Abstract
We investigated early cellular responses induced by infection with Leishmania major in macrophages from resistant C57/BL6 mice. Infection increased production of reactive oxygen species by resident, but not inflammatory peritoneal macrophages. In addition, infection increased activation of stress-activated protein kinases/c-Jun N-terminal kinases (SAPK/JNK) in resident, but not in inflammatory peritoneal macrophages. Infection also increased expression of membrane and soluble FasL, but infected macrophages remained viable after 48 h. Infection increased secretion of cytokines/chemokines TNF-α, IL-6, TIMP-1, IL-1RA, G-CSF, TREM, KC, MIP-1α, MIP-1β, MCP-1, and MIP-2 in resident macrophages. Addition of antioxidants deferoxamine and N-acetylcysteine reduced ROS generation and JNK activation. Addition of antioxidants or JNK inhibitor SP600125 reduced secretion of KC. Furthermore, treatment with antioxidants or JNK inhibitor also reduced intracellular parasite replication. These results indicated that infection triggers a rapid cellular stress response in resident macrophages which induces proinflammatory signals, but is also involved in parasite survival and replication in host macrophages.
Introduction
Infection with Leishmania affects nearly 350 million people worldwide. Parasites infect host macrophages and survive as intracellular amastigotes within phagolysosomal vesicles. Both tissue resident and inflammatory macrophages can be infected [1], [2]. Macrophages produce reactive oxygen species (ROS) upon infection with Leishmania [3]. Although ROS are regarded as toxic for the parasite, there is increasing evidence that ROS also function as signaling intermediates required for parasite differentiation to amastigotes [4], [5]. In addition, infection with L. major induces cytokine and chemokine gene expression in macrophages [6], [7] and recruits an early inflammatory reaction [6]. Subsequent interactions with inflammatory neutrophils either increases or decreases L. major replication in macrophages depending on host genotype, and through mechanisms involving either TGF-β or Neutrophil Elastase [8]–[10].
Mammalian cells respond to environmental stress by either adapting or undergoing programmed cell death [11]. Cellular stress activates the intracellular stress-activated protein kinases/c-Jun N-terminal kinases (SAPK/JNK) [11], [12]. Signalling through JNK activates c-Jun/AP-1 and increases expression of the death ligand FasL [13]–[15]. Therefore, cellular responses to stress could result in Fas-mediated apoptosis. However, the JNK pathway is also involved in non-apoptotic responses such as macrophage differentiation [16] and proinflammatory cytokine and chemokine production [17], [18].
Here we investigated early cellular and immunological responses to L. major infection in macrophages from genetically resistant mice. Our results indicated that infection triggers a cellular stress response in resident macrophages, characterized by increased production of reactive oxygen species (ROS), activation of the JNK stress pathway, and chemokine production. Addition of antioxidants or JNK inhibitor blocked both chemokine production and parasite replication. These results indicated that activation of macrophages to mediate an inflammatory response is triggered by a stress stimulus provided by the parasite, and mediated by ROS and the JNK signaling pathway.
Results
Production of ROS Induced by L. major Infection
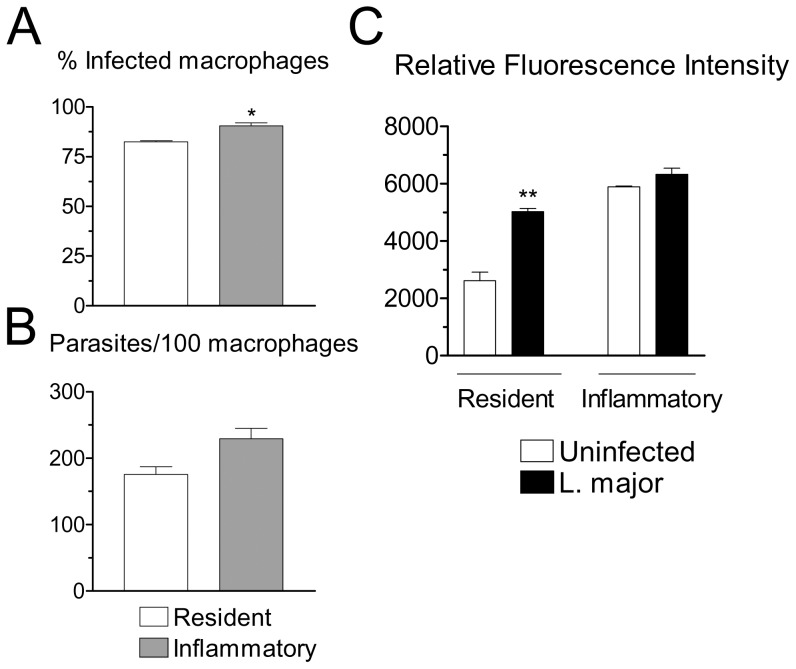
Peritoneal resident and inflammatory macrophages from C57BL/6 (B6) mice showed a comparable degree of infection 4 h after interaction with L. major promastigotes, in spite of a small, but statistically significant increase in percentage of infected inflammatory cells (Figures 1A and 1B). Infection with Leishmania parasites triggers production of ROS by macrophages [3], [19], [20]. We therefore investigated production of ROS 4 h after infection of macrophages with L. major promastigotes. In preliminary experiments, this time of infection gave the strongest signal of ROS production for the parasite isolate we employed in the present study. The timing of the peak ROS response depends on the parasite isolate employed. Infection increased the level of ROS produced by resident macrophages (Figure 1C). The levels of ROS produced by inflammatory macrophages were already elevated, and infection resulted in little or no additional increase in ROS production (Figure 1C). These results suggested that resident macrophages undergo a more pronouned oxidative response following infection with L. major, compared to inflammatory macrophages. In inflammatory macrophages, however, the levels of ROS were already elevated prior to infection.
Figure 1. Infection of macrophages with L. major and generation of ROS.
(A, B) Resident or inflammatory macrophages from B6 mice were infected with L. major for 4 h, and washed. Cells were stained and percentages of infected macrophages (A) and number of parasites per 100 macrophages (B) were determined. (C) Resident or inflammatory B6 macrophages were loaded with DCFH-DA, washed, treated with medium (Uninfected) or with L. major for 4 h, and fluorescence was measured. Results indicate arbitrary units of fluorescence and are mean and SE of triplicates. *P<0.05; **P<0.01.
Activation of SAPK/JNK Pathway by L. major Infection
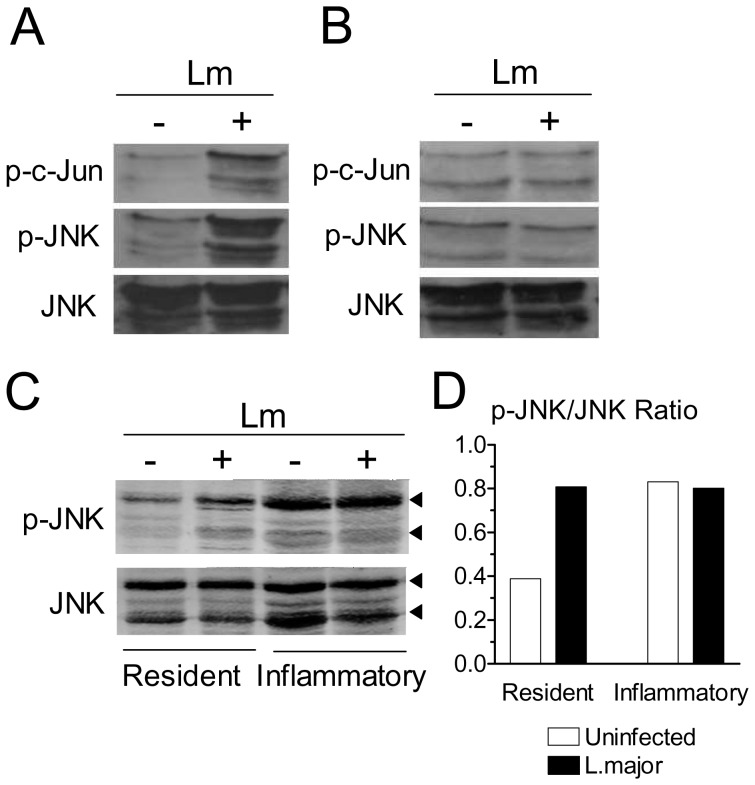
Oxidative stress is associated with activation of the SAPK/JNK pathway [21]–[23], where members of the c-Jun family are phosphorylated by JNK [13]–[15]. We investigated the activation of this pathway in macrophages. Western blotting analysis indicated that infection of resident macrophages with L. major markedly increased the levels of the phosphorylated forms of c-Jun and JNK over uninfected values (Figure 2A). By densitometric analysis, the increase was 4.1-fold for p-c-Jun, and 2.4-fold for p-JNK. On the other hand, infection induced only a small increase in the levels of p-c-Jun (1.3-fold) and failed to increase p-JNK (0.77-fold) in inflammatory macrophages (Figure 2B). The levels of total JNK protein did not change following infection (Figures 2A and 2B). Anti-p-c-Jun, p-JNK and JNK antibodies reacted with extracts of Leishmania promastigotes, but the bands had distinct molecular weight, compared to the mammalian proteins (data not shown). The results shown in Figures 2A and 2B were from independent experiments. We then compared the levels of p-JNK in resident and inflammatory macrophages infected in parallel. Again, infection increased the levels of p-JNK in resident macrophages (Figure 2C). The levels of p-JNK were already elevated in inflammatory macrophages, and did not change following infection (Figure 2C). A densitometric analysis of the blot shown in Figure 2C is presented in Figure 2D and confirms these observations. Infection with purified metacyclic forms also increased the levels of ROS and p-JNK in resident macrophages (not shown). The results indicated that, following infection with L. major, resident macrophages initiate a cellular stress response characterized by production of ROS and activation of the SAPK/JNK pathway. On the other hand, inflammatory macrophages were already activated, and infection did not change this ongoing activation state.
Figure 2. Infection with L. major activates the SAPK/JNK pathway.
Resident (A) or inflammatory (B) B6 adherent macrophages were infected or not with L. major (Lm). After 4 h, cell extracts were obtained and the levels of JNK, p-JNK and p-c-Jun were determined by western blotting. (C) Resident and inflammatory macrophages were adhered and infected in parallel. After 4 h, the levels of JNK and p-JNK were determined by western blotting. Top and bottom arrowheads indicate the p54 and p46 JNK bands, respectively. (D) Densitometric analysis of the blot shown in Figure 2C. The areas of both p46 and p54 bands were scanned. Results were normalized as the ratio between the intensities of the p-JNK and total JNK bands.
Upregulation of FasL Expression Following L. major Infection
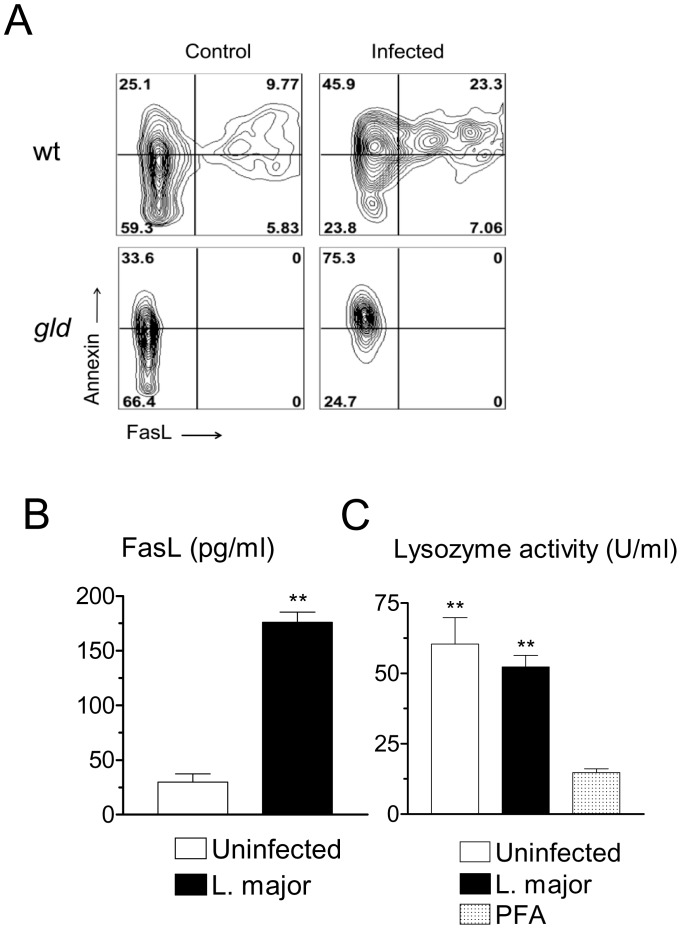
Cellular stress responses mediated by the SAPK/JNK pathway can be mediated through Fas and FasL molecules [13]–[15], [24]. We therefore, investigated expression of FasL. Infection increased expression of membrane FasL in resident macrophages (Figure 3A). In agreement with previous reports [25], [26], we found that a proportion of viable macrophages binds Annexin V (Figure 3A). Infection with L. major further increased Annexin V binding, including in FasL-deficient gld macrophages (Figure 3A). Infection with L. major also increased the amount of soluble FasL released by macrophages (Figure 3B). Infected macrophages expressed high levels of Fas receptor (not shown). However, we observed that infected macrophages remained viable and healthy, even after 48 h of culture. A quantitative viability assay based on the constitutive release of lysozyme by macrophages confirmed that, after 48 h, the viability of infected macrophages was comparable to that of uninfected macrophages (Figure 3C).
Figure 3. Infection with L. major increases FasL expression, but does not induce cell death.
(A) Resident B6 macrophages, either wild-type (wt) or FasL-deficient gld, were infected or not for 20 h. Monolayers were detached and stained for FCM. Gated populations comprise F4/80+ CD11b+7AAD− viable macrophages. Results indicate contour plots of Annexin V versus FasL staining. Numbers indicate percentages of cells in each quadrant. (B) Levels of soluble FasL in the supernatants of either control or infected resident macrophages 28 h after infection. (C) Resident macrophages were infected with L. major and cultured for 48 h. Supernatants were assayed for lyzozyme activity. As a control, macrophages were treated with paraformaldehyde (PFA) before collecting the supernatant. Results are mean and SE of triplicate cultures. **P<0.01.
Infection Induces a Defined Profile of Cytokine and Chemokine Production by Resident Macrophages
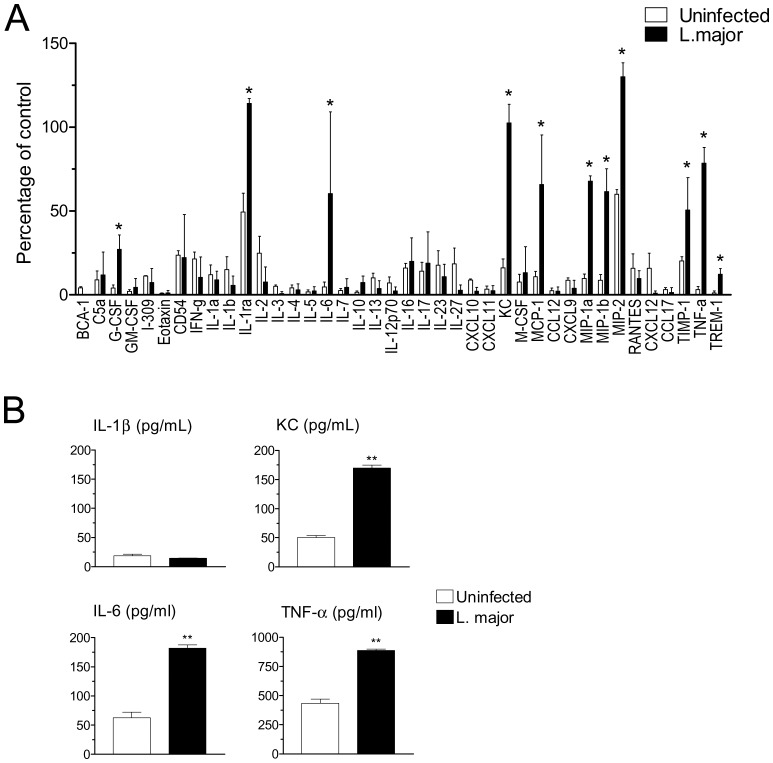
We used an antibody array to investigate global cytokine and chemokine production by resident macrophages at the protein level. Following infection with L. major, a defined response profile was identified, which could be reproduced in a repeat experiment. Infection increased secretion of cytokines/mediators IL-1RA, IL-6, TNF-α and TIMP-1 (Figure 4A). Infection also increased expression of G-CSF and TREM, although at relatively lower levels. Both IL-1α and IL-1β gave negative results. (Figure 4A). In addition, infection increased the release of chemokines KC, MCP-1, MIP-1α, MIP-1β and MIP-2 (Figure 4A). Individual ELISA assays for IL-1β, KC, IL-6 and TNF-α confirmed the results obtained with the antibody arrays (Figure 4B).
Figure 4. Induction of cytokine and chemokine release by L. major infection.
(A) Resident B6 macrophages were infected (closed bars) or not (open bars) for 20 h with L. major, and supernatants were probed with a mouse cytokine array. The intensity of the labeling for each cytokine/chemokine/mediator was quantitated and normalized as percentage of a positive control provided in the kit. Data indicate mean and SD of two independent arrays. Infected versus uninfected values were compared using non-parametric Mann-Whitney U-test. Cytokines showing a significant (P<0.05) increase following infection are indicated by an asterisk. (B) Supernatants were also probed by ELISA for IL-1β, KC, IL-6 and TNF-α, as indicated. **P<0.01.
Regulation of Chemokine Production and Parasite Replication by JNK and ROS
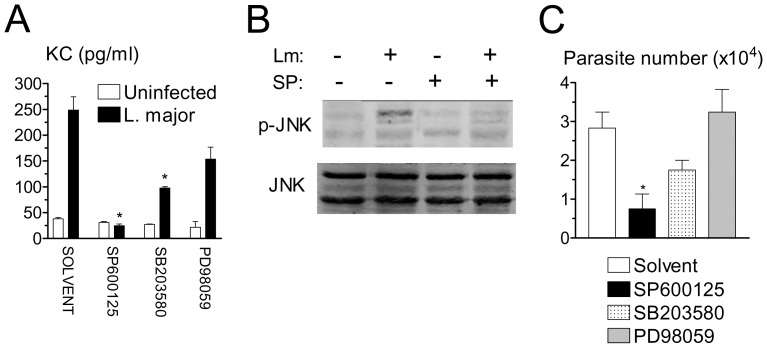
Based on the previous results, we employed secretion of KC as a marker of the inflammatory response of infected macrophages. JNK pathway is involved in inflammatory cytokine and chemokine production [17], [18]. To investigate the role of JNK activity in KC secretion, we employed selective MAPK inhibitors at optimal doses previously determined for peritoneal macrophages [27]. Secretion of KC was completely prevented by JNK inhibitor SP600125 at 10 µM, and partially prevented by ERK inhibitor SB203580 at 5 µM (Figure 5A). Addition of p38 inhibitor PD98059 induced a lesser reduction of KC secretion, and the effect was not statistically significant. We confirmed that treatment of infected macrophages with 10 µM SP600125 blocked JNK activation (Figure 5B). Interestingly, at the same dosages as above, JNK inhibitor SP600125 markedly reduced parasite replication in infected macrophages (Figure 5C), whereas addition of ERK inhibitor SB203580 and p38 inhibitor PD98059 did not result in significant effects (Figure 5C). Previous studies indicate that secretion of KC by infected BALB/c macrophages can be blocked by FasL neutralization [9]. However, secretion of KC induced by infection of B6 macrophages was not inhibited by a blocking mAb specific for FasL or by a neutralizating Fas/Fc chimera (data not shown). In adiition, neutrophil recruitment induced by L. major injection was similar in in wild type and FasL-deficient gld B6 mice (not shown). These results suggested that chemokine release and neutrophil recruitment were independent on FasL expression.
Figure 5. Effect of JNK inhibitor on release of KC, JNK activity and intramacrophagic parasite growth.
(A) Resident macrophages were infected or not with L. major in the presence of solvent or the indicated MAPK inhibitors. The levels of KC were determined by ELISA after 20 h of infection. (B) Macrophages were infected or not in the presence of solvent or JNK inhibitor SP600125. After 4 h, the levels of JNK and p-JNK were determined by western blotting. (C) Macrophages were infected overnight and cultured for additional 3 d in the presence of solvent or MAPK inhibitors. Intracellular load of parasites was evaluated. Results are mean and SE of the number of extracellular promastigotes produced. *P<0.05, compared to treatment with solvent.
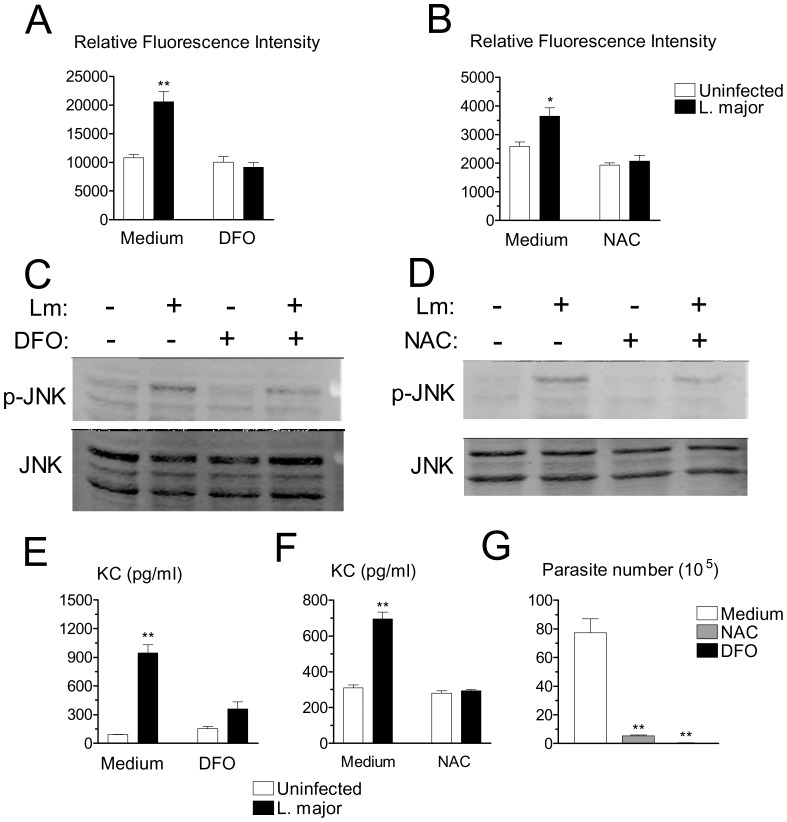
JNK activation can be mediated by ROS [21]–[23]. We therefore investigated the effects of antioxidants deferoxamine (DFO), an iron chelator that inhibits radical production, and N-acetylcysteine (NAC), a thiol compound that increases the levels of reduced glutathione. DFO, at 1 mM, and NAC, at 20 mM, markedly attenuated generation of ROS induced by L. major infection (Figure 6A and 6B). In addition, DFO and NAC at the same dosages, reduced JNK activation (Figure 6C and 6D) and production of KC induced by L. major in macrophages (Figure 6E and 6F). These results suggested that ROS are located upstream of JNK activation. In agreement with the effect of JNK inhibitor, addition of either NAC or DFO at the same dosages as above, markedly suppressed survival/replication of L. major in macrophages (Figure 6G). These results indicated important roles for ROS and JNK in both chemokine production and parasite replication in macrophages.
Figure 6. Effects of antioxidants on ROS generation, JNK activation, KC release, and intramacrophagic parasite growth.
(A, B) Macrophages were loaded with DCFH-DA, washed and infected or not with L. major for 4 h in the presence of medium, antioxidants DFO (A), or NAC (B). Results indicate arbitrary units of fluorescence and are mean and SE of triplicates. (C, D) Macrophages were infected or not in the presence of medium, DFO (C), or NAC (D). After 4 h, the levels of JNK and p-JNK were determined by western blotting. (E, F) Macrophages were infected or not in the presence of medium, DFO (E), or NAC (F). The levels of KC were determined by ELISA after 20 h of infection. (G) Macrophages were infected overnight and cultured for additional 3 d in the presence of medium, DFO or NAC. Intracellular load of parasites was evaluated. Results are mean and SE of extracellular promastigotes produced. *P<0.05, **P<0.01.
Discussion
Our results indicated that infection with L. major induces a cellular stress response in tissue resident macrophages, characterized by increased ROS generation, SAPK/JNK activation, c-Jun activation, and increased FasL expression. Previous studies indicate that infection with Leishmania induces oxidative stress in macrophages [3], [19], [20]. In agreement, our results indicated that infection with L. major increased ROS generation in tissue resident macrophages. Inflammatory macrophages, on the other hand, had already increased levels of ROS, which did not increase further upon Leishmania infection. Increased production of ROS activates the SAPK/JNK pathway [21]–[23]. In agreement with this notion, our data demonstrated that infection activated JNK and c-Jun in resident macrophages. Infection did not activate, or marginally activated JNK and c-Jun in inflammatory macrophages. However, it should be noted that inflammatory macrophages already expressed elevated levels of ROS and activated JNK prior to infection. Our results disagree with previous studies showing downregulation of MAPK activity induced by L. major infection [28]. Perhaps differences in the virulence of the parasite isolate and the use of a retrovirally transformed macrophage cell line in the latter studies [28] could explain the different results.
Cellular stress induces FasL expression through the JNK pathway [13]–[15]. In agreement, our data showed that infection increased expression of both surface and soluble FasL by macrophages. However, our results revealed strain differences in the effects of FasL on infected macrophages. In contrast to FasL-mediated death in BALB/c macrophages [9], infected B6 macrophages remained viable in spite of Fas and FasL expression. Expression of FasL is immunoprotective for L. major infection in resistant [29]–[31], but is deleterious in susceptible mice [9]. Furthermore, KC secretion and neutrophil extravasation did not require FasL. Different factors could be involved in these differences. First, BALB/c and B6 FasL molecules express a genetic polymorphism, where BALB/c FasL has greater cytotoxic activity than B6 FasL [32]. Second, soluble FasL could inhibit FasL-mediated cytotoxicity [33]. Third, as L. pifanoi and L. amazonensis block macrophage apoptosis through activation of PI3K/Akt pathway [34], L. major could induce anti-apoptotic signaling more efficiently in B6 macrophages. Our results suggested that FasL does not have a role in the initial stages of Leishmania infection in resistant mice.
Infection with L. major increased the secretion of TNF-α, IL-6, TIMP-1, IL-1RA, G-CSF and TREM, but not IL-1α or IL-1β. In addition, infection increased secretion of chemokines KC, MIP-1α, MIP-1β, MCP-1 and MIP-2. Our results agreed with previous reports of increased expression of TNF-α, MIP-1α, MIP-1β, MIP-2, MCP-1 and KC [6], [7]. One study also identified increased gene expression for IL-1RA and unchanged gene expression for IL-1β [7]. Our studies were done at the protein level, and found that infection did not induce secretion of IL-1β by resident macrophages. However, it is likely that IL-1 can be produced by other phagocytes [35]. The role of IL-1RA is unclear, since IL-1 is dispensable for protection of B6 mice [35]. Furthermore, our results showed that infection increased TIMP-1 expression by resident macrophages, and we also found increased metalloproteinase expression following infection (data not shown). These results are relevant for disease, since expression of TIMP-1 (a tissue inhibitor of metalloproteinases) could be involved in the regulation of metalloproteinase activity, tissue damage and spread of infection in cutaneous and visceral leishmaniasis [36], [37]. Our results also indicated a sentinel role for resident macrophages, through release of several chemokines upon infection with L. major.
Infection activated the JNK pathway and induced secretion of the chemokine KC (CXCL1). Secretion of KC was completely blocked by the JNK inhibitor SP600125, and partially blocked by the ERK inhibitor SB203580, but not by p38 inhibitor PD98059. These results suggested that JNK pathway, and ERK pathway to a lesser extent, are involved in chemokine secretion induced by infection. JNK inhibitor SP600125 also inhibited parasite replication in macrophages, suggesting a role for JNK in intracellular parasite survival and growth. It is interesting that JNK both induces inflammatory signals like KC and promotes parasite growth. However, Leishmania parasites express homologues of mammalian MAPK [38]. Therefore, we cannot discard that the JNK inhibitor could affect the parasite directly. Further studies are necessary to identify the mechanisms by which JNK inhibitor blocks the intramacrophage replication of the parasite. Oxidative stress activates the JNK pathway [21]–[23]. Our results demonstrated that, besides blocking ROS generation, antioxidants DFO and NAC partially decreased JNK activation and reduced KC secretion induced by infection. Taken together, these results suggested that infection triggers an intracellular pathway that sequentially recruits ROS, JNK and KC. In agreement with the anti-parasite effects of the JNK inhibitor, DFO and NAC potently inhibited intracellular parasite replication in macrophages. Our data agree with the recently identified role of ROS in intracellular survival/growth of Leishmania and Trypanosoma cruzi parasites [4], [5], [39]. However, it should be noted that ROS inhibitors induced a more potent blockade in parasite replication than in JNK activation. ROS could have direct effects on parasite replication and additional indirect effects besides activation of the JNK pathway. For example, ROS are critically involved in M2-type macrophage differentiation [40]. In agreement with this possibility, neutrophil elastase, a potent ROS inducer, promotes M2-type differentiation, which favors replication of L. major in macrophages [41].
In conclusion, infection with L. major induces a cellular stress response in tissue resident macrophages. The stress response includes ROS generation and activation of the JNK/c-Jun/FasL cascade, leading to chemokine secretion and increased parasite survival. How this stress response is generated remains to be investigated. Sustained movement of L. donovani parasites inside macrophages leads to plasma membrane wounding and repair through lysosomal exocytosis [42]. Membrane wounding could be the stimulus for triggering a stress response. Interestingly, infection of macrophages with L. donovani generates ceramide [43], which is known to activate the SAPK/JNK pathway [12], and is required for parasite survival [43]. Together, these and our results suggest new targets for therapeutic intervention in leishmanial infection.
Materials and Methods
Ethics Statement
This study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health (USA). The protocol was approved by the Committee on the Ethics of Animal Experiments of the Health Science Center of the Federal University of Rio de Janeiro (CEUA-CCS, Permit Number: IBCCF 178) and all efforts were made to minimize suffering.
Antibodies and Chemicals
Dulbecco’s Modified Eagle’s Medium (DMEM), RPMI medium, fetal calf serum (FCS), glutamine, gentamicin, sodium pyruvate, MEM nonessential amino acids, and HEPES buffer were obtained from GIBCO/Invitrogen. The following reagents were used: Nutridoma SP (Roche); propidium iodide, DMSO, PE-conjugated Annexin V, hamster IgG1/κ, PE- and FITC-conjugated hamster anti-mouse Fas and FasL monoclonal antibodies (mAbs), APC/Cy7-conjugated anti-Ly6G, purified hamster anti-FasL MFL3 mAb, hamster IgG1 isotype control, anti-CD16/CD32 mAb (FcBlock), all from BD Biosciences; PerCP/Cy5.5-conjugated anti-Ly6C mAb HK1.4 (eBioscience); rabbit SAPK/JNK mAb 56G8; phospho-SAPK/JNK (Thr183/Tyr185) mAb 81E11; anti-c-Jun mAb 60A8, phospho-c-Jun-Ser63 mAb 54B3, Goat anti-rabbit IgG, HRP-conjugated (Cell Signaling); JNK inhibitor SP600125 (Enzo Life Sciences), ERK (MEK) inhibitor PD98059, p38 inhibitor SB203580 (EMD Millipore).
Mice and Parasites
C57BL/6 (B6) and BALB/c mice were from Oswaldo Cruz Institute, Rio de Janeiro, Brazil. For flow cytometry experiments, wild-type B6 and FasL-deficient mutant gld B6 mice were obtained from The Jackson Laboratory. All animal work was approved and conducted according institutional guidelines. Leishmania major (L. major) strain LV39 (MRHO/Sv/59/P) was isolated from BALB/c mice, and maintained in vitro for up to 4 wk [44]. Parasites were maintained in Schneider medium (Life Technologies) supplemented with 10% FCS, 1% glutamine and 2% human urine [8], [45].
Macrophages and Infection
Resident macrophages were obtained by washing the peritoneal cavity of B6 mice and discarding nonadherent cells after 20 h culture. Inflammatory macrophages were obtained 4 d after i.p. injection of 1 ml of 3% thioglycollate broth (Sigma-Aldrich). Nonadherent cells were discarded after 4–20 h. Resident (2×105) and inflammatory cells (1.5×105) were cultured on 48-well plates (Nunc, Denmark), yelding approximately 1×105 adherent macrophages. Cultures were done in 0.5 ml supplemented DMEM medium containing 10% FCS or 1% Nutridoma. DMEM and RPMI media were supplemented with glutamine, 2-ME, gentamicin, sodium pyruvate, MEM nonessential amino acids, HEPES buffer, and 10% FCS or 1% Nutridoma. Adherent macrophages were infected with L. major promastigotes at 10∶1 parasite/macrophage ratio for 4–20 h at 37°C and 7% CO2.
Assessment of Parasite Load
For assessment of parasite internalization, resident and inflammatory macrophage monolayers (105 adherent cells) were established in glass coverslips and infected in replicates with L. major promastigotes at a 10∶1 parasite/cell ratio. After 4 h at 37°C, extracellular parasites were washed. Coverslips were stained by Romanowsky stain, and both percentage of infected macrophages and parasite number per 100 macrophages were determined. For assessment of parasite load after 3 d of infection, resident macrophages (1×105) were treated with either solvent or inhibitors 3 h prior to infection, and infected with 1×106 L. major promastigotes in DMEM supplemented with 10% FCS or 1% Nutridoma in 48-well vessels. After 20 h, extracellular parasites were removed, and macrophages were cultured with medium containing 10% FCS or 1% Nutridoma in the continued presence of the inhibitors for additional 3 d. All cultures were washed and transferred to Schneider medium (GIBCO-Invitrogen) supplemented with 20% FCS, 1% glutamine, 2% human urine, as described [8], [43], and maintained at 26°C for additional 3 d. The relative intracellular load of L. major was assessed by counting the number of motile extracellular promastigotes released in each well [8], [45].
Detection of ROS
Intracellular levels of ROS were measured by oxidation of nonfluorescent 2′, 7′ dichlorofluorescin probe, delivered as diacetate form (DCFH-DA), to the fluorescent product 2′,7′ dichlorofluorescein [46]. Resident and inflammatory macrophages (105 cells) were prepared in 96-well plates, and loaded for 10 min at 37°C with 10 µM DCFH-DA (Sigma-Aldrich). Macrophages were washed and infected with L. major for 4 h. In preliminary kinetic experiments, this time of infection gave the strongest signal for this parasite isolate. Macrophages were washed again and fluorescence was measured (485 nm excitation; 535 nm emission) after 60 min in an FLx800 Fluorescence Microplate Reader (BioTek).
Western Blot Analysis
Macrophages were infected or not with L. major, washed and incubated for 4 h. For detection of metalloproteinases, macrophages were incubated for 48–72 h. After culture, cells were washed in PBS and treated with ice-cold RIPA lysis buffer containing protease inhibitor cocktail and sodium orthovanadate 2 mM for 20 min. The suspensions were collected, homogenized and centrifuged in 10,000 g for 20 min at 4°C. The supernatants were obtained and the protein content evaluated by the Bradford method. Proteins were precipitated with 90% ice-cold ethanol in order to obtain equal amounts of protein samples. Protein samples (80 µg/lane) were suspended in 2X Laemmli sample buffer and 5% β-mercaptoethanol. After boiling for 5 min, samples were separated in 10% acrylamide SDS-PAGE, and electrotransferred to nitrocellulose membranes (Hybond-C, Amersham Biosciences) using the Bio-Rad mini vertical Trans-Blot Cell system. Blots were blocked with TBS-3% BSA for 1 h at room temperature, and incubated with the primary antibodies (1∶1,000) in TBS-3% BSA-0.05% sodium azide for 18 h at 4°C. Blots were then washed 3 times with TBS-0.05% Tween-20 for 10 min, once with TBS for 5 min at room temperature, and then incubated with HRP-conjugated (1∶2,000), IRDye 680LT or IRDye 800CW-conjugated (1∶10,000) secondary antibodies in TBS-3% BSA for 1 h at room temperature. After one more wash cycle, the antibodies were detected with ECL Plus Western Blotting detection system, GE Healthcare Life Sciences (Pittsburgh, PA) or by fluorescence imaging using a Li-Cor Odyssey infrared scanner. The images were processed using Adobe Photoshop CS and ImageJ softwares. Protein loading was verified by either red Ponceau staining or immunoblotting. For densitometric analysis, blots were scanned, and intensities of bands were quantitated with ImageJ software. The area of both p54 and p46 bands of p-JNK were measured. Intensities were normalized as percentages of the maximum values (total JNK staining).
Flow Cytometry
Adherent macrophages were detached by treatment with PBS-5 mM EDTA-1% FCS, washed in staining buffer containing 2% FCS, and incubated with anti-CD16/CD32 (Fc block). Cells were stained with antibodies for 30 min at 4°C. Cells were gated for F4/80+ CD11b+7AAD− viable macrophages, and analysed for staining with PE-Annexin V and FITC-anti-FasL. Cells were acquired on a FACSCalibur™ flow cytometer, by using Cell quest software (BD Biosciences). For analysis, FlowJo™ software was used (TreeStar).
Cell Viability Assay
Macrophage viability was determined by lysozyme activity in culture supernatants. Lysozyme is a marker of macrophage viability [47]. Lysozyme activity was measured by fluorescence quenching of fluorescently labeled Micrococcus lysodeikticus cell walls (EnzChek™ Lysozyme Assay Kit; Life Technologies). As a negative control, macrophages were fixed with 4% paraformaldehyde (PFA) to measure residual lysozyme activity.
Production of Cytokines and Chemokines
Supernatants from either uninfected or infected macrophages were simultaneously assayed for 40 different cytokines and chemokines using the Proteome Profiler™ Mouse Cytokine Antibody Array Kit, according to the manufacturer instructions (R&D Systems). The densities of individual stainings were compared with image processing software ImageJ 1.46 r. Data are mean and SE of duplicates. In addition, supernatants were assayed for soluble FasL, IL-1β, IL-6, KC, and TNF-α by sandwich ELISA (R&D Systems). Results are mean and SE of triplicate cultures.
Statistical Analysis
Quantitative data shown are representative experiments involving pools at 2–3 animals, and were repeated at least three times, with similar results. Data represent mean and SE of triplicates, at least. Data were analysed by Student’s t test for independent samples, using SigmaPlot™ for Windows. Differences with a P value < 0.05 or lower were considered significant. Proteomic profiling was repeated twice with similar results. Densitometric data of readings were normalized as percentage of a positive control provided by the kit. Data were compared in quadruplicates using non-parametric Mann-Whitney U test. Cytokines which gave a significant increase (P<0.05 or lower) following infection are marked by an asterisk.
Funding Statement
This work was supported by Brazilian National Research Council (CNPq), Rio de Janeiro State Science Foundation (FAPERJ), and Programa Institutos Nacionais de Ciência e Tecnologia (INCT), CNPq, Brazil. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Fortier AH, Hoover DL, Nacy CA (1982) Intracellular replication of Leishmania tropica in mouse peritoneal macrophages: amastigote infection of resident cells and inflammatory exudate macrophages. Infect Immun 38: 1304–1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Belkaid Y, Butcher B, Sacks DL (1998) Analysis of cytokine production by inflammatory mouse macrophages at the single-cell level: selective impairment of IL-12 induction in Leishmania-infected cells. Eur J Immunol 28: 1389–1400. [DOI] [PubMed] [Google Scholar]
- 3. Van Assche T, Deschacht M, da Luz RA, Maes L, Cos P (2011) Leishmania-macrophage interactions: insights into the redox biology. Free Radic Biol Med 51: 337–351. [DOI] [PubMed] [Google Scholar]
- 4. Mittra B, Cortez M, Haydock A, Ramasamy G, Myler PJ, et al. (2013) Iron uptake controls the generation of Leishmania infective forms through regulation of ROS levels. J Exp Med 210: 401–416.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sardar AH, Kumar S, Kumar A, Purkait B, Das S, et al. (2013) Proteome changes associated with Leishmania donovani promastigote adaptation to oxidative and nitrosative stresses. J Proteomics 81: 185–199. [DOI] [PubMed] [Google Scholar]
- 6. Matte C, Olivier M (2002) Leishmania-induced cellular recruitment during the early inflammatory response: modulation of proinflammatory mediators. J Infect Dis 185: 673–681. [DOI] [PubMed] [Google Scholar]
- 7. Rabhi I, Rabhi S, Ben-Othman R, Rasche A, Daskalaki A, et al. (2012) Transcriptomic signature of Leishmania infected mice macrophages: a metabolic point of view. PLoS Negl Trop Dis 6: e1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ribeiro-Gomes FL, Otero AC, Gomes NA, Moniz-De-Souza MC, Cysne-Finkelstein L, et al. (2004) Macrophage interactions with neutrophils regulate Leishmania major infection. J Immunol 172: 4454–4462. [DOI] [PubMed] [Google Scholar]
- 9. Ribeiro-Gomes FL, Moniz-de-Souza MC, Borges VM, Nunes MP, Mantuano-Barradas M, et al. (2005) Turnover of neutrophils mediated by Fas ligand drives Leishmania major infection. J Infect Dis 192: 1127–1134. [DOI] [PubMed] [Google Scholar]
- 10. Ribeiro-Gomes FL, Moniz-de-Souza MC, Alexandre-Moreira MS, Dias WB, Lopes MF, et al. (2007) Neutrophils activate macrophages for intracellular killing of Leishmania major through recruitment of TLR4 by neutrophil elastase. J Immunol 179: 3988–3994. [DOI] [PubMed] [Google Scholar]
- 11. Davis RJ (2000) Signal transduction by the JNK group of MAP kinases. Cell 103: 239–252. [DOI] [PubMed] [Google Scholar]
- 12. Verheij M, Bose R, Lin XH, Yao B, Jarvis WD, et al. (1996) Requirement for ceramide-initiated SAPK/JNK signalling in stress-induced apoptosis. Nature 380: 75–79. [DOI] [PubMed] [Google Scholar]
- 13. Faris M, Kokot N, Latinis K, Kasibhatla S, Green DR, et al. (1998) The c-Jun N-terminal kinase cascade plays a role in stress-induced apoptosis in Jurkat cells by up-regulating Fas ligand expression. J Immunol 160: 134–144. [PubMed] [Google Scholar]
- 14. Kasibhatla S, Brunner T, Genestier L, Echeverri F, Mahboubi A, et al. (1998) DNA damaging agents induce expression of Fas ligand and subsequent apoptosis in T lymphocytes via the activation of NF-kappa B and AP-1. Mol Cell 1: 543–551. [DOI] [PubMed] [Google Scholar]
- 15. Le-Niculescu H, Bonfoco E, Kasuya Y, Claret FX, Green DR, et al. (1999) Withdrawal of survival factors results in activation of the JNK pathway in neuronal cells leading to Fas ligand induction and cell death. Mol Cell Biol 19: 751–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Himes SR, Sester DP, Ravasi T, Cronau SL, Sasmono T, et al. (2006) The JNK are important for development and survival of macrophages. J Immunol 176: 2219–2228. [DOI] [PubMed] [Google Scholar]
- 17. Swantek JL, Cobb MH, Geppert TD (1997) Jun N-terminal kinase/stress-activated protein kinase (JNK/SAPK) is required for lipopolysaccharide stimulation of tumor necrosis factor alpha (TNF-alpha) translation: glucocorticoids inhibit TNF-alpha translation by blocking JNK/SAPK. Mol Cell Biol 17: 6274–6282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Das M, Sabio G, Jiang F, Rincon M, Flavell RA, et al. (2009) Induction of hepatitis by JNK-mediated expression of TNF-alpha. Cell 136: 249–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gantt KR, Goldman TL, McCormick ML, Miller MA, Jeronimo SM, et al. (2001) Oxidative responses of human and murine macrophages during phagocytosis of Leishmania chagasi . J Immunol 167: 893–901. [DOI] [PubMed] [Google Scholar]
- 20. Mallinson DJ, Coombs GH (1989) Interaction of Leishmania metacyclics with macrophages. Int J Parasitol 19: 647–656. [DOI] [PubMed] [Google Scholar]
- 21. Benhar M, Engelberg D, Levitzki A (2002) ROS, stress-activated kinases and stress signaling in cancer. EMBO Rep 3: 420–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hojo Y, Saito Y, Tanimoto T, Hoefen RJ, Baines CP, et al. (2002) Fluid shear stress attenuates hydrogen peroxide-induced c-Jun NH2-terminal kinase activation via a glutathione reductase-mediated mechanism. Circ Res 91: 712–718. [DOI] [PubMed] [Google Scholar]
- 23. Pfeiffer ZA, Guerra AN, Hill LM, Gavala ML, Prabhu U, et al. (2007) Nucleotide receptor signaling in murine macrophages is linked to reactive oxygen species generation. Free Radic Biol Med 42: 1506–1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kavurma MM, Khachigian LM (2003) Signaling and transcriptional control of Fas ligand gene expression. Cell Death Differ 10: 36–44. [DOI] [PubMed] [Google Scholar]
- 25. Marguet D, Luciani MF, Moynault A, Williamson P, Chimini G (1999) Engulfment of apoptotic cells involves the redistribution of membrane phosphatidylserine on phagocyte and prey. Nat Cell Biol 1: 454–456. [DOI] [PubMed] [Google Scholar]
- 26. Callahan MK, Williamson P, Schlegel RA (2000) Surface expression of phosphatidylserine on macrophages is required for phagocytosis of apoptotic thymocytes. Cell Death Differ 7: 645–653. [DOI] [PubMed] [Google Scholar]
- 27. Feng GJ, Goodridge HS, Harnett MM, Wei XQ, Nikolaev AV, et al. (1999) Extracellular signal-related kinase (ERK) and p38 mitogen-activated protein (MAP) kinases differentially regulate the lipopolysaccharide-mediated induction of inducible nitric oxide synthase and IL-12 in macrophages: Leishmania phosphoglycans subvert macrophage IL-12 production by targeting ERK MAP kinase. J Immunol 163: 6403–6412. [PubMed] [Google Scholar]
- 28. Gomez MA, Contreras I, Hallé M, Tremblay ML, McMaster RW, et al. (2009) Leishmania GP63 alters host signaling through cleavage-activated protein tyrosine phosphatases. Sci Signal 2: ra58. [DOI] [PubMed] [Google Scholar]
- 29. Conceição-Silva F, Hahne M, Schröter M, Louis J, Tschopp J (1998) The resolution of lesions induced by Leishmania major in mice requires a functional Fas (APO-1, CD95) pathway of cytotoxicity. Eur J Immunol 28: 237–245. [DOI] [PubMed] [Google Scholar]
- 30. Huang FP, Xu D, Esfandiari EO, Sands W, Wei XQ, et al. (1998) Mice defective in Fas are highly susceptible to Leishmania major infection despite elevated IL-12 synthesis, strong Th1 responses, and enhanced nitric oxide production. J Immunol 160: 4143–4147. [PubMed] [Google Scholar]
- 31. Chakour R, Guler R, Bugnon M, Allenbach C, Garcia I, et al. (2003) Both the Fas ligand and inducible nitric oxide synthase are needed for control of parasite replication within lesions in mice infected with Leishmania major whereas the contribution of tumor necrosis factor is minimal. Infect Immun 71: 5287–5295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kayagaki N, Yamaguchi N, Nagao F, Matsuo S, Maeda H, et al. (1997) Polymorphism of murine Fas ligand that affects the biological activity. Proc Natl Acad Sci USA 94: 3914–3919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Suda T, Hashimoto H, Tanaka M, Ochi T, Nagata S (1997) Membrane Fas ligand kills human peripheral blood T lymphocytes, and soluble Fas ligand blocks the killing. J Exp Med 186: 2045–2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ruhland A, Leal N, Kima PE (2007) Leishmania promastigotes activate PI3K/Akt signalling to confer host cell resistance to apoptosis. Cell Microbiol 9: 84–96. [DOI] [PubMed] [Google Scholar]
- 35. Kautz-Neu K, Kostka SL, Dinges S, Iwakura Y, Udey MC, et al. (2011) IL-1 signalling is dispensable for protective immunity in Leishmania-resistant mice. Exp Dermatol 20: 76–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Maretti-Mira AC, de Oliveira-Neto MP, Da-Cruz AM, de Oliveira MP, Craft N, et al. (2011) Therapeutic failure in American cutaneous leishmaniasis is associated with gelatinase activity and cytokine expression. Clin Exp Immunol 163: 207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Choudhury R, Das P, De T, Chakraborti T (2013) 115 kDa serine protease confers sustained protection to visceral leishmaniasis caused by Leishmania donovani via IFN-γ induced down-regulation of TNF-α mediated MMP-9 activity. Immunobiology 218: 114–126. [DOI] [PubMed] [Google Scholar]
- 38. Wiese M, Wang Q, Görcke I (2003) Identification of mitogen-activated protein kinase homologues from Leishmania mexicana . Int J Parasitol 33: 1577–1587. [DOI] [PubMed] [Google Scholar]
- 39. Paiva CN, Feijó DF, Dutra FF, Carneiro VC, Freitas GB, et al. (2012) Oxidative stress fuels Trypanosoma cruzi infection in mice. J Clin Invest 122: 2531–2542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Zhang Y, Choksi S, Chen K, Pobezinskaya Y, Linnoila I, et al. (2013) ROS play a critical role in the differentiation of alternatively activated macrophages and the occurrence of tumor-associated macrophages. Cell Res 23: 898–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Filardy AA, Pires DR, Nunes MP, Takiya CM, Freire-de-Lima CG, et al. (2010) Proinflammatory clearance of apoptotic neutrophils induces an IL-12(low)IL-10(high) regulatory phenotype in macrophages. J Immunol 185: 2044–2050. [DOI] [PubMed] [Google Scholar]
- 42. Forestier CL, Machu C, Loussert C, Pescher P, Späth GF (2011) Imaging host cell-Leishmania interaction dynamics implicates parasite motility, lysosome recruitment, and host cell wounding in the infection process. Cell Host Microbe 9: 319–330. [DOI] [PubMed] [Google Scholar]
- 43. Majumder S, Dey R, Bhattacharjee S, Rub A, Gupta G, et al. (2012) Leishmania-induced biphasic ceramide generation in macrophages is crucial for uptake and survival of the parasite. J Infect Dis 205: 1607–1616. [DOI] [PubMed] [Google Scholar]
- 44. Louis J, Moedder E, Behin R, Engers H (1979) Recognition of protozoan parasite antigens by murine T lymphocytes. I. Induction of specific T lymphocyte-dependent proliferative response to Leishmania tropica . Eur J Immunol 9: 841–847. [DOI] [PubMed] [Google Scholar]
- 45. Gomes NA, Gattass CR, Barreto-De-Souza V, Wilson ME, DosReis GA (2000) TGF-beta mediates CTLA-4 suppression of cellular immunity in murine kalaazar. J Immunol 164: 2001–2008. [DOI] [PubMed] [Google Scholar]
- 46. Sundaresan M, Yu ZX, Ferrans VJ, Irani K, Finkel T (1995) Requirement for generation of H2O2 for platelet-derived growth factor signal transduction. Science 270: 296–299. [DOI] [PubMed] [Google Scholar]
- 47. Gordon S, Todd J, Cohn ZA (1974) In vitro synthesis and secretion of lysozyme by mononuclear phagocytes. J Exp Med 139: 1228–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]