Abstract
Objective
Hashimoto encephalopathy (HE) is known as a steroid- responsive encephalopathy associated with autoimmune thyroiditis or nonvascular inflammation-related autoimmune meningoencephalitis. The average age of onset of HE is approximately 50 years; and it is more common in women. The onset of HE may be acute or subacute. The course of most HE cases is relapsing and remitting, which is similar to that of vasculitis and stroke.
Methods
In this article, we present a previously healthy 32 years old;veterinarian male with palatal myoclonus, as a rare presentation of this disorder, and review the neurologic aspects of hashimoto encephalitis.
Results
The clinical presentation of HE is characterized by progressive cognitive decline tremor, transient aphasia, seizures, abnormal gait, sleep disorder and stroke-like episodes.
Myoclonus, either generalized or multifocal, and tremor, often of the bilateral upper extremities, is the most frequently observed involuntary movements in HE.
Conclusion
The rapidly progressive cognitive dysfunction and encephalopathies observed.
Keywords: Hashimoto encephalopathy, palatal myoclonus, abnormal movement
The differential diagnosis for encephalopathy is wide. Once infectious causes are excluded, an autoimmune or inflammatory process may be suspected.
In this case report, a patient is presented with seizure, encephalopathy, palatal myorrhythmia and myoclonus with final diagnosis of hashimoto encephalopathy.
Case Description
A previously healthy 32 years old; veterinarian male, referred to the emergency department complaining about 2 episodes of generalized tonic clonic seizure within the past 24 hours.
According to his wife, he had depressed mood and psychomotor slowing during the past 3 weeks. He also had episodes of confusion, agitation, visual hallucinations, decrement of interpersonal relationship, generalized purities and flushing.
Three days before admission, he had abnormal movements of the palate and tongue.
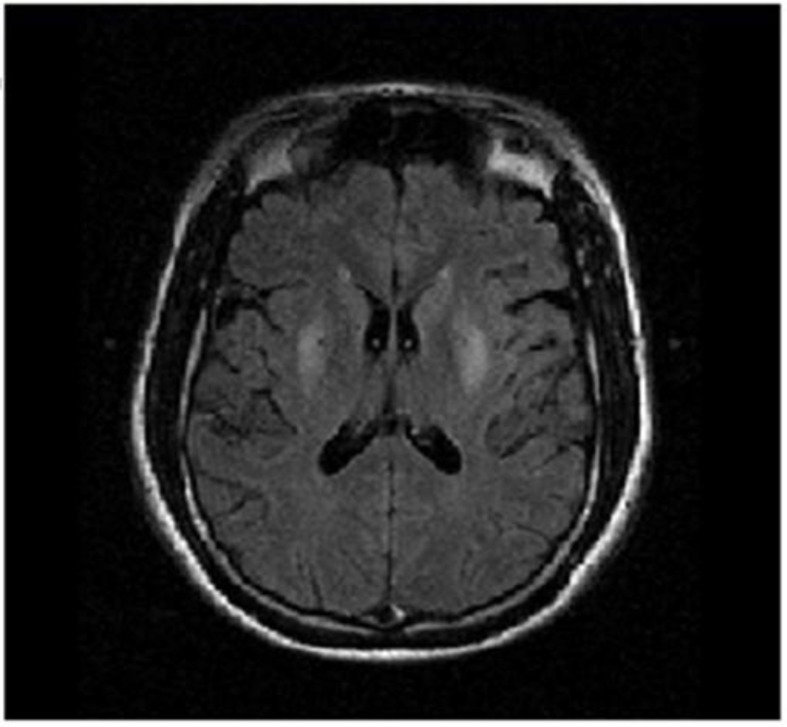
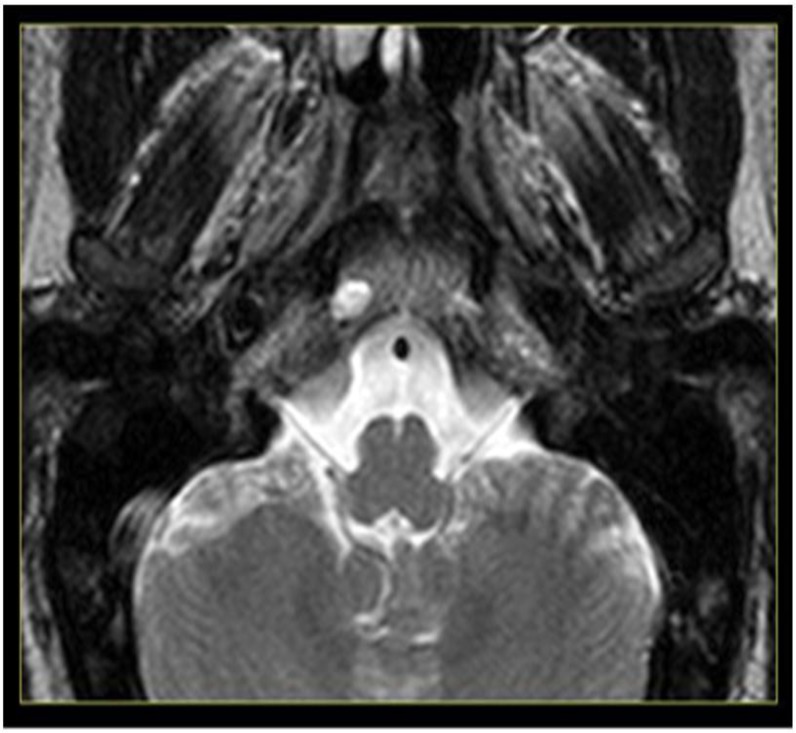
On physical examination, the patient was ill and lethargic. There was a low grade fever (Temp: 37.4 Auxiliary), but other vital signs were normal. His neck was supple. On general examination, there were itching excoriations on his skin, but other systemic examinations were normal. Neurologic examination was normal, apart from mild confusion and myorrhythmic movements of tongue and soft palate. The patients MRI showed abnormal symmetric hyper signality in both caudate nuclei and putamens on T2 and FLAIR. (Fig. 1) There was no abnormal signal in medulla (inf.olive nucleus). (Fig. 2)
Figure 1.
FLAIR sequence MRI were shown symmetric abnormal hypersignality in bilateral caudate and putamen
Figure 2.
T2 MRI of Medulla shows no abnormality in inferior olive
The CSF was clear with normal level of protein and glucose. There were 30 red blood cells, 20 lymphocytes and no polymorphonuclear in CSF. PCR for herpes simplex virus and mycoplasma were negative. The EEG showed intermittent delta and theta activity. Routine blood counts, renal function tests and glucose were within normal limits. Erythrocyte sedimentation rate (ESR) and C-reactive protein were normal. Liver function tests were elevated. Antinuclear antibodies, anti-ds-DNA, anti SS-A, anti SS-B, lupus anticoagulant, anti phospholipid Ab and RF were normal. The human immunodeficiency virus antibody was negative. Chest radiograph and ultrasonographic scan of the abdomen did not reveal any tumor. Thyroid function tests were within normal limits, but the thyroid thyroglobulin antibody (TGHA) titer was 120 IU/mL (normal < 22 IU/ml) and the thyroid peroxidase antibody (Anti-TPO) titer was 356U/mL (normal < 60 IU/ml).
A diagnosis of HE was made, and the patient was treated with oral prednisolone 1 mg/kg/d, levothyroxin and anticonvulsants. Before starting treatment with prednisolone, the patient had 3-4 episodes of simple focal seizures per day which were not controlled with antiepileptic drugs. Less than 24 hours after the initiation of prednisolone, the palatal myorrhythmic movements, itching, and flushing were subsided and focal seizures never repeated. We did not do needle biopsy of thyroid gland. On the follow-up, at days 10 and 40, the patient had no seizures and the palatal myorrhythmic movements disappeared; and EEG was normal at 40th. The Anti- TPO level was decreased to 73 IU/ml after 6 months.
Discussion
As our findings, we excluded our differential diagnoses such as CNS infection, acute disseminated encephalomyelitis, primary hypoxic injury, prolonged hypoglycemia, degenerative diseases, toxic encephalopathies and Lymphoma. Also, we confirmed our diagnosis, Hashimoto encephalopathy, with elevated serum levels of Anti-TPO and TGHA and the response of the patient to our treatment.
HE is known as steroid-responsive encephalopathy associated with autoimmune thyroiditis (1–3).
Brain et al. first reported this disorder in 1966 (4). The first set of criteria for the diagnosis of HE was published by Peschen-Rosin et al. in 1999 (5).
These criteria encompassed unexplained occurrence of relapsing myoclonus, generalized seizures, psychiatric disorders or focal neurological deficits and conditions among which are: abnormal EEG, elevated thyroid antibodies, elevated CSF protein, excellent response to steroids and unrevealing cerebral MRI.
The average age of onset, is approximately 50 years (range, 9 to 84 y), and HE is more common in women.(2, 6) The onset of HE may be acute or subacute. The course of most HE cases is relapsing and remitting, which is similar to that of vasculitis and stroke (1–3, 7).
The clinical presentation of HE is characterized by progressive cognitive decline, behavioral change, tremor, transient aphasia, seizures, abnormal gait, sleep disorder, stroke-like episodes, generalized hyper- reflexia and other signs of pyramidal tract involvement, psychosis (visual hallucinations and paranoid delusions) (1–3).
Myoclonus and tremor, often of the bilateral upper extremities and palatal myorrhytmia, are the most frequently observed involuntary movements in HE (8). Opsoclonus and generalized chorea have also been reported in isolated patients (9).
Our case illustrates the importance of considering rare but treatable causes of encephalopathy in a patient presenting with subacute cognitive decline, seizure and palatal myorrhythmia.
The role of antithyroid antibodies remains unclear. However, a recent report has shown that they are capable of binding cerebellar astrocytes suggesting a pathogenic role.
Almost all the patients presented with an abnormal EEG. EEGs typically show nonspecific abnormalities with slowing of background activity. focal spikes, sharp waves and transient epileptic activity may be seen (9).
Approximately 50% of cases with HE show brain- imaging abnormalities; cerebral atrophy is the most common alteration. Diffuse abnormalities in white matter and meningeal enhancement or nonspecific T2 signal abnormalities in subcortical white matter have been reported (1, 2).
As HE usually responds to corticosteroid therapy well, corticosteroids are the preferred drugs for its treatment, whereas other immunosuppressants have also been reported to treat HE successfully (6, 10).
Most patients have a good prognosis unless there is a delay in diagnosis and treatment.
We suggest that both thyroid function and thyroid antibody assessment be included in the assessment of patients with rapidly progressive cognitive dysfunction and encephalopathies.
References
- 1.Chong JY, Rowland LP, Utiger RD. Hashimoto encephalopathy: syndrome or myth? Arch Neurol. 2003;60:164–71. doi: 10.1001/archneur.60.2.164. [DOI] [PubMed] [Google Scholar]
- 2.Marshall GA, Doyle JJ. Long-term treatment of Hashimoto's encephalopathy. J Neuropsychiatry Clin Neurosci. 2006;18:14–20. doi: 10.1176/jnp.18.1.14. [DOI] [PubMed] [Google Scholar]
- 3.Castillo P, Woodruff B, Caselli R, Vernino S, Lucchinetti C, Swanson J, et al. Steroid- Responsive Encephalopathy Associated with Autoimmune Thyroiditis. Arch Neurol. 2006;63:197–202. doi: 10.1001/archneur.63.2.197. [DOI] [PubMed] [Google Scholar]
- 4.Ferracci F, Carnevale A. The neurological disorder associated with thyroid autoimmunity. J Neurol. 2006;253:975–84. doi: 10.1007/s00415-006-0170-7. [DOI] [PubMed] [Google Scholar]
- 5.Peschen-Rosin R, Schabet M, Dichgans J. Manifestation of Hashimoto's Encephalopathy Years before Onset of Thyroid Disease. Eur Neurol. 1999;41:79–84. doi: 10.1159/000008007. [DOI] [PubMed] [Google Scholar]
- 6.Katoh N, Yoshida T, Shimojima Y, Gono T, Matsuda M, Yoneda M, et al. An 85-year-old case with Hashimoto's encephalopathy, showing spontaneous complete remission. Intern. 2007;46:1613–6. doi: 10.2169/internalmedicine.46.0266. [DOI] [PubMed] [Google Scholar]
- 7.Brain L, Jellinek EH, Ball K. Hashimoto's Disease and Encephalopathy. Lancet. 1966;2:512–514. doi: 10.1016/s0140-6736(66)92876-5. [DOI] [PubMed] [Google Scholar]
- 8.Erickson JC, Carrasco H, Grimes JB, Jabbari B, Cannard KR. Palatal tremor and myorhythmia in Hashimoto's encephalopathy. Neurology. 2002;58:504–505. doi: 10.1212/wnl.58.3.504. [DOI] [PubMed] [Google Scholar]
- 9.Ryan SA, Kennedy C, Harrington HJ. Steroid- Responsive Encephalopathy Associated with Autoimmune Thyroiditis Presenting as Confusion, Dysphasia, and Myoclonus. Case reports in medicine. 2012;2012:782127. doi: 10.1155/2012/782127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zimmermann P, Stranzinger E. Steroid- Responsive Encephalopathy Associated with Hashimoto Thyroiditis. Pediatr Radiol. 2012;42:891–893. doi: 10.1007/s00247-011-2309-7. [DOI] [PubMed] [Google Scholar]