Abstract
Background
Rehabilitation treatment noncompletion is considered a risk factor for long term relapse in alcohol-dependent individuals. The aim of this analysis of in- and outpatients in alcohol dependence rehabilitation in Germany is to identify social, mental, and somatic risk profiles for treatment noncompletion.
Methods
A total of 92 individuals from an outpatient program and 303 individuals from two inpatient rehabilitation treatment units in three different locations in Germany were recruited and assessed with a structured interview and several measures of psychopathology (personality disorders, anxiety, depression, and impulsivity) at treatment admission, with termination at 12 months follow-up. Participants were subdivided into treatment completers and noncom-pleters for any reason.
Results
A total of 10.2% of inpatients and 16.1% of outpatients did not complete treatment. Compared with treatment completers, noncompleters had a significantly lower rate of continuous abstinence at 1-year follow-up, more recent alcohol consumption before admission, and a higher rate of borderline personality disorders. Among inpatients, an elevated rate of lifetime mental disorders, depression, and suicide attempts was found among treatment noncompleters; among outpatients, treatment noncompleters were more often than completers to be married but live separated.
Conclusion
Rates of treatment noncompletion in inpatient and outpatient rehabilitation programs correspond to results from previous research. Noncompletion is a significant correlate of relapse 1 year after treatment, and noncompleters show an elevated level of psychopathology. These findings may help rehabilitation treatment facilities to tailor specific therapies for these individuals to reduce risk for treatment noncompletion.
Keywords: alcohol dependence, rehabilitation treatment, noncompletion, inpatient, outpatient
Introduction
In Germany, approximately 1.3 million persons are currently alcohol-dependent and some 2.7 million individuals have harmful drinking (according to International Classification of Diseases-10); the overall direct and indirect societal costs of alcohol use disorders were estimated to account for €24.4 billion in 2002.1 In postacute treatment following in- or outpatient detoxification of alcohol-dependent individuals, rehabilitation treatment is one of the most common approaches in Germany and other European countries. Rehabilitation treatment of alcohol use disorders used to be conducted in an inpatient setting, usually with a structured daily schedule including single and group psychotherapies, sports, and visiting self-help groups. In the last decade, several health services have provided structured treatment programs for outpatient rehabilitation, for which efficacy and long term outcome has been empirically evaluated.2 Inpatient rehabilitation usually lasts 8–16 weeks (average duration of treatment in 17 rehabilitation hospitals in Germany: 81.61 ± 32.74 days).3 In comparison, outpatient treatment programs provide single and group therapies on several days per week for usually several months (average treatment duration in five German outpatient units 297.68 ± 190.51 days).4 More detailed description of the treatment program and characteristics in Germany are reported in a number of previous manuscripts.4–6
This previous research also points out that patients in outpatient treatment are usually socially better integrated, have a later onset and shorter duration of alcohol dependence and less comorbidity with mental or somatic diseases.5 However, the majority of rehabilitation treatment in Germany is conducted in inpatient facilities. For instance, in 2008, rehabilitation of alcohol- and substance use disorders was conducted in 55,963 individuals, of which 45,191 participants were treated in inpatient programs and 10,772 participants in outpatient programs.7 Several studies reported rates of continuous abstinence for inpatient treatment programs in Germany between 2003 and 2007 which range between 34.5% and 60.8% after 1 year follow-up.4 In comparison, fewer investigations are published on the efficacy of outpatient rehabilitation programs. Continuous abstinence rates in this latter setting range between 20% and 78%.8–10 The most important outcome criteria of abstinence and relapse are influenced by many characteristics and result most likely from a combination of various factors.11 These include individual characteristics such as comorbidity with mental disorders, alcohol, drug and environmental reinforcers, and problems coping with social factors such as unemployment.12 Another potential risk factor for negative outcome is premature therapy discharge or treatment noncompletion. Treatment noncompletion is defined as either the patient’s intention to leave treatment before time or the subject is discharged due to misconduct or offense against setting rules.13
Previous research indicated that treatment noncompletion is strongly associated with long term drinking outcomes, with unplanned discharges being more likely to result in relapse to previous patterns of alcohol misuse and less likely to maintain improvement than those who complete treatment.14,15 Though many factors influence continuation in treatment, these previous studies indicate that recording treatment completion is a useful predictor for progress beyond treatment. Rates of treatment noncompletion in alcohol treatment services vary remarkably in available data, from more than 50% in Scotland to approximately 10% to 20% over several years in inpatient rehabilitation programs in Germany, and are in general lower in alcohol-dependent individuals compared to participants with a substance use disorder.4,16–20
Thus, it is of relevance for therapists to identify potential risk factors across treatment settings (eg, in- versus outpatient) for treatment discontinuation. However, few studies have investigated the characteristics of participants which lead to premature therapy discontinuation. A previous study on treatment noncompletion in alcohol detoxification identified affective symptoms, low motivation and insight, and cognitive impairment as potential risk factors.18 Patients in acute detoxification treatment may have different characteristics from participants undergoing in- and outpatient rehabilitation programs since these individuals are in withdrawal and may have a different motivation to change their behavior for treatment than participants in longterm treatment. Furthermore, alcohol-dependent individuals have to complete detoxification before being admitted to rehabilitation programs in both in- and outpatient facilities.5 While inpatients are usually significantly more severely affected by the psychosocial and somatic consequences of an alcohol use disorder, it may be of interest for therapists to identify the different risk factors for treatment discontinuation across groups.5
The aim of this study was to identify such potential risk factors for treatment noncompletion among inpatient and outpatient alcohol-dependent participants in rehabilitation programs from three institutions. The assessment of participants included several dimensions of characteristics: sociodemographic, somatic, mental, personality, and alcohol use. We expected higher rates and intensity of psychosocial problems (living alone, unemployment) and comorbidity with mental disorders to be significantly associated with a higher rate of treatment discontinuation in both inpatient and outpatient participants.
Methods
Participants and designs
From January to December 2003, a total of 92 alcohol-dependent patients (60 males, 32 females) were consecutively recruited at the start of the outpatient rehabilitation program. Outpatients fulfilled the International Classification of Diseases-10 criteria for alcohol dependence. A further inclusion criterion was a stable residential situation. The outpatient treatment program and characteristics were detailed in previous publications.5,21
In brief, the study was conducted at the Client-oriented Problem Advice Centre Dachau, near Munich, Germany. This center offers a highly structured, intensive, two-phase treatment model. Treatment started with a 3-month motivational phase immediately after detoxification. This phase included a detailed medical/neurological and psychodiagnostic examination. Patients were seen on several days per week. They attended a weekly group therapy session and four individual psychotherapy/medical sessions. The motivational phase was followed by an 8-month rehabilitation program, which is the focus of this research. The therapy concept was integrative and eclectic, and included psychoanalytical as well as behavioral approaches and methods (three weekly sessions). It was an intensive abstinence-oriented program that was described in detail in a previous publication.2
All inpatients from the rehabilitation program in Greif-swald (KH Bethanien, Johanna-Odebrecht-Stiftung, n = 105, 87 males, 18 females, treated during the year 2004) and Wilhelmsheim (n = 198, 155 males, 43 females, treated in 2003 and 2004) were enrolled into the study. Exclusion criteria for all inpatients and outpatients were dependence on benzodiazepines and/or illicit drugs, severe physical illness, severe mental disorders, and mental disorders requiring inpatient psychiatric treatment (acute suicidality, psychosis).
Persons were referred from general physicians or resident psychiatrists to in- and outpatient rehabilitation if they were approved by the health care provider or the local pension fund. These organizations are in charge of financing the alcohol and substance use disorders rehabilitation in Germany. Inpatients were mainly referred from inpatient detoxification units in general or psychiatric hospitals. All patients were informed before referral that the treatment settings were oriented to longterm abstinence.
Assessments
For in- and outpatients, assessments were conducted on admission (T0), discharge (T1), and 12 months after treatment discharge (T2), using a face-to-face structured interview according to the German Society for Addiction Research and Therapy.22 This interview gathered information on current legal and socioeconomic situations, lifetime mental and somatic health, as well as characteristics of substance use disorders. At discharge, the length of time spent in the program, mode of discharge from the program (eg, successfully completed the program, left prematurely by choice, etc) and other incidents, like relapses during treatment, were recorded. The interviewers were trained psychologists, physicians, or medical students who were not involved in the treatment of interviewed participants. For the 1-year follow-up assessment (T2), the former in- and outpatients were contacted via mail. They were invited for a personal interview; otherwise, the interview was conducted via phone.
Relapse during the follow-up period was defined as any alcohol intake; continuous abstinence meant no reported alcohol intake during the assessment period. Abstinence after relapse was defined as no alcohol intake for more than a month (30 days) before the follow-up assessment.
In both groups, a number of self-rating instruments were employed, including the Barratt Impulsiveness Scale (BIS 11, German version), Beck’s Depression Inventory (BDI), the State Trait Anxiety Inventory (STAI, German version), the Structured Clinical Interview for DSM Disorders (SCID) II interview for Axis II disorders (12 personality disorders, SCID-II-PQ self-rating questionnaires and a subsequent SCID-II interview of the positively endorsed items and specific personality disorder diagnosis), and the Obsessive Compulsive Drinking Scale (OCDS, German version).23–28 Data from the baseline assessment were included in the analysis.
Ethical standards
Written informed consent was obtained from all participants after research staff described the experimental procedures in detail and explained that they may withdraw from the study at any time they wished and without reason. In particular, patients were assured that withdrawal would have no influence on their further treatment. The study was approved by the ethical committee of the Ernst-Moritz-Arndt-University, Greifswald, Germany, and was in accordance to the guidelines laid down in the current version of the Declaration of Helsinki.
Statistical analysis
All analyses were conducted by Predictive Analytics Software (v18; SPSS Inc, Chicago IL). Patients were sub grouped according to in- and outpatient status and treatment completion versus noncompletion. To reveal potential predictors for noncompletion, comparisons between treatment completers versus noncompleters were performed using univariate Chi2 statistics by Pearson (dichotomous and categorical data) and Student’s t-test, if variables did not deviate from normal distribution. Alternatively, Mann–Whitney U test for ordinal data was employed. Deviation from normal distribution was computed using Kolmogorov–Smirnov nonparametrical test. All statistical tests were two-tailed. A P-value of less than 0.05 was considered to be statistically significant.
Finally, adjusted logistic regression analysis was used to evaluate how patients’ characteristics influenced treatment completion after statistically controlling for setting (in- versus outpatients), gender, and age. Variables were included into the logistic regression equation if they significantly differentiated between treatment-completion groups for both settings in the univariate analyses.
Results
Characteristics of in- and outpatients
No significant differences with respect to marital status across groups were found. However, participants in outpatient versus inpatient treatment were significantly more often employed (76.2% versus 44.6%, P < 0.001), had more days of abstinence before treatment (T-test: 9.69, P < 0.001) and a higher number of mental disorders (T-test: 4.80, P < 0.001). When the two inpatient facilities were compared, inpatients from Greifswald relative to those from Wilhelmsheim were significantly less often employed (1.6% versus 49.4%, P < 0.001), which was related to local differences in the employment market. Moreover, inpatients in Greifswald had a higher number of somatic (t-test: 8.08, P < 0.001) and mental health problems (t-test: 2.07, P < 0.05).
Other sample characteristics with respect to inpatient and outpatient status and treatment completion versus noncompletion are presented in Table 1. A total of 31 inpatients (10.2%, 26 males, 5 females) and 15 outpatients (16.3%, 7 males, 8 females) did not complete treatment for any reason (treatment noncompleters). Compared with treatment completers, participants who did not complete treatment were significantly more often married but separated (inpatients), used alcohol more recently before admission (inpatients and outpatients), and had more mental health problems.
Table 1.
Sociodemographic data of inpatient and outpatient alcohol-dependent individuals
| Variables | Inpatient MEAN ± SD or %
|
Outpatient MEAN ± SD or %
|
χ2-, t-test values (inpatient/outpatient) | ||
|---|---|---|---|---|---|
| Treatment noncompleters | Treatment completers | Treatment noncompleters | Treatment completers | ||
| Gender (male/female), n | 26/5 | 216/56 | 7/8 | 53/25 | 0.34/2.72 |
| age (19–69 years) | 42.87 ± 7.5 | 44.73 ± 7.9 | 47.87 ± 6.5 | 45.87 ± 10.7 | 1.25/0.69 |
| Marital status | 2.61/6.91 | ||||
| Unmarried | 25.4% | 32.3% | 13.3% | 22.1% | 0.68/0.59 |
| Married, living together | 40.8% | 22.6% | 53.3% | 45.5% | 3.90*/0.31 |
| Married but separated | 5.9% | 6.6% | 26.7% | 6.5% | 0.16/5.8* |
| Divorced | 24.3% | 35.5% | 6.7% | 20.8% | 1.84/1.66 |
| Widowed | 0% | 0% | 0% | 0% | −/− |
| Other | 0.6% | 0% | 0% | 0% | 0.11/− |
| Unemployment | 69.2% | 30.8% | 27.3% | 23.1% | 2.31/0.09 |
| Last alcohol use before admission (days ago) | 37.87 ± 50.7 | 70.25 ± 80.5 | 109.29 ± 59.8 | 144.19 ± 53.1 | 3.32**/2.25* |
| Somatic disorders lifetime, n | 0.63 ± 0.72 | 0.76 ± 1.0 | 1.64 ± 1.22 | 1.45 ± 1.34 | 0.69/0.51 |
| Mental disorders lifetime, n | 1.29 ± 1.51 | 0.84 ± 1.1 | 0.66 ± 0.89 | 1.25 ± 1.2 | 2.08*/1.82 |
| Duration of in- or outpatient treatment (days) | 78.47 ± 103.6 | 103.57 ± 94.8 | 130.66 ± 94.5 | 246.49 ± 100.6 | 1.06/1.95 |
| Treatment completion scheduled termination | 100% | 100% | |||
| Treatment noncompletion | |||||
| By patient | 50.0% | 66.7% | |||
| By institution | 28.6% | 0% | |||
| By health care provider | 0% | 33.3% | |||
| Transfer to hospital | 0% | 0% | |||
| Other | 21.4% | 0% | |||
| Follow-up 12 months | |||||
| Continuous abstinence | 15.6% | 39.5% | 13.3% | 71.4% | 7.06*/20.2*** |
| Relapse | 75.0% | 52.9% | 80.0% | 22.1% | |
| Abstinent >1 month after relapse | 9.4% | 7.6% | 6.7% | 6.5% | |
Notes:
P < 0.05;
P < 0.01;
P < 0.001.
Abbreviation: SD, standard deviation.
Outcome measures across groups after 12 months are also shown in Table 1. In both inpatient and outpatient groups, treatment noncompleters had significantly higher relapse rates than treatment completers. Furthermore, there were no significant associations between any previous (in- or outpatient) treatment and current treatment continuation.
Personality disorders
Differences in Diagnostic and Statistical Manual of Mental Disorders (DSM) IV personality disorders between in- and outpatients by treatment completion status are depicted in Table 2. Among inpatients, treatment noncompleters had a greater number of personality disorders than completers (ie, paranoid, histrionic, narcissistic, and borderline personality disorders). The number of and rate of any DSM IV Cluster B personality disorders (ie, borderline, narcissistic, antisocial, and histrionic) were significantly higher among treatment noncompleters than the rate among treatment completers (76.9% versus 27.8%) for inpatients; no such differences were observed for outpatients.
Table 2.
Personality disorders among inpatients and outpatients by treatment completion status
| Type of personality disorder (DSM IV criteria met) | Inpatient MEAN ± SD or %
|
Outpatient MEAN ± SD or %
|
χ2-, t-value (Inpatient/outpatient) | ||
|---|---|---|---|---|---|
| Treatment noncompleters | Treatment completers | Treatment noncompleters | Treatment completers | ||
| DSM IV personality disorders, n | 2.70 ± 2.2 | 1.22 ± 1.8 | 0.25 ± 0.5 | 0.87 ± 1.1 | 2.50*/1.12 |
| Any cluster A | 33.3 | 16.0 | 0 | 9.7 | 2.2/0.43 |
| Any cluster B | 76.9 | 27.8 | 50.0 | 21.1 | 14.2**/2.58 |
| Any cluster C | 53.8 | 41.8 | 0 | 46.5 | 0.73/3.32 |
Notes:
P < 0.05;
P < 0.001. Cluster a personality disorders (DSM IV): paranoid, schizotypal, or schizoid; cluster B personality disorders (DSM IV): histrionic, narcissistic, borderline, or antisocial; cluster C personality disorders (DSM IV): avoidant, dependent, obsessive, negativistic, or depressive.
Abbreviation: SD, standard deviation.
Other lifetime mental health problems
Rates of lifetime mental health problems are shown in Table 3. Among inpatients, treatment noncompleters relative to completers were significantly more depressed, had a higher rate and number of suicide attempts, but there were no differences in these characteristics among outpatients by treatment completion status.
Table 3.
Lifetime mental health problems among inpatients and outpatients by treatment completion status
| Lifetime mental disorders | Inpatient MEAN ± SD or %
|
Outpatient MEAN ± SD or %
|
χ2-, t-value (inpatient/outpatient) | ||
|---|---|---|---|---|---|
| Treatment noncompleters | Treatment completers | Treatment noncompleters | Treatment completers | ||
| Severe depression | 41.9 | 22.8 | 20.0 | 23.4 | 5.47*/0.08 |
| Severe anxiety and tension | 32.3 | 24.3 | 26.7 | 46.8 | 0.95/2.06 |
| Suicidal ideas | 38.7 | 22.8 | 20.0 | 23.4 | 3.82/0.08 |
| Suicide attempts | 29.0 | 13.2 | 20.0 | 16.9 | 5.49*/0.09 |
| suicide attempts, n | 0.95 ± 1.5 | 0.30 ± 0.73 | 0.20 ± 0.41 | 0.26 ± 0.71 | 3.54**/0.31 |
| mental problems, n | 2.32 ± 2.3 | 1.50 ± 1.8 | 1.27 ± 1.9 | 1.92 ± 1.9 | 2.38*/1.21 |
Notes:
P < 0.05;
P < 0.01.
Abbreviation: SD, standard deviation.
Dimensional characteristics
Intensity of self-reported depressive and anxious symptoms and craving at rehabilitation program admission did not differ across groups (Figure 1). However, among inpatients, treatment noncompleters had significantly higher scores of self-reported impulsive behavior compared to treatment completers.
Figure 1.
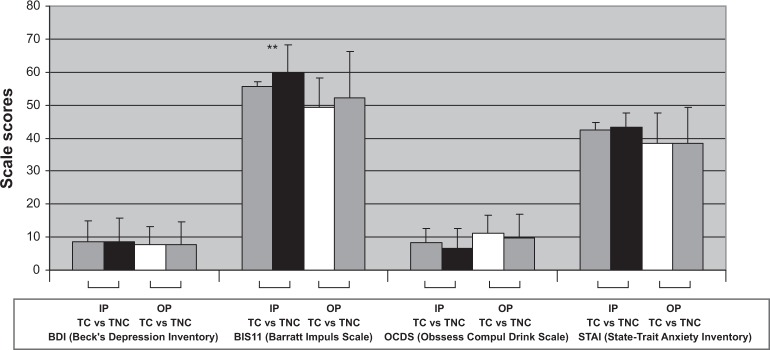
Dimensional characteristics of inpatients and outpatients by treatment completion status.
Note: **P < 0.01.
Abbreviations: IP, Inpatients; OP, Out patients; TC, Treatment completers; TNC, Treatment noncompleters.
Adjusted logistic regression analysis
The results of adjusted logistic regression analysis are reported in Table 4. Variables with potential deviations from linearity were dichotomized using median split (including number of mental problems and days of alcohol consumption before admission). After controlling for treatment setting, age, and gender, we found that shorter duration of abstinence before treatment admission and a diagnosis of any Cluster B Axis II personality disorder significantly increased the odds of treatment discontinuation.
Table 4.
Logistic regression analyses of characteristics associated with treatment noncontinuation
| Variables (n = 395) | Treatment continuation +/−
|
||
|---|---|---|---|
| χ2-value | Odds ratio | 95% CI | |
| Age (years) | 2.05 | 0.95 | 0.89–1.01 |
| Females vs males | 3.37 | 2.95 | 0.93–9.36 |
| Inpatient vs outpatient treatment | 5.35* | 10.23 | 1.43–7.29 |
| Separated or divorced | 0.08 | 1.17 | 0.39–3.58 |
| Last alcohol intake before treatment admission (days, median split) | 5.86* | 0.99 | 0.96–1.00 |
| Any other substance use | 0.54 | 0.43 | 0.05–4.06 |
| # of lifetime mental problems (median split) | 0.58 | 0.64 | 0.20–2.02 |
| Any DSM IV axis ii cluster B personality disorder | 12.68** | 6.95 | 2.39–20.19 |
Notes:
P < 0.05;
P < 0.001. Treatment continuation +/−: yes or no. DSM IV axis ii cluster B: including any histrionic, narcissistic, borderline, or antisocial personality disorders.
Abbreviation: CI, confidence interval.
Discussion
The aim of this study was to identify potential risk factors for treatment noncompletion among patients in in- and outpatient alcohol-dependent rehabilitation programs. Previous studies on individuals with alcohol and drug use disorders found treatment noncompletion as one significant risk factor for later relapse and adverse outcomes. This study used several well-evaluated instruments to characterize in- and outpatients in postacute rehabilitation programs, including sociodemographics, personality disorders, mental disorders, and somatic problems. The rates of treatment noncompletion differed by treatment setting: 10.2% of inpatients did not complete treatment, compared to 16.1% of outpatients. In comparison, the rates of inpatient treatment noncompletion of 10%–15% in large samples of alcohol rehabilitation are similar to the rates in our sample.4 However, data on treatment noncompletion in outpatient rehabilitation settings are limited. A recent study on treatment characteristics and outcomes among 275 participants with substance use disorders reported a therapy discontinuation rate of 25.8%, much higher than our outpatient rate and certainly exceeding the fraction of noncompleters in inpatient samples.10 In our sample, comorbid mental and personality disorders may be of more importance among inpatients for treatment noncompletion. By comparison, outpatient’s marital status (living alone or being separated) was of high significance for treatment completion. Familial and social factors have also been identified as significant predictors of outpatient treatment compliance in alcohol dependence treatment.29 Thus, while recognition and treatment of comorbid mental disorders need to be considered for inpatients, outpatients may require more therapeutic support and help regarding their partnership or coping with living alone.
It is also remarkable that approximately 50% of individuals in both groups who did not complete treatment had a diagnosis of borderline personality disorder. This disorder is known to manifest clinical characteristics such as impulsivity, emotional instability, identity disorders, and other significant problems, which may interfere with complying with setting rules and therapeutic schedules. This finding is supported by the logistic regression analysis showing that any Cluster B personality disorder diagnosis had elevated odds of treatment discontinuation, across settings. Nevertheless, participants with a comorbid Cluster B Axis II disorder and alcohol dependence present a therapeutic challenge. Previous studies indicated that treatment response among these individuals is at best moderate.30 Rehabilitation program settings would certainly profit from offering specific treatment to individuals with comorbid personality and alcohol use disorders, such as dialectical behavior therapy (DBT) and its modifications to reduce attrition in treatment and improve prognosis of these severely affected individuals.31,32 Therefore, future research may investigate whether treatment adherence would improve outcome in in- and outpatient participants with these modified DBT approaches. These DBT variations change the treatment focus to coping with abstinence and improvement of social factors.32
In both in- and outpatient groups, more recent alcohol consumption was also significantly related to treatment noncompletion, which may reflect the inability to stay abstinent. Moreover, among inpatients, number of lifetime mental disorders and rate of suicide attempt history were significantly higher in noncompleters compared to com-pleters. However, these factors did not remain significant in the adjusted logistic regression analysis and may be therefore of secondary relevance for treatment discontinuation. Thus, these individuals have extroverted personality problems and are less likely to stay abstinent, which characterize a group at risk for terminating treatment prematurely.
In line with previous research, the 12-month followup relapse rate in our study is significantly higher among noncompleters in both in- and outpatients. Thus, treatment noncompleters in both settings have a significantly worse outcome and in follow-up assessments of more than 2 years.29,33 In comparison, previous research reported continuous abstinence rates 12 months after inpatient rehabilitation treatment to range between approximately 35% and 61% across studies and samples.4,33 Other data on outpatient rehabilitation treatment reported continuous abstinence rates at 1 year of between 20% and 78%.9,34 Thus, treatment discontinuation is considered one of the significant risk factors for relapse. Other characteristics such as psychopathology or dependence severity may interact together and result in a combined influence on alcohol relapses and worse outcome 1 year later, all of which might contribute to a more chronic course of alcohol dependence.34
Our study had a number of limitations. The selection procedure of in- and outpatients was conducted before study initiation. Outpatients were assigned to treatment in accordance with health care providers’ coverage criteria, had a stable residential situation, and a rather good level of social adjustment, as indicated by the fairly low unemployment rate. In comparison, the two inpatient samples, coming from different areas of Germany, had an elevated rate of unemployment, and mental and somatic impairment. Another limitation includes the sample size. The outpatient sample size was rather small; the inpatient group had a moderate sample size. Other potential characteristics that may influence treatment noncompletion such as ratings of motivation to change, treatment goals, alcohol related expectancies, and self-efficacy should be included in future studies. Finally, specific treatment approaches or settings that account for both alcohol use and extroverted personality disorders are worthy of research, as they may improve outcome and reduce treatment noncompletion.
In conclusion, treatment noncompletion is confirmed in the current sample of in- and outpatients to be a significant correlate for adverse outcome in rehabilitation of alcohol use disorders 12 months later. Factors significantly related to treatment noncompletion include less abstinence time before treatment admission and any diagnosis of a DSM IV Cluster B personality disorder. Recommendations for future treatment research include the establishment of specific therapy approaches addressing both alcohol use and personality disorders (eg, modified DBT). Future research should investigate the efficacy of these approaches in treating these comorbid individuals and include other clinically relevant variables, like locus of control or motivation, into their assessments and analyses.
Acknowledgments
The study was in part funded by the German Pension Fund (Deutsche Rentenversicherung Bund, DRV, Berlin, Germany; Grant to M Soyka). We thank Dr WMJ Wong for native English language editing.
Footnotes
Disclosure
The authors have no conflicts of interest to disclose.
References
- 1.Konnopka A, König HH. Direct and indirect costs attributable to alcohol consumption in Germany. Pharmacoeconomics. 2007;25:605–618. doi: 10.2165/00019053-200725070-00006. [DOI] [PubMed] [Google Scholar]
- 2.Bottlender M, Soyka M. Outpatient alcoholism treatment: predictors of outcome after 3 years. Drug Alcohol Depend. 2005;80:83–89. doi: 10.1016/j.drugalcdep.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 3.Missel P, Schneider B, Bachmeier R, et al. Effektivität der stationären Suchtrehabilitation – FVS-Katamnese des Entlassjahrgangs 2006 von Fachkliniken für Alkohol- und Medikamentenabhängige [Effectiveness of inpatient addiction rehabilitation – FVS-follow-up evaluation of patients discharged 2006 from professional rehabilitation centres for alcohol and drug dependence] Sucht aktuell. 2009;16:5–16. [German.] [Google Scholar]
- 4.Missel P, Schneider B, Bachmeier R, et al. Effektivität der stationären Suchtrehabilitation – FVS-Katamnese des Entlassjahrgangs 2007 von Fachkliniken für Alkohol- und Medikamentenabhängige [Effectiveness of inpatient addiction rehabilitation – FVS-follow-up evaluation of patients discharged 2007 from professional rehabilitation centres for alcohol and drug dependence] Sucht aktuell. 2010a;17:9–203. [German.] [Google Scholar]
- 5.Schmidt P, Küfner H, Löhnert B, Kolb W, Zemlin U, Soyka M. Efficiency of outpatient and inpatient alcohol treatment – predictors of outcome. Fortscht Neurol Psychiatr. 2009;77:451–456. doi: 10.1055/s-0028-1109501. [DOI] [PubMed] [Google Scholar]
- 6.Soyka M. Outpatient detoxification and weaning of alcohol-dependence: new approaches and treatment research results. Bayerisches Ärzteblatt. 2004;2:80–83. [Google Scholar]
- 7.Beckmann U, Klosterhuis H, Naumann B. Jahrbuch Sucht. Geesthacht: Neuland Verlagsgesellschaft; 2010. Suchtrehabilitation durch die Rentenversicherung [Addiction rehabilitation by the German pension fund] pp. 189–202. [German.] [Google Scholar]
- 8.Burtscheidt W, Wölwer W, Schwarz R, Strauss W, Gaebel W. Out-patient behaviour therapy in alcoholism: treatment outcome after 2 years. Acta Psychiatr Scand. 2002;106:227–232. doi: 10.1034/j.1600-0447.2002.02332.x. [DOI] [PubMed] [Google Scholar]
- 9.Soyka M, Hasemann S, Scharfenberg CD, Löhnert B, Bottlender M. New possibilities in treatment and rehabilitation of alcohol-dependent patients – a catamnestic study on the efficiency of outpatient treatment programmes demonstrated by a model procedure. Nervenarzt. 2003;74:226–234. doi: 10.1007/s00115-002-1398-9. [DOI] [PubMed] [Google Scholar]
- 10.Missel P, Schneider B, Funke W, et al. Effektivität der ambulanten Suchtrehabilitation FVS-Katamnese des Entlassjahrgangs 2007 von Ambulanzen für Alkohol- und Medikamentenabhängige [Effectiveness of outpatient addiction rehabilitation – FVS-follow-up evaluation of patients discharged 2007 from outpatient centres for alcohol and drug dependence] Sucht aktuell. 2010b;17:57–63. [German.] [Google Scholar]
- 11.Bottlender M, Soyka M. Impact of craving on alcohol relapse during, and 12 months following, outpatient treatment. Alcohol Alcohol. 2004;39:357–361. doi: 10.1093/alcalc/agh073. [DOI] [PubMed] [Google Scholar]
- 12.Miller WR, Hester RK. Treating alcohol problems: toward an informed eclecticism. In: Hester RK, Miller WR, editors. Handbook of Alcoholism Treatment Approaches: Effective Alternatives. 2nd ed. Elmsford, New York: Pergamon Press; 1995. [Google Scholar]
- 13.Department of Health, Scottish Executive National Waiting Times Information Framework November2003Available from: http://www.drug-misuse.isdscotland.org/wtpilot/framework.htmAccessed December 13, 2011
- 14.Weisner C, Ray GT, Mertens JR, Satre DD, Moore C. Short-term alcohol and drug treatment outcomes predict long-term outcomes. Drug Alcohol Depend. 2003;71:281–294. doi: 10.1016/s0376-8716(03)00167-4. [DOI] [PubMed] [Google Scholar]
- 15.Baekeland F, Lundwall L. Dropping out of treatment: a critical review. Psychol Bull. 1975;82:738–783. doi: 10.1037/h0077132. [DOI] [PubMed] [Google Scholar]
- 16.Newham R, Russell C, Daviesm JB. Planned and unplanned discharge from alcohol services in Scotland, 2004–2008. Alcohol Alcohol. 2010;45:64–69. doi: 10.1093/alcalc/agp081. [DOI] [PubMed] [Google Scholar]
- 17.Zobel M, Missel P, Bachmeier R, et al. Effektivität der stationären Suchtrehabilitation – FVS-Katamnese des Entlassjahrgangs 2003 von Fachkliniken für Alkohol- und Medikamentenabhängige [Effectiveness of inpatient addiction rehabilitation – FVS-follow-up evaluation of patients discharged 2003 from professional rehabilitation centres for alcohol and drug dependence] Sucht aktuell. 2005;2:5–15. [German.] [Google Scholar]
- 18.Braune NJ, Schröder J, Gruschka P, Daecke K, Pantel J. Determinants of unplanned discharge from in-patient drug and alcohol detoxification: a retrospective analysis of 239 admissions. Fortschr Neurol Psychiatr. 2008;76:217–224. doi: 10.1055/s-2008-1038116. [DOI] [PubMed] [Google Scholar]
- 19.Sonntag D, Hellwich A, Bauer C. Deutsche Suchthilfestatistik 2006 für stationäre Einrichtungen [German addiction health care service statistics for inpatient institutions] Sucht. 2007;53(Suppl 1):42–63. [German.] [Google Scholar]
- 20.Küfner H, Feuerlein W, Flohrschütz T. Die stationäre Behandlung von Alkoholabhängigen: Merkmale von Patienten und Behandlungsein-richtungen, katamnestische Ergebnisse [Inpatient treatment of alcohol-dependent individuals: characteristics of treatment centres, patients and follow-up results] Suchtgefahren. 1996;32:1–86. [German.] [Google Scholar]
- 21.Soyka M, Schmidt P. Outpatient alcoholism treatment – 24-month outcome and predictors of outcome. Subst Abuse Treat Prev Policy. 2009;4:15. doi: 10.1186/1747-597X-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deutsche Gesellschaft für Suchtforschung und Suchttherapie Dokumentationsstandards 3 für die Behandlung von Abhängigen [German Society for Addiction Research and Therapy: Standards of documentation 3 for treatment of substance dependence] Sucht. 2001;47:3–94. [German.] [Google Scholar]
- 23.Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;52:768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 24.Preuss UW, Rujescu D, Giegling I, et al. Psychometric evaluation of the German version of the Barratt Impulsiveness Scale. Nervenarzt. 2008;79:305–319. doi: 10.1007/s00115-007-2360-7. [DOI] [PubMed] [Google Scholar]
- 25.Hautzinger M, Bailer M, Worall H, Keller F. BDI Beck-Depressions-Inventar Testhandbuch. 2 überarbeitete. Bern: Verlag Hans Huber; 1995. [BDI Beck’s depression inventory handbook. 2nd ed.] auflage. [German.] [Google Scholar]
- 26.Laux G, Ganzmann P, Schaffner P, Spielberger CD. State Trait Anxiety Inventory (STAI) [Das State-Trait-Anxiety-Inventory (STAI)] Weinheim: Beltz; 1981. [German.] [Google Scholar]
- 27.Farmer RF, Chapman AL. Evaluation of DSM-IV personality disorder criteria as assessed by the structured clinical interview for DSM-IV personality disorders. Compr Psychiatry. 2002;43:285–300. doi: 10.1053/comp.2002.33494. [DOI] [PubMed] [Google Scholar]
- 28.Mann K, Ackermann K. Psychometric characteristics of the Obsessive Compulsive Drinking Scale [Psychometrische Kennwerte der deutschen Version der Obsessive Compulsive Drinking Scale] Sucht. 2000;46:90–100. [German.] [Google Scholar]
- 29.Nielsen B, Nielsen AS, Wraae O. Factors associated with compliance of alcoholics in outpatient treatment. J Nerv Ment Dis. 2000;188:101–107. doi: 10.1097/00005053-200002000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Wölwer W, Burtscheidt W, Redner C, Schwarz R, Gaebel W. Outpatient behaviour therapy in alcoholism: impact of personality disorders and cognitive impairments. Acta Psychiatr Scand. 2001;103:30–37. doi: 10.1034/j.1600-0447.2001.00149.x. [DOI] [PubMed] [Google Scholar]
- 31.Linehan MM. Dialektisch-Behaviorale Therapie der Borderline-Persönlichkeitsstörung [Dialectical behavioral therapy for borderline personality disorder] München: CIP-Medien; 1996. [German.] [Google Scholar]
- 32.Mayer-Bruns F, Lieb K, Dannegger E, Jacob GA. Application of dialectical behavior therapy as in-patient treatment for alcohol dependency. Nervenarzt. 2005;76:339–343. doi: 10.1007/s00115-004-1860-y. [DOI] [PubMed] [Google Scholar]
- 33.Sonntag D, Künzel J. Hat die Therapiedauer bei alkohol- und drogenabhängigen Patienten einen positiven Einfluss auf den Therapieerfolg? [Is there a positive influence of therapy duration on treatment outcome in drug-dependent patients?] Sucht. 2000;46(Sonderheft 2 [Special issue 2]) [German.] [Google Scholar]
- 34.Adamson SJ, Sellman JD, Frampton CM. Patient predictors of alcohol treatment outcome: a systematic review. J Subst Abuse Treat. 2009;36:75–86. doi: 10.1016/j.jsat.2008.05.007. [DOI] [PubMed] [Google Scholar]