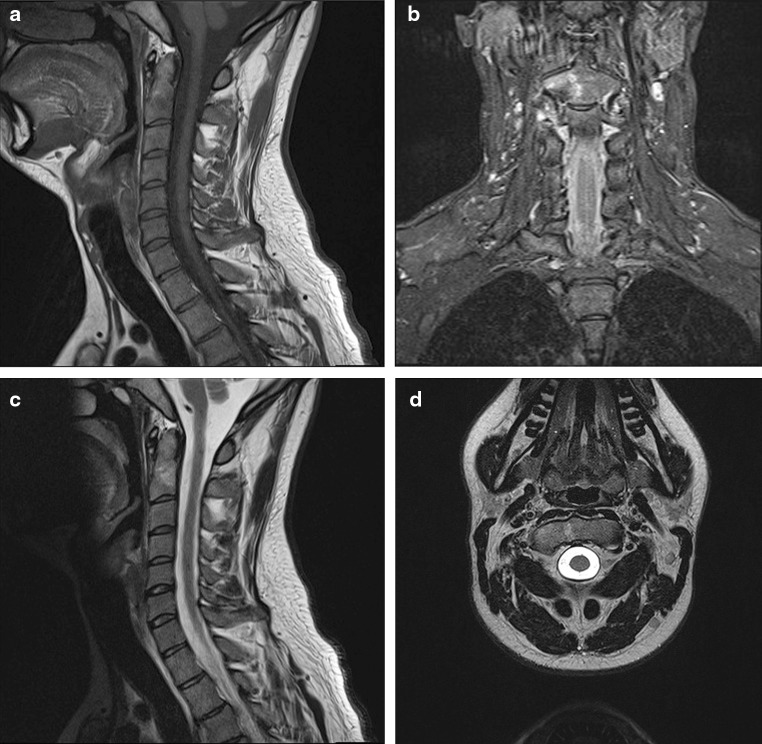
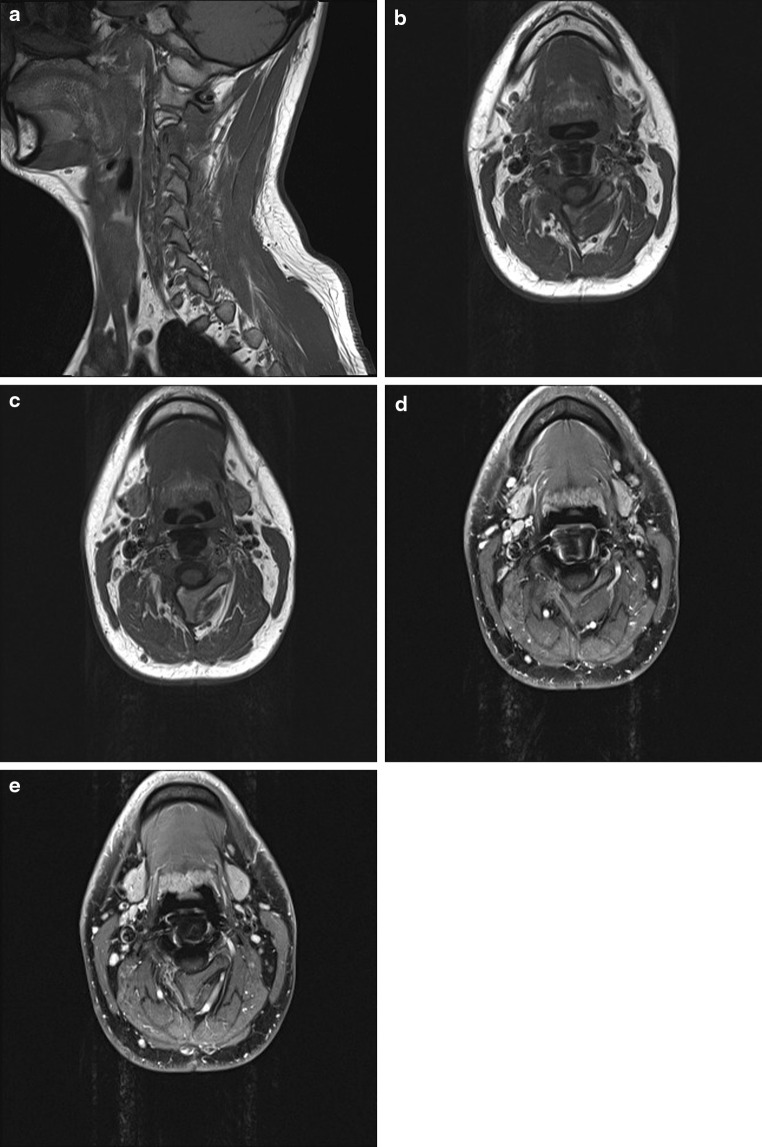
Neurological examination showed no abnormalities, but the MRI scan displayed a “right-sided osseous edema of the C2 vertebral body, without a visible fracture line or other abnormalities” (Fig. 1).
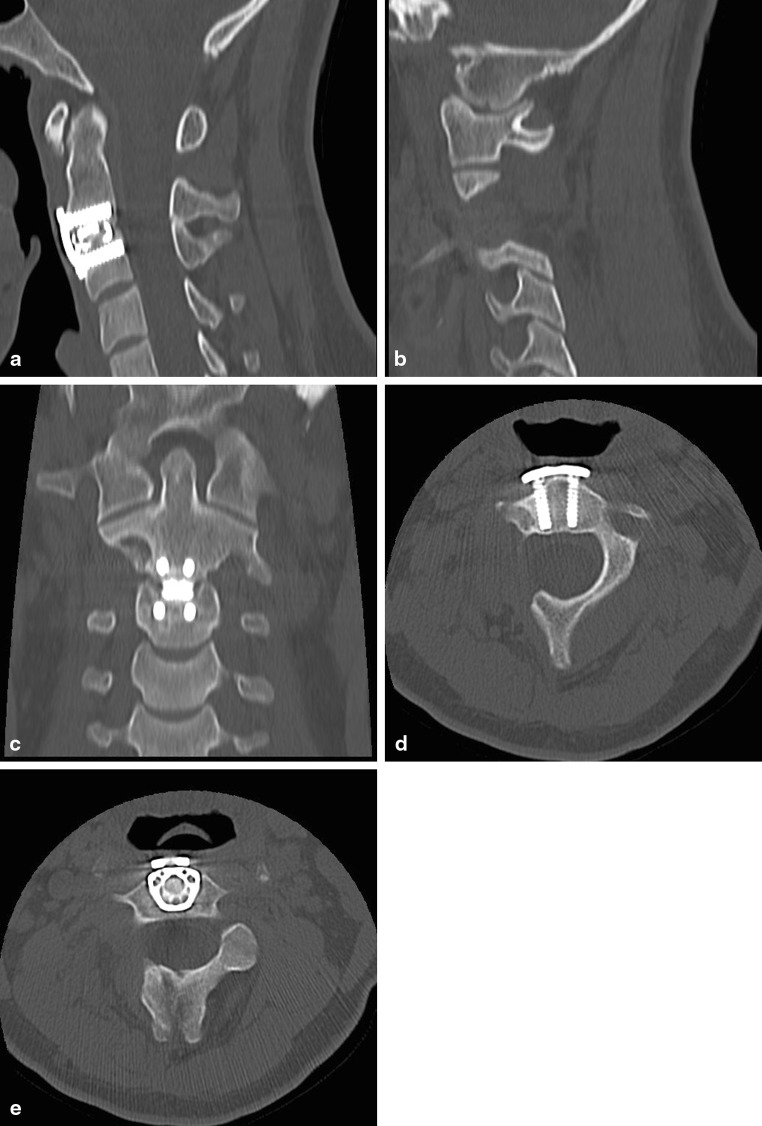
Fig. 1.
MRI scan of the cervical spine performed 6 weeks after the accident shows a non-specific right-sided osseous edema of the C2 vertebral body
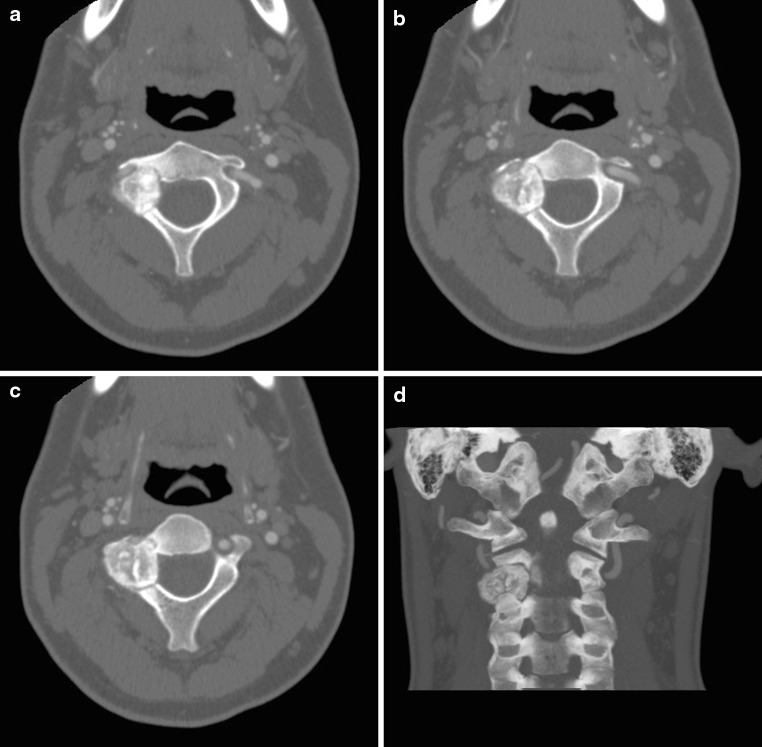
The subsequently performed CT scan demonstrated an almost 2 cm in diameter formation, situated in the lamina and the transverse process of C2. The mass displayed bubble-type calcifications and was almost completely surrounded by a foam-like zone. The adjacent bone appeared to be sclerotic, while there were no visible fresh fracture lines (Fig. 2).
Fig. 2.
CT scan displays an almost 2 cm in diameter formation, with bubble-type calcifications, surrounded by a foam-like zone and sclerosis of the adjacent bone, situated in the lamina and the transverse process of C2 and eroding the right C2/3 facet joint
According to these findings, the suspicion of a benign tumor, like osteoblastoma was raised and the decision for surgical treatment and removal of the tumor was made.
Because of the very close vicinity of the tumor to the vertebral artery and the common hypervascularity of such tumors, a CT-Angiography of the neck was performed a week prior to scheduled surgery to further assess the tumor and assist surgical planning. The angiography showed that the osteolytic formation with the sclerotic periphery and the central ossification caused a narrowing of the right C2 transverse foramen, with displacement but without infiltration or stenosis of the right vertebral artery (Fig. 3).
Fig. 3.
CT-angiography reveals that the tumor causes a narrowing of the right transverse foramen, with displacement but without infiltration or stenosis of the right vertebral artery
Historical review of the condition, epidemiology, diagnosis, pathology, differential diagnosis
Osteoblastoma is a rare, benign bone tumor that occurs in the spine approximately 32–46 % of the time, accounts for approximately 1 % of all primary bone tumors and 5 % of spinal tumors [1, 2]. The mean age at presentation in the largest series studied was 20.4 years, with a range of 6 months to 75 years. The male:female patient ratio is 2:1. [3, 4].
Osteoblastoma commonly affects the vertebral column. Most of these lesions arise within the posterior elements of the spine. Vertebral body involvement rarely occurs alone but may be involved via tumor extension through the pedicle [3, 5, 6]. The vertebral body may be more commonly affected in the cervical spine. Apart from the spine, equally common locations (30 %) are the long bones, typically the femur and the tibia [1].
Jaffe was the first to describe osteoid osteoma in 1935, and afterward Jaffe and Linctenstein independently defined benign osteoblastoma as a different entity in 1956 [7]. Some distinguish the two based on size with lesions less than 1.5 cm classified as osteoid osteoma, and those larger than 1.5 cm considered osteoblastoma [8].
Osteoblastoma is histologically similar to osteoid osteoma, but osteoblastoma occurs in slightly older patients, has a greater propensity for the spine and is more biologically aggressive, with a tendency to form a less sclerotic but more expansive mass [9, 10], often eroding through spinal cortical bone and creating large soft tissue masses [5, 8, 11, 12]. The nidus, characteristic of osteoid osteoma, is not found in osteoblastoma. Some osteoblastomas can be aggressive with a tendency to local recurrence and sometimes metastasis [12]. They can even develop a malignant transformation to osteosarcoma or sometimes the osteosarcoma can be misdiagnosed as an osteoblastoma [9].
The most important symptoms in patients with osteoid osteoma and osteoblastoma are a resistant localized neck or back pain and stiffness in the spine [7, 11]. The pain caused by an osteoblastoma is neither so severe at night nor relieves with aspirin, as does the pain caused by osteoid osteoma [9, 10, 13].
These general symptoms are often present for longer than 12 months prior to diagnosis. Delayed diagnosis occurs because initial symptoms are often nonspecific and osteoblastoma accounts for less than 1 % of all bone tumors [5]. Since in osteoblastoma pain is often accompanied by bone destruction and a bigger tumoral mass, the appearance of painful scoliosis or torticollis is more common [14] and the incidence of accompanying neurological deficits is higher [3, 7, 15].
Imaging modalities used to diagnose osteoid osteoma and osteoblastoma are primarily CT and MRI. Additional studies include plain X-ray and bone scan. Plain X-rays are more useful in the detection of osteoblastomas, but may miss small neoplasms [3, 8, 10, 11]. CT scan will delineate the location and osseous involvement of the mass and MRI will provide appreciation of the effect on soft tissues and neural elements [12, 16] but sometimes MRI images may over-diagnose the limits of the tumor [9].
If the diagnosis is uncertain or the CT and MRI are negative and there is clinical suspicion for an osteoblastoma, a technetium bone scan can be obtained [9].
The differential diagnosis in similar cases includes osteoblastoma, osteoid osteoma, tumoral calcinosis, aneurysmal bone cyst, exuberant callus, and osteochondroma [17]. Age, duration of pain and spine deformation, location of the lesion in the vertebra, imaging characteristics, tumor vascularity and pathology all have to be weighed up, even though not one of them is characteristic or specific for one of the above lesions [17].
Rationale for treatment and evidence-based literature
Expansively growing cervical spine osteoblastomas are rare, but can cause severe neurological damage as a result of their anatomical relationship to nerve structures. Moreover, cerebral vessels, especially the vertebral artery, are often covered by tumor tissue [1]. So, cervical osteoblastomas are treated for persistent pain, increase in size, or presence of a neurological deficit.
The goal of surgery for lesions involving the cervical spine is complete tumor removal and restoring functional stability. This is often accomplished with minimal morbidity despite the close proximity to vital neurovascular structures [18].
The use of advanced techniques, like intraoperative CT or navigation systems, may assist in achieving complete tumor resection [19]. Since the osteoblastoma is a hypervascularized tumor, preoperative embolization has been suggested as a tool to decrease intraoperative blood loss, reduce the incidence of tumor recurrence, and facilitate the total resection of the tumor mass [3, 9, 18]. However, this strategy has not been adopted universally regardless of the lesion’s vascularity [13].
Open surgery remains the treatment of choice of this lesion with a good prognosis when the complete resection is achieved. The most important factor to achieve a complete resection is an exact evaluation [9, 10, 12, 18]. Sometimes the tumor may present extensions to the paraspinal space that can impede the complete resection [9, 10]. Surgical treatment typically consists of marginal excision of the tumor mass with an edge of surrounding healthy tissue, decompression of adjacent neuronal structures, taking into consideration the close proximity of the vertebral arteries, followed by bone-defect filling and instrumented fusion if necessary. When the resection involves extended areas of the intervertebral articulations or pedicles, a stabilization and intervertebral fusion should be performed in order to avoid instability [1, 9, 10, 12, 18].
Atypical mass location, frequent local aggressiveness and proximity to the spinal cord and vertebral arteries often require a non-standardized surgical strategy for removal and segmental reconstruction of cervical osteoblastomas.
Radiotherapy is reserved for patients with tumors that are impossible to be completely resected or for tumors that continue to grow. The risk of potential malignant transformation after the radiation has been described [12, 18].
Marginal resection followed by instrumented fusion reconstruction was successful in preventing spinal deformity or tumor recurrence [12, 18].
However, despite complete tumor removal, lesions tend to recur in approximately 10 % of the patients, with increased recurrence rates reported in cases of partial tumor removal [11, 12, 18].
Procedure
With use of MAYFIELD-tongs and the patient in prone position a midline incision was performed following image intensifier level confirmation. The C2 and C3 lateral masses, as well as the dorsal part of C1 were exposed.
A raised osseous structure on the dorsal surface of C2 was identified as indicative of the underlying tumor, while the C2/3 facet joint could not be adequately separated.
A medially beginning osteotomy of the C2 lamina was performed, using a precise ultrasonic scalpel (Sonopet Ultrasonic Aspirator, Stryker, Kalamazoo, MI, USA), followed by an osteotomy of the C3 lateral mass, trending parallel to the C3/4 facet joint, thus leaving this unaffected. After exposing the lateral atlantoaxial joint without invading the joint capsule, the cranial border of the resection was defined and the respective osteotomy was performed. The tumor mass was removed in piecemeal fashion, displaying the dural sack and the exiting right C3 nerve root, which was completely exposed through a foraminotomy. Through further tumor mass removal the vertebral artery was exposed circumferentially, while the lateral atlantoaxial joint was spared. Finally, tumor tissue was removed from the right dorsolateral end of C2 vertebral body.
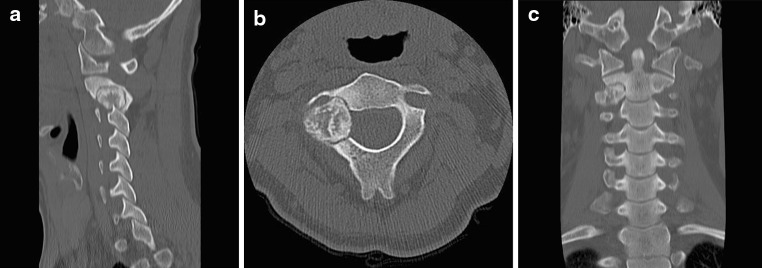
The performed intraoperative CT scan (Fig. 4) showed a tiny remnant of the tumor, lying just anteriorly to the vertebral artery. Following the CT scan, the artery was mobilized further medially and the last tumor remnants were removed.
Fig. 4.
The performed intraoperative CT scan shows a tiny remnant of the tumor, lying just anteriorly to the vertebral artery
Upon completion of the tumor removal, the dural sack, the C3 nerve root and the vertebral artery were completely exposed, while the facet joints C1/2 and C3/4 were spared.
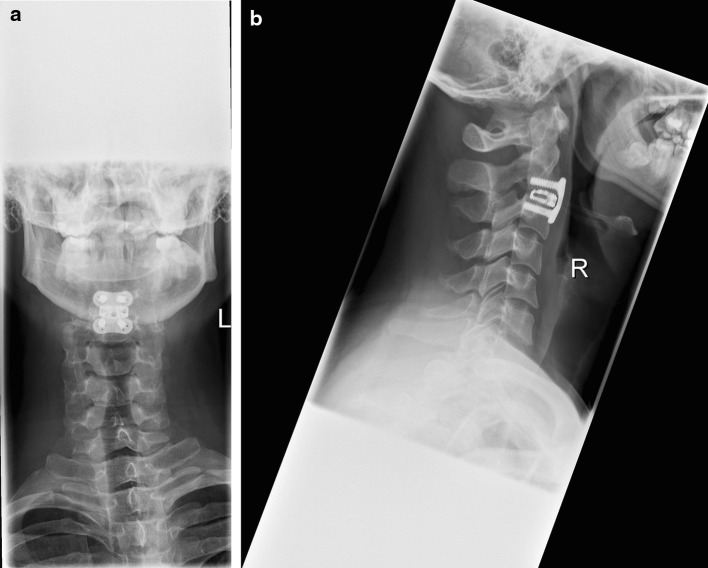
Following that, the patient was placed in a supine position and a C2/3 ACDF with use of a titanium cage (SYNCAGE C, Synthes, Umkirch, Germany) filled with fully synthetic cancellous bone graft substitute (pure β-tricalcium phosphate) (chronOS, Synthes) and an angular stable, locking plate (CSLP, Synthes) was performed in a typical fashion. Postoperative control X-rays demonstrated a correct implant positioning (Fig. 5).
Fig. 5.
Control X-rays 6 weeks post operative demonstrate a correct implant positioning
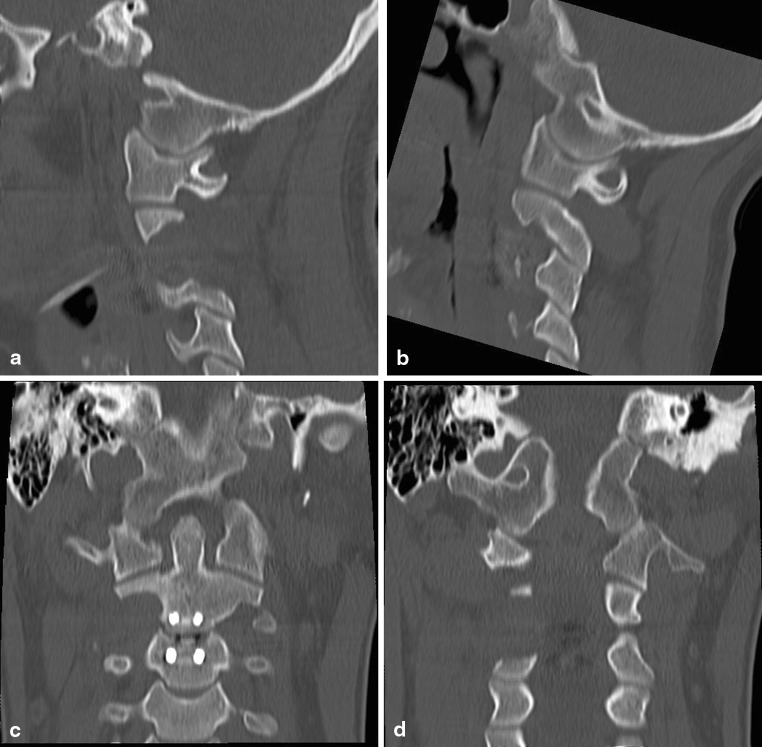
Outcome, follow-up
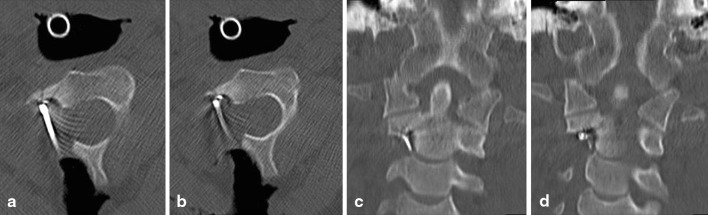
Histological examination confirmed the diagnosis of an osteoblastoma. Postoperatively, the patient was neurologically intact and he was mobilized the day after surgery, placed in a Miami collar. He reported a significant subsidence of his symptoms. The CT and MRI scans performed shortly after surgery manifested the complete removal of the tumor, as well as the lack of any neural element compression (Fig. 6a–d). At 6 and 18 months postoperatively, performed CT and MRI scans demonstrated a solid fusion, without any indication of tumor recurrence (Figs. 7a–e, 8a–e). The patient is almost completely free of symptoms and has returned to his previous level of activity. He will receive annual CT and MRI scans for the next several years to screen for possible tumor recurrence.
Fig. 6.
CT scan performed shortly after surgery demonstrates the complete removal of the tumor
Fig. 7.
6 months post operative control CT displays a solid C2–3 fusion without any indication for tumor recurrence
Fig. 8.
18 months post operative control MRI lacks any indication for tumor recurrence
Acknowledgments
No funding of any kind was received by any of the authors for this study.
Conflict of interest
There is no actual or potential conflict of interest in relation to this article.
References
- 1.Kandziora F, Pingel A. Posterior-anterior resection of a cervical spine osteoblastoma. Eur Spine J. 2010;19(6):1041–1043. doi: 10.1007/s00586-010-1461-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gutteck N, Mendel T, Held A, Wohlrab D. Cervical spine osteoblastoma in children: selective diagnostics as the basis for effective surgical management. Orthopade. 2010;39(1):92–96. doi: 10.1007/s00132-009-1530-7. [DOI] [PubMed] [Google Scholar]
- 3.Samdani A, Torre-Healy A, Chou D, Cahill AM, Storm PB. Treatment of osteoblastoma at C7: a multidisciplinary approach. A case report and review of the literature. Eur Spine J. 2009;18(Suppl 2):196–200. doi: 10.1007/s00586-008-0806-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knoeller SM, Uhl M, Adler CP, Herget GW. Differential diagnosis of benign tumors and tumor-like lesions in the spine. Own cases and review of the literature. Neoplasma. 2004;51(2):117–126. [PubMed] [Google Scholar]
- 5.Lucas DR, Unni KK, McLeod RA, O’Connor MI, Sim FH. Osteoblastoma: clinicopathologic study of 306 cases. Hum Pathol. 1994;25(2):117–134. doi: 10.1016/0046-8177(94)90267-4. [DOI] [PubMed] [Google Scholar]
- 6.Tripathy P, Sarkar S, Maiti B. Osteoblastoma of dorsal spine: a case report. Neurol India. 1999;47(4):330–331. [PubMed] [Google Scholar]
- 7.Kaner T, Sasani M, Oktenoglu T, Aydin S, Ozer AF. Osteoid osteoma and osteoblastoma of the cervical spine: the cause of unusual persistent neck pain. Pain Physician. 2010;13(6):549–554. [PubMed] [Google Scholar]
- 8.McLeod RA, Dahlin DC, Beabout JW. The spectrum of osteoblastoma. AJR Am J Roentgenol. 1976;126(2):321–325. doi: 10.2214/ajr.126.2.321. [DOI] [PubMed] [Google Scholar]
- 9.Combalia Aleu A, Popescu D, Pomes J, Palacin A. Long-standing pain in a 25-year-old patient with a non-diagnosed cervical osteoblastoma: a case report. Arch Orthop Trauma Surg. 2008;128(6):567–571. doi: 10.1007/s00402-007-0401-0. [DOI] [PubMed] [Google Scholar]
- 10.Zileli M, Cagli S, Basdemir G, Ersahin Y. Osteoid osteomas and osteoblastomas of the spine. Neurosurg Focus. 2003;15(5):E5. [PubMed] [Google Scholar]
- 11.Boriani S, Capanna R, Donati D, Levine A, Picci P, Savini R. Osteoblastoma of the spine. Clin Orthop Relat Res. 1992;278:37–45. [PubMed] [Google Scholar]
- 12.Ozaki T, Liljenqvist U, Hillmann A, Halm H, Lindner N, Gosheger G, Winkelmann W. Osteoid osteoma and osteoblastoma of the spine: experiences with 22 patients. Clin Orthop Relat Res. 2002;397:394–402. doi: 10.1097/00003086-200204000-00046. [DOI] [PubMed] [Google Scholar]
- 13.Nemoto O, Moser RP, Jr, Van Dam BE, Aoki J, Gilkey FW. Osteoblastoma of the spine. A review of 75 cases. Spine (Phila Pa 1976) 1990;15(12):1272–1280. doi: 10.1097/00007632-199012000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Saifuddin A, White J, Sherazi Z, Shaikh MI, Natali C, Ransford AO. Osteoid osteoma and osteoblastoma of the spine. Factors associated with the presence of scoliosis. Spine (Phila Pa 1976) 1998;23(1):47–53. doi: 10.1097/00007632-199801010-00010. [DOI] [PubMed] [Google Scholar]
- 15.Argyriou AA, Panagiotopoulos V, Masmanidis A, Tzortzidis F, Konstantinou D. Destructive cervical spine osteoblastoma at C5 in a young patient initially presenting with quadriparesis: case report and review of the literature. J Emerg Med. 2011 doi: 10.1016/j.jemermed.2011.05.089. [DOI] [PubMed] [Google Scholar]
- 16.Hosalkar HS, Garg S, Moroz L, Pollack A, Dormans JP. The diagnostic accuracy of MRI versus CT imaging for osteoid osteoma in children. Clin Orthop Relat Res. 2005;433:171–177. doi: 10.1097/01.blo.0000151426.55933.be. [DOI] [PubMed] [Google Scholar]
- 17.Amirjamshidi A, Abbassioun K. Osteoblastoma of the third cervical vertebra in a 16-year-old boy: case report and review of the literature. Pediatr Neurosurg. 2010;46(5):396–401. doi: 10.1159/000323422. [DOI] [PubMed] [Google Scholar]
- 18.Denaro V, Denaro L, Papalia R, Marinozzi A, Di Martino A. Surgical management of cervical spine osteoblastomas. Clin Orthop Relat Res. 2007;455:190–195. doi: 10.1097/01.blo.0000238846.34047.d9. [DOI] [PubMed] [Google Scholar]
- 19.Rajasekaran S, Kanna RM, Kamath V, Shetty AP. Computer navigation-guided excision of cervical osteoblastoma. Eur Spine J. 2010;19(6):1046–1047. doi: 10.1007/s00586-010-1463-1. [DOI] [PMC free article] [PubMed] [Google Scholar]