Abstract
Purpose
Computed tomography can be used for three-dimensional (3D) evaluation of adolescent idiopathic scoliosis (AIS) patients, but at the expense of high radiation exposure, and with the limitation of being performed in the supine position. These drawbacks can now be avoided with low-dose stereoradiography, even in routine clinical use. The purpose of this study was to determine the 3D postoperative correction of AIS patients treated by posteromedial translation.
Methods
Forty-nine consecutive patients operated for AIS (Lenke 1–4) using posteromedial translation were included. Corrections were evaluated preoperatively, postoperatively and after at least 2 years using the EOS imaging system. 3D angles were measured in the plane of maximum deformity.
Results
Mean number of levels fused and operative time were 13.5 ± 1 and 215 ± 25 min, respectively. Main thoracic, proximal thoracic, and lumbar curves corrections averaged 64.4 ± 18, 31 ± 10 and 69 ± 20 %, respectively. Mean T4–T12 kyphosis increased 18.8° ± 9° in the subgroup of hypokyphotic patients. Mean apical vertebral rotation reduction was 48.3 ± 20 %. Trunk height gain averaged 27.8 ± 14 mm. There was no pseudarthrosis or significant loss of correction in any plane during follow-up. Two patients (4 %) developed asymptomatic proximal junctional kyphosis, despite having normal thoracic kyphosis. Their sagittal balance was shifted posteriorly by 36 and 47 mm, respectively, by the operation, but revision surgery was not performed.
Conclusions
Low-dose stereoradiography provided 3D reconstructions of the fused and unfused spine in routine clinical use. Postoperative 3D analysis showed that posteromedial translation enhanced sagittal balance correction, without sacrificing frontal or axial correction of the deformity.
Keywords: Adolescent idiopathic scoliosis, Hybrid constructs, Three-dimensional, Universal clamp, Posteromedial translation
Introduction
Correcting the spine in the frontal plane while achieving or maintaining physiological sagittal curves is now one of the most challenging goals in adolescent idiopathic scoliosis (AIS) surgery [1–4]. As emphasized by Imrie et al. [5], the development and application of powerful pedicle screw instrumentation constructs has sometimes led to great coronal correction, but at the expense of sagittal alignment. The difficulty of restoring adequate thoracic kyphosis, observed in AIS patients treated by selective posterior thoracic fusion, has also been pointed out when direct vertebral derotation is used for correction in all-pedicle screw constructs [6, 7]. Hybrid constructs that depend on posteromedial translation for spinal correction have demonstrated very satisfying results in both the frontal and sagittal planes, but their efficacy in the axial plane has never been assessed in three dimensions (3D) [8, 9].
The clinical relevance and impact of 3D analysis on scoliotic deformities has recently been pointed out by the Scoliosis Research Society (SRS), which is currently in the process of developing a 3D classification of AIS [10]. Indeed, significant correlations between 3D parameters of deformities and clinical outcomes have been reported [11]. Computer scanning can be used for this type of analysis, but at the expense of high radiation exposure, and with the limitation of being performed in the supine position. These drawbacks can now be avoided by the use of low-dose stereoradiography in standing AIS patients to obtain 3D reconstructions, the validity of which in routine preoperative and postoperative use has been recently confirmed [12]. Therefore, in surgical units that dispose of this imaging system, the efficacy of AIS treatment procedures can now be accurately measured in all three planes, routinely, without a trade-off in safety [13]. The long-term risks posed by former methods of 3D imaging probably account for the paucity of literature reports to date evaluating postoperative results of AIS. Routine clinical use of this new low dose imaging system at the authors’ institution permitted the present study, the purpose of which was to determine the 3D postoperative correction in a cohort of AIS patients treated by posteromedial translation.
Materials and methods
Patients
Following institutional review board approval, 49 consecutive patients operated for AIS (Lenke 1–4) were prospectively included. A minimum 2-year follow-up was required. All patients were evaluated preoperatively, in the early postoperative period (within 3 months), and at last follow-up. None of the patients had prior spinal surgery.
Operative procedure
All patients underwent posterior spinal fusion and instrumentation using hybrid constructs that included Universal Clamps (UC) (Zimmer Spine, Bordeaux, France) in the thoracic spine, lumbar pedicle screws (Java, Zimmer Spine, Bordeaux, France), and hooks at the upper thoracic spine (Zimmer Spine, Bordeaux, France or Medtronic, Minneapolis, MN, USA) (Fig. 1). Fusion levels were selected following the same criteria during the entire study period, and 5.5 titanium alloy rods were used in all cases [14, 15]. The two rods were contoured to the desired sagittal profile and connected with two transverse connectors before placement. The rods were first introduced in the pedicle screws, and lumbar correction was performed. Posteromedial translation was the primary technique used for thoracic correction, while in situ contouring, compression and/or distraction were also performed as needed to improve levelling of the uninstrumented spine both proximal and distal to the fusion construct [8, 9, 14, 15]. No patient underwent anterior release before posterior correction and fusion. During all 49 procedures, spinal cord function was monitored by means of somatosensory/motor-evoked potentials.
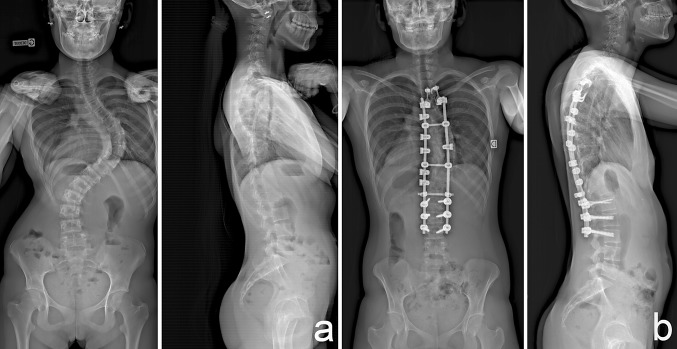
Fig. 1.
Preoperative (a) and postoperative (b) radiographs of a 15-year-old patient operated for a right thoracic curve using posteromedial translation
Biplanar radiographic system
Low dose biplanar radiographs (EOS imaging, Paris, France) were obtained preoperatively, postoperatively and at the latest patient visit as part of the routine work-up and follow-up [12]. Patients were in the weight-bearing standing position, arms folded at 45° in order to avoid superposition with the spine. All images included the base of the skull and the upper third of the femurs.
The EOS system is a slot-scanning radiologic device consisting of two X-ray sources, allowing simultaneous acquisition of orthogonal images [13]. The sources are coupled to linear detectors that are based upon micromesh gaseous structure technology [16]. The two source detector pairs are positioned orthogonally, so the patient’s anteroposterior and lateral images are generated line-by-line while the whole system is vertically translated. Scan time lasts from 8 to 15 s for a spine examination, depending on the patient’s height. Entrance surface doses were recorded for all acquisitions, and then converted into effective doses for each organ using the dedicated weighting factors reported by Hart et al. [17].
Reconstruction process
As previously described, full 3D images of the spine were reconstructed by an independent senior radiologist, experienced with the method (total 147 reconstructions) [12, 18, 19]. The preliminary step was the identification of a segment on the sacral endplate and two spheres around the femoral heads in the acetabuli, which permitted the creation of a ‘patient frame’ that is compatible with the reference axis used by the SRS for classification of AIS [20]. The spinal curve, the T1 upper endplate and the L5 lower endplate were then digitalized, and used as predictors to statistically estimate the other descriptors of the parametric spine. A highly detailed 3D model was generated then projected on both X-rays so that the operator could verify and, if necessary, perform fine adjustments of the position and shape of each reconstructed vertebra (T1–L5).
3D parameters
The following clinical measurements were calculated from the reconstructions: T4/T12 kyphosis, L1/L5 and L1/S1 lordoses, Cobb’s angle of the different curves, axial vertebral rotation of the apical vertebra (AVR), pelvic incidence, pelvic tilt, and sacral slope. All measurements were 3D angles. Vertebral axial rotations were calculated as recommended by the SRS 3-D Committee [21]. From the 3D reconstructions, a local frame was automatically calculated and attached to each vertebra. Rotations were measured as the axial rotation of the local vertebral coordinate system, in relation to the global body coordinate system [22].
In addition, the torsion index of the main thoracic curve (sum of the axial vertebral rotations of the curve), the iliolumbar angle (angle between the upper endplate of L4 and a line joining the sacroiliac joints), and the residual frontal and axial tilts of the lowest instrumented vertebra (LIV) were reported.
As recommended by the SRS 3D committee, the central hip vertical axis (CHVA) was used as the reference axis to evaluate patients’ balance [20]. Sagittal and frontal alignments were determined by measuring the distances between the projection of the center of T1 on the different axes (x and y, respectively) and the CHVA (positive value in case of anterior shift). Trunk height gain was estimated by comparing the postoperative and preoperative projections of the center of T1 on the CHVA (z coordinate). The distances between the projection of the center of each vertebra on the different axis and the CHVA were also calculated, and used if necessary to represent vertebral vectors as described by Illes et al. [23].
Statistical analysis
Two-tail paired t tests were used to compare preoperative and postoperative measurements. A p value < 0.05 was considered to be significant. All statistical analyses were conducted using the software Statview (SAS Institute Inc, Cary, NC, USA).
Results
Demographic data and operative procedures
There were 45 girls and 4 boys (average age, 15 years; range 13–17), with 17 Lenke 1 curves, 9 Lenke 2, 15 Lenke 3, and 8 Lenke 4. Mean follow-up was 34 ± 6 months. The mean number of levels fused was 13.5 ± 1 (11–15). The number of UCs used for thoracic correction averaged 6.8 (5–10). The apical vertebra was instrumented with two UCs in all cases. The average operative time was 215 ± 25 min. No intraoperative complication was reported. In particular, no significant change in the monitored somatosensory/motor-evoked potentials was recorded during insertion of the sublaminar bands.
Analysis of 3D reconstructions
Dose radiation
According to the average weighting factors reported by Abul-Kasim et al. [24], the mean calculated entrance surface doses obtained with EOS were 0.18 (±0.05) mGy for the frontal view and 0.30 (± 0.07) mGy for the lateral view, thus corresponding to an effective dose of 0.06 mSv.
Spinal parameters
Reconstruction time averaged 12 ± 0.8 min. The anatomic landmarks were clearly distinguishable by varying the luminosity and contrast to optimally reveal the vertebrae and pelvis. In particular, the superior endplate of T1 and the femoral heads were visible in all cases.
Corrections obtained in the frontal and axial planes, calculated in the plane of maximum deformity, are reported in Table 1. All parameters improved significantly, and no significant loss of correction was observed between early postoperative and latest follow-up.
Table 1.
Corrections in the coronal and axial planes obtained from 3D reconstructions
| Preop | Postop | Follow-up | Final correction (%) | p | |
|---|---|---|---|---|---|
| Main thoracic curve | 61.2° ± 13° | 19.5° ± 10° | 22° ± 10° | 64.4 ± 18 | <0.0001 |
| Apical vertebral rotation | 19.9° ± 7° | 11° ± 6° | 10.2° ± 5° | 48.3 ± 20 | <0.0001 |
| Torsion index | 15.8 ± 6 | 8.5 ± 6 | 8.6 ± 5 | 44 ± 30 | <0.0001 |
| Proximal thoracic curve | 30° ± 11° | 19° ± 9° | 20° ± 7° | 31 ± 10 | <0.0001 |
| Distal lumbar curve | 42° ± 11° | 11° ± 6° | 13° ± 7° | 69 ± 20 | <0.0001 |
| Iliolumbar angle | 11.2° ± 8° | 3.8° ± 3° | 4.2° ± 3° | 56 ± 30 | <0.0001 |
Values are presented with standard deviation
p values are given for the differences between preoperative and final values
Sagittal parameters obtained from 3D reconstructions are reported in Table 2. Twenty-nine patients (59 %) were hypokyphotic preoperatively (i.e., <20°). In these 29 patients, thoracic kyphosis significantly increased after the procedure (average 18.8° ± 9°), without loss of correction during follow-up, and 94 % of the cohort had normal thoracic kyphosis (i.e., 20°–40°) at latest examination (Fig. 2). None of the patients had <10° of thoracic kyphosis at follow-up.
Table 2.
Sagittal parameters obtained from 3D reconstructions
| Preop | Postop | Follow-up | p | |
|---|---|---|---|---|
| T4–T12 kyphosis | 18° ± 13° | 28° ± 8° | 32.4° ± 9° | <0.0001 |
| L1–L5 lordosis | 47.7° ± 7° | 48.2° ± 9° | 48.7° ± 11° | 0.15 |
| L1–S1 lordosis | 53.7° ± 14° | 54.3° ± 10° | 56° ± 12° | 0.12 |
| Lordosis of the instrumented spine | 16.5° ± 10° | 18° ± 12° |
Values are presented with standard deviation
p values are given for the differences between preoperative and final values
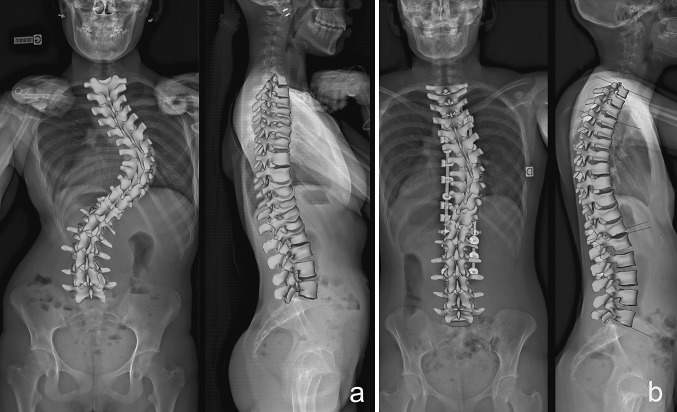
Fig. 2.
Preoperative (a) and postoperative (b) 3D reconstructions of a 15-year-old patient operated for a right thoracic curve using posteromedial translation. The reduction technique was efficient to correct the thoracic hypokyphosis
The frontal residual tilt of the LIV averaged 3.7° ± 2° at follow-up. A residual tilt >5°, thus exceeding the preoperative goal, was observed in nine patients (18 %), but no revision surgery was performed for loss of frontal balance or residual progressive deformity of the unfused spine. Mean axial rotation of the LIV was 3.6° ± 2.5° postoperatively, and was under 5° in 79.5 % of the patients at latest follow-up.
Spinal balance
Modifications of the position of the center of T1, with regard to the CHVA, are summarized in Table 3. No significant change was observed between the early postoperative period and latest examination. Ninety percent of the patients were posteriorly balanced preoperatively, and the sagittal balance of the spine was not significantly modified after the surgical procedure (average 6.3 ± 21 mm). The frontal balance was significantly improved, with 94 % of the cohort being balanced (i.e., <20 mm) at latest follow-up. Trunk height gain averaged 27.8 ± 14 mm.
Table 3.
Position of the center of T1 with regard to the central hip vertical axis
| Preop (mm) | Follow-up (mm) | p | |
|---|---|---|---|
| Sagittal balance (projection on the x axis) | −28 ± 25 | −34 ± 21 | 0.07 |
| Frontal balance (projection on the y axis) | 16 ± 12 | 11 ± 8 | 0.04 |
| Height (projection on the z axis) | 475 ± 30 | 504 ± 27 | <0.0001 |
Values are presented with standard deviation
Pelvic parameters
Measures of pelvic parameters obtained from 3D reconstructions are reported in Table 4. None was significantly modified postoperatively.
Table 4.
Pelvic parameters measurements
| Preop | Follow-up | p | |
|---|---|---|---|
| Pelvic incidence | 54.3° ± 14° | 54.1° ± 13° | 0.81 |
| Sacral slope | 43.3° ± 10° | 43° ± 10° | 0.76 |
| Pelvic tilt | 11° ± 7° | 11.1° ± 8° | 0.99 |
| Pelvic axial rotation | 3.4° ± 3° | 2.3° ± 4° | 0.12 |
Values are presented with standard deviation
Complications
No neurological complication occurred during or after the procedures. No pseudarthrosis or significant loss of correction was reported during follow-up. One patient underwent early revision (1 month postoperative), for mobilization of a proximal supralaminar hook. Two patients (4 %) developed asymptomatic proximal junctional kyphosis (PJK), despite having normal thoracic kyphosis. Their sagittal balance was shifted posteriorly by 36 and 47 mm, respectively, by the operation, but revision surgery was not performed.
Discussion
Low dose biplanar stereoradiography
The limitation of 2D radiological measurements and the clinical usefulness of measurements obtained from 3D reconstruction have been recently emphasized by the SRS “3D Scoliosis Committee” [10, 11, 20, 25]. Preliminary 3D assessment of intervertebral deviation has already been performed by Hattori et al. [26] using bone models, but stereoradiography allows a routine clinical use. The images of scoliosis patients in the standing position, provided by the new EOS imaging device and its 3D reconstruction software (SterEOS, EOS imaging, Paris, France), contribute substantially to understanding of both preoperative scoliotic deformities and postoperative correction. The method does not require additional examination to assess the axial plane, and vertebral axial rotations, in particular, can be assessed accurately in routine pre- and postoperative clinical use with greatly reduced exposure to ionizing radiation [12]. As a matter of fact, the mean effective dose calculated in the current study was 6 times lower than the one reported by Abul-Kasim [24, 27] with low-dose CT. The device is expensive, but the cost of an examination remains the same as the one of a conventional full spine radiograph in our institution.
Illes et al. [23] have also recently described potential advantages of viewing the spine from above and introduced the concept of vertebra vectors .These vectors furnish the surgeon easy-to-understand interpretation of the deformity, reflecting the distance of each vertebra from the CHVA and the orientation of the axis of each vertebral body in the horizontal plane (Figs. 3 and 4). In addition, postoperative 3D reconstructions provide accurate measurements of residual axial and frontal tilts of the LIV, essential when evaluating the long-term outcome of the unfused spinal segments and risk of “adding-on” surgery [28]. Eventhough radiation dose is a major concern for pediatric patients who require repeated imaging, recent studies have emphasized that no patient health outcomes has ever been reported to date in the literature, and that further clinical studies are required to investigate the long-term benefits of EOS on patient management [29–31].
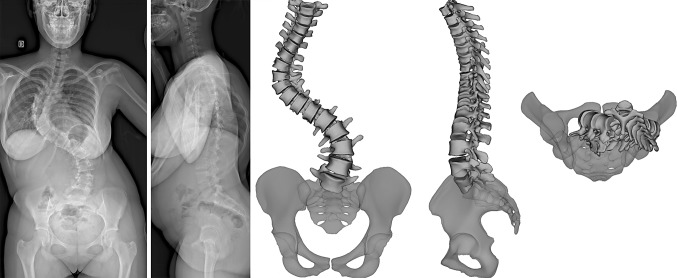
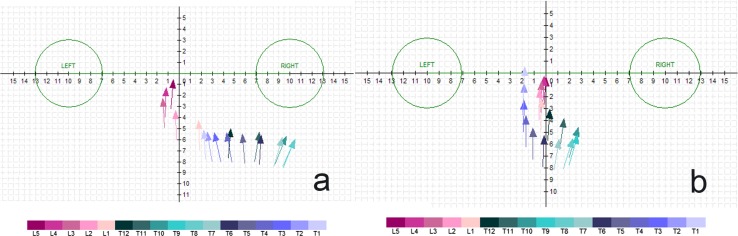
Fig. 3.
Preoperative stereoradiographs and 3D reconstructions of a 14-year-old patient. The “top view” provides helpful information to the clinician regarding the axial component deformity and global postural balance
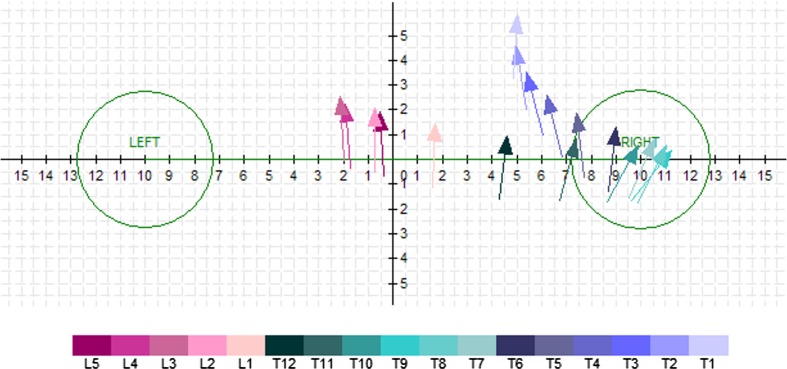
Fig. 4.
Representation of the same deformity (Fig. 2) using the vertebra vectors method. The position of the vector reflects the distance of each vertebra with regard to the central hip vertical axis, while its orientation represents the axis of each vertebral body in the horizontal plane
Postoperative analysis of the correction
Results of the current study confirm that posteromedial translation, performed with UCs, is an effective correction technique for AIS. Ranging from 35 to 98 %, the frontal correction rates were consistent with previous reports about sublaminar bands, and with previous 2D postoperative analysis after Luque or hybrid instrumentations [8, 9, 14, 32, 33]. Delorme et al. [34] had already investigated the 3D postoperative change of the spinal shape in patients treated with the Colorado system, with correction rates consistent with the ones reported in the current study, but the follow-up was very short (1 month), and the assessment did not use the low-dose stereoradiography. However, we share the concern of Winter et al. [4] that there is an overemphasis in recent publications on achieving a few supplemental degrees of coronal reduction, and feel that it is more important to obtain a balanced fusion. This goal was properly achieved with respect to the CHVA in 94 % of the present patients. One must note that the number of levels fused in the current study (13.5 ± 1) was relatively high, but this can be explained by (1) the high percentage of patients (47 %) having structural lumbar curves, and (2) the fact that according to our general fusion criteria, no matter the construct selected, the arthrodesis never ended above L2 distally, in order to avoid distal junctional kyphosis, and therefore selective fusions were rarely performed.
The current study provides the first reliable values of the rotational correction achieved with UCs. Surprisingly, the torsion index reduction reached 44 %, and the apical vertebral rotation correction averaged 48.3 %, approaching the rates reported in the literature obtained using direct vertebral rotation (DVR) (42.5–64 %) [35–37] while obviating potential risks associated with DVR [38]. The unexpectedly high apical vertebral rotational reduction observed in the present patients might be explained by the fact that the corrective maneuver was mediated simultaneously by both rods, preassembled using fixed transverse connectors (Fig. 5). During the correction, the spine was pulled posteriorly using the sublaminar bands on the concave rod, but the convex rod also pushed the lamina on the convex side, thus creating a “detorsion effect” on the instrumented spine. These modifications of the vertebral body axes of the segments included in the curve are more clearly revealed with modelized vertebral vectors (Fig. 6).
Fig. 5.
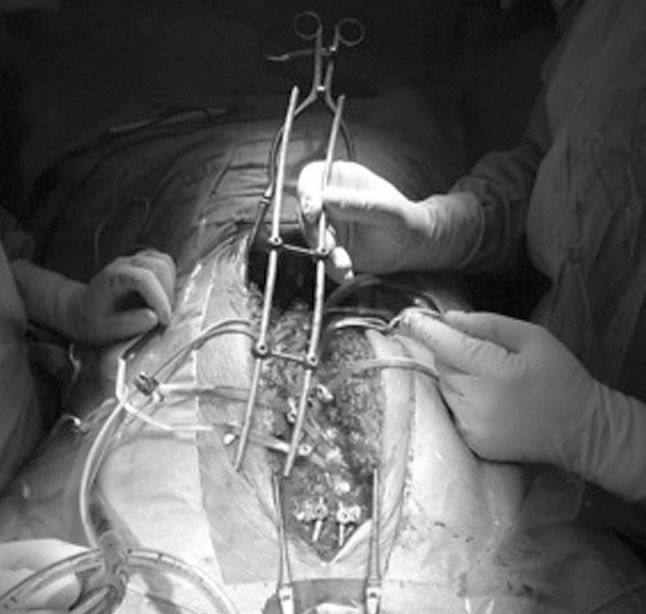
Intraoperative view of the frame created before reduction, using two 5.5 rods connected by two closed connectors. Rods are precontoured in the sagittal plane before insertion in the pedicle screws
Fig. 6.
Preoperative (a) and postoperative (b) representations, using the vectors method, of a thoracic deformity in a 16-year-old girl treated by posteromedial translation
Restoring the sagittal balance of the spine remains one of the most challenging goals in scoliosis surgery, and undercorrection of thoracic kyphosis has been associated with an increased risk of PJK [3]. In the current series, UCs improved the thoracic kyphosis, regardless of the preoperative sagittal modifier, confirming that hybrid constructs can enhance sagittal correction [3, 9, 39–41]. Only 3 (6 %) patients remained hypokyphotic at latest follow-up, with a mean T4–T12 kyphosis improvement of 14.3° ± 10°, and a low incidence of PJK (4 %) was observed. These results confirm that posteromedial translation effectively corrects sagittal alignment instead of worsening it, as has been observed in studies of direct vertebral body derotation [1, 6].
CHVA and spinal balance
The main parameters of spino-pelvic sagittal alignment (pelvic incidence, lumbar lordosis, and thoracic kyphosis) measured on our 3D reconstructions were comparable to the same parameters measured on 2D standing radiographs, reported in a series of 160 AIS patients [42].
As recommended by the SRS “3D Scoliosis Committee”, the CHVA was used as a reference axis in the current series [20]. More reproducible than the center sacral vertical line, the CHVA represents the physiologic center of balance of the spino-pelvic unit because it takes into account femoral head support. It was easily computed on the present 3D reconstructions from low dose biplanar radiographs, and was used for spinal balance analysis. Mac Thiong et al. [43] reported that the C7 plumbline of most pediatric patients lies behind the hip axis on standing radiographs, but that the C7 plumbline lies in front of both hip axis and sacrum in 12 % of normal subjects between 10 and 18 years of age. Results of the current 3D analysis confirm that tendency in AIS patients, with 90 % of the subjects posteriorly balanced preoperatively with regard to the CHVA. The global sagittal balance of the spine was not modified after the correction, but in the two patients who developed PJK, sagittal balance was significantly shifted posteriorly after the procedure even though they had normal values of thoracic kyphosis. This suggests that postoperative change in thoracic kyphosis might not be the most important risk factor for PJK, and that the influence of postoperative modifications in sagittal balance with regard to the CHVA warrant further study in 3D [3].
Limitations of the study
There are several weaknesses in this study. No control group was used, and the corrections obtained with posteromedial translation will need to be compared in the future to other reduction techniques assessed with low dose stereoradiography. Although the follow-up period was short (34 months) in the UC group, it is now accepted that loss of correction after fusion in AIS primarily occurs during the first postoperative year and that results of spine surgery can be reliably evaluated radiologically after a minimum follow-up of 2 years [44]. However, the long-term outcomes of patients with PJK or a residual frontal tilt of the LIV >5° would merit further investigation. The measurements obtained with the EOS system were not compared to another imaging method, since the purpose of the study was not to evaluate the reliability of stereoradiography, which has already been reported previously in AIS [12]. Finally, this was a purely radiological study, no functional score being used to evaluate the clinical outcome of these patients.
In conclusion, routine clinical use of the EOS imaging system safely provided 3D reconstructions, which reliably demonstrated for the first time that posteromedial translation could enhance sagittal balance correction without sacrificing either frontal or axial correction of AIS. Radiological outcome in all planes was maintained at more than two and a half years, but needs to be confirmed at longer follow-up and correlated with functional scores.
Conflict of interest
None.
References
- 1.Hwang SW, Samdani AF, Gressot LV, Hubler K, Marks MC, Bastrom TP, Betz RR, Cahill PJ. Effect of direct vertebral body derotation on the sagittal profile in adolescent idiopathic scoliosis. Eur Spine J. 2012;21:31–39. doi: 10.1007/s00586-011-1991-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hwang SW, Samdani AF, Tantorski M, Cahill P, Nydick J, Fine A, Betz RR, Antonacci MD. Cervical sagittal plane decompensation after surgery for adolescent idiopathic scoliosis: an effect imparted by postoperative thoracic hypokyphosis. J Neurosurg Spine. 2011;15:491–496. doi: 10.3171/2011.6.SPINE1012. [DOI] [PubMed] [Google Scholar]
- 3.Kim YJ, Lenke LG, Bridwell KH, Kim J, Cho SK, Cheh G, Yoon J. Proximal junctional kyphosis in adolescent idiopathic scoliosis after 3 different types of posterior segmental spinal instrumentation and fusions: incidence and risk factor analysis of 410 cases. Spine. 2007;32:2731–2738. doi: 10.1097/BRS.0b013e31815a7ead. [DOI] [PubMed] [Google Scholar]
- 4.Winter RB, Lonstein JE, Denis F. How much correction is enough? Spine. 2007;32:2641–2643. doi: 10.1097/BRS.0b013e31815a5207. [DOI] [PubMed] [Google Scholar]
- 5.Imrie M, Yaszay B, Bastrom TP, Wenger DR, Newton PO. Adolescent idiopathic scoliosis: should 100% correction be the goal? J Pediatr Orthop. 2011;31:S9–S13. doi: 10.1097/BPO.0b013e3181fd8a24. [DOI] [PubMed] [Google Scholar]
- 6.Mladenov KV, Vaeterlein C, Stuecker R. Selective posterior thoracic fusion by means of direct vertebral derotation in adolescent idiopathic scoliosis: effects on the sagittal alignment. Eur Spine J. 2011;20:1114–1117. doi: 10.1007/s00586-011-1740-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmidt C, Liljenqvist U, Lerner T, Schulte TL, Bullmann V. Sagittal balance of thoracic lordoscoliosis: anterior dual rod instrumentation versus posterior pedicle screw fixation. Eur Spine J. 2011;20:1118–1126. doi: 10.1007/s00586-011-1784-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mazda K, Ilharreborde B, Even J, Lefevre Y, Fitoussi F, Pennecot GF. Efficacy and safety of posteromedial translation for correction of thoracic curves in adolescent idiopathic scoliosis using a new connection to the spine: the universal clamp. Eur Spine J. 2009;18:158–169. doi: 10.1007/s00586-008-0839-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sales de Gauzy J, Jouve JL, Accabled F, Blondel B, Bollini G. Use of the Universal Clamp in adolescent idiopathic scoliosis for deformity correction and as an adjunct to fusion: 2-year follow-up. J Child Orthop. 2011;5:273–282. doi: 10.1007/s11832-011-0357-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Labelle H, Aubin CE, Jackson R, Lenke L, Newton P, Parent S. Seeing the spine in 3D: how will it change what we do? J Pediatr Orthop. 2011;31:S37–S45. doi: 10.1097/BPO.0b013e3181fd8801. [DOI] [PubMed] [Google Scholar]
- 11.Hong JY, Suh SW, Easwar TR, Modi HN, Yang JH, Park JH. Evaluation of the three-dimensional deformities in scoliosis surgery with computed tomography: efficacy and relationship with clinical outcomes. Spine (Phila Pa 1976) 2011;36:E1259–E1265. doi: 10.1097/BRS.0b013e318205e413. [DOI] [PubMed] [Google Scholar]
- 12.Ilharreborde B, Steffen JS, Nectoux E, Vital JM, Mazda K, Skalli W, Obeid I. Angle measurement reproducibility using EOS three-dimensional reconstructions in adolescent idiopathic scoliosis treated by posterior instrumentation. Spine (Phila Pa 1976) 2011;36:E1306–E1313. doi: 10.1097/BRS.0b013e3182293548. [DOI] [PubMed] [Google Scholar]
- 13.Deschenes S, Charron G, Beaudoin G, Labelle H, Dubois J, Miron MC, Parent S. Diagnostic imaging of spinal deformities: reducing patients radiation dose with a new slot-scanning X-ray imager. Spine (Phila Pa 1976) 2010;35:989–994. doi: 10.1097/BRS.0b013e3181bdcaa4. [DOI] [PubMed] [Google Scholar]
- 14.Ilharreborde B, Even J, Lefevre Y, Fitoussi F, Presedo A, Pennecot GF, Mazda K. Hybrid constructs for tridimensional correction of the thoracic spine in adolescent idiopathic scoliosis: a comparative analysis of Universal Clamps versus hooks. Spine (Phila Pa 1976) 2010;35:306–314. doi: 10.1097/BRS.0b013e3181b7c7c4. [DOI] [PubMed] [Google Scholar]
- 15.Ilharreborde B, Even J, Lefevre Y, Fitoussi F, Presedo A, Souchet P, Pennecot GF, Mazda K. How to determine the upper level of instrumentation in Lenke types 1 and 2 adolescent idiopathic scoliosis: a prospective study of 132 patients. J Pediatr Orthop. 2008;28:733–739. doi: 10.1097/BPO.0b013e318185a36b. [DOI] [PubMed] [Google Scholar]
- 16.Despres P, Beaudoin G, Gravel P, de Guise JA. Physical characteristics of a low-dose gas microstrip detector for orthopedic X-ray imaging. Med Phys. 2005;32:1193–1204. doi: 10.1118/1.1876592. [DOI] [PubMed] [Google Scholar]
- 17.Hart D, Jones DG, Wall BF, Board GBNRP. Coefficients for estimating effective doses from paediatric x-ray examinations, Report National Radiology Protection on Board-R279. London: HMSO; 1996. [Google Scholar]
- 18.Humbert L, De Guise JA, Aubert B, Godbout B, Skalli W. 3D reconstruction of the spine from biplanar X-rays using parametric models based on transversal and longitudinal inferences. Med Eng Phys. 2009;31:681–687. doi: 10.1016/j.medengphy.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 19.Pomero V, Mitton D, Laporte S, de Guise JA, Skalli W. Fast accurate stereoradiographic 3D-reconstruction of the spine using a combined geometric and statistic model. Clin Biomech (Bristol, Avon) . 2004;19:240–247. doi: 10.1016/j.clinbiomech.2003.11.014. [DOI] [PubMed] [Google Scholar]
- 20.Sangole A, Aubin CE, Labelle H, Lenke L, Jackson R, Newton P, Stokes IA. The central hip vertical axis: a reference axis for the scoliosis research society three-dimensional classification of idiopathic scoliosis. Spine (Phila Pa 1976) 2010;35:E530–E534. doi: 10.1097/BRS.0b013e3181cc39cb. [DOI] [PubMed] [Google Scholar]
- 21.Stokes IA. Three-dimensional terminology of spinal deformity. A report presented to the Scoliosis Research Society by the Scoliosis Research Society Working Group on 3-D terminology of spinal deformity. Spine (Phila Pa 1976) 1994;19:236–248. doi: 10.1097/00007632-199401001-00020. [DOI] [PubMed] [Google Scholar]
- 22.Skalli W, Lavaste F, Descrimes JL. Quantification of three-dimensional vertebral rotations in scoliosis: what are the true values? Spine (Phila Pa 1976) 1995;20:546–553. doi: 10.1097/00007632-199503010-00008. [DOI] [PubMed] [Google Scholar]
- 23.Illes T, Tunyogi-Csapo M, Somoskeoy S. Breakthrough in three-dimensional scoliosis diagnosis: significance of horizontal plane view and vertebra vectors. Eur Spine J. 2011;20:135–143. doi: 10.1007/s00586-010-1566-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abul-Kasim K, Overgaard A, Maly P, Ohlin A, Gunnarsson M, Sundgren PC. Low-dose helical computed tomography (CT) in the perioperative workup of adolescent idiopathic scoliosis. Eur Radiol. 2009;19:610–618. doi: 10.1007/s00330-008-1178-4. [DOI] [PubMed] [Google Scholar]
- 25.Kadoury S, Labelle H. Classification of three-dimensional thoracic deformities in adolescent idiopathic scoliosis from a multivariate analysis. Eur Spine J. 2012;21:40–49. doi: 10.1007/s00586-011-2004-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hattori T, Sakaura H, Iwasaki M, Nagamoto Y, Yoshikawa H, Sugamoto K. In vivo three-dimensional segmental analysis of adolescent idiopathic scoliosis. Eur Spine J. 2011;20:1745–1750. doi: 10.1007/s00586-011-1869-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abul-Kasim K, Ohlin A, Strombeck A, Maly P, Sundgren PC. Radiological and clinical outcome of screw placement in adolescent idiopathic scoliosis: evaluation with low-dose computed tomography. Eur Spine J. 2010;19:96–104. doi: 10.1007/s00586-009-1203-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang Y, Hansen ES, Hoy K, Wu C, Bunger CE. Distal adding-on phenomenon in Lenke 1A scoliosis: risk factor identification and treatment strategy comparison. Spine (Phila Pa 1976) 2011;36:1113–1122. doi: 10.1097/BRS.0b013e3181f51e95. [DOI] [PubMed] [Google Scholar]
- 29.Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, Howe NL, Ronckers CM, Rajaraman P, Sir Craft AW, Parker L, Berrington de González A. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380:499–505. doi: 10.1016/S0140-6736(12)60815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wade R, Yang H, McKenna C, Faria R, Gummerson N, Woolacott N (2012) A systematic review of the clinical effectiveness of EOS 2D/3D X-ray imaging system. Eur Spine J. 19(5) [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 31.McKenna C, Wade R, Faria R, Yang H, Stirk L, Gummerson N, Sculpher M, Woolacott N. EOS 2D/3D X-ray imaging system: a systematic review and economic evaluation. Health Technol Assess. 2012;16:1–188. doi: 10.3310/hta16140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Luque ER. Segmental spinal instrumentation for correction of scoliosis. Clin Orthop Relat Res. 1982;163:192–198. [PubMed] [Google Scholar]
- 33.Bridwell KH, Hanson DS, Rhee JM, Lenke LG, Baldus C, Blanke K. Correction of thoracic idiopathic scoliosis with segmental hooks, rods, and Wisconsin wires posteriorly: it’s bad and obsolete, correct ? Spine. 2002;27:2059–2066. doi: 10.1097/00007632-200209150-00018. [DOI] [PubMed] [Google Scholar]
- 34.Delorme S, Labelle H, Aubin CE, de Guise JA, Rivard CH, Poitras B, Dansereau J. A three-dimensional radiographic comparison of Cotrel-Dubousset and Colorado instrumenttaions for the correction of idiopathic scoliosis. Spine. 2000;25:205–210. doi: 10.1097/00007632-200001150-00010. [DOI] [PubMed] [Google Scholar]
- 35.Asghar J, Samdani AF, Pahys JM, D’Andrea LP, Guille JT, Clements DH, Betz RR. Computed tomography evaluation of rotation correction in adolescent idiopathic scoliosis: a comparison of an all pedicle screw construct versus a hook-rod system. Spine (Phila Pa 1976) 2009;34:804–807. doi: 10.1097/BRS.0b013e3181996c1b. [DOI] [PubMed] [Google Scholar]
- 36.Lee SM, Suk SI, Chung ER. Direct vertebral rotation: a new technique of three-dimensional deformity correction with segmental pedicle screw fixation in adolescent idiopathic scoliosis. Spine. 2004;29:343–349. doi: 10.1097/01.BRS.0000109991.88149.19. [DOI] [PubMed] [Google Scholar]
- 37.Di Silvestre M, Lolli F, Bakaloudis G, Maredi E, Vommaro F, Pastorelli F (2012) Apical vertebral derotation in the posterior treatment of adolescent idiopathic scoliosis: myth or reality? Eur Spine J 7 [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 38.Wagner MR, Flores JB, Sanpera I, Herrera-Soto J. Aortic abutment after direct vertebral rotation: plowing of pedicle screws. Spine (Phila Pa 1976) 2011;36:243–247. doi: 10.1097/BRS.0b013e31820107d0. [DOI] [PubMed] [Google Scholar]
- 39.Vora V, Crawford A, Babekhir N, Boachie-Adjei O, Lenke L, Peskin M, Charles G, Kim Y. A pedicle screw construct gives an enhanced posterior correction of adolescent idiopathic scoliosis when compared with other constructs: myth or reality. Spine. 2007;32:1869–1874. doi: 10.1097/BRS.0b013e318108b912. [DOI] [PubMed] [Google Scholar]
- 40.Blondel B, Lafage V, Farcy JP, Schwab F, Bollini G, Jouve JL. Influence of screw type on initial coronal and sagittal radiological correction with hybrid constructs in adolescent idiopathic scoliosis correction priorities. Orthop Traumatol Surg Res. 2012;98:873–878. doi: 10.1016/j.otsr.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 41.Ilharreborde B, Vidal C, Skalli W, Mazda K. (2012) Sagittal alignment of the cervical spine in adolescent idiopathic scoliosis treated by posteromedial translation. Eur Spine J 11 [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 42.Mac-Thiong JM, Labelle H, Rooze M, Feipel V, Aubin CE. Evaluation of a transpedicular drill guide for pedicle screw placement in the thoracic spine. Eur Spine J. 2003;12:542–547. doi: 10.1007/s00586-003-0549-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mac-Thiong JM, Labelle H, Roussouly P. Pediatric sagittal alignment. Eur Spine J. 2011;20(Suppl 5):586–590. doi: 10.1007/s00586-011-1925-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Remes V, Helenius I, Schlenzka D, Yrjonen T, Ylikoski M, Poussa M. Cotrel-Dubousset (CD) or Universal Spine System (USS) instrumentation in adolescent idiopathic scoliosis (AIS): comparison of midterm clinical, functional, and radiologic outcomes. Spine. 2004;29:2024–2030. doi: 10.1097/01.brs.0000138408.64907.dc. [DOI] [PubMed] [Google Scholar]