Abstract
Background
In the present study, we want to demonstrate the correlation between obstructive sleep apnea syndrome (OSAS) whose independent effect on carotid artery intima-media thickness (IMT) was demonstrated, with Framingham risk score (FRS) showing the overall cardiovascular risk.
Methods
IMT of the carotid artery was measured with ultrasonography and 10-year risk of coronary heart disease (CHD) was defined with FRS in 90 consecutive patients referred to our sleep clinic and who underwent polysomnography (PSG), with vascular risk factors and without a clinical atherosclerotic disease.
Results
IMT and FRS were found to be statistically significantly increased in the severe OSAS group compared to the other two groups. Carotid IMT was found to be significantly positively correlated with, apnea-hypopnea index (AHI), oxygen desaturation index (ODI) and time duration with oxygen saturation (SpO2) <90%, and negatively correlated with minimum oxygen saturation at sleep (minimum SpO2) and mean SpO2. In control and mild OSAS group IMT and FRS have significantly positive correlation (r: 0.501, P: 0.027; r: 0.625, P<0.001), while in severe OSAS group no significant correlation was detected between IMT and FRS (r: 0.321, P: 0.06). In the regression analysis AHI and ODI were found to be an independent predictor of carotid IMT. ODI was found to have an independent effect on the progression of atherosclerosis.
Conclusions
Increased carotid IMT in severe OSAS group could not be explained with the classical risk factors. In this respect, FRS might be insufficient to determine correctly the cardiovascular risk and protection strategies against the disease in OSAS patients.
KEYWORDS : Carotid artery, Framingham risk score (FRS), sleep apnea
Introduction
Relapsing episodes of hypoxia observed in obstructive sleep apnea syndrome (OSAS) are associated with the activation of various neural, humoral, thrombotic, metabolic and inflammatory mechanisms playing a role in pathophysiology of many cardiac and vascular diseases (1). OSAS was shown to be correlated with numerous factors causing endothelial damage and atherosclerosis, such as inflammation, increased vascular endothelial growth factor, production of reactive oxygen radicals, elevated levels of the soluble adhesion molecules and coagulation (2).
Alterations in vascular structure can be reliably assessed with ultrasonographic measurements of the lumen size, tension, wall thickness and plaque formation (3-5). Various studies demonstrated that measurements of the intima-media thickness (IMT) of common carotid artery (CCA) is a useful marker both in determination of the atherosclerotic load and in prediction of the cardiovascular risk (6,7). Despite the differences in selection of the patients and control groups, IMT is increased in OSAS patients independent of other factors (8-10).
Alterations in vascular structure can be reliably assessed with ultrasonographic measurements using the risk factors found in the Framingham study such as age, total cholesterol, HDL cholesterol, smoking, diabetes mellitus (DM) and blood pressure, risk of CAD for the next ten years can be predicted (11). Framingham risk score (FRS) is widely used for determination of the prognosis and the need for treatment in general population (12-14). However, as far as we know, there is no study so far showing the correlation between IMT and FRS in OSAS patients.
In the present study, we aimed to evaluate the effect of OSAS on progression of atherosclerosis, correlation between severity of OSAS and IMT measurement and also correlation with FRS using carotid artery IMT measurements in the population with and without OSAS.
Materials and methods
Consecutive 90 patients referred to Sleep Disorders Center of Dışkapı Yıldırım Beyazıt Teaching Hospital, Ankara between December 2006 and May 2007, with provisional diagnosis of OSAS and who met the inclusion criteria were included in the study. Detailed histories of the patients were elicted and physical examinations were performed. All the patients were informed, and their consents were received.
Patients
People between the ages of 30-74 years who do not have a previous diagnosis of ischemic heart disease, cerebrovascular disease, peripheral arterial disease, clinical symptoms of these diseases and a treatment for these diseases; a diagnosis of known renal, pulmonary, liver diseases and malignant diseases; and who did not undergo any specific treatment for OSAS [continuous positive airway pressure (CPAP) or surgical treatment] were included in the study. People using hypnotic and sedative medications, who have a diagnosis of central sleep apnea with polysomnography (PSG) and who did not satisfy the inclusion criteria were excluded from the study.
Risk factors
Hypercholesterolemia was defined as having a previous diagnosis for hypercholesterolemia, lipid-lowering medication use or a serum total cholesterol >240 mg/dL and low density lipoprotein (LDL) cholesterol >160 mg/dL. Blood pressures of the individuals were taken with a mercury sphygmomanometer from the right arm in two consecutive days in the morning at 08:00, following at least ten minutes resting. Average of the two measurements was recorded as systolic and diastolic blood pressure. The presence of hypertension (HT) was defined as; having a previous HT diagnosis, antihypertensive medication use or a blood pressure >140/90 mmHg. The people who regularly smoked for the last two months were considered as smokers. The people who received oral antidiabetic drugs or insulin therapy, and those diagnosed with DM according to the American Diabetes Association guide were considered as DM patients.
FRS, which was defined by evaluation of the cardiovascular risk factors in Framingham study, is a method used to predict 10-year risk for CHD. FRS in the persons was calculated using age, total cholesterol, high density lipoprotein (HDL) cholesterol, smoking, DM and blood pressure. Giving a specific point to each factor, 10-year risk for CHD corresponding to the total score was calculated as the percentage (11).
Laboratory work-up
Venous blood samples were collected following a full-night PSG after 12-hour fasting. Levels of fasting glucose, total cholesterol, triglyceride and HDL cholesterol were found using an automatic analyzer (P800 Roche Hitachi and Olympus AU 5200, Olympus corp., USA). Level of LDL cholesterol was calculated by the Friedwald method in the case of triglyceride <400 mg/dL.
Polysomnography (PSG)
With polysomnographic recording, EEG, EOG, chin EMG and bilateral anterior tibial muscle EMG, ECG, nasal airflow, respiratory effort (thorax and abdomen movements), oxygen saturation (from fingertip), tracheal microphone and body position recordings were obtained using Compumedics E-series (Compumedics, Australia). The data were collected in PSG recording system and evaluated by a single physician trained on sleep disorders and PSG who was unaware of measurements. In the polysomnographic records, sleep stages were evaluated according to Rechtschaffen and Kales criteria with 30-second epochs. Apnea was accepted as the pause in breathing lasting for at least ten seconds and hypopnea was accepted as a 30% (or greater) reduction in flow lasting for ten seconds or longer and an associated 4% (or greater) desaturation in the oxygen levels, or if it results in arousal or fragmentation of sleep. Apnea-hypopnea index (AHI) was taken as the number of apneas and hypopneas per hour and oxygen desaturation index (ODI) as the number of decrease in desaturation >4% per hour of sleep. In addition, T90 which is the percentage of the total sleep time with oxygen saturation below, mean oxygen saturation (mean SpO2) and minimum oxygen saturation at sleep (min SpO2) were recorded. Severity of OSAS was defined according to AHI. An AHI of 5 to15 is classified as mild obstructive sleep apnea; 15 to 30 is moderate OSA; 30 or more is severe OSA.
Carotid artery IMT measurement
Gray scale and color doppler sonography of the bilateral carotid arteries was performed using a SSA-390A Power Vision 8000 scanner (Toshiba, Tokyo, Japan) equipped with a 6-11 MHz linear-array transducer. People included in the study underwent scanning by a single radiologist within one week after PSG. The people were laid down in the supine position and right and left common carotid arteries and carotid bulbs were carefully examined. IMT measurements were made in the right and left carotid arteries, at 1 cm proximal of the bulb from areas without plaque in the proximal and distal walls of the artery (arterial wall next to the skin was considered as proximal and far from the skin as distal wall) (15). Plaque presence was accepted as the areas with a localized thickness >1.2 mm, which did not involve entire diameter of the artery (16). Two IMT measurements were made from the right and left common carotid arteries and average of these four values was recorded as the CCA IMT.
Statistical analysis
People in the three groups were compared in terms of the demographic, clinic and PSG findings, IMT and FRS. Quantitative data were expressed as the mean (mean) ± standard deviation (SD). Tukey HSD post-hoc test was used in comparison of the quantitative data, while chi-square test was used in evaluation of the qualitative data. Correlation of FRS and IMT measurements, demographic, clinic and polysomnographic data were evaluated the Pearson correlation analysis. Regression analysis was performed in order to define the independent factors of IMT. Regression analysis included Framingham risk factors (age, gender, smoking, total and HDL cholesterol, DM presence and blood pressure), body mass index (BMI), level of triglyceride and AHI, which is the marker of the severity of OSAS. Values of P<0.05 were considered as statistically significant.
Results
Consecutive 90 subjects who met the inclusion criteria with a mean age of 44.7±6.3 years were included in the study. They were divided into three groups according to AHI status. Demographic and clinical features of the groups are summarized in Table 1, and the polysomnographic data, mean carotid artery IMT and FRS values of the groups are seen in in Table 2.
Table 1. Comparison of demographic and clinic features of the groups.
| Features | Control | Mild-moderate OSAS | Severe OSAS | P |
|---|---|---|---|---|
| n | 20 | 35 | 35 | |
| Age (years) | 41.8±5.1 | 44.5±6.6 | 46.9±6.3 | 0.016º |
| Male n, (%) | 15, (75%) | 32, (91.4%) | 33, (94.3%) | 0.106 |
| BMI (kg/m2) | 29.0±5.1 | 29.5±3.5 | 33.1±4.4 | <0.0011 |
| Smokers n, (%) | 10, (50%) | 10, (28.6%) | 18, (51.4%) | 0.112 |
| Systolic BP (mmHg) | 113.6±11.5 | 124.3±14.8 | 127.1±13.7 | 0.0022 |
| Diastolic BP (mmHg) | 75.3±8.8 | 84.6±13.1 | 86.9±10.4 | 0.0013 |
OSAS, obstructive sleep apnea syndrome; BMI, body mass index. Comparison of the groups with Tukey HSD; ºgroup 1-2, P>0.05, group 1-3, P<0.05, group 2-3, P>0.05; 1group 1-2, P>0.05, group 1-3, P<0.05, group 2-3, P<0.05; 2group 1-2, P<0.05, group 1-3, P<0.05, group 2-3, P>0.05; 3group 1-2, P<0.05, group 1-3, P<0.05, group 2-3, P>0.05.
Table 2. Comparison of the PSG findings and carotid IMT measurements and FRS.
| Parameters | Control | Mild-moderate OSAS | Severe OSAS | P |
|---|---|---|---|---|
| Sleep efficiency (%) | 88.90±8.30 | 87.50±9.40 | 88.10±13.90 | 0.908 |
| TST (minutes) | 365.70±47.40 | 371.70±54.60 | 366.30±82.40 | 0.924 |
| AHI | 2.09±1.39 | 14.05±7.65 | 65.00±24.14 | <0.001 |
| ODI | 2.19±2.34 | 12.68±7.81 | 58.81±24.72 | <0.001 |
| T90 | 0.29±0.52 | 1.78±3.42 | 31.13±24.93 | <0.001 |
| Mean SpO2 | 94.44±1.35 | 93.03±1.24 | 89.28±3.80 | <0.001 |
| Min. SpO2 | 88.60±3.79 | 83.83±4.9 | 72.77±10.53 | <0.001 |
| ESS | 9.70±5.06 | 9.97±4.59 | 15.29±4.11 | <0.001 |
| IMT (mm) | 0.77±0.13 | 0.83±0.15 | 0.95±0.14 | <0.001 |
| FRS | 5.95±3.38 | 9.97±4.59 | 11.26±5.13 | <0.001 |
OSAS, obstructive sleep apnea syndrome; TST, total sleep time; AHİ, apnea-hypopne index; ODI, oxygen desaturation index; T90, which is the percentage of the total sleep time with oxygen saturation below; Mean SpO2, mean oxygen saturation at sleep; Min. SpO2, minimum oxygen saturation at sleep; ESS, epworth sleepiness scale; IMT, carotid arter intima-media thickness (mm); FRS, Framingham risk score.
Properties of groups in terms of presence of HT, DM, hyperlipidemia and medication use for these indications are given in Table 3.
Table 3. Comorbidities and medications.
| Comorbidities and medications | Control n [%] |
Mild-moderate OSAS n [%] |
Severe OSAS n [%] |
P | ||
|---|---|---|---|---|---|---|
| 20 | 35 | 35 | ||||
| Hypertension* | 0 [0] | 16 [45.7] | 16 [45.7] | 0.001 | ||
| Medication* | 0 [0] | 3 [8.6] | 6 [17.1] | 0.051 | ||
| DM* | 0 [0] | 3 [8.6] | 3 [8.6] | 0.208 | ||
| Medication* | 0 [0] | 0 [0] | 2 [5.7] | 0.146 | ||
| Hypercholeterolemi* | 1 [5] | 11 [31.4] | 10 [28.6] | 0.069 | ||
| Medication* | 1 [5] | 1 [2.9] | 3 [8.6] | 0.570 |
OSAS, obstructive sleep apnea syndrome; DM, diabetes mellitus. *n [%] was shown as number of the patients and percentage of them.
In the comparison of the carotid artery IMT measurement with ANOVA, a statistically significant difference was found between the groups (P<0.001) (Figure 1). No statistically significant difference was found between the control and mild-moderate OSAS groups in terms of IMT measurements with Tukey HSD analysis (P>0.05), while a statistically significant difference was found between severe OSAS group and both control and mild-moderate OSAS groups (P<0.001, P=0.001; respectively). When the carotid arteries were evaluated for the plaque existence, no plaque was found in any case in the control group (0%) whilst plaques were found in four patients (11.4%) in the mild-moderate OSAS group and in nine patients (25.7%) in the severe OSAS group.
Figure 1.
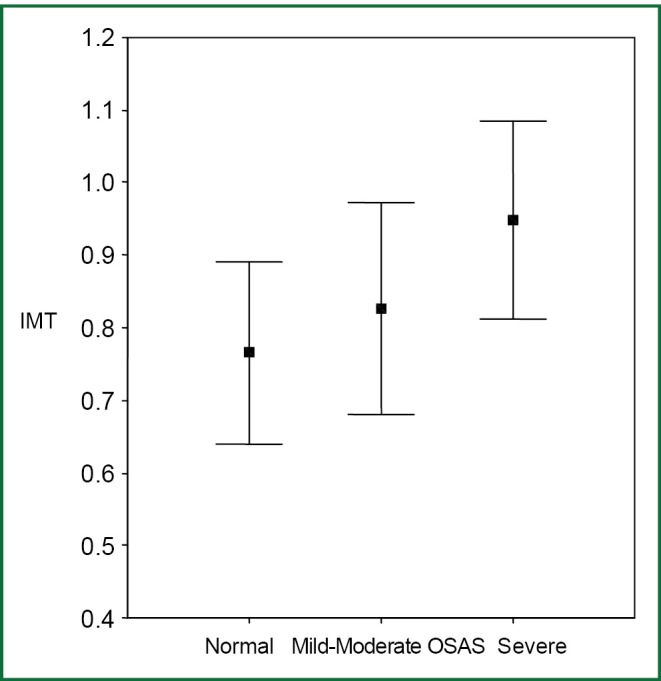
Comparison of the carotid IMT measurements between the groups. IMT, intıma-media thickness; OSAS, obstructive sleep apnea syndrome.
In the present study, FRS in the control group was 5.95±3.38, while in OSAS patients (n: 70) it was found to be 9.77±5.21. Statistically significant difference was found between patients with and without OSAS (P=0.003). Mean FRS was higher in the severe OSAS group (11.26±5.13), than that both the control (5.95±3.38) and mild-moderate group (9.97±4.59) and a statistically significant difference was found between three groups in the oneway ANOVA analysis regarding FRS (P<0.001). With Tukey HSD test, no statistically significant difference was found between the control and mild-moderate OSAS groups (P>0.05), while there were statistically significant differences both between severe OSAS and control groups and between severe and mild-moderate OSAS groups (P<0.01, P<0.05; respectively) (Table 2). When Pearson’s correlation analysis of FRS and IMT measurements were separately carried out in each group; the correlation of FRS and IMT measurements was found to be statistically significant in the control and mild-moderate OSAS groups (P<0.05, P<0.001; respectively), while the correlation was not statistically significant in the severe OSAS group (P>0.05).
In the correlation analysis between the IMT values and clinical and polysomnographic properties in the patient and control groups; IMT was found to be positively correlated with age, BMI, systolic and diastolic blood pressures, presence of HT, AHI, ODI and time duration in which SpO2 was <90% (T90), while it was negatively correlated with min SpO2 and mean SpO2. No statistically significant correlation was found between IMT and total cholesterol, HDL and LDL cholesterol, levels of triglyceride, DM existence, smoking and hypercholesteremia (P>0.05) (Table 4).
Table 4. Correlation of carotid IMT with demographic, clinic and PSG findings (n=90).
| Parameters | IMT measurements |
|
|---|---|---|
| r | P | |
| Age | 0.437 | <0.001 |
| BMI | 0.411 | <0.001 |
| Systolic BP | 0.464 | <0.001 |
| Diastolic BP | 0.454 | <0.001 |
| Total cholesterol | 0.156 | 0.142 |
| Triglyseride | 0.177 | 0.096 |
| HDL cholesterol | –0.107 | 0.313 |
| LDL cholesterol | 0.025 | 0.815 |
| Smoking | 0.03 | 0.981 |
| Hypertension | 0.361 | <0.001 |
| Diabetes mellitus | 0.176 | 0.97 |
| Hypercholesterolemia | 0.127 | 0.232 |
| AHI | 0.430 | <0.001 |
| ODI | 0.418 | <0.001 |
| T90 | 0.355 | 0.001 |
| Min. SpO2 | –0.363 | <0.001 |
| Mean SpO2 | –0.359 | 0.001 |
PSG, polysomnography; BMI, body mass index; IMT, intıma-media thickness; AHI, apnea-hypopne index; ODI, oxygen desaturation index; T90, which is the percentage of the total sleep time with oxygen saturation below; Mean SpO2, mean oxygen saturation at sleep; Min. SpO2, minimum oxygen saturation at sleep; ESS, epworth sleepiness scale.
In the stepwise regression analysis carried out to determine the independent predictors of IMT, besides the Framingham cardiovascular risk factors (age, gender, total cholesterol, HDL cholesterol, smoking, DM, systolic and diastolic blood pressures) BMI and levels of triglyceride were also included. Severity of OSAS was expressed using AHI. In the regression analysis, systolic blood pressure, AHI, age and HDL cholesterol were found to be independent predictors affecting IMT. When T90, min SpO2, mean SpO2 and ODI which are the markers of nocturnal hypoxemia in OSAS were used in the regression model instead of AHI, only ODI was found to be the independent predictor of IMT.
Discussion
In the present study, effect of OSAS on IMT and the correlation between IMT and FRS were evaluated in the population examined with the provisional diagnosis of OSAS and who had no clinical atherosclerotic disease. Changes in the arterial wall with development of atherosclerotic disease have long been evaluated with IMT measurements. Risk of coronary artery disease was shown to be increased with IMT values and it was demonstrated that IMT measurements can be used in determination of the cardiovascular risk (17). Cardiovascular risks determined in the Framingham study for cardiovascular diseases are widely used in prediction and prevention of CAD. Again, previous studies found a correlation between IMT and FRS, which is widely used in determination of the risk for CAD and this correlation was demonstrated to be useful in prediction of the risk for cardiovascular disease (12-14). Besides the epidemiological studies showing a correlation between OSAS and cardiovascular diseases, generalized atherosclerosis and carotid artery IMT, which is an important marker of coronary artery atherosclerosis, were also demonstrated to increase in OSAS patients and OSAS also was shown to play part in progression of atherosclerosis (8-10,18-20). However, as far as we know, so far, there is no study showing the correlation between FRS and IMT in OSAS.
In a study by Silvestrini et al. (9) carried out on male patients with severe OSAS, it was demonstrated for the first time that there was an increased tendency in the carotid arteries for atherosclerotic degeneration by using IMT measures independent of other cardiovascular risk factors, but they could not find a difference between OSAS patients and controls in terms of the prevalence of plaque. In that study, employment the ambulatory polysomnographic monitoring was a limiting factor, while in the present of study, PSG was applied to the patients in the sleep laboratory all night long. In a study by Schulz et al. (8) enrolling only subjects of male gender, which included severe OSAS and control groups matched for other cardiovascular risk factors, CCA IMT was shown to increase in untreated OSAS patients and a strong correlation was demonstrated between IMT measurements and degree of nocturnal hypoxemia. In a study by Minoguchi et al. (19) with obese controls and OSAS group, the time below SpO2 90% was shown to be a strong predictor of IMT. In our study also severity of OSAS and nocturnal desaturation were found to exert effect, independent of the other risk factors, on the prognosis of atherosclerosis, which is determined with IMT and our results are congruent with those of the earlier studies.
Chronic intermittent hypoxia developing during sleep was suggested to have a role in occurrence of the atherosclerotic alterations in OSAS (21). Reactive oxygen radicals emerging during hypoxia/reoksigenation periods cause inflammatory changes and atherosclerotic alterations. In addition, inflammatory markers of atherosclerosis such as CRP, cytokines and VEGF were shown to be correlated with OSAS in numerous studies (2). In our study; we demonstrated independent effect of ODI, which is a marker of nocturnal hypoxia on IMT, supporting the view that hypoxia associated with OSAS might be account for the atherogenic effect.
In OSAS, not only the severity of the disease but also duration of the disease could be important in the emergence of the complications. In the study done by Ciccone et al., they showed that carefully determined duration of the disease have an effect on the carotid IMT progression beside AHI which shows the severity of OSAS (22). In this study not only the severity of OSAS but also the duration of symptoms showed to significantly affect the atherosclerotic changes in OSAS. For this reason duration of symptoms should also be taken into account although difficulties in the determination, for the further studies.
In the current study, when the groups were compared in terms of FRS, FRS was found to be significantly higher in the severe OSAS group than in the other two groups. Similarly, carotid artery IMT was also found to be significantly increased in the severe OSAS group compared to the other two groups. A significant correlation was found between IMT values and FRS in the control and mild-moderate groups, while no significant correlation was found between the increased IMT and FRS in the severe OSAS group. In other words, while in both controls and mild-moderate OSAS groups FRS and IMT was found to be significantly correlated, this correlation was not detected in severe OSAS group in which FRS and IMT was significantly higher compared to the other two groups. This suggests that, in severe OSAS patients in which AHI and ODI values were significantly high, effect of OSAS on IMT was different from other traditional risk factors.
In a study by Drager et al. (23) with 12 normotensive male patients having severe OSAS, 4-month CPAP therapy was shown to have corrective effects on the markers of atherosclerosis, including carotid artery IMT, pulse-wave velocity, catecholamines and CRP, providing support to the view that OSAS is an independent risk factor for development of atherosclerosis. Again in a recent study of a group administered CPAP therapy for one year and a group followed-up with conservative treatment, IMT was demonstrated to be decreased in CPAP group (24). In our study, AHI showing the severity of OSAS was found to have effect independent of other risk factors on IMT, corroborating the view that OSAS has a role in development of atherosclerosis. This role of OSAS in development of atherosclerosis might be responsible for the increased IMT, which can not be fully explained with FRS.
Although there is evidence suggesting OSAS might be a risk factor for CAD, other co-existing risk factors for development of cardiovascular disease such as the obesity, advanced age, insulin resistance and HT make it difficult to evaluate the cause-and-effect relationship. In our study, OSAS group consisted of more obese persons than the other two groups. There is a strong correlation between OSAS and obesity and these often accompany each other. Conditions such as atherosclerosis, insulin resistance and HT, which are known to be caused by obesity are seen in OSAS patients, suggesting obesity might be partly implicated for the cardiovascular risk of OSAS (25). In brief, both OSAS and obesity might be effective in increased IMT, distinct from other FRS related factors.
Besides the development in the diagnosis and treatment, complications related to cardiovascular diseases are still very important health problem. By using Framingham CHD risk score, cardiovascular disease risk can be predicted and changeable rsik factors like as hipertension, smoking, DM and hyperlipidemiacan be prevented by planned preventive treatments. Risk factors other than traditional ones like as OSAS which was better known to cause atherosclerotic hearth-vessel disease nowadays was not included in this scoring system but this should also be kept in mind for the detection of cardiovascular risk and description of preventive treatments. In a previous study, evaluation of 10-year cardiovascular disease risk used for the initiation of statin therapy for the primary protection against cardiovascular disease was shown to be insufficient in determination of the statin need in OSAS patients (26). Results both from that and our study demonstrated that evaluation of 10-year cardiovascular disease risk is insufficient both in determination of the need for treatment and in indicating the atherosclerotic load found through IMT measurement.
Limitation of the present study was the small number of the patients. The reason why BMI, which is a very important risk factor for the development of cardiovasculer diseases, was not found to be a predictor in the regression analysis could be small sample size. Another limiting aspect was that persons in the control group who snored were also included in the study. In a former study, snoring was proposed to affect the progression of atherosclerosis (27). This situation and lack of a full comparison between the groups in terms of the cardiovascular risk factors might be responsible for not finding a difference between the control and mild-moderate OSAS groups in terms of IMT. Duration of OSAS symptoms could also affect carotid IMT (22). One of the limitation of our study is that we did not evaluated the disease duration.
In conclusion, in the evaluation of the normal individuals and OSAS patients presenting to the sleep clinic with vascular risk and having no clinic atherosclerotic disease; AHI and ODI, were demonstrated to have independent effects in progression of atherosclerosis, confirming the view that OSAS might be an independent risk factor in development of atherosclerosis. Increased IMT in the severe OSAS group could not be fully explained with the classical risk factors defined with FRS, suggesting that OSAS factors affect IMT independent to the other risk factors. FRS, which is used in prediction of CHD risk and treatment planning, might be insufficient in this respect in order to determine the risk accurately and guide intervention for protection from disease in OSAS patients. To clarify this situation, determination of the correlation between IMT and FRS through the follow-up studies with larger patient series will be helpful in planning treatment in this population at increased risk of cardiovascular disease and in correctly establishing treatment strategies for prevention of the cardiovascular diseases.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Shamsuzzaman AS, Gersh BJ, Somers VK. Obstructive sleep apnea implications for cardiac and vasculer disease. JAMA 2003;290:1906-14 [DOI] [PubMed] [Google Scholar]
- 2.Drager LF, Polotsky VY, Lorenzi-Filho G. Obstructive sleep apnea: an emerging risk factor for atherosclerosis. Chest 2011;140:534-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sawabe M, Takahashi R, Matsushita S, et al. Aortic pulse wave velocity and the degree of atherosclerosis in the elderly: a pathological study base on 304 autopsy cases. Atherosclerosis 2005;179:345-51 [DOI] [PubMed] [Google Scholar]
- 4.O’Leary DH, Polak JF. Intima-media thicness: a tool for atherosclerosis imaging and event prediction. Am J Cardiol 2002;90:18L-21L [DOI] [PubMed] [Google Scholar]
- 5.Burke GL, Evans GW, Riley WA, et al. Arterial wall thickness is associated with prevalent cardiovascular disease in middle-aged adults. The Atherosclerosis Risk in Communities (ARIC) Study. Stroke 1995;26:386-91 [DOI] [PubMed] [Google Scholar]
- 6.Megnien JL, Simon A, Gariepy J, et al. Preclinical changes of extracoronary arterial structures as indicators of coronary artery atherosclerosis in men. J Hypertens 1998;16:157-63 [DOI] [PubMed] [Google Scholar]
- 7.Grobbee DE, Bots ML. Carotid artery intima media thickness as an indicator of generalized atherosclerosis. J Intern Med 1994;236:567-73 [DOI] [PubMed] [Google Scholar]
- 8.Schulz R, Seeger W, Fegbeutel C, et al. Changes in extracranial arteries in obstructive sleep apnoea. Eur Respir J 2005;25:69-74 [DOI] [PubMed] [Google Scholar]
- 9.Silvestrini M, Rizzato B, Placidi F, et al. Carotid artery wall thickness in patients with obstructive sleep apnea syndrome. Stroke 2002;33:1782-5 [DOI] [PubMed] [Google Scholar]
- 10.Suzuki T, Nakano H, Maekawa J, et al. Obstructive sleep apnea and carotid-artery intima-media thickness. Sleep 2004;27:129-33 [DOI] [PubMed] [Google Scholar]
- 11.Wilson PW, D’Agostino RB, Levy D, et al. Prediction of coronary heart disease using risk factor categories. Circulation 1998;97:1837-47 [DOI] [PubMed] [Google Scholar]
- 12.Kieltyka L, Urbina EM, Tang R, et al. Framingham risk score is related to carotid artery intima-media thickness in both white and black young adults: the Bogalusa Heart Study. Atherosclerosis 2003;170:125-30 [DOI] [PubMed] [Google Scholar]
- 13.Campuzano R, Moya JL, García-Lledó A, et al. Endothelial dysfunction, intima-media thickness and coronary reserve in relation to risk factors and Framingham score in patients without clinical atherosclerosis. J Hypertens 2006;24:1581-8 [DOI] [PubMed] [Google Scholar]
- 14.Baldassarre D, Amato M, Pustina L, et al. Measurment of carotid artery intima-media thickness in dyslipidemic patients increases the power of traditional risk factors to predict cardiovascular events. Atherosclerosis 2007;191:403-8 [DOI] [PubMed] [Google Scholar]
- 15.O’Leary DH, Polak JF, Kronmal RA, et al. Thickening of the carotid wall. A marker for atherosclerosis in the elderly? Cardiovascular Health Study Collaborative Research Group. Stroke 1996;27:224-31 [DOI] [PubMed] [Google Scholar]
- 16.Nicolaides AN, Shifrin EG, Bradbury A, et al. Angiographic and duplex grading of internal carotid stenosis: can we overcome the confusion? J Endovasc Surg 1996;3:158-65 [DOI] [PubMed] [Google Scholar]
- 17.Chambless LE, Heiss G, Folsom AR, et al. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987-1993. Am J Epidemiol 1997;146:483-94 [DOI] [PubMed] [Google Scholar]
- 18.Drager LF, Bortolotto LA, Lorenzi MC, et al. Early signs of atherosclerosis in obstructive sleep apnea. Am J Respir Crit Care Med 2005;172:613-8 [DOI] [PubMed] [Google Scholar]
- 19.Minoguchi K, Yokoe T, Tazaki T, et al. Increased carotid intima-media thickness and serum ınflammatory markers in obstructive sleep apnea. Am J Respir Crit Care Med 2005;172:625-30 [DOI] [PubMed] [Google Scholar]
- 20.Protogerou AD, Laaban JP, Czernichow S, et al. Structural and functional arterial properties in patients with obstructive sleep apnoea syndrome and cardiovascular comorbidities. J Hum Hypertens 2008;22:415-22 [DOI] [PubMed] [Google Scholar]
- 21.Dean RT, Wilcox I. Possible atherogenic effects of hypoxia during obstructive sleep apnea. Sleep 1993;16:S15-21; discussion S21-2. [DOI] [PubMed]
- 22.Ciccone MM, Scicchitano P, Mitacchione G, et al. Is there a correlation between OSAS duration/severity and carotid intima-media thickness? Respir Med 2012;106:740-6 [DOI] [PubMed] [Google Scholar]
- 23.Drager LF, Bortolotto LA, Figueiredo AC, et al. Effects of continuous positive airway pressure on early sings of atherosclerosis in obstructive sleep apnea. Am J Respir Crit Care Med 2007;176:706-12 [DOI] [PubMed] [Google Scholar]
- 24.Hui DS, Shang Q, Ko FW, et al. A prospective kohort study of the long-term effects of CPAP on carotid artery intima-media thickness in obstructive sleep apnea syndrome. Respir Res 2012;13:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wolk R, Somers VK. Obesity-related cardiovascular disease: implications of obstructive sleep apnea. Diabetes Obes Metab 2006;8:250-60 [DOI] [PubMed] [Google Scholar]
- 26.Horwood F, Gruber A, Sithole J, et al. Cardiovascular disease risk assesment in patients with obstructive sleep apnoea: clinical utility of the Framingham risk equation for initiating statins. Diabetes Obes Metab 2008;10:181-2 [DOI] [PubMed] [Google Scholar]
- 27.Lee SA, Amis TC, Byth K, et al. Heavy snoring as a cause of carotid artery atherosclerosis. Sleep 2008;31:1207-13 [PMC free article] [PubMed] [Google Scholar]


