Abstract
Purpose
To investigate which pre- and postoperative radiographic parameters are significantly correlated with the immediate postoperative coronal balance (CB) in Lenke 5C AIS patients, and to identify any radiographic parameter that is correlated with the ultimate CB at a minimum follow-up of 2 years.
Methods
Forty Lenke 5C AIS patients were recruited in the current study. Preoperative, immediate postoperative, and the latest follow-up radiographs were reviewed measuring various radiographic parameters related to UIV and LIV. The correlations between different parameters and CB were then studied.
Results
The average follow-up time was 35.2 months. Correlation analysis showed that the following radiographic parameters significantly associated with the immediate postoperative CB in Lenke 5C patients: preoperative CB (r = 0.66, p < 0.01), preoperative UIV translation (r = 0.61, p < 0.01), preoperative LIV tilt (r = 0.61, p < 0.01), postoperative UIV translation (r = 0.51, p < 0.05), and postoperative LIV tilt (r = 0.50, p < 0.05). At the last follow-up, only the final UIV tilt was inversely correlated with the ultimate CB (r = −0.58, p < 0.05). Seven patients presented with coronal imbalance immediately after surgery. However, only one of the seven patients presented with coronal imbalance at the last follow-up, and the other six achieved C7PL–CSVL distance within 10 mm.
Conclusions
In Lenke 5C patients, preoperative UIV translation and LIV tilt are two important parameters that can predict the immediate postoperative CB. During the postoperative follow-up, UIV tilt may play a very important role in compensating for postoperative coronal imbalance.
Keywords: Idiopathic scoliosis, Lenke type 5 curve, Coronal balance, Lowest instrumented vertebra, Upper instrumented vertebra
Introduction
Patients with adolescent idiopathic scoliosis (AIS) can be treated by spinal fusion using diverse types of instrumentations [1]. It is of primary importance that not only this surgery offers long-term stability until biological stability is achieved [2], but also restore a well-balanced spine in the coronal and sagittal planes [3]. Traditionally, coronal balance (CB) is measured and quantified by the perpendicular distance between the coronal C7 plumbline (C7PL) and the central sacral vertical line (CSVL), with a value >20 mm being defined as imbalance [4]. Numerous studies have used the C7PL–CSVL distance as an assessment tool for surgical outcomes of AIS [5–8], but there is a paucity of data specifically addressing the postoperative CB in AIS [9], especially the ultimate CB after a long period of follow-up.
A recent study [9] investigated the associations between the preoperative radiographic parameters and the immediate postoperative CB in 27 Lenke 5C patients and found that the preoperative lowest instrumented vertebra (LIV) tilt was strongly associated with the postoperative CB [9]. In addition, preoperative LIV tilt ≥25° and postoperative LIV tilt ≥8° were found to be two risk factors for developing coronal imbalance after surgery [9]. However, two limitations were also noted in their study [9]. First, it lacked the consideration of the probable effect of the upper instrumented vertebra (UIV) on regulating postoperative CB. Second, “postoperative” was just referred to “immediately after surgery”, other than the long-term CB.
In our practice, we have noticed that during selective posterior fusion for Lenke 5C patients, centering the UIV in the midline was difficult in some patients, and coronal imbalance might occur in these patients immediately after surgery, indicating that the coronal imbalance might associate with the translation of the UIV. In addition, we also noticed that over a longer period of follow-up, the postoperative coronal imbalance could be compensated for, implying that the final outcome of CB of the Lenke 5C patients after selective posterior fusion and instrumentation might not be simply dependent on the aforementioned radiographic parameters. Hence, the purpose of this study was to investigate which of the pre- and postoperative radiographic parameters, including the parameters pertinent to the UIV and the LIV, significantly correlated with the immediate postoperative CB in Lenke 5C AIS patients. Furthermore, we also attempted to identify any radiographic parameter that is correlated with the ultimate CB at a minimum follow-up of 2 years.
Materials and methods
Subjects
This is a retrospective case series study approved by the institution review board (IRB) of our hospital. From January 2006 to September 2009, 40 Lenke 5C AIS patients who underwent selective posterior spinal fusion at a single institution were recruited. The inclusion criteria were as follows: (1) patients diagnosed with AIS who had a major thoracolumbar/lumbar curve classified as type 5C according to the Lenke classification system [10], (2) patients who underwent a one-stage selective posterior surgery, and (3) patients who had a minimum follow-up of 2 years. The average age at surgery was 14.6 ± 1.5 years (range 12–18 years). There were 36 females and 4 males. At the time of surgery, skeletal maturity according to Risser’s sign was 3 in 10 cases, 4 in 25, and 5 in 5 with a mean of 4.1. Any AIS girl with one or more of the following features was excluded: evidence of congenital deformities, neuromuscular diseases, metabolic diseases, skeletal dysplasia, connective tissue abnormalities, mental retardation, or a history of recent steroid intake.
Posterior fusion was accomplished with local and iliac bone, and the fusion levels were basically decided according to Lenke et al. [11]. Specific screw–rod instrumentation systems used in this series were the TSRH system (Medtronic Sofamor Danek, USA) in 10 cases, the CDH Legacy system (Medtronic Sofamor Danek, USA) in 26 cases and the Expedium system (DePuy Spine, USA) in the remaining 4 cases. All the surgeries were performed by one team under intraoperative neuroelectrophysiological monitoring.
Radiographic evaluation
Pre- and postoperative standing upright posteroanterior and lateral radiographs as well as preoperative supine left and right side-bending radiographs were used for radiographic assessment. Preoperative, immediate postoperative (10 days after surgery), and the latest follow-up radiographs were obtained on long-cassette films in routine fashion. All radiographic and clinical data collections were done by an independent observer (Z.L.) who was not involved in the treatment of the patients. A total of 34 patients had a left-sided thoracolumbar/lumbar (TL/L) curve, while the remaining 6 patients had a right-sided TL/L curve whose radiographs were measured as mirror images.
Cobb angles of the major TL/L curve and minor thoracic curve were measured on all radiographs using the standard method [12]. Coronal balance was measured in millimeters as the perpendicular distance between the C7 plumbline and the central sacral vertical line (C7PL–CSVL) [9]. The radiographic parameters relevant to the UIV and LIV were measured as follows [9]: (1) UIV and LIV translation was defined as the distance in millimeters from the geometric center of the UIV and LIV to the CSVL, (2) UIV and LIV rotation was graded according to the Nash-Moe technique [13], (3) UIV and LIV tilt was defined as the inclination in degrees of the superior endplate to the horizontal for the UIV and of the inferior endplate to the horizontal for the LIV, (4) UIV disc angle was defined as the angle subtended between the superior endplate of the UIV relative to the inferior endplate of the adjacent upper vertebra, while LIV disc angle was subtended between the inferior endplate of the LIV relative to the superior endplate of the adjacent lower vertebra. If the C7PL or the center of UIV and LIV shifted to the preoperative convex side relative to the CSVL, the CB or UIV and LIV translation was accordingly defined as “+”, otherwise as “−”. The UIV and LIV tilt and disc angle were defined as “+” when opening to the preoperative concave side and as “−” when opening to the preoperative convex side. Using Surgimap Spine imaging software (download from www.surgimap.com, Version: 1.1.2.271, provided by Nemaris Inc., New York), all the radiographic parameters were measured.
Statistics
The data were analyzed using SPSS 16.0 statistical software (SPSS Inc., Chicago, IL). All the data were presented as mean ± SD. Paired student’s t tests were performed to assess the differences of radiographic parameters between three time points (preoperatively, immediate postoperatively and at the last follow-up). Bivariate correlation tests were carried out to analyze the correlation of each radiographic parameter to the CB immediately after surgery and at the last follow-up. Spearman’s correlation coefficient was used for the ordinal data, while Pearson’s correlation coefficient was used for the continuous data. Correlation coefficient of “r” was stratified as follows: high correlation (0.80–1.00), marked correlation (0.60–0.79), moderate correlation (0.40–0.59), and <0.40 was regarded as low or no correlation. In addition, curve estimation analysis was performed to determine the best-fit trend (e.g., linear, quadratic, cubic, etc.) of the correlation between significant radiographic parameters and postoperative CB. A p value <0.05 was considered to be significant.
Results
In the current study, the upper end vertebra (UEV) and the lower end vertebra (LEV) were determined using the Cobb method. The UIV was T10 (n = 20), T11 (n = 18), or T12 (n = 2). The UIV was equal to the UEV (UIV = UEV) in 22 patients, 1 above the UEV (UIV = UEV−1) in 14 patients, and 1 below the UEV (UIV = UEV + 1) in 4 patients. The LIV was L3 (n = 28) or L4 (n = 12). The LIV was equal to the LEV (LIV = LEV) in 28 patients, 1 above the LEV (LIV = LEV−1) in 8 patients, and 1 below the LEV (LIV = LEV + 1) in 4 patients.
The preoperative and postoperative characteristics of the AIS patients are presented in Table 1. The average follow-up time was 35.2 months (range 24–55 months). The average preoperative Cobb angle of the TL/L curve was 48.9° ± 4.8°, and the average immediate postoperative Cobb angle of the TL/L curve was 13.1° ± 2.7°, representing an average surgical correction rate of 74.3 ± 10.2 %. As for the thoracic curve, the average preoperative Cobb angle was 26.5° ± 6.8°, and the average immediate postoperative Cobb angle was 11.5° ± 7.6°, representing an average surgical correction rate of 60.0 ± 26.9 %. In addition, there were significant differences between the pre- and postoperative CB (17.4 ± 11.4 vs. 7.1 ± 7.8 mm, p < 0.05). The average preoperative UIV tilt was 17.7° ± 4.0° and the average preoperative UIV disc angle was 2.2° ± 1.8°, while the average preoperative LIV tilt was 22.9° ± 4.0° and the average preoperative LIV disc angle was 3.4° ± 3.6°. The preoperative UIV rotation was grade 0 in 24, grade 1 in 15 patients, and grade 2 in the remaining 1 patients. The preoperative LIV rotation was grade 0 in 12 patients, grade 1 in 24 patients, and grade 2 in the remaining 4 patients. The average preoperative supine side-bending Cobb angles of the TL/L curve and thoracic curve were, respectively, 12.5° ± 7.9° and 10.3° ± 5.2°, representing an average preoperative curve flexibility of 72.4 ± 15.6 % for the TL/L curve and 62.0 ± 17.8 % for the thoracic curve. Furthermore, on the convex side-bending radiograph, the UIV/LIV should be derotated to neutral position (Nash-Moe Grade 0), and meanwhile all the UIV and LIV were horizontal in the preoperative side-bending films.
Table 1.
Preoperative and postoperative radiographic characteristics of Lenke 5C patients
| Preoperation | Postoperation | Last follow-up | |
|---|---|---|---|
| TL/L Cobb angle (°) | 48.9 ± 4.8 | 13.1 ± 2.7a | 15.4 ± 3.1a |
| Thoracic Cobb angle (°) | 26.5 ± 6.8 | 11.5 ± 7.6a | 14.1 ± 7.4a |
| Coronal balance (mm) | 17.4 ± 11.4 | 7.1 ± 7.8a | 6.6 ± 7.3a |
| UIV translation (mm) | 20.3 ± 7.0 | 4.8 ± 9.5a | 3.6 ± 10.0a |
| UIV tilt (°) | 17.7 ± 4.0 | 6.2 ± 3.4a | 7.2 ± 3.4a |
| UIV disc angle (°) | 2.2 ± 1.8 | 0.4 ± 2.2a | 0.1 ± 2.3a |
| LIV translation (mm) | 19.7 ± 4.6 | 11.4 ± 3.3a | 11.4 ± 4.1a |
| LIV tilt (°) | 22.9 ± 4.0 | 2.5 ± 2.9a | 2.9 ± 3.0a |
| LIV disc angle (°) | 3.4 ± 3.6 | −6.1 ± 2.8a | −5.1 ± 2.6a |
| Thoracic kyphosis | 12.4 ± 7.7 | 20.0 ± 8.0a | 24.0 ± 7.8a |
| Lumbar lordosis | −49.6 ± 6.8b | −47.8 ± 6.8b | −54.4 ± 6.8 |
aSignificantly different from the preoperative value, p < 0.05
bSignificantly different from the last follow-up value, p < 0.05
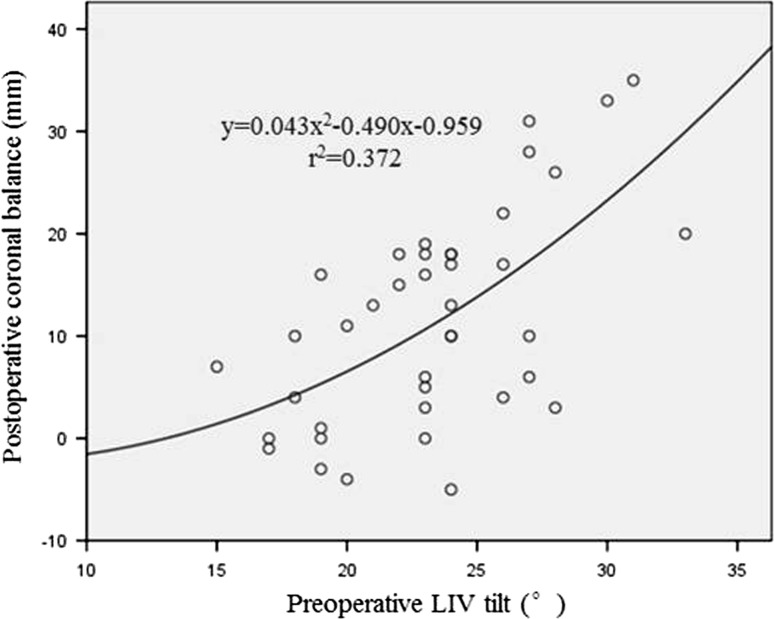
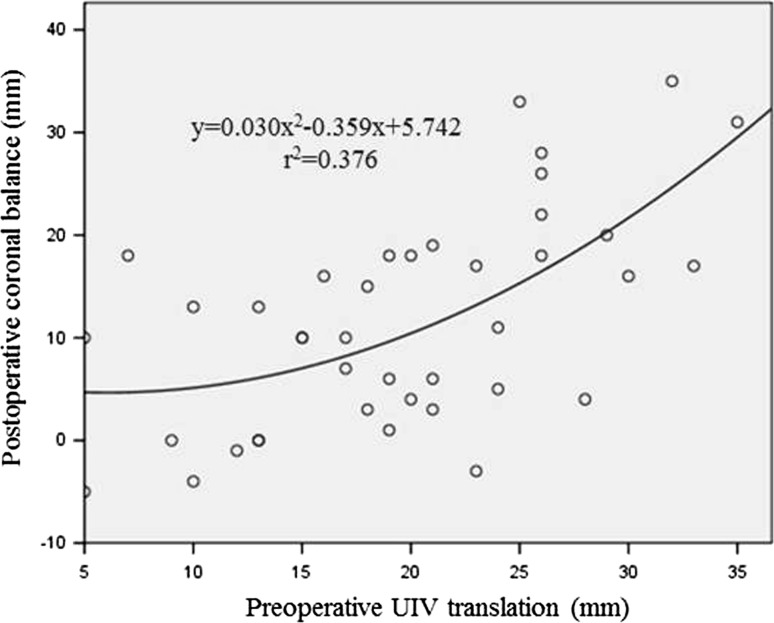
Correlation analysis showed that the following radiographic parameters significantly associated with the immediate postoperative CB: preoperative CB (r = 0.66, p < 0.01), preoperative UIV translation (r = 0.61, p < 0.01), preoperative LIV tilt (r = 0.61, p < 0.01), postoperative UIV translation (r = 0.51, p < 0.05), and postoperative LIV tilt (r = 0.50, p < 0.05). Curve estimation analysis demonstrated that the preoperative UIV translation and LIV tilt both exhibited a quadratic trend with the immediate postoperative CB (Figs. 1, 2).
Fig. 1.
Correlation of the preoperative LIV tilt and the postoperative coronal balance
Fig. 2.
Correlation of the preoperative UIV translation and the postoperative coronal balance
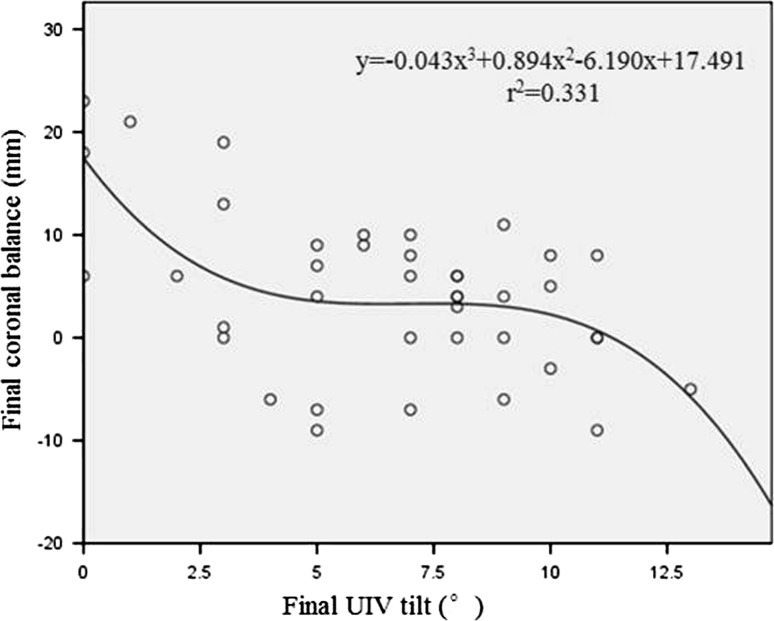
However, neither the preoperative radiographic parameters nor the immediate postoperative parameters were associated with the final CB. Only the final UIV tilt was inversely correlated with the ultimate CB (r = −0.58, p < 0.05). Curve estimation analysis demonstrated that the final UIV tilt exhibited a cubic trend with the final follow-up CB (Fig. 3).
Fig. 3.
Correlation of the final UIV tilt and the final coronal balance
Fusion was achieved in all patients at the last follow-up and no instrumentation-related complications were noted. Seven patients presented with coronal imbalance immediately after surgery. Five of the seven patients exhibited pre-existing coronal imbalance before surgery. The preoperative UIV translation of these seven patients was equal to or greater than 25 mm, and the preoperative LIV tilt of all the seven patients exceeded 25°. The postoperative UIV translation of all seven patients failed to reduce to <10 mm, whereas all but one patient achieved C7PL–CSVL distance within 10 mm at the last follow-up, with the average UIV tilt increased from 3.8° postoperatively to 8.4° at the last follow-up.
Discussion
CB has been commonly used as an evaluation tool for scoliosis correction [14–17]. However, few authors have explicitly addressed postoperative CB in Lenke 5C AIS patients [9]. Li et al. [9] observed a strong relationship between postoperative CB and preoperative LIV tilt, as well as between postoperative CB and postoperative LIV tilt. Nevertheless, his study [9] was limited because it overlooked the significance of UIV and lacked analysis of the final CB at the last follow-up. In Lenke 5C patients, UIV was frequently selected as the vertebra at the thoracolumbar junction, which might also have an effect on regulating postoperative CB. In addition, a postoperatively imbalanced spine can be rebalanced over a period of follow-up according to the compensatory mechanism. Therefore, the significance of UIV and the final outcome of CB have to be recognized to further improve the surgical treatment of AIS patients with Lenke type 5.
To our best knowledge, this is the first study that comprehensively investigated the correlations between radiographic parameters and postoperative CB in Lenke 5C patients with a long-term follow-up. Our study demonstrated that preoperative CB, UIV translation, and LIV tilt had significant correlation with immediate postoperative CB. Again, postoperative UIV translation and LIV tilt also had significant correlation with immediate postoperative CB. However, the postoperative CB was not related to the preoperative UIV/LIV rotation. The above results indicated that the Lenke 5C AIS patients who had a greater UIV translation and LIV tilt before surgery might be at higher risk of developing immediate postoperative coronal imbalance. We further analyzed seven patients who presented with coronal imbalance immediately after surgery in our cohort. The preoperative UIV rotation was grade 0 in five patients, grade 1 in one patient, and grade 2 in the remaining one patient. The preoperative LIV rotation was grade 0 in two patients, grade 1 in four patients, and grade 2 in the remaining one patient. Furthermore, the preoperative UIV and LIV rotation in the side-bending radiographs were neutral (grade 0) in all the seven patients. The common radiographic features of these seven patients were as follows: preoperative UIV translation ≥25 mm, postoperative UIV translation ≥10 mm, and preoperative LIV tilt ≥25°. Based on these results, we concluded that, in Lenke 5C AIS patients, preoperative UIV translation equal to or exceeding 25 mm and preoperative LIV tilt equal to or exceeding 25°, as well as the inability of surgical correction to decrease the postoperative UIV translation below 10 mm were risk factors for developing coronal imbalance immediately after surgery.
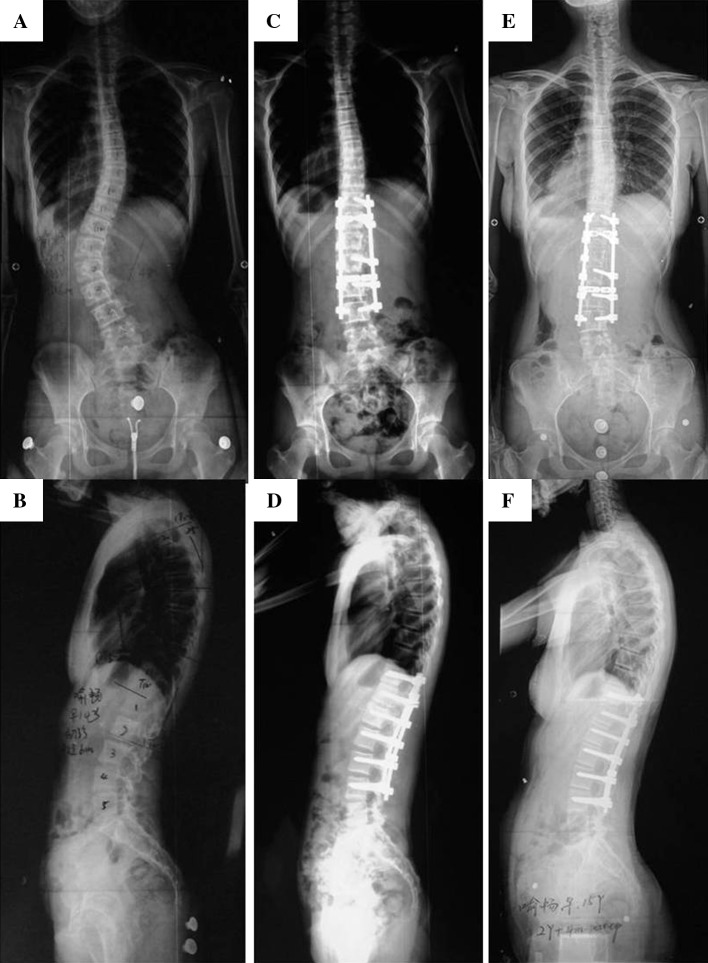
With regard to the CB at the last follow-up, surprisingly, only the final UIV tilt was inversely correlated with the C7PL–CSVL distance. This result suggests that the ultimate outcome of CB may not be dependent on either preoperative or postoperative radiographic status, but on self-compensation during follow-up. Further analysis of the seven patients who presented with immediate postoperative coronal imbalance revealed that only one of them still had coronal imbalance at the last follow-up, and the other six patients all demonstrated good CB with C7PL–CSVL distance <10 mm. The common radiographic feature of these six patients was that the postoperative UIV tilt increased during the follow-up, with an average increment of approximately 5°. Accordingly, the patient who still had coronal imbalance at the last follow-up presented the same degrees of UIV tilt as it was postoperatively. Based on these results, we concluded that, in Lenke 5C type curves, patients with coronal imbalance immediately after surgery may not be associated with a higher risk of presenting coronal imbalance at the 2-year follow-up, and the UIV tilt was of primary importance in compensating for coronal imbalance during the postoperative period of follow-up (Fig. 4).
Fig. 4.
a, b Preoperative radiographs of a 14-year-old girl with Lenke 5C AIS showed a major TL/L curve of 48° and a minor thoracic curve of 32°. Preoperative C7PL–CSVL distance was 22 mm. Preoperative UIV (T11) translation was 26 mm and preoperative LIV (L4) tilt was 27°. c, d Immediate postoperative radiographs of the same patient showed that postoperative C7PL–CSVL distance was increased to 28 mm, with a postoperative UIV translation of 16 mm and a postoperative LIV tilt of 8°. The TL/L curve was corrected to 10° (correction rate, 79.2 %) and the thoracic curve was corrected to 9° (correction rate, 71.9 %). Postoperative UIV tilt was 2°. e, f As shown in the final radiographs (28 months after surgery), the final C7PL–CSVL distance was reduced to 1 mm, with an increase of UIV tilt up to 7°. The final UIV translation was 6 mm and the final LIV tilt was 6°. The TL/L curve mildly increased to 13° (correction rate, 72.9 %), while the thoracic curve markedly increased to 15° (correction rate, 53.1 %)
After selective posterior fusion and instrumentation, the major structural TL/L curve is directly corrected, with spontaneous correction of the minor thoracic curve. According to the results of the current study, UIV tilt may play a very important role in this process, because it is the inflection point connecting the upper non-instrumented thoracic spine and the lower instrumented TL/L spine. The equilibrium of the thoracic curve and TL/L curve can be easily restored by simply increasing the inclination of the UIV. In the authors’ opinions, two mechanisms could lead to increase in the UIV tilt. One possible mechanism is the decrease of the LIV tilt, and the other is the loss of correction of the TL/L curve. In most cases, both mechanisms simultaneously contribute to the inclination of the UIV. This is supported by our results that the UIV tilt was negatively correlated with the LIV tilt and TL/L correction rate. Furthermore, as the UIV tilts, the upper thoracic curve increases accordingly. Finally, the equilibrium of the thoracic curve and TL/L curve could be obtained, which in turn leads to a well-balanced spine in the coronal plane.
One possible negative effect of the UIV compensation is the loss of correction of the thoracic and TL/L curve. Analysis of the imaging features of the six patients who restored CB at the last follow-up showed mild changes in the postoperative Cobb angle and correction rate of the TL/L curve at the last follow-up, probably because the TL/L curve was fused, but the average thoracic Cobb angle significantly increased from 11.1° postoperatively to 15.9° at the last follow-up. Therefore, it is concluded that the compensation for postoperative coronal imbalance via the UIV tilt can be obtained, however, probably, at the price of correction loss of the unfused thoracic spine.
Though the final CB was negatively correlated with the final UIV tilt, over-inclination of the UIV may likewise lead to the imbalance of the spine. Curve estimation analysis showed that the final UIV tilt exhibited a cubic trend with the final CB (Fig. 3), which meant that too small or too large UIV tilt both could result in increasing C7PL–CSVL distance, but in different directions.
The choice of UIV and LIV in Lenke 5C patients has been a subject of debate in the past decade [18, 19]. Although rare general algorithms have been proposed for reference, spine surgeons usually select the UIV and LIV prior to surgery based on experiences and preferences. In this study, the flexibility and rotation of the lumbar curve both in standing and side-bending films were two important factors for determining the fusion levels. In addition, our study indicated that preoperative UIV translation and LIV tilt were strongly correlated with immediate postoperative CB and should be considered as essential factors in decision-making for Lenke 5C patients. When the preoperative UIV translation was equal to or greater than 25 mm in Lenke 5C patients, we recommend extending the instrumentation to one more upper vertebra to obtain better CB after surgery. Similarly, when the planned LIV tilts by more than 25°, we recommend extending the instrumentation to one more lower vertebra.
One primary limitation of the current study was a lack of investigation into the preoperative and postoperative quality of life in Lenke 5C patients. Evaluation of patients’ quality of life serves as an important tool that determines the long-term outcome of surgical intervention. Further studies that include patients’ quality of life at different stages may be conducted in a similar manner to refine our findings.
Conclusions
In Lenke 5C patients, preoperative UIV translation and LIV tilt are two important parameters that can predict the immediate postoperative CB. Preoperative UIV translation ≥25 mm and LIV tilt ≥25° are associated with a high risk of developing immediate postoperative coronal imbalance. During the postoperative follow-up, UIV tilt may play a very important role in compensating for postoperative coronal imbalance.
Acknowledgments
This work was supported by the National Public Health Benefit Research Foundation, China (Grant No. 201002018).
Conflict of interest
No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Footnotes
Z. Liu and J. Guo contributed equally to the study.
References
- 1.Remes V, Helenius I, Schlenzka D, Yrjonen T, Ylikoski M, Poussa M. Cotrel-Dubousset (CD) or Universal Spine System (USS) instrumentation in adolescent idiopathic scoliosis (AIS): comparison of midterm clinical, functional, and radiologic outcomes. Spine (Phila Pa 1976) 2004;29:2024–2030. doi: 10.1097/01.brs.0000138408.64907.dc. [DOI] [PubMed] [Google Scholar]
- 2.Suk SI, Lee SM, Chung ER, Kim JH, Kim SS. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year follow-up. Spine (Phila Pa 1976) 2005;30:1602–1609. doi: 10.1097/01.brs.0000169452.50705.61. [DOI] [PubMed] [Google Scholar]
- 3.Fischer CR, Kim Y. Selective fusion for adolescent idiopathic scoliosis: a review of current operative strategy. Eur Spine J. 2011;20:1048–1057. doi: 10.1007/s00586-011-1730-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhao Y, Wang Z, Zhu X, Wang C, He S, Li M. Prediction of postoperative trunk imbalance after posterior spinal fusion with pedicle screw fixation for adolescent idiopathic scoliosis. J Pediatr Orthop B. 2011;20:199–208. doi: 10.1097/BPB.0b013e328344e727. [DOI] [PubMed] [Google Scholar]
- 5.Dobbs MB, Lenke LG, Walton T, Peelle M, Della Rocca G, Steger-May K, Bridwell KH. Can we predict the ultimate lumbar curve in adolescent idiopathic scoliosis patients undergoing a selective fusion with undercorrection of the thoracic curve? Spine (Phila Pa 1976) 2004;29:277–285. doi: 10.1097/01.BRS.0000106488.51299.75. [DOI] [PubMed] [Google Scholar]
- 6.Richards BS, Scaduto A, Vanderhave K, Browne R. Assessment of trunk balance in thoracic scoliosis. Spine (Phila Pa 1976) 2005;30:1621–1626. doi: 10.1097/01.brs.0000170298.89145.b4. [DOI] [PubMed] [Google Scholar]
- 7.Ni HJ, Su JC, Lu YH, Zhu XD, He SS, Wu DJ, Xu J, Yang CW, Wang CF, Zhao YC, Li M. Using side-bending radiographs to determine the distal fusion level in patients with single thoracic idiopathic scoliosis undergoing posterior correction with pedicle screws. J Spinal Disord Tech. 2011;24:437–443. doi: 10.1097/BSD.0b013e31820500c9. [DOI] [PubMed] [Google Scholar]
- 8.Lee CS, Chung SS, Shin SK, Park YS, Park SJ, Kang KC. Changes of upper thoracic curve and shoulder balance in thoracic adolescent idiopathic scoliosis treated by anterior selective thoracic fusion using VATS. J Spinal Disord Tech. 2011;24:462–468. doi: 10.1097/BSD.0b013e318204d553. [DOI] [PubMed] [Google Scholar]
- 9.Li J, Hwang SW, Shi Z, Yan N, Yang C, Wang C, Zhu X, Hou T, Li M. Analysis of radiographic parameters relevant to the lowest instrumented vertebrae and postoperative coronal balance in Lenke 5C patients. Spine (Phila Pa 1976) 2011;36:1673–1678. doi: 10.1097/BRS.0b013e3182091fba. [DOI] [PubMed] [Google Scholar]
- 10.Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, Blanke K. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83-A:1169–1181. [PubMed] [Google Scholar]
- 11.Lenke LG, Edwards CC, 2nd, Bridwell KH. The Lenke classification of adolescent idiopathic scoliosis: how it organizes curve patterns as a template to perform selective fusions of the spine. Spine (Phila Pa 1976) 2003;28:S199–S207. doi: 10.1097/01.BRS.0000092216.16155.33. [DOI] [PubMed] [Google Scholar]
- 12.Cobb J. Outline for the study of scoliosis. Instr Course Lect. 1948;5:261–275. [Google Scholar]
- 13.Nash CL, Jr, Moe JH. A study of vertebral rotation. J Bone Joint Surg Am. 1969;51:223–229. [PubMed] [Google Scholar]
- 14.Puno RM, An KC, Puno RL, Jacob A, Chung SS. Treatment recommendations for idiopathic scoliosis: an assessment of the Lenke classification. Spine (Phila Pa 1976) 2003;28:2102–2114. doi: 10.1097/01.BRS.0000088480.08179.35. [DOI] [PubMed] [Google Scholar]
- 15.Satake K, Lenke LG, Kim YJ, Bridwell KH, Blanke KM, Sides B, Steger-May K. Analysis of the lowest instrumented vertebra following anterior spinal fusion of thoracolumbar/lumbar adolescent idiopathic scoliosis: can we predict postoperative disc wedging? Spine (Phila Pa 1976) 2005;30:418–426. doi: 10.1097/01.brs.0000153342.89478.d2. [DOI] [PubMed] [Google Scholar]
- 16.Suk SI, Lee SM, Chung ER, Kim JH, Kim WJ, Sohn HM. Determination of distal fusion level with segmental pedicle screw fixation in single thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 2003;28:484–491. doi: 10.1097/01.BRS.0000048653.75549.40. [DOI] [PubMed] [Google Scholar]
- 17.Behensky H, Cole AA, Freeman BJ, Grevitt MP, Mehdian HS, Webb JK. Fixed lumbar apical vertebral rotation predicts spinal decompensation in Lenke type 3C adolescent idiopathic scoliosis after selective posterior thoracic correction and fusion. Eur Spine J. 2007;16:1570–1578. doi: 10.1007/s00586-007-0397-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shufflebarger HL, Geck MJ, Clark CE. The posterior approach for lumbar and thoracolumbar adolescent idiopathic scoliosis: posterior shortening and pedicle screws. Spine (Phila Pa 1976) 2004;29:269–276. doi: 10.1097/01.BRS.0000109881.63411.48. [DOI] [PubMed] [Google Scholar]
- 19.Geck MJ, Rinella A, Hawthorne D, Macagno A, Koester L, Sides B, Bridwell K, Lenke L, Shufflebarger H. Comparison of surgical treatment in Lenke 5C adolescent idiopathic scoliosis: anterior dual rod versus posterior pedicle fixation surgery: a comparison of two practices. Spine (Phila Pa 1976) 2009;34:1942–1951. doi: 10.1097/BRS.0b013e3181a3c777. [DOI] [PubMed] [Google Scholar]