Abstract
Using the universe of patient transitions from inpatient hospital care to skilled nursing facilities and home health care in 2005, we show how integration eliminates task misallocation problems between organizations. We find that vertical integration allows hospitals to shift patient recovery tasks downstream to lower-cost organizations by discharging patients earlier (and in poorer health) and increasing post-hospitalization service intensity. While integration facilitates a shift in the allocation of tasks and resources, health outcomes either improved or were unaffected by integration on average. The evidence suggests that integration solves coordination problems that arise in market exchange through improvements in the allocation of tasks across care settings.
1.Introduction
This paper examines how integration solves task allocation problems between organizations. In particular, we focus on timing problems in market exchange that arise from the misallocation of tasks between two vertically distinct stages of production. Since the seminal work of Masten, Meehan and Snyder (1991) scholars have made great progress toward understanding how timing problems in market exchange influence vertical integration. For example, Nickerson and Silverman (2003) demonstrate that trucking firms vertically integrate in the less-than-truckload (LTL) segment to avoid disruption of closely coordinated breakbulk operations, and Forbes and Lederman (2009) show how the risk of cascading delays lead major airlines to own regional carriers that operate routes originating or terminating at the majors’ hubs (or other cities that are important to the majors’ network). We build on the idea that the timing of exchange influences transactional efficiency, and thereby vertical integration. However, instead of studying timing as an adaptation problem (Nickerson and Silverman 2003; Masten, Meehan and Synder 1991; Forbes and Lederman 2009), we focus instead on timing issues stemming from the misallocation of tasks to assets (or sites) that may arise under bilateral market exchange.1
We test the idea that the misallocation of tasks across sites of production has performance implications in the context of the patient care continuum, where patients transition across organizational settings, from acute care facilities (hospitals) into post-acute care (nursing homes and home health). The empirical application demonstrates the role of task allocation in influencing the efficiency of transactions and firm boundary decisions. Taking the sequence of clinical interventions (or tasks) along the care continuum as fixed—patients need a well-defined set of clinical interventions to address their health care needs—exchange is, therefore, characterized solely by the timing of transitions across settings. Systematic variation in cost structures and reimbursement rates between hospitals and post-acute care providers coupled with regulatory restrictions on side-payments (which represent a strong form of contractual incompleteness) ensures that tasks will not be efficiently assigned unless the hospital and downstream providers are vertically integrated. However, integration costs are non-trivial such that there is substantial heterogeneity in governance regimes: about one-third of nursing homes and home health agencies are vertically integrated into hospitals.
One major advantage of our empirical design is that we can track patients across organizations, which allows us to pinpoint how integration influences tasks on both sides of the exchange relationship. The ability to observe the clinical procedures patients receive in post-acute care at a high-level of detail is particularly important to our empirical assessment of patient health at the time of discharge. A second advantage of our empirical approach is that health markets are distinct and heterogeneous, allowing us to exploit exogenous variation in local market conditions as part of our empirical strategy. In particular, we use other hospital’s vertical integration status in the same geographic market as instrumental variable that is correlated with the costs and benefits of integration, but uncorrelated with a focal hospital’s discharge decisions.
The evidence shows that, on average, vertical integration leads to shorter hospital stays for patients discharged to post-acute care. We also find that patients received higher intensity of care from vertically integrated home health providers. The results support the central thesis of the paper: integration changes the allocation of tasks across organizational settings to achieve efficiency. Notably, while we find striking differences in the organization of services across sites, vertical integration does not lead to a decline in patient health outcomes, suggesting that different allocations of tasks across sites produces similar levels of care quality.
The results contribute to the literature on firm boundaries by demonstrating how integration changes the allocation of tasks to assets and, thereby, mitigates inefficiencies in market exchange that arise even in the absence of cascading organizational problems typically described in the literature on timing and vertical integration (Masten, Mehan and Snyder 1991; Pirrong 1993; Nickerson and Silverman 2003; Forbes and Lederman 2009, 2010). Moreover, given the result that tasks are misallocated across non-integrated organizations along with the assumption that the fixed costs of vertical integration are heterogeneous; the evidence can explain why we observe a mix of integrated and non-integrated organizational forms in this segment of the industry.
2.Theory and related literature
When counterparties’ objectives conflict with respect to a focal task and contracts are incomplete (i.e., due to regulation of side-payments, as in our application), market exchange will likely fail to generate the optimal allocation of tasks. In such cases, vertical restraints will not yield the efficient level of task allocation achieved through vertical integration; and even though hierarchical governance leads to bureaucratic costs under integration, the misallocation of tasks under market exchange can generate costs that would justify integration. The conceptual approach, discussed in more detail below, is formalized in David, Rawley, and Polsky (2011).
By examining the relationship between vertical integration and task allocation we build on an emerging literature that links vertical integration to adaptation and performance. For example, Novak and Stern (2008) show how vertical integration allows automobile manufactures to adapt to unforeseen contingencies, and Forbes and Lederman (2010) demonstrate that vertical integration facilities real-time adaptation decisions between major airlines and their regional partners. However, rather than focusing on adaptation mechanisms, our approach emphasizes the implication of joint decision-making (i.e., integration) on task allocation. Our emphasis on task allocation is similar in spirit to the concept of temporal specificity, which locates the source of contracting problems in the timely production or delivery of goods or services (Masten, Meehan and Snyder 1991).
As is standard in the temporal specificity literature, we assume that production takes a sequential form in which a sequence of tasks leads to production of an output. For example, Pirrong (1993) studies timing problems in the context of the bulk shipping market where shipping must follow production and precede sales in a pre-determined sequence, and contracting over the timing of shipments can lead to inefficiencies because capacity “spoils” if it is not filled when a ship leaves the harbor. Similarly, in our context, given a technologically determined sequence of production, beginning with a clinical intervention (e.g. surgery) followed by patient monitoring and recovery, and ending with nursing services to ensure full recovery or management of a chronic illness, we examine how the boundaries of firms along the patient care continuum vary in the response to task allocation problems.
We extend the literature on timing problems in market exchange by highlighting the role of task allocation in influencing firm boundaries. While acknowledging the fundamental insight in the extant literature—that temporal considerations can create coordination problems that influence the efficiency of exchange—we focus on the less well understand implication of the impact of task misallocation on transactional performance by analyzing how the partitioning of the sequence of tasks across organizations (or sites) influences production efficiencies. Thus, we propose that an important class of timing problems need not necessarily arise from cascading effects that create externalities for the rest of the organization through ripple effects inside firms within network industries, as is well documented in the literature, but can also be due to fundamental differences between firms over the optimal allocation of production tasks to assets (or sites), which can lead to inefficiencies in market-based exchange.
We analyze the allocation of tasks to sites of production in the case of a two-way vertical exchange relationship, using a framework where contracts are inherently incomplete. As is standard in the literature, we define integration as the joining of assets under unified management (Klein, Crawford and Alchian 1978; Williamson 2010). Transactions are characterized by exchanges between assets (or sites), and tasks are production activities used in conjunction with assets to produce outputs for exchange, where, for tractability, the sequence of tasks needed to achieve an outcome is assumed to be technologically pre-determined. As is common in the theory of the firm literature, we assume that integration results in increased bureaucratic costs, arising from the management of different lines of business. Our key insight is that in the case of vertical integration, the allocation of tasks is internal to the firm, while in the case of market exchange, the allocation is the result of a bargaining process. Note that if all tasks are performed in conjunction with a particular site, tasks and assets are redundant constructs and task allocation has no substantive meaning beyond the standard incomplete contracting models of vertical integration. In our framework, however, when some tasks are not site-dedicated, misallocation of such tasks across sites forms the basis for the cost of market exchange.
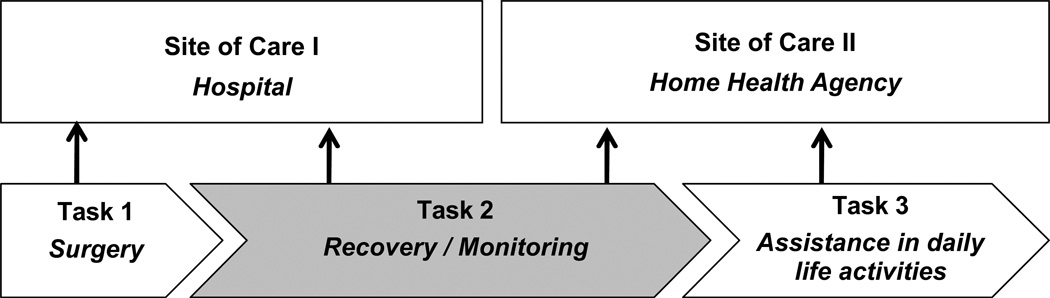
From these foundations, we propose that the allocation of tasks to sites shapes firm boundaries by influencing production costs. Following the discussion above, we divide tasks into two groups: tasks dedicated to a particular site and tasks that can be performed at multiple sites. The first class of tasks—site-dedicated tasks—represent the focal source of governance costs, as the management of heterogeneous site-task pairs within a single firm requires costly managerial oversight (Schoar 2002). By definition, site-dedicated tasks are always allocated efficiently, as these tasks never cross the boundaries of their corresponding sites. Our second class of tasks, general tasks, are of particular interest, as they may span sites—that is, in an exchange relationship between two sites, both sites are technologically capable of performing the general tasks—and, therefore, may be allocated to sites differently under integration versus market exchange. Thus, in the presence of incomplete contracts, vertical integration represents a tradeoff between incurring administrative inefficiencies from governing additional site-dedicated tasks against the benefits of allocating general tasks optimally to sites. In our application, a major clinical intervention (e.g., surgery) is a hospital-dedicated task, while assistance with daily activities is a home health-dedicated task. Patient recovery, on the other hand, is an example of a general task that may span both acute and post-acute care settings (see Figure 1).
Figure 1.
An illustration of asset-dedicated and general tasks along the care continuum
Notes: surgical interventions, which are hospital-dedicated tasks, are always performed in acute care sites (i.e., hospitals), while assistance in daily home activities, which are post-acute-dedicated tasks, are always performed at the patient’s residence or in a nursing home. Recovery/Monitoring, to a large extent, is a general task, which can be performed at the hospital or in a post-acute care setting. Vertical integration gives the firm control over the allocation of this general task.
The misallocation of general tasks is the primary source of transaction costs in our framework, as market exchange can distort the allocation of tasks across sites. The tension between the bureaucratic costs of integration and the cost of inefficiencies associated with market exchange leads to two alternative second best solutions to the problem of exchange. A first best solution can be achieved if firms maximize joint surplus, and contract to share the additional surplus from cooperatively choosing the allocation of general tasks. However, when contracts are incomplete, tasks will not be assigned to maximize joint surplus—the externality imposed on their exchange partners will not be internalized—and, therefore, market exchange is likely to distort the efficient allocation of general tasks. By contrast, integration allows the firm to correct production inefficiencies associated with market exchange by shifting general tasks either downstream or upstream. Nevertheless, integration dampens incentives and creates bureaucracy costs that are avoided under market exchange. Thus, while our theory is consistent with transaction cost economics models, which highlight the tension between transaction costs and hierarchical governance costs (Williamson 1985), we explicitly consider transaction costs in terms of production inefficiencies associated with task misallocation.
Our approach is also similar to Corts’s (2006) analysis of the allocation of tasks to assets. In Corts’s (2006) model a single asset (a truck) and a potentially delegable task (maintenance) is allocated between a principal (a firm) and an agent (a driver). When the principal delegates the maintenance task downstream, efficiency dictates asset ownership by the agent, which in turn results in greater effort in performing the delegated task. As in his model, we also link task allocation and asset ownership, but in Corts’s (2006) model principal asset ownership hinders the delegation of tasks to the agent. In contrast, our analysis relies on the notion that asset (or site) ownership facilitates task delegation to achieve an efficient allocation of tasks.
It is important to note that contractual incompleteness and the existence of general tasks are not sufficient to produce inefficiencies in market exchange. There also must be a divergence in the preferences of firms regarding how general tasks are to be divided among them. If both firms strictly preferred the optimal allocation of general tasks, market exchange would achieve the first best solution. As a case in point, consider the hospice industry, which provides palliative care for terminally ill patients. Unlike the case of home health or nursing home care, candidates for hospice care are dying, not recovering. Therefore, delaying discharge to hospice means that patients transition when they are sicker. Moreover, hospice providers are paid per day while the cost of care typically rises as the patient deteriorates; therefore, both hospitals and hospice providers benefit economically when patients are discharged from the hospital earlier. The lack of conflict suggests a diminished role for vertical integration. Consistent with the idea that preferences over the timing of exchange drive vertical integration decisions we observe that while 31% of home health agencies and 36% of skilled nursing facilities are vertically integrated, only 17% of hospices are owned and operated by hospitals.
3. Empirical context: Patient transitions from hospitals to post-acute-care settings
To focus our predictions, we map the theoretical constructs developed in section 2 (above) to our empirical setting. We test the predictions of the theory by comparing practice patterns between vertically integrated (i.e., hospitals with home health agencies and hospitals with skilled nursing facilities) and non-integrated providers along the care-continuum from acute to post-acute care settings. Health care organizations on both sides of the hospital to post-acute care exchange have divergent preferences regarding the partition of the general task; because both hospitals and home health agencies are paid prospectively, each entity would like the other to oversee patient recovery. Hospitals gain from early patient discharge while home health agencies gain from admitting patients later in the process. Since, on the margin, recovery under post-acute care is less costly, hospitals would be willing to pay post-acute care entities to accept patients sooner, but side-payments are illegal in health care (due to fear that referrals will be governed by financial interest, as opposed to clinical considerations). Therefore, inefficiency with regard to the timing of discharge arises under market exchange and is resolved under integration.
The empirical context is particularly appealing for a number of reasons. First, the health care industry is large: in 2007, national expenditures were $190 billion in nursing homes and home health care and $696 billion in hospitals. Second, contracts are inherently incomplete between hospitals and post-acute care providers because they are subject to fixed prices set by Medicare with strict prohibitions on side payments between hospitals and post-acute providers. Fixed price exchange gives rise to incomplete contracting because the counterparties cannot use price to adjust for supply and demand imbalances in bilateral exchange. Limitations on side payments make it difficult for relational contracts to remedy the rigidities of fixed price exchange. Third, there is substantial cross-sectional variation in vertical integration into both skilled nursing facilities and home health across hospitals, which suggests that the costs and benefits of integration vary meaningfully across organizations in our setting. Fourth, there are clear cut site-dedicated and general tasks in this setting, and the timing of exchange influences the efficiency of care in a direct and important way. Hospitals perform specialized hospital-dedicated acute care tasks, such as surgery, but once patients are stabilized, post-operative care rapidly becomes a task that need not necessarily be bundled with the physical infrastructure of a hospital (i.e. post-operative care becomes a general task once the patient is stabilized). Home health agencies and skilled nursing facilities also deliver site-dedicated and general tasks, providing care services that are only performed in patients’ homes2 or in a skilled nursing facility,3 and assisting recuperating patients in a manner that is customized to their living environment, but also by offering a range of services that could be provided in a hospital setting, particularly monitoring, therapy, and recovery services. These general tasks are produced at much higher cost in a hospital setting compared with a post-acute setting primarily due to the higher opportunity cost of a hospital bed (Candrilli and Mauskopf 2006, MetLife 2009), which, when coupled with incomplete contracts, creates coordination costs and provides the impetus for vertical integration. Fifth, the health services industry is a collection of hundreds of distinct local markets producing roughly homogenous outputs. We exploit variation in local market conditions in our empirical design to overcome the effect of selection on unobservables to identify the impact of vertical integration on health outcomes; yet, the homogenous nature of outputs across markets facilitates an accurate comparison of the effects of vertical integration on hospitals across markets. Finally, we have access to a large and novel dataset on hundreds of thousands of patients’ medical history records that tracks their care across facilities, allowing us to measure the impact of vertical integration on the allocation of tasks to sites at an unusual level of detail.
Medicare reimburses care delivered by home health agencies and skilled nursing facilities through a Prospective Payment System (PPS). Under PPS for home care, a fixed reimbursement is given for a 60-day episode independent of the number of visits during the episode. Reimbursement is fixed and prospective. The amount of reimbursement is set at admission, and while it is indexed to the severity of the patient's condition and local labor costs, the reimbursement rate is a purely administrative price, which may not be directly related to the cost of managing the patient, and is not altered based on the intensity of care delivered.4 In the case of skilled nursing facilities, reimbursement is given for each day of stay (up to 100 days) independent of the intensity of care while at the facility. Within this reimbursement strategy, skilled nursing facilities and home health agencies are free to provide the intensity of care that they deem appropriate for their patient. In general, the amount of service provided does not change the amount of reimbursement, which strengthens the foundation for our assumption that contracts are incomplete in our empirical context.5 Though the payment process is different, admitting a patient earlier to either a home health agency or to a skilled nursing facility erodes margins downstream, as it is more costly to care for patients who are still in intensive stages of recovery. Thus, even though skilled nursing facilities are reimbursed per day instead of per episode their incentives are still not well aligned with the hospital’s, which wants to discharge patients as soon as they are stabilized.
Hospitals are also reimbursed through a prospective payment system, the Inpatient Prospective Payment System (IPPS). Under IPPS, each admission is categorized into a diagnostic-related group (DRG) which has a payment assigned to it based on the expected intensity of resources used to treat that DRG. Rare and unusually costly cases get an increased payment, but despite this, there is no incentive for hospitals to keep their patients longer than medically necessary. Indeed, hospitals focus intensely on managing inpatient costs conditional on physicians’ medical opinions about the ability of the patient to recover outside of the hospital setting through the discharge planning process.
Discharge planning is a professional process that customizes a unique plan for moving a patient from one level of care to another (Collier and Harrington, 2005). The American Medical Association and the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO) offer recommendations for discharge planning, however, their recommendations are not binding and there is heterogeneity in the discharge process across hospitals (Chiplin, 2005; Moore et al., 2007). While only physicians can authorize a patient discharge, the actual process of discharge planning is handled by social workers, nurses, case managers, and discharge planners (Naylor et al., 1994). These hospital agents communicate with their counterparts at post-acute care entities to facilitate patient transitions on case-by-case basis.
The interaction between hospital and post-acute care provider over a patient’s discharge can be characterized as a bargaining process, where bargaining over the timing of exchange yields inefficiencies in the sense that the parties will not maximize joint surplus. Post-acute care providers are not required to accept a patient, and in general, have an incentive to convince the hospital that they should discharge the patient to them at a later date. Of course, in practice, there is some give and take in the negotiating process—not every patient is haggled over—and market power undeniably influences the outcomes of the bargaining game. But, the fundamental implication of market exchange is clear: on the margin non-integrated post-acute care providers can delay the discharge process.
Given incomplete contracts and general tasks that may be performed at either hospital or post-acute care sites vertical integration should result in improved task allocation. In particular, we examine whether hospitals that are vertically integrated discharge their patients to skilled nursing facilities and home health agencies sooner (Hypothesis 1) and when the patients are in poorer health compared to non-integrated hospitals (Hypothesis 2). The two predictions arise directly from the idea that vertical integration allows hospitals to allocate general tasks (i.e., recovery tasks) to their own skilled nursing facility and home health agency in a manner that is more efficient than under market exchange, subject to a bureaucratic cost penalty for integrating acute and post-acute organizations. Taking the integration penalty to be positive but of a magnitude that varies by upstream firm-downstream firm pair based on exogenous factors such as the availability of land near the hospital for building a skilled nursing facility (it is generally easier to manage a post-acute care facility when it is close to the hospital), the relatedness of post-acute care provision to the hospital’s portfolio of services (unrelated services are typically thought to be more expensive to provide), or the extent to which post-acute care provision is considered to be central to the hospital’s mission (which changes the willingness of the hospital to incur an integration cost), we can infer the nature of the benefits of vertical integration by studying the behavior of efficiency maximizing hospitals. Our conceptual framework suggests that vertically integrated firms will improve the efficiency of the allocation of tasks by shifting the general task to the low-cost provider sooner, here the skilled nursing facility or home health agency. Thus, it follows that vertically integrated hospitals will allocate recovery tasks to the downstream firm by shifting patients sooner in the recovery process and when they are in worse health.6 Since we have assumed throughout that post-acute care providers will respond to early transitions by increasing the intensity of care downstream, we also subject the data to a further test by stating this premise as a hypothesis: on average, the quality of care patients receive should not decline when the timing of the transition is accelerated (Hypothesis 3).
4. Data and samples
Having shown how the concept of task allocation applies, in the context of patient care, we now turn to the empirical analysis. Our core data come from the Medicare Provider and Analysis Review (MEDPAR) Files for 2005. The MEDPAR is a research file compiled by the Center for Medicare and Medicaid Services, based on the billing claims of facility stays for fee-for-service Medicare beneficiaries. Each MEDPAR record represents a facility stay including acute-care-hospital stays and skilled nursing facility stays. It summarizes services provided to a beneficiary from time of admission to a facility through discharge. Each record includes: date of admission and discharge; codes procedures and diagnoses (DRG); socioeconomic information; the patient’s zip code; and a unique identification number that is specific to a beneficiary and the hospital. This is a near-complete record of health care facility encounters for Americans over 65.7
To identify and characterize post-acute care home health care episodes that follow hospitalizations, we link the MEDPAR file acute-care-hospital stays to the Medicare claims for skilled nursing facilities and home health services by the scrambled identifier of the Medicare beneficiary. Home health services are recorded on the Medicare Home Health Agency Standard Analytical Files. We identify admissions to skilled nursing facilities and home health care agencies as those occurring within 3 days of the hospital discharge. Because all qualifying skilled nursing facility and home health care episodes of Medicare beneficiaries are paid by Medicare, these claims files are a complete record of home health use for the beneficiaries with MEDPAR hospitalizations. We also capture data on home health care services provided, including number of home health visits, the dates and types of visits as well as unique home health agency identifiers.
The claims data is augmented with survey data on hospitals from the American Hospital Association (2005) and with data from the 2005 Hospital Cost Reports and the 2005 Provider of Service Files. We use these three data sources to determine whether hospitals are vertically integrated into skilled nursing facilities and into home health, conservatively coding hospitals as vertically integrated when all three sources agree, though our results are robust to other criteria.
Our analysis focuses on MEDPAR hospitalizations for new health events that resulted in post-acute care admissions either directly into skilled nursing facilities or into home health. We exclude hospitalizations of existing health events from our sample, MEDPAR hospitalizations that were preceded in the 90 days prior to admission by a hospitalization or by post-acute care with a home health agency or in a skilled nursing or rehabilitation facility (though the results are not sensitive to this exclusion). We then eliminate all hospitals with indeterminate vertical integration status (20% of the sample), leaving us with 399,616 discharges to home health and 460,761 discharges to skilled nursing facilities from 2,571 hospitals.
Table1-A displays shows summary statistics for patients discharged to home health. Columns (1) and (2) show the means and the standard deviations for the full sample. Medicare patients are elderly; the average age is 78, primarily female (62%) and white (88%). On average, patients in the home health hospital discharge sample have between one and two additional serious diseases that are not directly related to their hospitalization event (1.45 co-morbidities), are admitted to hospitals 48.5 miles from their home (median distance is 7 miles), and average length of stay—the number of days the patient remains in the hospital—is approximately 6 days. 5% of patient discharges to home health are to home health centers that are co-located with the discharging hospital (co-located is defined as being located within 0.1 miles). 31% of patient discharges go to vertically integrated home health agencies, and approximately two-thirds of these patient discharges (21% of all patient discharges) come from the parent hospital of these agencies.8 Approximately one-quarter of transfers to integrated home health agencies come from non-integrated hospitals (8% of all patient discharges). Home health intensity for the home health hospital discharge population is approximately one visit every three days.
Table 1.
| A Descriptive statistics for key variables: home health (HHA) | ||||
|---|---|---|---|---|
| Full sample n=399,616 |
non-VI hosp. n=270,165 |
VI hosp. N=129,451 |
||
| (1) | (2) | (3) | (4) | |
| Patient characteristics | Mean | Stdv | Mean | Mean |
| Length of stay (days) | 5.86 | 4.96 | 5.89 | 5.86 |
| Age (years) | 78.1 | 7.56 | 78.1 | 78.2 |
| Male | 0.38 | 0.49 | 0.38 | 0.38 |
| White | 0.88 | 0.32 | 0.87 | 0.91 |
| Black | 0.08 | 0.27 | 0.09 | 0.07 |
| Number of comorbities | 1.45 | 1.18 | 1.44 | 1.46 |
| Chronic lung disease | 0.20 | 0.40 | 0.20 | 0.21 |
| Diabetes | 0.19 | 0.39 | 0.19 | 0.19 |
| Cong. heart failure | 0.10 | 0.30 | 0.10 | 0.11 |
| Distance to home from hospital (miles) | 18.4 | 28.5 | 19.0 | 17.1 |
| Hospital characteristics | ||||
| Vert. integrated into home health (VI_HOSP) | 0.32 | 0.47 | 0.00 | 1.00 |
| Co-located with a home health center | 0.05 | 0.23 | 0.02 | 0.13 |
| Rehospitalization rate | 0.17 | 0.37 | 0.17 | 0.17 |
| For-profit | 0.14 | 0.35 | 0.19 | 0.03 |
| Government | 0.11 | 0.31 | 0.09 | 0.14 |
| Teaching hospital | 0.22 | 0.42 | 0.23 | 0.21 |
| Total beds | 381 | 266 | 382 | 379 |
| Home health agency characteristics* | ||||
| Home health intensity (visits/day) | 0.38 | 0.21 | 0.38 | 0.38 |
| Vertically integrated (VI_HHA) | 0.31 | 0.46 | 0.11 | 0.72 |
| Within firm transfer (VI_HOSP_TX) | 0.21 | 0.41 | 0.00 | 0.65 |
| VI_HOSP to other HHA (VI_HOSP_EXT) | 0.11 | 0.32 | 0.00 | 0.35 |
| VI_HOSP to non-VI_HHA (VI_EXT_NON) | 0.09 | 0.29 | 0.00 | 0.28 |
| VI_HOSP to other VI_HHA (VI_EXT_VI) | 0.02 | 0.15 | 0.00 | 0.08 |
| Non-VI_HOSP to VI_HHA (VI_HHA_IN) | 0.08 | 0.26 | 0.11 | 0.00 |
| Market characteristics (counties) | ||||
| Others vert. int. into home health (VI_HOSP-h) | 0.29 | 0.23 | 0.25 | 0.36 |
| Hospital concentration | 752 | 1,288 | 691 | 878 |
| SNF concentration | 221 | 423 | 201 | 262 |
| Home health concentration | 508 | 675 | 488 | 550 |
| % population <9 yr school | 7.27 | 4.41 | 7.22 | 7.36 |
| % population college graduates | 23.62 | 9.47 | 24.43 | 21.93 |
| Median HH income ($K) | 47.25 | 12.44 | 48.04 | 45.62 |
| % population aged 65+ | 13.52 | 4.01 | 13.34 | 13.89 |
| Metropolitan area dummy | 0.80 | 0.40 | 0.84 | 0.72 |
| Population density (pop./square miles) | 2,018 | 6,764 | 2,407 | 1,209 |
| Hospital beds | 2,588 | 4,472 | 2,920 | 1,898 |
| Long term care hosp. beds | 182 | 406 | 207 | 131 |
| Skilled nursing facility beds | 3,894 | 6,566 | 4,291 | 3,071 |
| % 15–44 female pop. | 20.91 | 2.24 | 21.00 | 20.72 |
| HMO enrollment rate | 0.62 | 0.25 | 0.65 | 0.56 |
| B Descriptive statistics for key variables: skilled nursing facility (SNF) | ||||
|---|---|---|---|---|
| Full sample n=460,761 |
Non VI hosp. n=294,059 |
VI hospitals n=166,702 |
||
| (1) | (2) | (3) | (4) | |
| Patient characteristics | Mean | Stdv | Mean | Mean |
| Length of stay (days) | 6.92 | 6.15 | 7.02 | 6.76 |
| Age (years) | 81.47 | 7.60 | 81.67 | 81.14 |
| Male | 0.28 | 0.45 | 0.28 | 0.29 |
| White | 0.90 | 0.30 | 0.90 | 0.90 |
| Black | 0.07 | 0.26 | 0.07 | 0.07 |
| Number of comorbities | 1.71 | 1.21 | 1.71 | 1.69 |
| Chronic lung disease | 0.19 | 0.40 | 0.19 | 0.20 |
| Diabetes | 0.17 | 0.38 | 0.17 | 0.18 |
| Cong. heart failure | 0.14 | 0.35 | 0.14 | 0.15 |
| Hypertension | 0.14 | 0.34 | 0.14 | 0.14 |
| Distance to home from hospital (miles) | 18.3 | 32.0 | 18.7 | 17.6 |
| Hospital characteristics | ||||
| Vertically integrated into SNF (VI_HOSP) | 0.36 | 0.48 | 0.00 | 1.00 |
| Co-located with a SNF | 0.23 | 0.46 | 0.26 | 0.38 |
| Rehospitalization rate | 0.20 | 0.40 | 0.20 | 0.19 |
| For-profit | 0.12 | 0.32 | 0.13 | 0.08 |
| Government | 0.10 | 0.30 | 0.10 | 0.10 |
| Teaching hospital | 0.20 | 0.40 | 0.21 | 0.17 |
| Total beds | 356 | 247 | 355 | 358 |
| Skilled nursing facility characteristics* | ||||
| Vertically integrated (VI_SNF) | 0.21 | 0.41 | 0.03 | 0.53 |
| Within firm transfer (VI_HOSP_TX) | 0.19 | 0.39 | 0.00 | 0.51 |
| VI_HOSP to other SNF (VI_HOSP_EXT) | 0.18 | 0.38 | 0.00 | 0.49 |
| VI_HOSP to non-VI_SNF (VI_EXT_NON) | 0.17 | 0.38 | 0.00 | 0.47 |
| VI_HOSP to other VI_SNF (VI_EXT_VI) | 0.01 | 0.08 | 0.00 | 0.02 |
| Non-VI_HOSP to VI_SNF (VI_SNF_IN) | 0.02 | 0.14 | 0.03 | 0.00 |
| Market characteristics (counties) | ||||
| Others vertically integrated (VI_HOSP-h) | 0.30 | 0.23 | 0.28 | 0.32 |
| Hospital concentration | 744 | 1,279 | 762 | 711 |
| SNF concentration | 229 | 461 | 217 | 248 |
| Home health concentration | 493 | 658 | 509 | 464 |
| % population <9 yr school | 6.89 | 3.88 | 6.72 | 7.18 |
| % population college graduates | 24.15 | 9.42 | 24.93 | 22.77 |
| Median HH income ($K) | 48.20 | 12.34 | 49.29 | 46.28 |
| % population aged 65+ | 13.40 | 3.79 | 13.27 | 13.64 |
| Metropolitan area dummy | 0.81 | 0.39 | 0.83 | 0.76 |
| Population density (pop./square miles) | 1,644 | 5,006 | 1,862 | 1,260 |
| Hospital beds | 2,539 | 4,497 | 2,496 | 2,615 |
| Long term care hosp. beds | 181 | 382 | 172 | 195 |
| Skilled nursing facility beds | 3,991 | 6,748 | 3,944 | 4,072 |
| % 15–44 female pop. | 20.99 | 2.12 | 20.99 | 20.99 |
| HMO enrollment rate | 0.63 | 0.25 | 0.65 | 0.59 |
VI_HOSP = VI_HOSP_TX + VI_HOSP_EXT. VI_HOSP_EXT = VI_EXT_NON + VI_EXT_VI. VI_HHA = VI_HOSP_TX + VI_EXT_VI + VI_HHA_IN.
VI_HOSP = VI_HOSP_TX + VI_HOSP_EXT. VI_HOSP_EXT = VI_EXT_NON + VI_EXT_VI. VI_SNF = VI_HOSP_TX + VI_SNF_IN + VI_EXT_VI.
Our main explanatory variable is whether a hospital is vertically integrated into home health (VI_HOSP), a binary variable that is equal to one if a hospital owns at least one home health agency and zero otherwise. Columns (3) and (4) show the means of the covariates by observations from non-integrated and integrated hospitals, respectively. Integrated hospitals are clearly different from non-integrated hospitals; for example, they are less likely to be for-profit more likely to be government hospitals, and operate less frequently in dense urban areas. As we discuss in more detail below, we deal with this issue by creating a matched sample of patients from vertically integrated and non-integrated hospitals on all observable characteristics, as well as through instrumental variables techniques.
Table 1-B shows summary statistics for patients discharged to skilled nursing facilities. The mean and standard deviation of skilled nursing facility discharges are shown in columns (1) and (2) respectively. Medicare patients discharged to skilled nursing facilities are somewhat older (average age of 81 years), in worse health (1.71 co-morbid conditions), and more female (72%) than Medicare patients discharged to home health. They also stay longer in the hospital before being discharged (about a day longer), and are more likely to be discharged to a co-located facility: 36% of patient discharges to skilled nursing facilities (SNFs) go to SNFs that are co-located with the discharging hospital. For these tests, vertical integration (VI_HOSP) is defined by whether the hospital owns its skilled nursing facility.
Columns (3) and (4) compare skilled nursing facility discharges from non-integrated and integrated hospitals. As in home health discharges, for-profit hospitals are less likely to be vertically integrated into skilled nursing facilities. However, the difference between the proportion of non-integrated for-profit (13%) and integrated for-profit hospitals (8%) is smaller than in the home health discharge sample. Also, as with home health discharges, vertically integrated hospitals operate in areas where population density and HMO penetration is lower, but SNF concentration is higher.
To measure how quickly a hospital discharges their patients, we use a measure of length of stay in the hospital (LOS) that is computed relative to the average length of stay of similar patients in other hospitals by de-meaning from the national average length of stay within each Diagnosis Related Group. Our second dependent variable captures the impact of integration on the (downstream) intensity of home health care provision. The intensity of home health care is measured as the number of visits to a patient’s home divided by the number of days the patient remains in the care of a home health agency, where visits are weighted by the average wages by occupation of the home health provider as determined from the 2004 Current Population Survey. While most visits are by registered nurses (RN), many visits are by home health aides who are paid considerably less than RNs, while some visits are by specialized therapists who earn more. Our third dependent variable is one of the crucial observable measures of the quality of care patients’ receive along the care continuum: patient rehospitalization rate.
5. Empirical design
We test the three hypotheses, developed above, by focusing on how length of stay, home health intensity, and rehospitalization rates (within 60 days of a discharge) vary between patients from non-integrated and hospitals that are vertically integrated into home health care and skilled nursing facilities. Since general tasks—monitoring and recovery activities—are costly to perform in our empirical setting, the conceptual framework suggests that vertically integrated hospitals will use fiat to force its downstream facilities to accept patients (i) faster and (ii) in poorer health compared to in an arm’s length exchange, but that vertically integrated hospitals will manage the cost savings opportunities such that (iii) rehospitalization rates are no greater than in non-integrated settings.
While we are concerned with the endogeneity of vertical integration, we first test these predictions using the simple OLS model (1):
Yl = a + β1VIh + Xcβc + ei,
where l indexes patients, h indexes hospitals, and Y measures three outcomes: length of stay in the hospital (LOS), intensity of care in home health, and rehospitalization rates. VI is an indicator variable that is equal to unity when the hospital is vertically integrated into home health and zero otherwise. We also allow VI to enter as an interaction with each patient’s discharge location, that is, whether a patient is discharged to a hospital’s own post-acute care facility as opposed to a non-owned post-acute care facility. X is a vector of patient, hospital, home health agency and market controls that might plausibly shift hospital practice patterns. Patient level controls include variables that capture the health of the patient at admission, measured by 28 comorbidities as well as patients’ demographic characteristics, such as age, gender and race. We also include a control for the Euclidian distance between the exact address of the hospital the patient is discharged from and the centroid of the patient’s home zip code, as physicians might be expected to keep patients in the hospital longer when they are further from home. Hospital controls include a set of dummies for co-location with the focal type of post-acute care provider (home health center, or skilled nursing facility), ownership (for-profit, not-for-profit, and government), teaching status, and the number of licensed beds. Market controls include hospital, skilled nursing facility, and home health center concentration (Herfindahl) indices, demographic variables such as the average years of schooling of the local population, median income, the percentage of the population over age 65, the percentage of the population of childbearing age (females aged 15–44), population density, and a categorical variable for metropolitan areas; supply shifters including the total number of hospital beds, skilled nursing facility beds, and the number of long-term care beds in the market; and the strength of insurance companies, measured by HMO enrollment rate. Standard errors are clustered at the hospital market level, as defined by the Dartmouth Health Atlas (1999).
When VI enters as an interaction with each patient’s discharge location we also include a full set of interactions that capture other types of transfers as control variables. The simplest way to implement this approach is to control for transfers from vertically integrated hospitals to any non-owned post-acute care facility. A more detailed set of controls captures transfers from vertically integrated hospitals to both non-owned vertically integrated post-acute care providers and non-integrated post-acute care providers, and transfers from non-integrated hospitals to vertically integrated post-acute care providers. Allowing VI to enter as vector offers a robustness check on our tests of the first and third hypotheses, but is particularly important for tests of our second hypothesis since vertically integrated hospitals have strong incentives to steer patients who are expensive to serve to outside home health agencies.
Our basic tests are OLS cross-sectional regressions of vertical integration on hospital and home health practice patterns. Although we include a number of detailed controls, the cross-sectional nature of the analysis precludes us from making strong causal inferences from the OLS results, particularly in tests of the first hypothesis that vertical integration leads to shorter length of stay. Since both vertical integration and length of stay are choice variable for hospitals, our results are vulnerable to selection biases that might lead to heterogeneous treatment effects and omitted variable bias. While it is possible that our OLS estimates could be biased downward due to selection into vertical integration based on organizational quality, it seems more plausible that the OLS estimates of vertical integration on length of stay will be biased toward zero as vertically integrated hospitals tend to be institutions with care management philosophies that emphasize care delivery over management of financial objectives. For example, non-profit hospitals are sometimes thought to “over-deliver” services. While profit status is observable, the hospital’s care management philosophy is not, and we must, therefore, be concerned that our OLS estimates will confound the causal effect of vertical integration with selection effects.
We deal with the endogeneity of vertical integration using two approaches. First, we adjust for selection on observable differences between patient populations, by matching post-acute care patients from integrated hospitals to patients from non-integrated hospitals, based on all observable characteristics of patients, hospitals and markets. To do so, we use the Coarsened Exact Matching (CEM) procedure described by Iacus, King and Porro (2011), which facilitates multi-dimensional exact matching. CEM is similar to standard two-stage matching techniques in that it controls for selection bias by eliminating non-analogous observations in the treatment (i.e. integrated) and control (i.e., non-integrated) populations.9 CEM has some advantages over standard matching approaches: it requires fewer post-estimation assumptions; has superior computational properties for large data sets, and is well suited for applications where most regressors are discrete. While CEM is a powerful tool for eliminating observable differences between hospitals, markets and the patient population, no matching method can control for sources of heterogeneity that arise from unobservable characteristics of hospitals.
To adjust for selection on unobservables, we exploit variation in local market conditions in the industry, using the rate of vertical integration into home health or skilled nursing facilities by other hospitals in the same market (weighted by patient volume) as an instrument for the focal hospital’s decision to vertically integrate into home health (VI_HOSP-h). Thus, our key identifying assumption is that there are no unobserved market-level factors that are correlated with both local hospitals’ vertical integration decisions and the timing of patient discharge. In general, we believe that the key insurance characteristics of a local market are adequately captured by HMO penetration and the percentage of the local population over age 65 (i.e., eligible for Medicare), because these measures are good proxies for the pressure that payers may exert on hospitals to reduce costs. Furthermore, other hospitals’ integration decisions should not have any direct effect on a focal hospital’s practice patterns, particularly given the extensive patient, hospital and market controls in specification (1); yet, discussions with industry experts suggest that hospital integration decisions are often determined by idiosyncratic local market conditions. In particular, we expect that our instrument will pick up the effects of the historical spatial distribution of the local population and local market vertical foreclosure effects, which influence a focal hospital’s integration decisions without directly influencing length of stay.
Spatial effects stem from the fact that patients typically want to have post-acute care delivered close to their home or one of their children’s homes. If the local elderly population and their family members tended to live close to, or within an easy commute of, the main urban hospitals in a given area historically, then post-acute care providers also will have tended to locate near the hospitals (whether they are integrated or not). On the one hand, one should expect to see more vertical integration in a market when the at risk population lives near the hospital since the cost of administering a post-acute care center is generally thought to be lower when it is co-located with the hospitals main administrative offices. On the other hand, if a mass of post-acute care providers cluster near urban hospitals it will give hospitals more bargaining power vis-à-vis the post-acute care providers, which will lead to less vertical integration. Thus, the direction of spatial effects on integration depends crucially on the order of entry (which we do not observe in the data). If independent care providers entered before hospitals vertically integrated we would be more likely to see a decentralized equilibrium, but, if hospitals tended to enter the post-acute care market initially via vertical integration we would be more likely to see an equilibrium where most hospitals were vertically integrated. Regardless of the historical order of entry, our instrument should generate a strong first stage since markets will tend to tip one way or the other. However, given that we control directly for the distance between each patient’s home and the hospital they are discharged from in 2005, spatial effects captured by our instrument should only reflect the historical development of the market and should not have any direct effect on a focal hospital’s length of stay concurrently.
Similar logic applies to vertical foreclosure effects. If another hospital vertically integrates in a focal hospital’s market it reduces the focal hospital’s bargaining power because it forecloses a downstream trading partner to the focal hospital. Thus, vertical integration is an idiosyncratic path dependent process that is highly contingent on other hospital’s characteristics. For example, if a competing hospital in a market has low integration costs or a social mission that emphasizes post-acute care provision they will tend to integrate, which will raise the chances that the focal hospital will integrate. Thus, other hospital’s integration decisions influence the focal hospital’s integration decision, but other hospital’s integration costs should not influence the focal hospital’s discharging practices, once we control for bargaining power using hospital, skilled nursing facility, and home health concentration ratios by market, so the instrument should be powerful in the first stage, but should also satisfy the exclusion restriction.
A practical drawback of our instrumental variable is that it only generates market-level variation. We could not identify any hospital-level shifters of the costs or benefits of diversification that would satisfy the exclusion restriction. However, we find that our instrument generates substantial between-hospital variation in practice, since the 2,571 hospitals in our sample operate in hundreds of different local markets. For the purposes of measuring the instrument, we define the competitive hospital markets based on the 306 Hospital Referral Regions (HRRs) as defined by the Dartmouth Health Atlas (1999).10 Because the HRR boundaries are defined based on patient referral patterns, they closely represent the competitive market for hospitals when making decisions regarding vertical integration. Given the large number of localized health care markets we expect our instrument to be strong in the first stage. However, if there are unobservable market-level health characteristics or variations in hospitals’ bargaining power that are correlated with both vertical integration and length of stay, and our controls do not adequately capture these factors directly or indirectly, our instrument will fail the exclusion restriction and our two-stage estimates will be invalid.
Because our main concern is with the endogeneity of hospital decisions, our key tests of Hypotheses 1 and 3 apply the instrument VI_HOSP-h to correct for selection on unobservables at the hospital-level. Specifically, we use the two-stage residual inclusion (2SRI) method first proposed by Hausman (1978) and more recently by Terza, Basu and Rathouz (2008). The first stage of our 2SRI procedure is a logit model predicting hospital vertical integration into home health or skilled nursing facilities (VI_HOSP),including all of the controls in (1) aggregated to the hospital level, where the integration rate of other hospitals in the same market is the source of exogenous variation in each hospital’s vertical integration decision. The second stage of the 2SRI procedure includes the residual from the first stage, which by definition is uncorrelated with the covariates in X in (1), and controls for selection into vertical integration based on unobservables. 2SRI estimators have econometric properties that are similar to other two-stage estimators, like two-stage least squares (2SLS), but are particularly well suited for our application. Importantly, they are consistent when endogenous regressors are non-linear and have correct asymptotic standard errors in the first stage, which facilitates a two-stage instrumental variables approach at two different levels of analysis (i.e., hospital and patient) without manually adjusting the standard errors. As a robustness check, we perform a similar analysis, using the more familiar 2SLS estimator, which predicts vertical integration with a first stage linear probability model, replacing the explanatory variable (VI_HOSP) in the second stage with the predicted probability of vertical integration into home health. The results are robust to matching using CEM prior to 2SRI estimation as well.
Tests of our second hypothesis—that vertically integrated hospitals will discharge patients to their own home health agencies when the patients require more intensive care—compares home health intensity in vertically integrated health systems with intensity in non-integrated home health agencies, using OLS on the full and matched samples. Ideally, we would want to isolate the causal effect of vertical integration on home health intensity; however, a valid instrument that would generate exogenous variation in the choice of discharge outlet is difficult to identify. Given that endogeneity should bias our results on intensity toward zero due to selection effects—the effect of moral hazard would suggest that hospitals want to keep the healthiest patients for themselves while sending the sickest patients to other agencies—we can test Hypothesis 2 by recovering the cost of the decision to vertically integrate, conditional on the hospital’s choice to vertically integrate. Nevertheless, we want to ensure that the treatment and control groups are comparable along all observable dimensions, so that our results are not being driven by unusual observations or model specification issues. To do so, our baseline specification includes a full set of interactions between a hospital’s vertical integration status and each patient’s discharge location. We also use CEM, as above, to match control observations to treatment observations. The impact of hospital vertical integration on the intensity of home health care is then estimated on the matched sample, using OLS model (1).
6. Results
Table 2-A shows the relationship between hospitals vertically integrated into home health and average length of stay at the patient-level. Column 1 reports a −0.12 raw correlation between vertically integration and length of stay, which means that vertical integration is associated with shaving one day off a hospital stay for one out of every eight patients. Including patient controls reduces the correlation to −0.11, while including the full set of patient, hospital and market controls reduces the point estimate to −0.07, and the coefficient estimate becomes indistinguishable from zero (column 2). However, the results in Column 3 demonstrate that patient-level selection effects bias the OLS results toward zero as the coefficient estimate on VI_HOSP in the matched sample increases to −0.09. Columns 4-I and 4-II reveal the strength of our instrument and the influence of omitted variable bias on the OLS estimates. Column 4-I is the first stage instrumental variables regression predicting vertical integration at the hospital level. The instrument VI_HOSP-h—other hospitals’ rate of vertical integration in the same market (weighted by patient volume)—is very strong: the F-statistic on VI_HOSP-h in the first stage is 63, reflecting the fact that local market characteristics have a strong impact on any individual hospital’s decision to vertically integrate, and a 1% increase in the market vertical integration rate leads to a 0.30% increase in a focal hospital’s propensity to vertically integrate. The second stage of our instrumental variables approach includes the residual from the first stage to adjust for the effects of unobservable hospital-specific factors that might influence vertical integration decisions. The, result is a point estimate on the coefficient on vertical integration that is twice as large as the OLS estimate at −0.20—approximately a one day reduction in length of stay for every five patients discharged—but continues to be imprecisely estimated. Columns 5 and 6 report the results controlling for patients’ discharge location. Length of stay is reduced by one day for every ten patients transferred within a vertically integrated health system (i.e., the coefficient on “within firm transfers” is −0.10), and is statistically significant compared to patients transferred to home health agencies from non-integrated hospitals (the excluded group), while the difference in length of stay for patients transferred from vertically integrated hospitals to non-owned home health agencies is indistinguishable from the excluded group (column 5). Breaking down length of stay for transfers that are not completed within a vertically integrated health system in column 6 yields a similar result for the coefficient of interest.
Table 2.
| A Vertical integration and length of stay: home health (HHA) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dep. var: ΔLOS | (1) | (2) | (3) | (4-I) | (4-II) | (5) | (6) | |||||||
| OLS | OLS Controls |
Matched (CEM) |
1st stage IV (logit) |
2nd stage 2SRI |
OLS Interaction 1 |
OLS Interaction 2 |
||||||||
| Hosp. vertically int. into home health | −0.12 (0.05) | ** | −0.07 (0.05) | −0.09 (0.05) | ** | −0.20 (0.15) | ||||||||
| Other hosp. vert. int. into home health | 0.30 (0.04) | *** | ||||||||||||
| Residual from 1st stage | 0.06 (0.06) | |||||||||||||
| Within firm transfer (VI_HOSP_TX) | −0.10 (0.04) | ** | −0.09 (0.04) | ** | ||||||||||
| VI_HOSP to other HHA (VI_HOSP_EXT) | −0.04 (0.05) | |||||||||||||
| VI_HOSP to non-VI_HHA (VI_EXT_NON) | −0.04 (0.05) | |||||||||||||
| VI_HOSP to other VI_HHA (VI_EXT_VI) | −0.02 (0.07) | |||||||||||||
| Non-VI_HOSP to VI_HHA (VI_HHA_IN) | 0.09 (0.06) | |||||||||||||
| Patient controls | N | Y | Y | Y | Y | Y | Y | |||||||
| Hospital controls | N | Y | Y | Y | Y | Y | Y | |||||||
| Market controls | N | Y | Y | Y | Y | Y | Y | |||||||
| Constant | Y | Y | Y | Y | Y | Y | Y | |||||||
| R2/Adj.-R2/Pseudo-R2 | 0.00 | 0.04 | 0.04 | 0.16 | 0.04 | 0.05 | 0.05 | |||||||
| F-test on IV | 60 | |||||||||||||
| N | 399,616 | 399,616 | 344,384 | 2,571 | 399,616 | 399,616 | 399,616 | |||||||
| B Vertical integration and length of stay: skilled nursing facility (SNF) | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dep. var: ΔLOS | (1) | (2) | (3) | (4-I) | (4-II) | (5) | (6) | |||||||
| OLS | OLS Controls |
Matched (CEM) |
1st stage IV (logit) |
2nd stage 2SRI |
OLS Interaction 1 |
OLS Interaction 2 |
||||||||
| Hosp. vertically int. into SNF | −0.27 (0.08) | *** | −0.22 (0.06) | *** | −0.20 (0.07) | *** | −0.64 (0.02) | ** | ||||||
| Other hosp. vert. int. into home health | 0.34 (0.04) | *** | ||||||||||||
| Residual from 1st stage | 0.20 (0.13) | |||||||||||||
| Within firm transfer (VI_HOSP_TX) | −0.37 (0.08) | *** | −0.38 (0.08) | *** | ||||||||||
| VI_HOSP to other SNF (VI_HOSP_EXT) | −0.04 (0.08) | |||||||||||||
| VI_HOSP to non-VI_SNF (VI_EXT_NON) | −0.03 (0.08) | |||||||||||||
| VI_HOSP to oth. VI_SNF (VI_EXT_VI) | −0.52 (0.20) | *** | ||||||||||||
| Non-VI_HOSP to VI_SNF (VI_SNF_IN) | −0.07 (0.11) | |||||||||||||
| Patient controls | N | Y | Y | Y | Y | Y | Y | |||||||
| Hospital controls | N | Y | Y | Y | Y | Y | Y | |||||||
| Market controls | N | Y | Y | Y | Y | Y | Y | |||||||
| Constant | Y | Y | Y | Y | Y | Y | Y | |||||||
| R2/Adj.-R2/Pseudo-R2 | 0.00 | 0.06 | 0.06 | 0.08 | 0.06 | 0.06 | 0.06 | |||||||
| F-test on IV | 72 | |||||||||||||
| N | 460,761 | 460,761 | 397,038 | 2,571 | 460,761 | 460,761 | 460,761 | |||||||
Standard errors are robust and clustered at the market level.
Significant at 1%,
Significant at 5%,
Significant at 10%
Patient controls include: age, gender, race, 28 controls for patient health characteristics upon admission to the hospital (Elixhauser comorbidities). Hospital controls include: co-location dummy (with home health), ownership form dummies {for-profit, government, not-for-profit}, number of beds, and a dummy for teaching hospital. Market controls include: hospital, home health, and SNF concentration; avg. educational attainment, median household income, % of population over 65 year old, a dummy for metropolitan area, population density, number of hospital beds, number of long-term care hospital beds, number of skilled nursing facilities beds, the percentage of women of child bearing age (% of population that is female aged 15–44), and the HMO enrollment rate.
Standard errors are robust and clustered at the market level.
Significant at 1%,
Significant at 5%,
Significant at 10%
Patient controls include: age, gender, race, 28 controls for patient health characteristics upon admission to the hospital (Elixhauser comorbidities). Hospital controls include: co-location dummy (with SNF), ownership form dummies {for-profit, government, not-for-profit}, number of beds, and a dummy for teaching hospital. Market controls include: hospital, home health, and SNF concentration; avg. educational attainment, median household income, % of population over 65 year old, a dummy for metropolitan area, population density, number of hospital beds, number of long-term care hospital beds, number of skilled nursing facilities beds, the percentage of women of child bearing age (% of population that is female aged 15–44), and the HMO enrollment rate.
The interpretation of Table 2-A is that there is some evidence that hospital vertical integration allows hospitals to discharge patients to home health sooner relative to non-integrated hospitals, but the effect is small—representing savings of only about 3% of bed-days.11 Because the point estimates on within firm transfers are small, and between-firm transfers from vertically integrated hospitals to other home health agencies are imprecisely estimated, Table 2-A does not provide strong evidence that within-firm transfers occur faster than between-firm transfers from vertically integrated hospitals.
Table 2-B shows that the results on length of stay effects for hospital vertically integrated into skilled nursing facilities are larger and more precise compared to vertical integration into home health. Without controls, the correlation between vertical integration and length of stay is −0.27, (column 1), and is precisely estimated. The point estimate is slightly larger at −0.28 when including patient controls, but falls to −0.22 when including the full set of patient, hospital and market controls (column 2). Column 3 shows the matched sample estimate. Matching exactly based on all observable characteristics of patients, hospitals, and markets yields a precisely estimated point estimate of −0.20. Finally, columns 4-I and 4-II show the two stages of our instrumental variables analysis. Column 4-I displays marginal effect of other hospitals’ integration rate on the focal hospital’s probability of vertically integrating, while column 4-II shows the second-stage estimates of integration on length of stay. The interpretation of the coefficient on the instrument is that increasing the extent of vertical integration in a local market by 1% increases the probability that a focal hospital will be vertically integrated by 0.34%. As with home health, the second stage estimate on vertical integration is substantially larger than the OLS estimate. The interpretation of the point estimate of −0.64 on vertical integration is that when hospitals are vertically integrated into skilled nursing facilities they are able to reduce patient length of stay in the hospital by one day for six out of every ten patients who eventually receive post-acute care at a skilled nursing facility, a reduction in total bed-days of about 9%.12
We also estimate the impact of vertical integration on length of stay controlling for patients’ discharge location in columns 5 and 6. The point estimate on transfers within a vertically integrated health system (“within firm transfer”) is −0.36, and statistically significant, in both cases—when controlling for transfers from vertically integrated hospitals to outside skilled nursing facilities, and when controlling for the larger set of interactions as described in Table 2-A, respectively. The coefficient estimates on within firm-transfers are not only statistically different from the omitted group, transfers from non-integrated hospitals, and transfers from non-integrated hospitals to non-integrated skilled nursing facilities respectively, they are also statistically different from other types of transfers. The only exception is that speed at which patients are transferred between vertically integrated hospitals and vertically integrated skilled nursing facilities that are owned by different parent firms are not statistically different, though this type of transfer is quite unusual, accounting for only 1% of all transfers. The interpretation is that the key action in our data comes from exactly the types of transfers we expect: within firm transfers along the care continuum are effectuated much faster than transfers between firms. Putting the economic effects in perspective, if the average hospital could shift one hospital bed-day to a skilled nursing facility for six out of every ten patients that go to skilled nursing facilities they could profitably incur up to approximately $100,000 per year of additional administrative costs associated with vertical integration.13 Of course, establishing break-even points for the average hospital with averages can be misleading because capacity constraints and bureaucratic costs vary across institutions.
Table 3 summarizes the tests of the relationship between integration and the intensity of home health care provided to patients who are admitted to home health.14 Discharges from vertically integrated hospitals to their own home health agencies (“within firm transition”) receive an additional 0.010 visits/day, relative to the baseline rate for patients discharged from non-integrated hospitals, while patients discharged from integrated hospitals to external non-affiliated home health agencies had 0.003 fewer visits per day compared to the baseline (column 1). The F-test on the difference between within firm transitions and external transitions from vertically integrated hospitals is significant at the 1% level, which suggests that within firm transitions are more demanding on the downstream organization relative to market transitions. Controlling for whether external discharges go to other integrated agencies or to non-integrated agencies and for discharges from non-integrated hospitals to vertically integrated agencies with a more refined set of interactions has little effect on the main result. After matching and including the full set of interactions, the point estimate on within firm transitions is 0.012 or 1.2 additional home health visits per 100 day episode. With an average length of a home health episode around 33 days, this suggests that approximately one of every three patients experiencing a within firm transition gets an extra home health visit. Increasing one home health visit for one-third of the 400,000 home health admissions per year that come directly from hospitals would have increased total costs by about $13 million, assuming the average home health visit costs approximately $100. Under prospective payment, these costs are borne by the agencies rather than by Medicare.
Table 3.
Vertical integration and intensity of home health care
| Dependent variable: home health intensity (visits/day) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Full sample | Matched sample | |||||||
| (1) | (2) | (3) | (4) | |||||
| Within firm transfer (VI_HOSP_TX) | 0.010 (0.004) | ** | 0.010 (0.004) | ** | 0.012 (0.004) | *** | 0.012 (0.004) | *** |
| VI_HOSP to other HHA (VI_HOSP_EXT) | −0.003 (0.004) | −0.001 (0.004) | ||||||
| VI_HOSP to other VI HHA (VI_EXT_VI) | −0.004 (0.005) | −0.002 (0.006) | ||||||
| VI_HOSP to non-VI_HHA (VI_EXT_NON) | −0.002 (0.004) | −0.001 (0.004) | ||||||
| Non-VI_HOSP to VI_HHA (VI_HHA_IN) | 0.004 (0.005) | 0.002 (0.005) | ||||||
| Patient controls | Y | Y | Y | Y | ||||
| Hospital controls | Y | Y | Y | Y | ||||
| Market controls | Y | Y | Y | Y | ||||
| Constant | Y | Y | Y | Y | ||||
| R2 | 0.04 | 0.04 | 0.04 | 0.04 | ||||
| N | 399,368 | 399,368 | 342,886 | 342,886 | ||||
Standard errors are robust and clustered at the market level.
Significant at 1%,
Significant at 5%,
Significant at 10%.
HHA stands for Home Health Agency. Controls are as in Table 2-A.
The higher speed with which integrated hospitals discharge patients and the greater severity of patients’ health at admission to their home health agency raises an important policy question. Are vertically integrated hospitals delivering lower quality care by discharging their patients sicker and quicker or do hospitals use integration to increase their efficiency while holding quality of care constant? To answer this question, we test in Table 4 whether health outcomes differ between integrated and non-integrated hospitals for patients discharged to post-acute care by regressing integration on incidence of rehospitalization. We find that in home health the correlation between integration and rehospitalization is indistinguishable from zero in full-sample OLS regressions (column 1), 2SRI tests (column 2), and after including controls for patients’ discharge location (columns 3 and 4), suggesting that under integration into home health, patient recovery tasks are shifted downstream without meaningfully affecting quality of care. Column (5) shows that rehospitalization rates for patients discharged to skilled nursing facilities within a vertically integrated system are 0.5% lower compared to patients discharged to skilled nursing facilities from non-integrated hospitals. Similar results are obtained when controlling for patients’ discharge location and comparing within-firm transfers against transfers from non-integrated hospitals (column 7) or against transfers from non-integrated hospitals to non-integrated skill nursing facilities (column 8). While the coefficient is precisely estimated, the effect is small economically compared to a baseline rehospitalizaiton rate of approximately 20%. However, after adjusting for the endogeneity of vertical integration using the 2SRI method the point estimate on vertical integration increases to −2.0% (column 6). The interpretation is that integration actually leads to improved health outcomes. The results suggest that while integration enables quicker and sicker discharges, the savings obtained are not the result of lowering the quality of care received by patients. Moreover, the result suggests that vertical integration does not mechanically lead to faster discharges through improved coordination in the channel, but rather supports discharges of patients who can be supported outside of the hospital environment.
Table 4.
Vertical integration and rehospitalization
| Dependent variable: rehospitalization rate within 60 days of discharge | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Home health | Skilled nursing facility | |||||||||||
| (1) OLS |
(2) 2SRI |
(3) OLS |
(4) OLS |
(5) OLS |
(6) 2SRI |
(7) OLS |
(8) OLS |
|||||
| Hosp. vertically integrated | −0.002 (0.002) | 0.002 (0.006) | −0.005 (0.002) | ** | −0.020 (0.008) | ** | ||||||
| Residual from 1st stage | −0.002 (0.002) | 0.007 (0.004) | * | |||||||||
| Within firm transfer | −0.001 (0.002) | −0.001 (0.002) | −0.006 (0.003) | ** | −0.007 (0.003) | ** | ||||||
| VI_HOSP to other post-acute provider | −0.004 (0.003) | −0.004 (0.003) | ||||||||||
| VI_HOSP to other VI post-acute provider | 0.001 (0.005) | −0.029 (0.010) | *** | |||||||||
| VI_HOSP to non-VI post-acute provider | −0.005 (0.003) | −0.003 (0.003) | ||||||||||
| Non-VI_HOSP to VI post-acute provider | 0.001 (0.002) | −0.023 (0.005) | *** | |||||||||
| Patient controls | Y | Y | Y | Y | Y | Y | Y | Y | ||||
| Hospital controls | Y | Y | Y | Y | Y | Y | Y | Y | ||||
| Market controls | Y | Y | Y | Y | Y | Y | Y | Y | ||||
| Constant | Y | Y | Y | Y | Y | Y | Y | Y | ||||
| R2 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | 0.02 | ||||
| N | 399,616 | 399,616 | 399,616 | 399,616 | 460,761 | 460,761 | 460,761 | 460,761 | ||||
Standard errors are robust and clustered at the market level.
Significant at 1%,
Significant at 5%,
Significant at 10%
Controls are as in Tables 2-A and 2-B for home health and skilled nursing facility regressions, respectively.
The results suggest that vertical integration creates economically meaningful opportunities for hospitals to discharge patients earlier and in worse health to post-acute care following hospitalization. We interpret the results as evidence that integration allows firms to solve coordination problems by allocating tasks to assets more efficiently. Our findings do not dispute the idea that vertical integration increases administrative costs. Nor do we dispute the importance of cascading organizational effects associated with timing problems, as described in the extant literature. Nevertheless, the results point to one of the heretofore underappreciated advantages of vertical integration—control over the allocation of tasks to sites or assets.
7. Conclusion
This paper examines how integration addresses coordination issues in market exchange by solving task allocation problems. In our framework, we demonstrate how the allocation of general tasks to assets (or sites) influences the efficiency of an economic system by determining the timing of exchange. The findings offer a step toward integrating the powerful idea that tradeoffs between discrete structural alternatives define the boundary of the firm in equilibrium, as in transaction cost economics (Williamson 1985), with the intuitively appealing idea that tasks or routines, can also shape firm boundaries by influencing the efficiency of production (Nelson and Winter 1985).
Controlling for the endogeneity of vertical integration, patient characteristics, as well as a host of hospital and market factors, we find hospitals that are vertically integrated tend to discharge patients to their own home health agencies and skilled nursing facilities sooner and in poorer health compared with non-integrated hospitals; yet, health outcomes are actually better for patients who transition to hospitals’ own skilled nursing facilities and no worse for patients who transition to hospital’s own home health agencies. The variation in practice patterns and health outcomes reflects the integrated entity’s ability to use fiat to shift patients in need of recovery and monitoring services (general tasks) from the hospital setting to post-acute care settings. Thus, the evidence suggests that vertical integration reduces coordination problems that arise due to the misallocation of tasks under market exchange.
Our results highlight the unintended consequences of restrictions on gain-sharing across entities. These prohibitions on side-payments and kickbacks, instituted to prevent referrals based on financial interests, contribute to the misallocation of tasks and may create a strong impetus for integration. In this regard, our paper contributes to the ongoing health care reform debate, which focuses on the role of both clinical and financial integration of health care entities in reducing costs and improving the quality of care. More generally, our approach calls for further research on the role of the interplay between tasks and assets in defining the boundaries of firms in other settings.
Footnotes
We are grateful to Iwan Barankay, Avi Dor, Silke Forbes, Vit Henisz, Mireille Jacobson, Raffaella Sadun, Aly Shogan, Brian Silverman, Tim Simcoe, Pai-Ling Yin as well as participants at the 2010 Foundations of Business Strategy Conference at Washington University, the Third Biennial Conference of the American Society of Health Economists at Cornell University, the 2010 NYU Economics of Strategy Conference, the 2010 Institutions and Innovation Conference at Harvard Business School, the 2011 DRUID conference, the 2011 SRF workshop in Annapolis, the Bowman Seminar at Wharton, the 2011 Academy of Management conference, and the International Health Economics Association 8th World Congress in Toronto for helpful comments and suggestions. Mike Punzalan and Jianing Yang provided excellent research assistance. This work is supported by NIH/NHLBI grant # R01 HL088586-01.
We use the terms assets and sites interchangeably throughout this paper. In health care, as in most service industries, tasks may be performed in multiple physical settings. These settings can be thought of as assets or sites.
Home health care is skilled health care services provided in the home, for a limited duration; most often by registered nurses, rehabilitative therapists, social workers, or home health aides.
Skilled nursing facilities (also called long-term care facilities or nursing homes) are establishments that house chronically ill patients, and provide post-acute and long-term nursing care.
The risk-adjusted payment is most sensitive to differences in the complexity of care a patient requires, primarily based on the surgical procedure they are recovering from, and is less sensitive to the timing of a transition.
The reimbursement for a nursing home stay is fixed per-diem, increasing linearly with length of stay.
Our key predictions are also broadly consistent with an informal health economics literature on vertical integration in hospitals (Robinson 1996, Lehrman and Shore 1998).
10% of beneficiaries in Medicare Advantage plans do not have MEDPAR records and are excluded.
Typically, discharges from an integrated hospital go to a non-integrated home health agency when a patient’s home is outside of the hospital’s home health service area.
We create a single measure of propensity to vertically integrate, using all secondary controls in (2), which we include along with our key controls: age, gender, comorbidities, DRG type, hospital bed quartiles, and a metropolitan market dummy.
We treat counties as markets for measuring market-level controls.
At an average length of stay of six days, five patients would need 30 bed-days in a non-integrated hospital. In a vertically integrated hospital, the same five patients would require only 29 bed-days. (30-29)/30=3%.
At an average length of stay of seven days, ten patients would need 70 bed-days in a non-integrated hospital. In a vertically integrated hospital, the same ten patients would require only 64 bed-days. (70-64)/70=9%
There are approximately 461,000 patients discharged to SNFs each year. If six out of every ten were moved one day earlier it would result in 276,600 bed-days saved (461,000×0.6). The average bed-day reimbursement is $1,121 in a hospital (Candrilli and Mauskopf, 2006), compared to $212 in a SNF (MetLife, 2009), thus the total savings would be $251.4M (276,600×$929) or $97,832 for each of the 2,570 hospitals in the U.S.
124 patients (out of 399,368 patients) are coded without valid home health claims information.
Contributor Information
Guy David, The Wharton School, University of Pennsylvania and NBER, 202 Colonial Penn Center, 3641 Locust Walk, Philadelphia, PA 19104-6218.
Evan Rawley, Email: rawley@wharton.upenn.edu, The Wharton School, University of Pennsylvania, 2000 Steinberg Hall-Dietrich Hall, 3620 Locust Walk, Philadelphia PA 19104-6370.
Daniel Polsky, Email: Polsky@mail.upenn.edu, University of Pennsylvania, Blockley Hall, Room 1204, 423 Guardian Drive, Philadelphia, PA 19104.
References
- Candrilli S, Mauskopf J. How much does a day in the Hospital Cost? Value in Health. 2006;9(3):A56. [Google Scholar]
- Chiplin Alfred J. Breathing Life into Discharge Planning. Elder Law Journal. 2005;13:1–84. [Google Scholar]
- Collier Eric J, Charlene Harrington. Discharge planning, nursing home placement, and the Internet. Nursing Outlook. 2005;53:95–103. doi: 10.1016/j.outlook.2004.02.002. [DOI] [PubMed] [Google Scholar]
- Corts K. The Interaction of Task and Asset Allocation. International Journal of Industrial Organization. 2006;24:887–906. [Google Scholar]
- The Dartmouth Atlas of Health Care. Appendix: Geography of Health Care in the United States. 1999:289–307. [Google Scholar]
- David G, Rawley E, Polsky D. Integration and Task Allocation: Evidence from Patient Care. NBER working paper #17419. 2011 doi: 10.1111/jems.12023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes SJ, Lederman M. Adaptation and Vertical Integration in the Airline Industry. American Economic Review. 2009;99:1831–1849. [Google Scholar]
- Forbes SJ, Lederman M. Does Vertical Integration Affect Firm Performance? Evidence from the Airline Industry. RAND Journal of Economics. 2009;41:765–790. [Google Scholar]
- Hausman JA. Specification Tests in Econometrics. Econometrica. 1978;46:1251–1271. [Google Scholar]
- Holmstrom B, Milgrom P. Multitask Principal-Agent Analyses: Incentive Contracts, Asset Ownership and Job Design. Journal of Law, Economics and Organization. 1991;7:24–52. [Google Scholar]
- Iacus SM, King G, Porro G. Causal Inference Without Balance Checking: Coarsened Exact Matching. Political Analysis. 2011 (forthcoming). [Google Scholar]
- Klein B, Crawford RA, Alchian AA. Vertical Integration, Appropriable Rents and the Competitive Contracting Process. Journal of Law and Economics. 1978;21:297–326. [Google Scholar]
- Lehrman S, Shore K. Hospitals’ Vertical Integration into Skilled Nursing: A Rational Approach to Controlling Transaction Costs. Inquiry-Blue Cross & Blue Shield Association. 1998;35:303–314. [PubMed] [Google Scholar]
- Masten SE, Meehan JW, Snyder EA. The Costs of Organization. Journal of Law, Economics and Organization. 1991;7:1–25. [Google Scholar]
- MetLife. Market Survey of Nursing Home, Assisted Living. [Accessed July 25, 2011];Adult Day Services, and Home Care Costs. 2009 http://www.metlife.com/assets/cao/mmi/publications/studies/mmi-market-survey-nursing-home-assisted-living.pdf. [Google Scholar]
- Moore C, McGinn T, Halm E. Tying up loose ends: Discharging patients with unresolved medical issues. Archives of Internal Medicine. 2007;167:1305–1311. doi: 10.1001/archinte.167.12.1305. [DOI] [PubMed] [Google Scholar]
- Naylor M, Brooten D, Jones R, Lavizzo-Mourey R, Mezey M, Pauly M. Comprehensive Discharge Planning for the Hospitalized Elderly: A Randomized Clinical Trial. Annals of Internal Medicine. 1994;120:999–1006. doi: 10.7326/0003-4819-120-12-199406150-00005. [DOI] [PubMed] [Google Scholar]
- Novak S, Stern S. How Does Outsourcing Affect Performance Dynamics? Evidence from the Automobile Industry. Management Science. 2008;54:1963–1979. [Google Scholar]
- Nelson R, Winter S. An Evolutionary Theory of Economic Change. Cambridge, MA: Harvard Press; 1985. [Google Scholar]
- Nickerson JA, Silverman BS. Why Firms Want to Organize Efficiently and What Keeps Them from Doing So: Inappropriate Governance, Performance, and Adaptation in a Deregulated Industry. Administrative Science Quarterly. 2003;48:433–465. [Google Scholar]
- Pirrong SC. Contracting Practices in Bulk Shipping Markets: A Transactions Cost Explanation. Journal of Law and Economics. 1993;36:937–976. [Google Scholar]
- Robinson JC. Administered Pricing and Vertical Integration in the Hospital Industry. Journal of Law and Economics. 1996;39:357–378. [Google Scholar]
- Schoar A. Effects of Corporate Diversification on Productivity. Journal of Finance. 2002;57:2379–2403. [Google Scholar]
- Terza JV, Basu A, Rathouz Paul J. Two-stage Residual Inclusion Estimation: Addressing Endogeneity in Health Econometric Modeling. Journal of Health Economics. 2008;27:531–543. doi: 10.1016/j.jhealeco.2007.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson Oliver E. The Economic Institutions of Capitalism. New York, NY: Free Press; 1985. [Google Scholar]
- Williamson Oliver E. Comparative Economic Organization: The Analysis of Discrete Structural Alternatives. Administrative Science Quarterly. 1991;36:269–296. [Google Scholar]
- Williamson Oliver E. Transaction Cost Economics: The Natural Progression. American Economic Review. 2010;100:673–690. [Google Scholar]