Abstract
HIV replication is only partially controlled by HIV-specific activated effector T cells in chronic HIV infection and strategies are warranted to improve their efficacy. Chronic T cell activation is generally accompanied by regulation of antigen-specific T cell responses which may impair an effective control of chronic infections. The impact of HIV-induced T cell regulation on individual patients’ disease progression is largely unknown, since classical T cell activation assays reflect net activation with regulation as unknown contributing factor. We here explore a quantitative parameter for antigen-induced cytokine-mediated regulation (RAC) of HIV-specific effector T cell activation by functional antibody-blockade of IL-10 and transforming growth factor-β. HIV Env- and Gag-specific T cell activation and RAC were estimated in peripheral blood mononuclear cells from 30 treatment-naïve asymptomatic HIV-infected progressors (CD4 count 472/µl, HIV RNA 37500 copies/ml) stimulated with overlapping peptide panels for 6 days. RAC was estimated from differences in T cell activation between normal and blocked cultures, and related to annual CD4 loss, immune activation (CD38) and microbial translocation (plasma lipopolysaccharides). RAC was heterogeneously distributed between individual patients and the two HIV antigens. Notably, RAC did not correlate to corresponding classical activation. Env RAC correlated with CD38 and CD4 loss rates (r> = 0.37, p = <0.046) whereas classical Gag activation tended to correlate with HIV RNA (r = −0.35, p = 0.06). 14 patients (47%) with low RAC’s to both Env and Gag had higher CD8 counts (p = 0.014) and trends towards lower annual CD4 loss (p = 0.056) and later start with antiretroviral treatment (p = 0.07) than the others. In contrast, patients with high RAC to both Env and Gag (n = 8) had higher annual CD4 loss (p = 0.034) and lower CD8 counts (p = 0.014). RAC to Env and Gag was not predicted by classical activation parameters and may thus provide additional information on HIV-specific immunity. RAC and other assessments of regulation deserve further in-depth exploration.
Introduction
Chronic human immunodeficiency virus type 1 (HIV) infection leads to a variable but progressive loss of immune functions in most patients. The progression rate is mainly influenced by two opposing factors, namely HIV-associated chronic immune activation [1]–[3] and the efficacy of HIV-specific T cell responses [4], [5]. Chronic immune activation expressed by CD38 on T cells, correlates strongly to disease progression and mortality [6]–[8]. It is partly sustained by enhanced systemic translocation of microbial products such as bacterial lipopolysaccharide (LPS) [9], [10] and induces polyclonal B and T cell activation [11], [12], accelerated T cell turnover [13], [14] and immune exhaustion [2], [15]. Effective viral control, on the other hand, seems to depend on the presence of polyfunctional HIV-specific CD8+ T cells [4].
A less clarified aspect of HIV-specific immunity is downregulation of the HIV-specific effector T cells, where regulatory T cells (Treg) play a central role [16], [17]. Regulation of effector T cells protects the host from damage in chronic infection, but may also impair effective immune control. It is mediated by a number of mechanisms, including the expression of inhibitory receptors in the immune synapse such as CTLA-4 [18] and programmed death-1 (PD-1) [19], [20], or via soluble inhibitory cytokines, particularly IL-10 and transforming growth factor-β (TGF-ß). These two key inhibitory cytokines impede pro-inflammatory responses by T cells, natural killer cells, monocytes and macrophages and are secreted by a number of cell types including Treg [21]–[24].
The efficacy of T cell responses depends on the sum of stimulatory and regulatory signals. T cell regulation has been intensively studied, but with focus on single regulating mechanisms. However, how these various regulating mechanisms finally and in concert influence HIV-specific T effector cells and disease progression in individual patients has been little explored. This might be assessed for T cells in vitro by blocking downstream intracellular regulatory signal pathways during antigen stimulation. Recently we tested such an in vitro quantitative parameter for regulation in patients on antiretroviral treatment (ART) during reboost with a Gag peptide-based therapeutic HIV vaccine [25]. We estimated vaccine-specific cytokine-mediated regulation of CD8+ T cell responses by blocking the effects of IL-10 and TGF (antigen-induced cytokine-mediated regulation, RAC). Notably, changes in RAC explained the substantial variations in booster efficacy, including cases where vaccine responses waned after each booster.
Since RAC seemed to reflect important features of HIV vaccine-specific T cell immunity during immunization, we hypothesized that the same parameter also would provide novel information in natural chronic HIV infection. In this study, we therefore compared RAC and activation of Gag- and Env-specific T effector cells in treatment-naïve patients. We found RAC to be heterogeneous, both between individual patients and between the two HIV antigens, and unfavourably related to HIV progression.
Materials and Methods
Patients
Thirty asymptomatic HIV-1 seropositive ART-naïve viremic progressors were included (23 males, 7 females). Their clinical characteristics are shown in Table 1. The patients represented a spectre of HIV-associated immune activation determined by CD38 densities on total CD8+ and CD8+PD-1+ T cells [8] and were chosen from a larger cross-sectional prospective study on immunological factors in HIV. The study was approved by the Norwegian South-Eastern Regional Committee for Medical and Health Research Ethics. Informed consent was signed by each participant.
Table 1. Cohort characteristics.
| All (n = 30) | |
| Median (IQ range) | |
| Age (years) | 42 (33–49) |
| Time HIV seropositive (months) | 57 (16–83) |
| CD4+ T cell count (×106/l) | 472 (325–695) |
| CD8+ T cell count (×106/l) | 1084 (788–1828) |
| HIV-RNA in plasma (copies/ml) | 37500 (2300–72000) |
| Annual CD4 T cell count loss (cells ×106/l) | 11 (−69–177) |
| β2-microglobulin in serum (mg/l) | 2.5 (1.9–3.3) |
| CD38 on CD8+ T cells (molecules/cell) | 3285 (1834–7226) |
| CD38 on CD8+CD38+PD-1+ T cells (molecules/cell) | 4127 (2095–8704) |
| LPS (pg/µl) | 70 (59–86) |
Activation Assays and Flow Cytometry
Peripheral-blood mononuclear cells (PBMC) were isolated using Cell Preparation Tubes (Becton Dickinson (BD), CA, USA) and preserved, thawed and cultured in serum-free AIM culture medium containing 0.5% human albumin at 5% CO2 at 37°C, as described elsewhere [26]. To evaluate activation and proliferation parameters, the fractions of T cells co-expressing CD25 and HLA-DR [27] or having low carboxyfluorescein succinimidyl ester (CFSEdim) signal [28] were compared. PBMC were pulse-labelled with CFSE (3 µM, 5 min (Invitrogen Molecular Probes, OR, USA) as detailed previously [29] and subjected to HIV antigens (four HIV-1 Gag p24 consensus peptide sequences, represented by 15-mer overlapping by 2 amino acid panels [29] and non-HIV antigens (23 15-mer peptides from cytomegalovirus, Epstein-Barr virus and influenza virus (CEF, Mabtech, Sweden)).
For the estimates of antigen-specific cytokine-mediated regulation of T cell activation (RAC), cryopreserved PBMC were thawed, washed and reconstituted in serum-free AIM overnight, and then stimulated with complete 15-mer Env or Gag overlapping peptide panels (NIH AIDS Research and Reference Reagent Program, MD, USA) as detailed elsewhere [30]. Peptide panels in all experiments were used at 2 µg/ml/peptide. Peptide-exposed and control cultures were in parallel incubated with inhibitory monoclonal antibodies (mAbs) to IL-10 and TGF-ß, each at 10 µg/ml final concentration according to the instructions by the manufacturer (R&D Systems Europe, Abingdon, UK), a concentration that abolished IL-10 in cell culture supernatants (Luminex assay of supernatants from antigen stimulated T cells cultured for 6 days, data not shown). Staphylococcal enterotoxin B (Sigma-Aldrich, MO, USA) was used as positive control at 0.5 µg/ml.
Cells were cultured at 37 Co in 5% CO2 for 6 days, and then harvested, stained and prepared for flow cytometric analysis as previously described [31]. The following fluorochrome-labelled mAbs were used: CD3 Pacific Blue, CD8 AmCyan, HLA-DR PE-Cy7 (BD), CD4 PE and CD25 APC (eBioscience, CA, USA). 7-aminoactinomycin (7-AAD, BD) was added to discriminate between viable and non-viable cells according to the manufacturer. Flow cytometry data were obtained with a BD FACS Canto II with BD Diva software v6.1. Only lymphocyte and lymphoblast gates containing live 7-AAD− CD3+ T lymphocytes were evaluated.
Quantification of Env and Gag Related T Cell Activation
Antigen-specific activation of T cell subsets was defined as the difference in activation marker between peptide-stimulated cells and corresponding control cells without peptides. In preceding experiments exploring T cell regulation by HIV vaccine antigens in patients on ART, regulation and activation were determined by differences in proliferation (CFSEdim) in CFSE pulse-labelled cells [25]. In our experience, thawed PBMC samples from ART-naïve individuals are more vulnerable to toxic effects of CFSE [32], even after short exposure and low concentrations. We therefore compared fractions of CFSEdim, defined by median fluorescence intensities equal to or below the second proliferated generation in CFSE-labelled PBMC, and fractions of CD25+HLA-DR+. These parameters reflect overlapping aspects of T cell activation [27], i.e. proliferation, IL-2 receptor expression and increased HLA class II expression), as illustrated in Fig. 1A, with correlating activation results after exposure to both non-HIV and HIV antigens (Fig. 1B). T cell activation within the cohort was therefore determined by the frequency of subsets co-expressing CD25 and HLA-DR in antigen-stimulated cultures corrected for unstimulated controls [27].
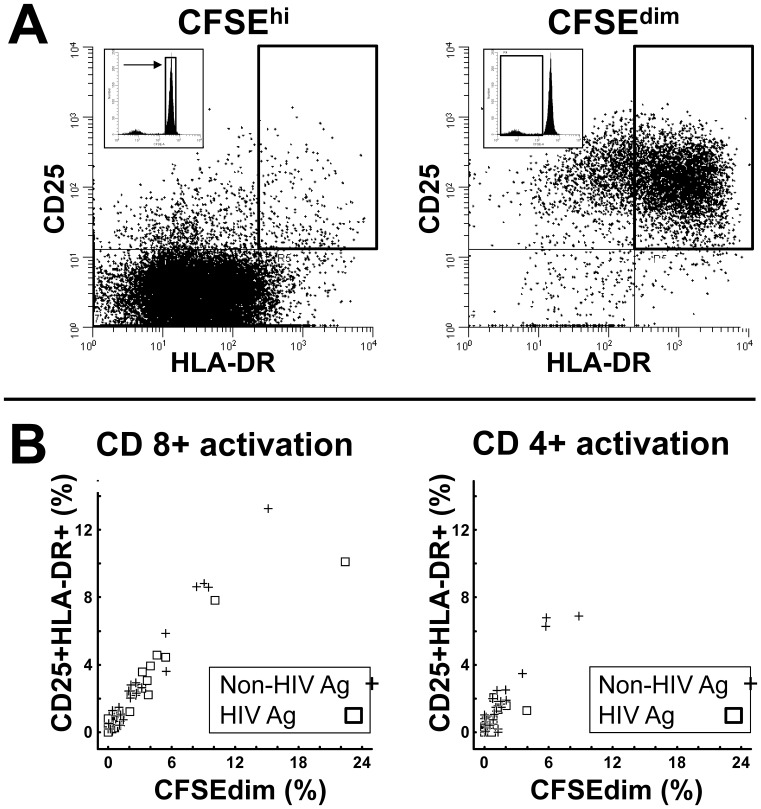
Figure 1. Comparison of CD25+HLA-DR+ expression and CFSEdim as measures for antigen-induced activation and regulation of T cells.
CFSE-labelled PBMC from 28 HIV-infected individuals were stimulated for 6 days with peptides encoding either HIV p24 consensus regions (HIV Ag) or a pool of commonly encountered non-HIV viral peptides (Non-HIV Ag). A. Co-expression of CD25 and HLA-DR on live CD8+CD3+ T cells on non-divided CFSEhigh (left panel) and proliferated CFSEdim T cells (right panel), showing excessive difference in fractions of CD25+HLA-DR+ in the activated subset to the right. B. Scatter plots of activation measured in the same culture by CFSEdim or HLA-DR+CD25+, respectively, to non-HIV (+) and HIV antigen (□) within the CD8+ (left panel) and CD4+ (right panel) T cell subsets. Significant and high correlations obtained for both Non-HIV antigens (CD8+, r = 0.92, p<0.001: CD4+ r = 0.64, p<0.001) and HIV Gag p24 (CD8+, r = 0.90, p<0.001: CD4+ r = 0.71, p<0.001).
Quantification of Env- and Gag-induced Cytokine-mediated T Cell Regulation
In parallel with classical activation cultures, IL-10 and TGF-ß blocked activation was determined as the difference between antigen-stimulated and control samples that received IL-10 and TGF-ß blocking mAbs (Fig. 2A). The magnitude of antigen-induced IL-10 and TGF-ß mediated regulation of T cell activation (RAC) was calculated by the difference in activation between these two culture conditions (Fig. 2B). RAC calculated by CFSEdim correlated with RAC determined by the CD25+HLA-DR+ subsets (Fig. 2C).
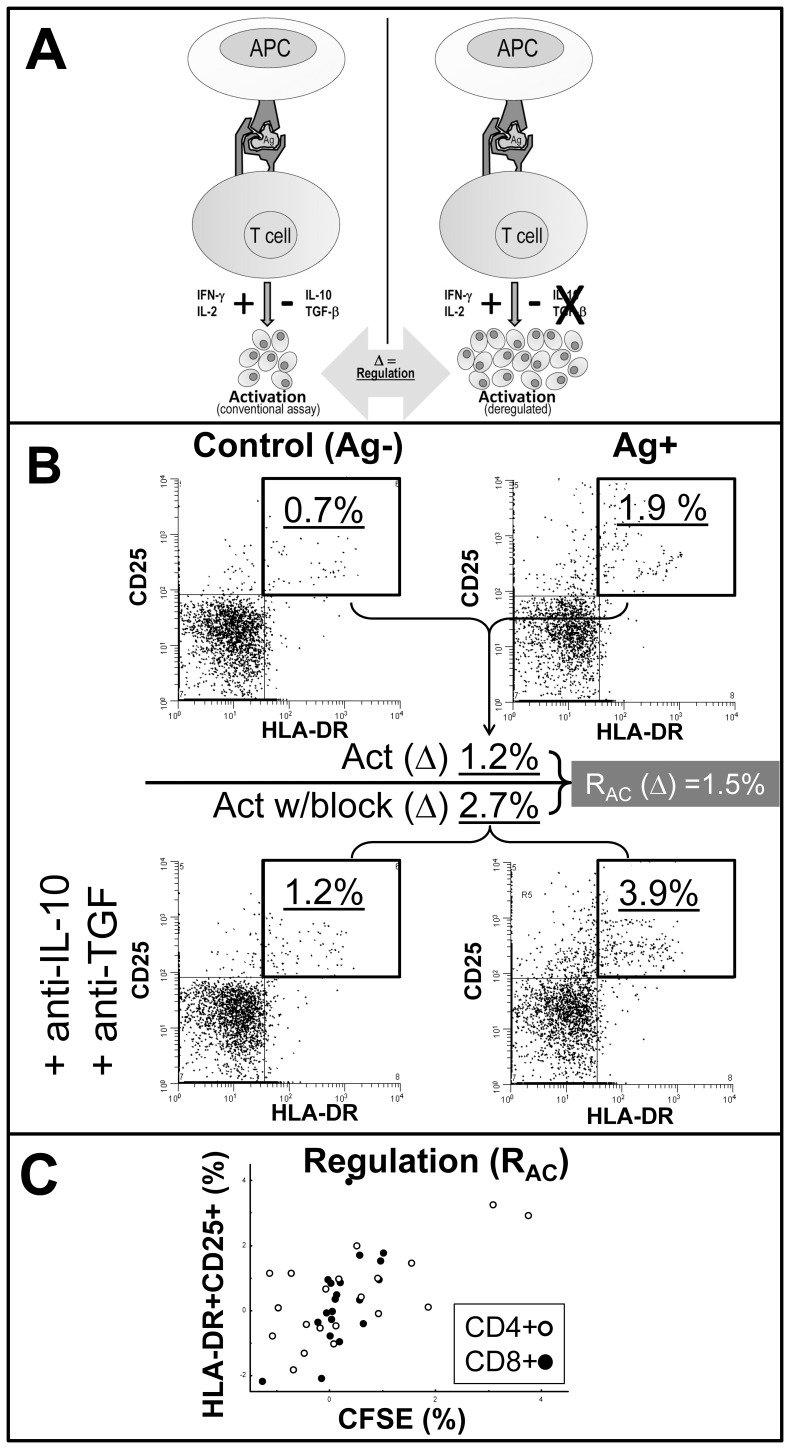
Figure 2. Schematic outline and examples of the T cell regulation assay.
A. Schematic outline of the assay measuring antigen-induced cytokine-mediated induced regulation (RAC) of T cell activation by IL-10 and TGF-ß. Left panel shows a conventional T cell assay where the final activation measurements are regarded as net results of proinflammatory and regulatory signals. Right panel show a possible outcome when blocking T cell regulatory cytokines. T cell regulation (Δ) is here defined as the difference in activation responses to the same antigen between these panels. B. Detailed example calculating classical activation (upper panels) and regulation (calculated from activation in the presence blocking mAbs to IL-10 and TGF, lower panels), all gated for viable CD8+ CD3+ T cells. Activation in both upper and lower panels calculated as the difference (Δ) in CD25+HLA-DR+ fractions between control and antigen-stimulated (Ag+). Note a typical slight increase in background activation (lower left panel). Regulation (RAC) calculated as the difference (Δ) between activation in cytokine-blocked culture and conventional activation culture. C. Scatter plots of regulation calculated in the same cultures by CFSEdim or HLA-DR+CD25+, respectively, for the CD8+ (λ, r = 0.67, p<0.001) and CD4+ (Υ, r = 0.45, p = 0.026) T cell subsets.
LPS Measurement
EDTA plasma obtained concurrently with the isolation of PBMC was separated and snap-frozen at −70°C. LPS was later measured en bloc in thawed plasma with the Limulus Amebocyte Lysate chromogenic assay (Lonza, MD, USA) according to the manufacturer’s instructions with the following modifications: Samples were diluted 10-fold to avoid interference with background colour and preheated to 70°C for 12 minutes prior to analysis to dissolve immune complexes, as previously described [10].
Plasma Levels of Cytokines and Chemokines
Soluble cytokines representing Th1 (TNF-α, INF-γ) and Th2 (IL-4, IL-5, IL-10 and IL-13) profiles were measured in snap-frozen EDTA plasma (see above) using Bio-Plex XMap technology (TX, USA) with a Luminex IS100 instrument (BIO-RAD, CA, USA) and Bio-Plex manager Software v6, according to the instructions by the manufacturer.
Statistics
To not underestimate regulation, antigen-specific activation readouts relative to control cultures were treated as raw data. Non-parametrical statistics were applied throughout the study; Mann-Whitney U- and Kruskal-Wallis test to compare differences between two or more groups, and Spearman Rank for correlation analysis. All continuous variables are presented as medians (interquartile range). The Fisher Exact test was performed to analyse cross-tabulated categorical data. The annual CD4 count loss rates were calculated as previously described [26]. Statistica v7 statistical software (StatSoft Inc., OK, USA) was used for all analysis. A p-value ≤0.05 was regarded as significant.
Results
Cohort Characteristics Including Parameters for Immune Activation
Thirty asymptomatic ART-naïve HIV-infected patients (CD4+ T cell counts, 472; HIV RNA, 37,500 copies/ml, medians) were included to represent a spectrum of HIV-associated immune activation. CD38, microbial translocation (LPS) and HIV RNA correlated (r between 0.44–0.60, p<0.02, detailed data not shown). In keeping with previous observations where CD38 density on CD8+ T cells and on CD8+PD-1+ cells had higher correlation with other progression markers than frequencies of CD38+HLA-DR+CD8+ T cells [8], [25], [26], CD38 density was used to represent chronic immune activation in the following analysis.
T cell Activation by Gag and Env
T cell activation to Gag and Env peptide panels varied between patients and was generally higher for Gag, in keeping with previous observations [30] (Fig. 3A, x-axis). Moreover, Gag and Env activation correlated within both the CD8+ (r = 0.40, p = 0.027) and CD4+ (r = 0.53, p = 0.003) T cell subsets (data not shown).
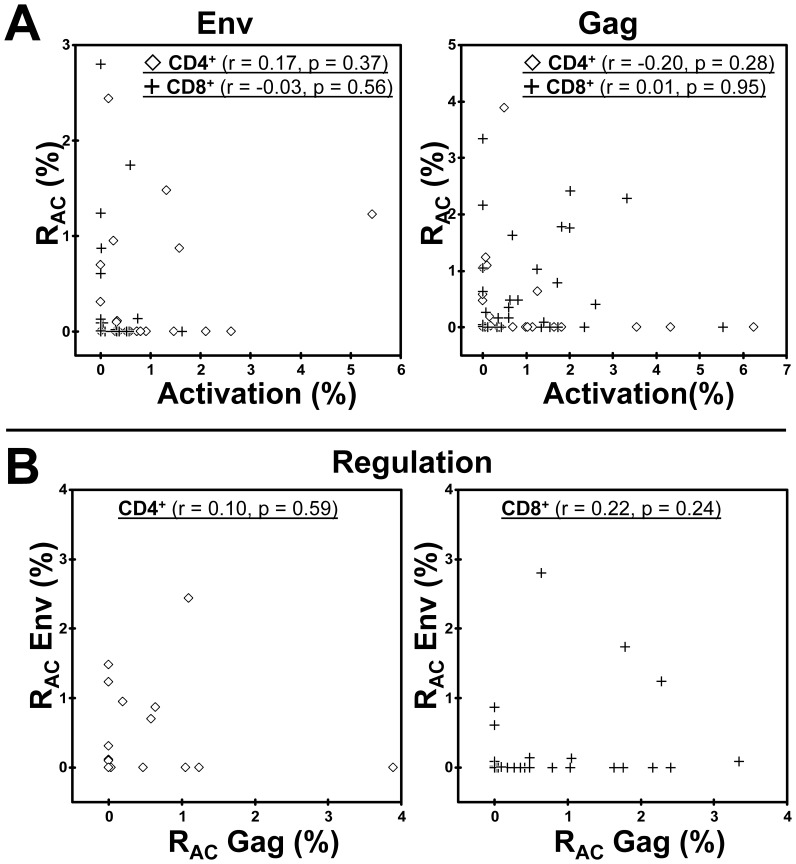
Figure 3. Insignificant relations between T cell activation and RAC induced by Env and Gag peptide panels.
A. Relations between regulation and activation to Env (left panels) and Gag (right panels) within the CD4+ and CD8+ T cell subsets respectively, correlation coefficients indicated. B. Relations between Env- and Gag-induced regulation within the CD4+ (right panel) and the CD8+ (right panel) T cell subsets, respectively, correlation coefficients indicated.
Variable T Cell Regulation (RAC) without Correlation to Activation
A parameter for HIV antigen-specific cytokine-mediated T cell regulation (RAC) was determined by parallel antigen activation cultures and controls in the absence and presence of IL-10 and TGF-ß blocking mAbs. It should be noted that RAC calculated by CFSE correlated significantly with RAC determined by the co-expression of CD25 and HLA-DR (Fig. 2C).
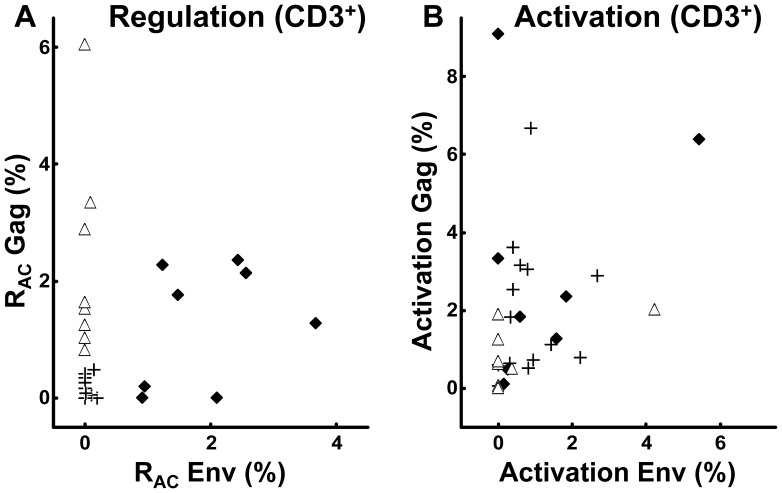
A substantial variability was observed in RAC related to Gag and Env exposure (Fig. 3A, y-axis). No correlations were found between RAC induced by the two HIV antigens (Fig. 3B), in contrast to the corresponding activation. Perhaps more importantly, Gag or Env related RAC and corresponding activation did not correlate (Fig. 3A). Thus, RAC quantified this way could not have been predicted by the conventional activation assay.
Activation and RAC to HIV-antigens in Relation to Progression Markers
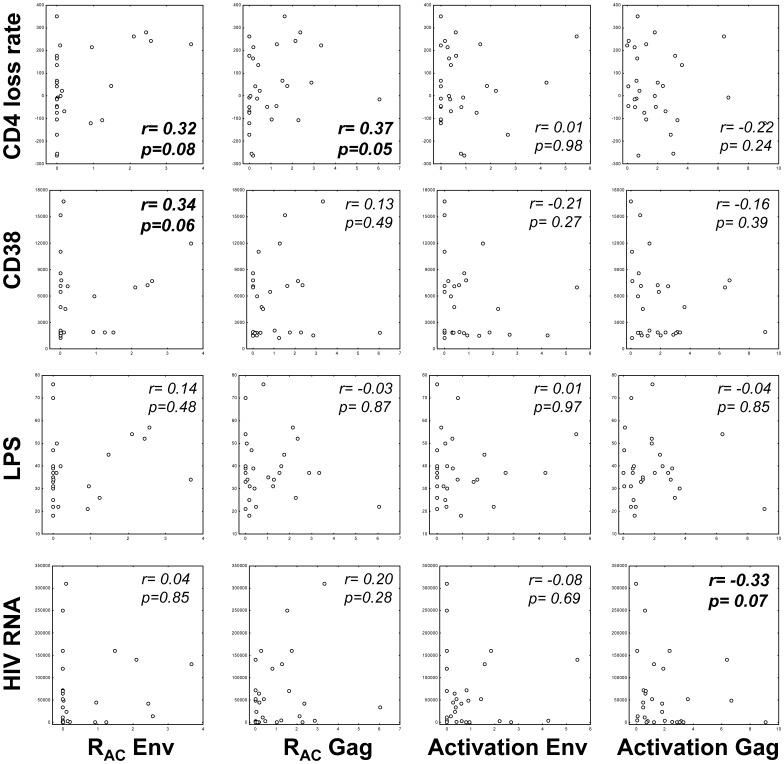
We next explored how RAC was related to markers of chronic HIV activation (CD38 density on CD8+ T cells and PD-1 subsets [8], [26]), microbial translocation (LPS), HIV replication and annual CD4+ T cell loss rates. Significant and unfavourable correlations were revealed between Env related RAC in either T cell subsets and chronic immune activation (CD8+, r = 0.41, p = 0.024) and CD4 loss rates (CD4+, r = 0.39, p = 0.032), whereas Gag-induced T cell activation tended to correlate with HIV RNA (CD8+, r = −0.35, p = 0.060). These heterogeneous relations are depicted in Fig. 4, for simplicity illustrated by overall CD3+ T cell activation and regulation.
Figure 4. Relations between Env- and Gag-induced RAC and activation and markers related to progression of chronic HIV infection.
RAC and corresponding activation (x-axis), for simplicity represented as overall CD3+ estimates (CD4+ plus CD8+ combined) induced by Env and Gag peptide panels, respectively, and in relations to various progression markers (y-axis). Spearman rank r and corresponding p-values indicated, values with p<0.10 bolded.
Clusters of Patients with Low and High HIV Antigen-induced Regulation
One cluster of patients appeared to have low RAC induced by both Gag and Env within the CD4+ and CD8+ subsets (Fig. 3B). The same cluster was seen when we examined RAC for all CD3+ T cells (Fig. 5A). This is in keeping with the notion that IL-10 and TGF-ß inhibit both the CD4+ and CD8+ T cell subsets [23], [33]. This cluster of patients with overall low RAC induced by Gag and Env was defined as Low regulators [n = 14 (47%)] (Fig. 5A) whereas the remaining 53% (n = 16) were termed High regulators. Notably, the magnitude of RAC in suppressing corresponding activation was quite substantial for the High regulator patients, as illustrated by high RAC/Activation-ratios [3.0 (0.8–4.1) for Env and 2.4 (0.8–12.4) for Gag, respectively] (data not shown). Again, conventional activation for CD3+ T cells did not correlate with the corresponding RAC. Thus, High regulators could not have been identified by the activation assay (Fig. 5B).
Figure 5. Relations between total CD3+ T cell activation and RAC induced by Env and Gag peptide panels.
A. Relations between total CD3+ T cell regulation calculated after Env and Gag peptide panel stimulations, respectively. Low regulators (+), Gag regulators (▵) and Pan regulators (⧫) indicated as defined in the text. B. Relations between total CD3+ T cell activation to Env and Gag, respectively, in the same patient groups as in panel A.
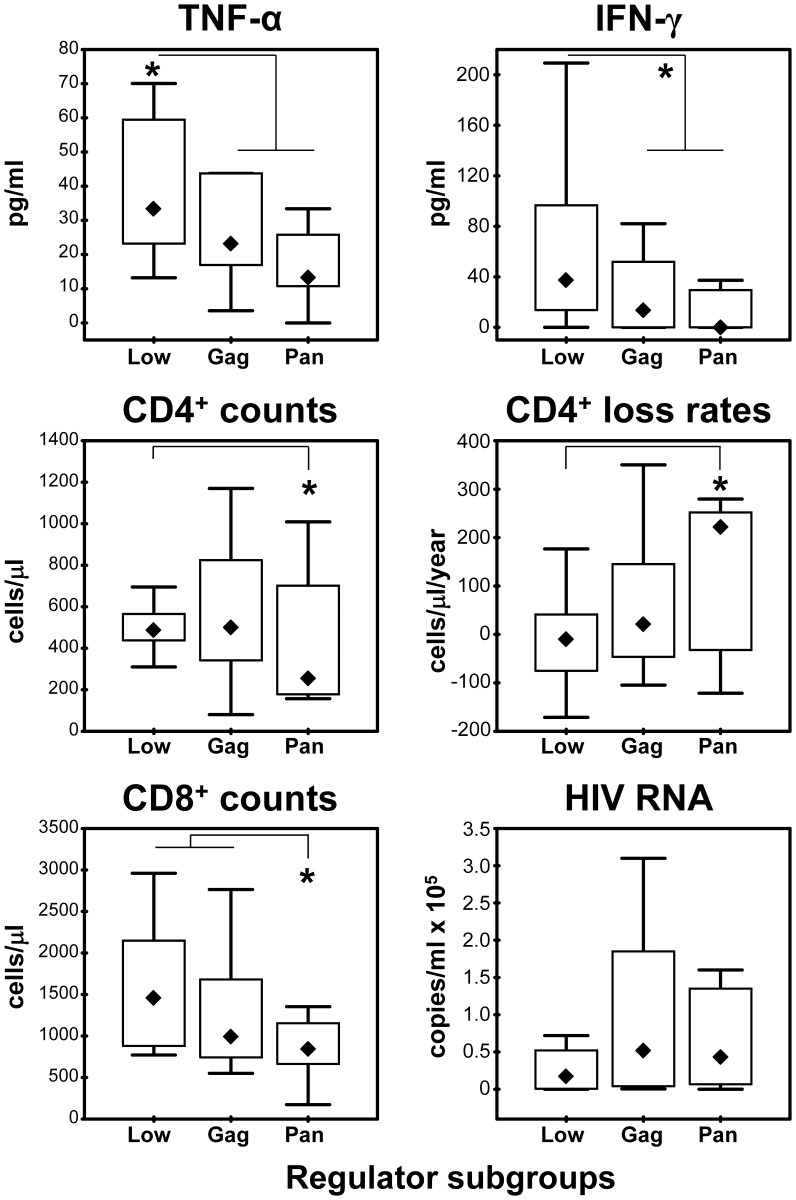
The Low and High regulator patient groups were also compared with respect to clinical parameters, immune activation, LPS and conventional activation. High regulators had lower CD8 counts in blood (p = 0.031) and a trend towards faster CD4 loss rates (p = 0.056) (Table 2). High regulators also had significantly lower levels of plasma Th1 cytokines INF-γ (p = 0.04) and TNF-α (p = 0.04) (Fig. 6), but no differences were found for Th2 cytokines including IL-10 between the two regulation groups.
Table 2. Characteristics of regulator groups.
| Low regulators (n = 14) | High regulators (n = 16) | Low vs. high regulators | |
| Median (IQ range) | Median (IQ range) | p* | |
| Age (years) | 43 (39–49) | 40 (30–52) | 0.755 |
| Time HIV seropositive (months) | 65 (16–100) | 52 (21–68) | 0.510 |
| CD4+ T cell count (×106/l) | 488 (438–565) | 392 (225–825) | 0.262 |
| CD8+ T cell count (×106/l) | 1458 (880–2148) | 938 (663–1261) | 0.031 |
| HIV-RNA in plasma (copies/ml) | 17000 (670–52000) | 43000 (4000–135000) | 0.220 |
| Annual CD4 T cell count loss (cells ×106/l) | −10 (−75–41) | 62 (−46–235) | 0.056 |
| β2-microglobulin in serum (mg/l) | 2.5 (2.1–3.0) | 2.3 (1.5–5.3) | 0.965 |
| CD38 on CD8+ T cells (molecules/cell) | 1894 (1770–7116) | 4271 (1688–11165) | 0.244 |
| CD38 on CD8+CD38+PD-1+ T cells (molecules/cell) | 2541 (1938–8101) | 4946 (1962–13798) | 0.228 |
| LPS (pg/µl) | 70 (57–76) | 70 (59–92) | 0.693 |
Comparisons between patient groups, p<0.05 bolded, p<0.10 italic.
Figure 6. Distributions between regulator subgroups.
Box and whisker plots representing medians, interquartile ranges and overall ranges for cytokines in snap-frozen plasma (upper two panels), CD4 counts and CD4 loss rates (two middle panels) and CD8 counts as well as HIV RNA levels (two lower panels). “Low regulators” (Low) as defined in the text are represented as one group, whereas the “High regulator” patients are split into “Gag regulators” (Gag) and “Pan regulators” (Pan), respectively. Significant differences p<0.05 between groups (Mann-Whitney) indicated (*).
Characterization of Study Patients with High HIV Antigen-induced Regulation
Examining the High regulator patients in more detail, we found that they either had substantial RAC induced by Gag (denoted Gag regulators, n = 8), or by both Gag and Env (Pan regulators, n = 8) (Fig. 5A). Gag regulators appeared more similar to Low regulators in most parameters except that they had less conventional activation to both Gag (CD4+ subset, p = 0.016) and Env (p = 0.025). Pan regulators, on the other hand, had a profile compatible with more accelerated disease, such as higher annual CD4 loss (221 vs −10 cells/year, p = 0.034), lower CD8 counts (median 841 vs 1458 cells/µl, p = 0.014) and possibly lower CD4 counts (median 254 vs 488 cells/µl, p = 0.065) compared with the Low regulator patients (Fig. 6). Thus, one might speculate whether Gag and Pan regulators represent a continuum of an unfavourable regulator phenotype which could not be identified by the classical activation assay. Finally, of the 14 patients who had started ART according to current guidelines within one year post-inclusion, more patients tended to be Pan regulators than belonging to the other subgroups (6 of 8 vs. 8 of 22, p = 0.07).
Discussion
HIV-specific T effector cells are potentially able to control viral replication in HIV infection, but their responses are critically weakened by the initial loss of HIV-specific CD4+ T cells, viral immune escape, and T cell exhaustion driven by immune activation [5], [34]. An additional counteracting factor might be the regulation of effective HIV specific T effector cells. We here assessed a functional quantitative parameter for T cell regulation (RAC) which we think could be relevant when evaluating HIV infected patients and developing therapeutic vaccines. Therapeutic vaccines might play an essential role in a future cure for HIV by inducing effective T cell responses against re-activated, latently infected cells [34]. Theoretically, pre-existing or induced regulation can evoke T cell anergy and thus hamper the effects of therapeutic vaccination in some patients. This notion was supported by our recent observation where changes in RAC explained variable and in some cases negative responses to therapeutic HIV vaccine boosters [25].
To our knowledge, this is the first attempt to determine RAC or similar quantitative parameters for HIV antigen-specific regulation in chronically infected treatment-naïve patients. The study was motivated by our expectation that RAC would provide additional prognostic information. We found considerable variability in RAC not only between individual patients, but also between the two tested HIV antigens. Thus, our data suggest that at least in some patients, RAC does not reflect “global” regulation of HIV antigens. RAC was in some cases substantial, exceeding activation more than ten-fold. Moreover, RAC did not relate to corresponding conventional activation readouts, showing that it provided additional otherwise hidden information.
This exploratory approach to characterize a parameter apparently reflected at least some aspects of cytokine-mediated regulatory “capacity” in the individual patient. However, although our data suggest that RAC can differentiate HIV-infected patients in a new way and may reflect processes that are related to progression of HIV, our choices of assay read-out and culture conditions needs to be commented: Several assays are frequently used to assess HIV-specific T cell activation and function. For example, polyfunctional T cells in 6 to 18 h cultures have been shown to coincide with control of viral replication [32]. However, we did not prioritize this assay due to shortage of cells from this clinically well-defined cohort, and 6 day cultures were chosen for several reasons: First, we expected a priori that antigen-related regulation is a slower, secondary response, to primary activation. This assumption is in keeping with the observation that stimulation of resting Treg reach maximal expression of FoxP3 34–44 h after simulation [35]. Second, it is still not clear whether early polyfunctionality actually persists over time, including early markers for proliferation such as Ki-67 [32]. Third, a fundamental element of effector lymphocytes is the ability to proliferate, indicating responsiveness to IL-2 (via its receptor CD25), whereas proinflammatory cytokines such as IFN-γ upregulate HLA class II (including DR) on T cells. Moreover, HIV-specific proliferative T cell responses have been long known to associate with slow progression [36]. Our assay use changes in CD25+HLA-DR+ as readout, parameters that both reflect activation and proliferation, the latter illustrated in Fig. 1A. Nevertheless, we appreciate that our approach only reflect one out of several ways by which classical “net” T cell responses can be estimated in vitro. Indeed, other major regulatory pathways may influence overall activation. Finally, in-depth interpretation and characterization of our assay can certainly be extended, such as to address whether the “gain” in activation by blockade of regulatory pathways also provides an increase in effector cell functions, such as cytotoxic capacity or polyfunctionality.
A possible clinical relevance of this new exploratory parameter was suggested by the significant correlations between RAC and the classical prognostic markers CD38 and CD4 loss rates. These correlations were not found for the activation results (Fig. 4). Even if the study included only a limited number of cases, we were still able to cover a wide spectrum of chronic immune activation. Gag-specific T cell responses correlated negatively with concurrent HIV RNA levels, an association also found in other and larger study cohorts [37], [38]. It should be noted that our group favours bead-calibrated measures for CD38 density rather than the more simple and conventional measure for HIV-associated chronic immune activation, namely % CD38+HLA-DR+. We have previously shown that CD38 density is even better related to other progression markers [8], [25], [26].
Post-hoc we observed clusters of patients having either particularly low (Low regulators) or high (High regulators) regulation (i.e. RAC). The High regulators seemed to have more rapid HIV progression, in keeping with our expectation. In contrast, Low regulators had more favourable clinical characteristics in terms of slower CD4 loss rates and higher CD8 counts [39]. The levels of the proinflammatory cytokines TNF-α and IFN-γ were also higher in Low regulators. This has previously been interpreted as a sign of unfavourable immune activation in patients with lower CD4 counts [40], [41]. From our data, derived from patients with higher CD4 counts, one might conversely speculate whether higher TNF-α and IFN-γ levels rather reflect a beneficial type of immune activation.
RAC or similar quantitative parameters for HIV antigen-specific regulation should be further explored in larger cohorts. This may help to better understand the complex interplay between regulation and activation, to select patients for immune therapy studies, and to determine the prognostic significance of regulation. Future studies should also explore the individual contribution of IL-10 and TGF-ß along with other regulating mechanisms such as CTLA-4 and PD-1. This was hampered by a scarcity of patients and samples in this study. Both a broader range of HIV antigens and even non-HIV antigens should be tested. In this study Gag was selected based on the relation between Gag-specific T cell responses to control viral replication [37], [38] and Env as a relevant antigen for HIV vaccines.
Conclusions
In summary, this study on regulation of Gag- and Env-specific T cell activation by IL-10 and TGF-ß (RAC) in chronic HIV infection revealed heterogeneous levels of regulation between both patients and HIV antigens. The magnitude of RAC was substantial in some individuals and RAC could not be predicted by the corresponding, classical antigen-specific activation parameters. High RAC seemed clinically unfavourable, particularly when induced by Env peptides. Thus, assessments of regulation deserve further in-depth exploration and extension to larger cohorts.
Acknowledgments
We particularly thank all participants and the invaluable technical assistance from Hans Christian Aass, Malin Holm and Mette Sannes as well as the contribution of peptide antigen panels from the NIH AIDS Research and Reference Reagent Program.
Funding Statement
The study was supported by the Research Council of Norway (RCN) in the GLOBVAC program (http://www.forskningsradet.no/prognett-globvac/Home_page/1224697869238), RCN grant no. 179389. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Hunt PW (2012) HIV and inflammation: mechanisms and consequences. Curr HIV/AIDS Rep 9: 139–147. [DOI] [PubMed] [Google Scholar]
- 2. Moir S, Chun TW, Fauci AS (2011) Pathogenic mechanisms of HIV disease. Annu Rev Pathol 6: 223–248. [DOI] [PubMed] [Google Scholar]
- 3. Appay V, Sauce D (2008) Immune activation and inflammation in HIV-1 infection: causes and consequences. J Pathol 214: 231–241. [DOI] [PubMed] [Google Scholar]
- 4. Betts MR, Nason MC, West SM, De Rosa SC, Migueles SA, et al. (2006) HIV nonprogressors preferentially maintain highly functional HIV-specific CD8+ T cells. Blood 107: 4781–4789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McDermott AB, Koup RA (2012) CD8(+) T cells in preventing HIV infection and disease. AIDS 26: 1281–1292. [DOI] [PubMed] [Google Scholar]
- 6. Giorgi JV, Hultin LE, McKeating JA, Johnson TD, Owens B, et al. (1999) Shorter survival in advanced human immunodeficiency virus type 1 infection is more closely associated with T lymphocyte activation than with plasma virus burden or virus chemokine coreceptor usage. J Infect Dis 179: 859–870. [DOI] [PubMed] [Google Scholar]
- 7. Deeks SG, Kitchen CM, Liu L, Guo H, Gascon R, et al. (2004) Immune activation set point during early HIV infection predicts subsequent CD4+ T-cell changes independent of viral load. Blood 104: 942–947. [DOI] [PubMed] [Google Scholar]
- 8. Holm M, Pettersen FO, Kvale D (2008) PD-1 predicts CD4 loss rate in chronic HIV-1 infection better than HIV RNA and CD38 but not in cryopreserved samples. Curr HIV Res 6: 49–58. [DOI] [PubMed] [Google Scholar]
- 9. Brenchley JM, Price DA, Schacker TW, Asher TE, Silvestri G, et al. (2006) Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med 12: 1365–1371. [DOI] [PubMed] [Google Scholar]
- 10. Trøseid M, Nowak P, Nystrom J, Lindkvist A, Abdurahman S, et al. (2010) Elevated plasma levels of lipopolysaccharide and high mobility group box-1 protein are associated with high viral load in HIV-1 infection: reduction by 2-year antiretroviral therapy. AIDS 24: 1733–1737. [DOI] [PubMed] [Google Scholar]
- 11. Lane HC, Masur H, Edgar LC, Whalen G, Rook AH, et al. (1983) Abnormalities of B-cell activation and immunoregulation in patients with the acquired immunodeficiency syndrome. N Engl J Med 309: 453–458. [DOI] [PubMed] [Google Scholar]
- 12. Hazenberg MD, Stuart JW, Otto SA, Borleffs JC, Boucher CA, et al. (2000) T-cell division in human immunodeficiency virus (HIV)-1 infection is mainly due to immune activation: a longitudinal analysis in patients before and during highly active antiretroviral therapy (HAART). Blood 95: 249–255. [PubMed] [Google Scholar]
- 13. Sachsenberg N, Perelson AS, Yerly S, Schockmel GA, Leduc D, et al. (1998) Turnover of CD4+ and CD8+ T lymphocytes in HIV-1 infection as measured by Ki-67 antigen. J Exp Med 187: 1295–1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hellerstein M, Hanley MB, Cesar D, Siler S, Papageorgopoulos C, et al. (1999) Directly measured kinetics of circulating T lymphocytes in normal and HIV-1-infected humans. Nat Med 5: 83–89. [DOI] [PubMed] [Google Scholar]
- 15. Jin HT, Jeong YH, Park HJ, Ha SJ (2011) Mechanism of T cell exhaustion in a chronic environment. BMB Rep 44: 217–231. [DOI] [PubMed] [Google Scholar]
- 16. Fazekas de St GB, Landay AL (2008) Regulatory T cells in HIV infection: pathogenic or protective participants in the immune response? AIDS 22: 671–683. [DOI] [PubMed] [Google Scholar]
- 17. Hunt PW, Landay AL, Sinclair E, Martinson JA, Hatano H, et al. (2011) A low T regulatory cell response may contribute to both viral control and generalized immune activation in HIV controllers. PLoS One 6(1): e15924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kaufmann DE, Kavanagh DG, Pereyra F, Zaunders JJ, Mackey EW, et al. (2007) Upregulation of CTLA-4 by HIV-specific CD4+ T cells correlates with disease progression and defines a reversible immune dysfunction. Nat Immunol 8: 1246–1254. [DOI] [PubMed] [Google Scholar]
- 19. Keir ME, Butte MJ, Freeman GJ, Sharpe AH (2008) PD-1 and its ligands in tolerance and immunity. Annu Rev Immunol 26: 677–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Day CL, Kaufmann DE, Kiepiela P, Brown JA, Moodley ES, et al. (2006) PD-1 expression on HIV-specific T cells is associated with T-cell exhaustion and disease progression. Nature 443: 350–354. [DOI] [PubMed] [Google Scholar]
- 21. Letterio JJ, Roberts AB (1998) Regulation of immune responses by TGF-beta. Annu Rev Immunol 16: 137–161. [DOI] [PubMed] [Google Scholar]
- 22. Couper KN, Blount DG, Riley EM (2008) IL-10: the master regulator of immunity to infection. J Immunol 180: 5771–5777. [DOI] [PubMed] [Google Scholar]
- 23. Brockman MA, Kwon DS, Tighe DP, Pavlik DF, Rosato PC, et al. (2009) IL-10 is up-regulated in multiple cell types during viremic HIV infection and reversibly inhibits virus-specific T cells. Blood 114: 346–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Li MO, Flavell RA (2008) TGF-beta: a master of all T cell trades. Cell 134: 392–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lind A, Brekke K, Sommerfelt M, Holmberg JO, Aass HC, et al.. (2013) Boosters of a therapeutic HIV-1 vaccine induce divergent T cell responses related to regulatory mechanisms. Vaccine (in press). doi:10.1016/j.vaccine.2013.07.037. PMID: 23906886. [DOI] [PubMed]
- 26. Pettersen FO, Torheim EA, Dahm AE, Aaberge IS, Lind A, et al. (2011) An exploratory trial of cyclooxygenase type 2 inhibitor in HIV-1 infection: downregulated immune activation and improved T cell-dependent vaccine responses. J Virol 85: 6557–6566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Reddy M, Eirikis E, Davis C, Davis HM, Prabhakar U (2004) Comparative analysis of lymphocyte activation marker expression and cytokine secretion profile in stimulated human peripheral blood mononuclear cell cultures: an in vitro model to monitor cellular immune function. J Immunol Methods 293: 127–142. [DOI] [PubMed] [Google Scholar]
- 28. Lyons AB (2000) Analysing cell division in vivo and in vitro using flow cytometric measurement of CFSE dye dilution. J Immunol Methods 243: 147–154. [DOI] [PubMed] [Google Scholar]
- 29. Lind A, Sommerfelt M, Holmberg JO, Baksaas I, Sorensen B, et al. (2012) Intradermal vaccination of HIV-infected patients with short HIV Gag p24-like peptides induces CD4+ and CD8+ T cell responses lasting more than seven years. Scand J Infect Dis 44: 566–572. [DOI] [PubMed] [Google Scholar]
- 30. Pettersen FO, Tasken K, Kvale D (2010) Combined Env- and Gag-specific T cell responses in relation to programmed death-1 receptor and CD4+ T cell loss rates in human immunodeficiency virus-1 infection. Clin Exp Immunol 161: 315–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kran AM, Sorensen B, Nyhus J, Sommerfelt MA, Baksaas I, et al. (2004) HLA- and dose-dependent immunogenicity of a peptide-based HIV-1 immunotherapy candidate (Vacc-4x). AIDS 18: 1875–1883. [DOI] [PubMed] [Google Scholar]
- 32. Chattopadhyay PK, Roederer M (2010) Good cell, bad cell: flow cytometry reveals T-cell subsets important in HIV disease. Cytometry A 77: 614–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. McKarns SC, Schwartz RH (2005) Distinct effects of TGF-beta 1 on CD4+ and CD8+ T cell survival, division, and IL-2 production: a role for T cell intrinsic Smad3. J Immunol 174: 2071–2083. [DOI] [PubMed] [Google Scholar]
- 34. Pantaleo G, Levy Y (2013) Vaccine and immunotherapeutic interventions. Curr Opin HIV AIDS 8: 236–242. [DOI] [PubMed] [Google Scholar]
- 35. Kalland M, Oberprieler NG, Vang T, Taskén K, Torgersen KM (2011) T cell-signaling network analysis revieals distinct differences between CD28 and CD2 costimulation responses in various subsets and in the MAPK pathway between resting and activated regulatory T cells. J Immunol 187: 5233–5245. [DOI] [PubMed] [Google Scholar]
- 36. Lieberman J, Shankar P, Manjunath N, Anderson J (2001) Dressed to kill? A review of why antiviral CD8 T lymphocytes fail to prevent progressive immunodeficiency in HIV-1 infection. Blood 98: 1667–1677. [DOI] [PubMed] [Google Scholar]
- 37. Kiepiela P, Ngumbela K, Thobakgale C, Ramduth D, Honeyborne I, et al. (2007) CD8+ T-cell responses to different HIV proteins have discordant associations with viral load. Nat Med 13: 46–53. [DOI] [PubMed] [Google Scholar]
- 38. Zuniga R, Lucchetti A, Galvan P, Sanchez S, Sanchez C, et al. (2006) Relative Dominance of Gag p24-Specific Cytotoxic T Lymphocytes Is Associated with Human Immunodeficiency Virus Control. J Virol 80: 3122–3125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kvale D, Aukrust P, Osnes K, Muller F, Froland SS (1999) CD4+ and CD8+ lymphocytes and HIV RNA in HIV infection: high baseline counts and in particular rapid decrease of CD8+ lymphocytes predict AIDS. AIDS 13: 195–201. [DOI] [PubMed] [Google Scholar]
- 40. von Sydow M, Sönnerborg A, Gaines H, Strannegard O (1991) Interferon-alpha and tumor necrosis factor-alpha in serum of patients in various stages of HIV-1 infection. AIDS Res Hum Retroviruses 7: 375–380. [DOI] [PubMed] [Google Scholar]
- 41. Thea DM, Porat R, Nagimbi K, Baangi M, St Louis ME, et al. (1996) Plasma cytokines, cytokine antagonists, and disease progression in African women infected with HIV-1. Ann Intern Med 124: 757–762. [DOI] [PubMed] [Google Scholar]