We present pre- and post-operative imaging findings in a 29-year-old man with a bicuspid aortic valve (BAV) with fusion of the right and left coronary leaflets and a 6.1 cm × 6.3 cm ascending aorta aneurysm (Figure 1). The patient underwent a valve-sparing aortic root replacement with a 34-mm Dacron graft and BAV repair with resection of the raphe of the fused leaflet and leaflet shortening of the noncoronary cusp.
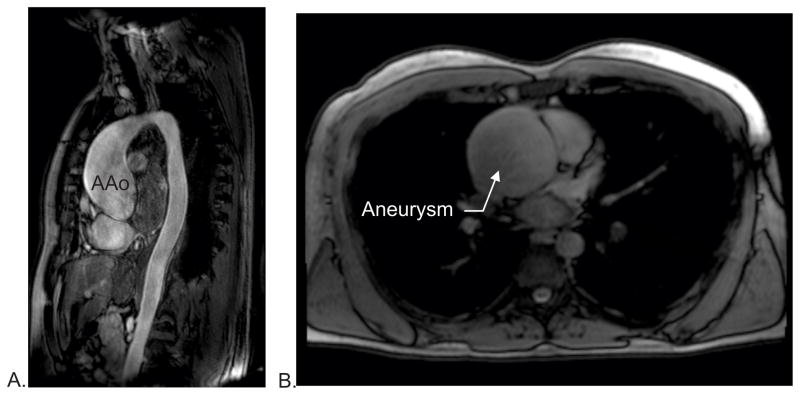
Figure 1.
Sagital (A) and axial (B) pre-operative MRI demonstrating a 6.1 × 6.3 cm ascending aorta (AAo) aneurysm.
To better understand the pre-operative flow characteristics in the large aneurysm and the impact of surgical repair and reconstruction on thoracic aorta hemodynamics, time-resolved three-dimensional phase contrast (4D flow) MRI was performed before and after surgery. The MRI examinations (pre: 3.0 T Skyra, post: 1.5 T Avanto, Siemens, Germany) included both 4D flow MRI (velocity sensitivity - pre:150 cm/s, post: 250 cm/s, spatial/temporal resolution – pre: 3.14×2.13×3.2 mm3/39 ms, post: 2.88×2.13×2.15 mm3/38ms) and dynamic 2D cine imaging of the heart (steady-state free precession, spatial/temporal resolution – pre: 1.25×1.25×6 mm3/29 ms post:1.8×1.8×6 mm3/39 ms). The study was approved by the local IRB, and informed consent was obtained from the patient.
Blood flow patterns within the thoracic aorta were visualized using time-resolved 3D pathlines to illustrate complex blood flow dynamics over the entire cardiac cycle (EnSight, CEI, North Carolina). In addition, 3D velocity streamlines drawn tangent to the time-resolved velocity field were employed to illustrate instantaneous flow dynamics in the thoracic aorta. Forward and retrograde flow, regurgitant fraction, and peak velocity were quantified at the aortic root, mid-ascending aorta, mid-arch, and proximal descending aorta.
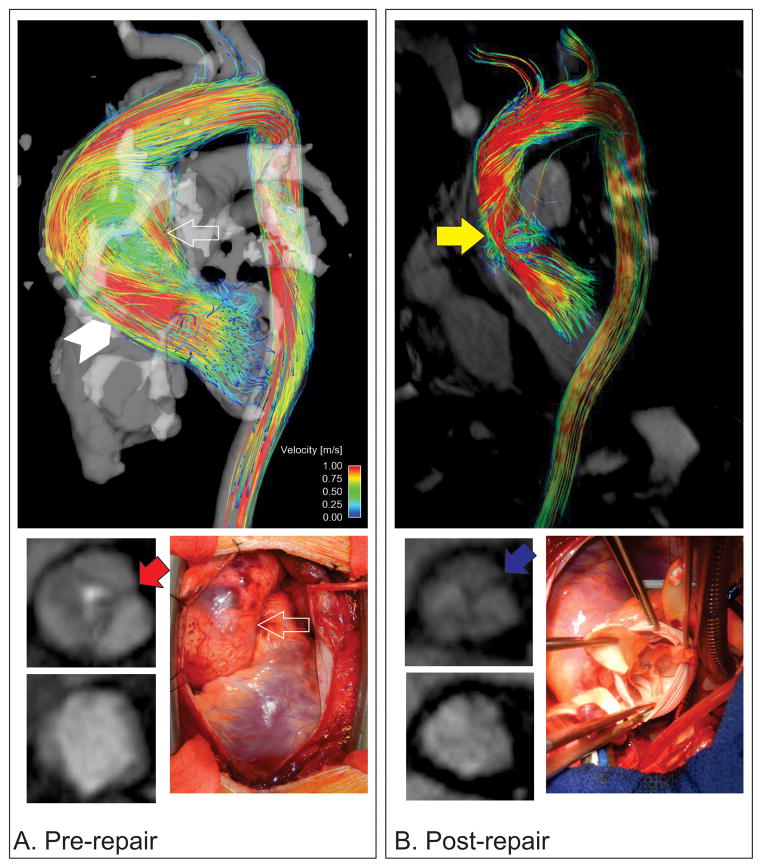
Pre-operative MRI findings and intraoperative photographs demonstrate the large aneurysm and BAV, and 4D flow analysis reveals the presence of an eccentric flow jet directed toward the posterolateral wall of the ascending aorta with the peak velocity (1.45 m/s) concentrated along the wall in this region (Figure 2A, Movies 1 and 2). The flow within the ascending aorta evolves into a large vortex that fills the aneurysm and results in large volume retrograde flow anteriorly within the ascending aorta. The downstream effects of this flow pattern in combination with moderate to severe aortic valve aortic valve insufficiency result in substantial distal flow reversal reflected by large retrograde flow fractions in the arch (29%) and proximal aorta (32%). Post-operative MRI shows grossly normalized aortic anatomy secondary to the aortic graft. Follow-up 4D flow analysis shows more uniform flow in the aortic root and the presence of a physiologically normal right handed helix in the ascending aorta (Figure 2B, Movies 3,4, and 5). There are greatly increased peak velocities at the aortic root (3.1 m/s), mid ascending aorta (2.5 m/s), arch (2.2 m/s), and descending aorta (2.43 m/s). Downstream retrograde flow fractions are decreased in comparison to pre-operative findings in the mid-ascending aorta (6.9%), arch (13.8%), and descending aorta (14.2%).
Figure 2.
Pre- and post-operative comparisons between 3D velocity streamlines generated from 4D flow data, intra-operative images, and aortic valve 2D phase contrast MRI images with valve open and closed (clockwise from top in each panel). A. A large vortex fills the ascending aorta aneurysm (white outlined arrow) and there is a high velocity, eccentric, systolic flow jet directed posterolaterally (white arrowhead). The right and left coronary cusps of the aortic valve are fused with a visible raphe (red arrow), and there is incomplete closure of the valve leaflets. B. High velocity flow is seen in a majority of the surgically repaired aorta (yellow arrow) with grossly normalized flow patterns. Intraoperative image shows the repaired aortic valve with Dacron graft. The aortic valve has been surgical repaired and now appears trileaflet after separation of the fused leaflets (blue arrow).
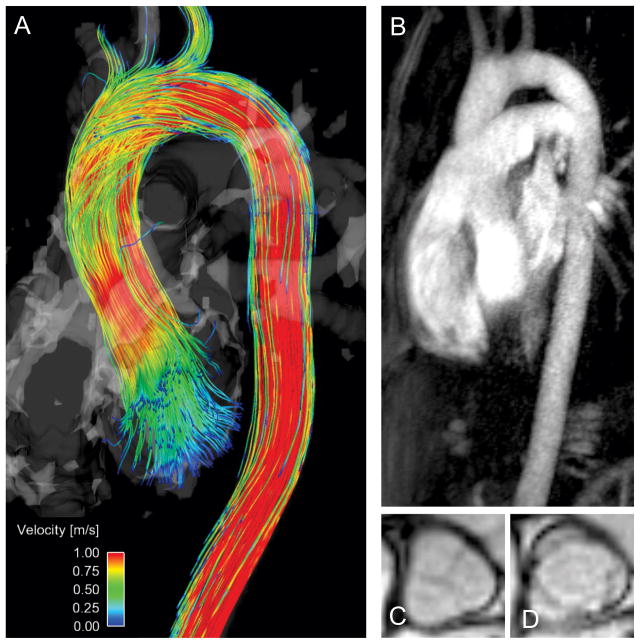
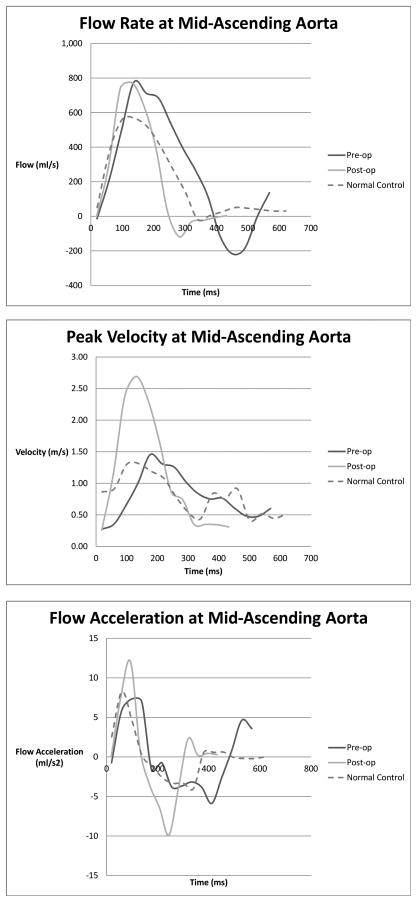
As a comparison, results of MRI assessment in a healthy 30-year-old male volunteer that included 4D flow, MR angiography of the thoracic aorta, and aortic valve imaging are provided in Figure 3 (Movie 6). In this subject, mild physiologic right-handed helix flow is present in the ascending aorta, with cohesive flow along length of the thoracic aorta. Peak systolic velocities were measured at the aortic root (1.33 m/s), mid ascending aorta (1.31 m/s), arch (1.27 m/s), and descending aorta (1.52 m/s). Retrograde flow fraction was <5% at all aortic regions. This case illustrates that flow patterns and quantifiable hemodynamic parameters within the aorta are highly dependent on aortic anatomy, and can be substantially influenced by surgical intervention. Eccentric flow jets have been associated with aorta diameter growth rates as well as an increase in serum markers that are correlated with the presence of aneurysm in patients with BAV.1 In patients with BAV, 4D flow MRI analysis has shown that eccentric high velocity flow jets are correlated with regionally increased wall shear stress.2 The combination of flow jet angle and wall shear stress is likely to contribute to aneurysm growth as a consequence of fluid-mechanical shear forces triggering a cell signaling cascade which may influence molecular changes within the vessel wall.1, 2 The dramatic increase in post-operative velocities after surgical anatomic repair are likely the result of lower compliance in the Dacron aortic graft relative to physiologic tissues, thus leading to increased bulk flow acceleration along the aorta (Figure 4). Decreased aortic compliance will result in decreased Windkessel effects and may decrease physiologic flow to the coronary arteries and other downstream vascular beds during diastole3. Reduced elasticity of the graft compared to the normal aortic wall will also result in an increased pulse wave velocity and reflected wave amplitude that has been associated with an increase in hypertensive end-organ damage and may explain the continued presence of elevated retrograde fractions observed in our patient even after aortic valve repair.4
Figure 3.
MRI imaging in a normal volunteer. A: 3D velocity streamlines generated from 4D flow data in the thoracic aorta. Note the presences of physiologic right-handed helix flow in the proximal ascending aorta. B. MR angiography of the thoracic aorta and pulmonary artery. C, D: Normal tricuspid aortic valve in diastole and systole.
Figure 4.
Quantitative analysis of flow in the mid-ascending aorta of a normal volunteer and in the patient pre- and post-operatively. In the patient, post-operative peak velocity is dramatically increased and there is rapid flow acceleration and deceleration during systole indicative of a loss of reduced compliance of the Dacron graft. Relative to the normal volunteer, both pre- and postoperative flow analyses demonstrated higher flow, greater peak velocities, and greater bulk flow acceleration.
In conclusion, in-vivo analysis of aortic 3D hemodynamics in this patient reveals marked flow alterations after valve sparing root replacement with aortic valve repair. Physiologic 3D flow patterns were normalized, but there is substantially increased flow velocity and flow acceleration that may result in increased post-intervention left ventricular afterload and increase the risk of end-organ damage.4 The use of 4D flow MRI to assess the interplay between complex 3D temporal/spatial flow characteristics and clinical outcomes enhances the capability of clinicians to provide data-driven options regarding risk-stratification and treatment modalities, as well as offering new insights for improved surgical devices and techniques to better approximate physiologic conditions.
Supplementary Material
Acknowledgments
Funding Sources: NIH NHLBI grant R01HL115828; NUCATS Institute NIH grant UL1RR025741, and the Northwestern Memorial Foundation Dixon Translational Research Grants Initiative; American Heart Association Scientist Development Grant 13SDG14360004.
Footnotes
Conflict of Interest Disclosures: None.
References
- 1.den Reijer PM, Sallee D, 3rd, van der Velden P, Zaaijer ER, Parks WJ, Ramamurthy S, Robbie TQ, Donati G, Lamphier C, Beekman RP, Brummer ME. Hemodynamic predictors of aortic dilatation in bicuspid aortic valve by velocity-encoded cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2010;12:4. doi: 10.1186/1532-429X-12-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barker AJ, Markl M, Burk J, Lorenz R, Bock J, Bauer S, Schulz-Menger J, von Knobelsdorff-Brenkenhoff F. Bicuspid aortic valve is associated with altered wall shear stress in the ascending aorta. Circ Cardiovasc Imaging. 2012;5:457–466. doi: 10.1161/CIRCIMAGING.112.973370. [DOI] [PubMed] [Google Scholar]
- 3.Kingwell BA, Waddell TK, Medley TL, Cameron JD, Dart AM. Large artery stiffness predicts ischemic threshold in patients with coronary artery disease. J Am Coll Cardiol. 2002;40:773–779. doi: 10.1016/s0735-1097(02)02009-0. [DOI] [PubMed] [Google Scholar]
- 4.Weber T, Wassertheurer S, Rammer M, Haiden A, Hametner B, Eber B. Wave reflections, assessed with a novel method for pulse wave separation, are associated with end-organ damage and clinical outcomes. Hypertension. 2012;60:534–541. doi: 10.1161/HYPERTENSIONAHA.112.194571. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.