Abstract
Background:
Not recognising a symptom as suspicious is a common reason given by cancer patients for delayed help-seeking; but inevitably this is retrospective. We therefore investigated associations between recognition of warning signs for breast, colorectal and lung cancer and anticipated time to help-seeking for symptoms of each cancer.
Methods:
Computer-assisted telephone interviews were conducted with a population-representative sample (N=6965) of UK adults age ⩾50 years, using the Awareness and Beliefs about Cancer scale. Anticipated time to help-seeking for persistent cough, rectal bleeding and breast changes was categorised as >2 vs ⩽2 weeks. Recognition of persistent cough, unexplained bleeding and unexplained lump as cancer warning signs was assessed (yes/no). Associations between recognition and help-seeking were examined for each symptom controlling for demographics and perceived ease of health-care access.
Results:
For each symptom, the odds of waiting for >2 weeks were significantly increased in those who did not recognise the related warning sign: breast changes: OR=2.45, 95% CI 1.47–4.08; rectal bleeding: OR=1.77, 1.36–2.30; persistent cough: OR=1.30, 1.17–1.46, independent of demographics and health-care access.
Conclusion:
Recognition of warning signs was associated with anticipating faster help-seeking for potential symptoms of cancer. Strategies to improve recognition are likely to facilitate earlier diagnosis.
Keywords: symptom recognition, warning signs, anticipated delay, help-seeking, awareness
Evidence that cancer outcomes are better with earlier stage at diagnosis makes minimising delays across the diagnostic pathway a priority in cancer control (Allgar and Neal, 2005; Olesen et al, 2009; Richards, 2009). Delays accumulate from a range of health professional and health system factors (Roetzheim et al, 1999; Macleod et al, 2009; Singh et al, 2010), but there is particular interest in how the public's recognition of cancer warning signs contributes to their decisions to seek medical help.
Many early cancer symptoms (e.g. change in the appearance of a mole, post-menopausal bleeding) do not in themselves cause pain or interfere with functioning; consequently they may not trigger help-seeking unless they are recognised as warning signs of cancer. Not recognising a symptom as suspicious is one of the commonest reasons given by cancer patients for delayed help-seeking (Chapple et al, 2004; Smith et al, 2005), and there is evidence of longer delay with ambiguous rather than classic (e.g. lump) symptoms (Macleod et al, 2009). Systematic reviews have concluded that failure to recognise early warning signs is a key contributor to delayed presentation in clinical populations (Ramirez et al, 1999; Macdonald et al, 2006; Mitchell et al, 2008).
The results of these clinical studies have highlighted the need for research into awareness of early warning signs of cancer in the general population. Several surveys have identified low symptom awareness in general population samples (Nichols et al, 1996; Grunfeld et al, 2002; McCaffery et al, 2003; Lockwood-Rayermann et al, 2009; Robb et al, 2009). There is also evidence that groups from lower socioeconomic status (SES) and ethnic minority background have lower awareness (Yu et al, 2001; Waller et al, 2009; Forbes et al, 2011); the same groups who tend to have cancer diagnosed at a later stage (Palmer and Schneider, 2005; Woods et al, 2006; Cuthbertson et al, 2009). Just one study has tested the association between awareness and delay in a non-clinical sample. Using data from a population-based survey in the UK, there was a significant negative association between the total number of cancer warning signs recognised from a list of nine (Stubbings et al, 2009; CR-UK, 2012a, 2012b), and the number of symptoms (out of the same list of nine) for which respondents said they would delay more than two weeks before seeking medical advice (Robb et al, 2009). However, given that recognition and help-seeking vary greatly among warning signs and symptoms (Macleod et al, 2009; Robb et al, 2009), the use of aggregate scores for awareness (total number of signs) and help-seeking (total number of symptoms with anticipated delay >2 weeks) may underestimate the strength of the association.
The present study therefore used data from a population-based sample of UK adults to test the hypothesis that anticipated time to help-seeking for potential early symptoms of three common cancers (lung, colorectal, and breast) would be associated with recognition of the warning sign associated with each cancer type. Tracking actual help-seeking for real symptoms would require unfeasibly large samples and study duration, so we therefore used a hypothetical question (how soon would you seek medical help with ….) as a proxy indicator of delay.
Materials and methods
We used data from a survey carried out as part of the International Cancer Benchmarking Partnership (ICBP) which was set up to investigate the causes of international differences in cancer outcomes (CR-UK, 2010). Module 2 of the ICBP assessed awareness of cancer warning signs and anticipated help-seeking for symptoms using computer-assisted telephone interviews with adults age ⩾50 years in six countries in 2011 (CR-UK, 2010; Forbes et al, 2013). For the present analyses, we used data from respondents in three UK nations (England, Wales and Northern Ireland). Random probability sampling was used to achieve population-representative samples of at least 2000 from each nation using electronic telephone directories as sampling frames. The last two digits from each telephone number were substituted with randomly generated digits, to include numbers that were not publicly available. Households were eligible if one or more person was aged 50 or over and spoke English. Where more than one person was eligible, an individual was randomly chosen using the ‘Rizzo' method (Rizzo et al, 2004).
Awareness of warning signs and anticipated help-seeking were assessed using questions from the internationally validated Awareness and Beliefs about Cancer Measure (ABC) (Simon et al, 2012). This had been adapted from the Cancer Awareness Measure (CAM) (Stubbings et al, 2009), and pre-existing surveys for use in telephone interviews (Paul et al, 2006; Park and Clery, 2010). The ABC has acceptable internal validity (Cronbach's α>0.70), content validity (>78%), and test–retest reliability (r⩾0.60) (Simon et al, 2012).
Anticipated time to help-seeking for target symptoms
Help-seeking items from the ABC (Simon et al, 2012) assessed anticipated delay for symptoms that could be indicative of each of the three target cancers: (i) persistent cough, (ii) rectal bleeding, and (iii) breast changes. The interview instructions were: ‘I'm going to read you out a list of signs and symptoms; for each one can you tell me how long it would take you to go to the doctor from the time you first noticed the symptom'. Responses were categorised by the interviewer into predefined time intervals (as soon as I noticed, up to 1 week, 1–2 weeks, 2–3 weeks, 3–4 weeks, more than a month, and I would not contact a doctor). Responses indicating help-seeking from another health professional (e.g. nurse and pharmacist) were excluded from the analyses (persistent cough: n=254; rectal bleeding: n=70; breast changes: n=59). The primary analyses used a dichotomous anticipated help-seeking variable (⩽2 weeks vs >2 weeks) as used in previous analyses (Robb et al, 2009). Analyses were repeated using >4 weeks as a cutoff in a sensitivity analysis.
Recognition of cancer warning signs
Recognition of the three warning signs most closely related to the target symptoms were used in this analysis: (i) persistent cough or hoarseness, (ii) unexplained bleeding, and (iii) unexplained lump or swelling. The interview instructions were: ‘I'm now going to list some symptoms that may or may not be warning signs for cancer. For each one can you tell me whether you think it could be a warning sign for cancer'. The order was rotated and answers were recorded as yes, no, don't know, and refused. For the present analysis, ‘don't know' responses were combined with ‘no', and ‘refused' was coded as missing.
Demographic characteristics and health-care access
Data were collected on gender, age, ethnicity (categorised as white vs other ethnicity), marital status (categorised as married/cohabiting vs single/divorced/separated/widowed), highest level of education (school/further education vs university), and UK region (England, Northern Ireland, and Wales). As an indicator of health-care access, respondents were asked: ‘How easy or difficult, is it for you to get to see the doctor if you have a symptom that you think might be serious' with four response options from ‘very difficult' to ‘very easy'. Responses were dichotomised as difficult vs easy for analysis. This item also allowed us to test whether anticipated time to help-seeking was associated predictably with ease of health-care access.
Analysis
Univariate chi-square analyses were used to explore predictors of recognition of warning signs and anticipated time to help-seeking. Multivariable logistic regression analysis was used to test the associations between recognition of each warning sign and anticipated time to help-seeking for each potential cancer symptom controlling for gender, age, marital status, ethnicity, education, and health-care access.
Results
The sample size was 6965; drawn from England (n=2360), Wales (n=2298), and Northern Ireland (n=2307). Of 24 231 households contacted and assessed for eligibility, 10 997 were eligible to take part, of whom 3468 declined and 564 only partially completed the interview. The final response rate was therefore 40% (AAPOR response rate three conventions: The American Association of Public Opinion Research, 2011; Forbes et al, 2013); similar to previous household telephone surveys (O'Toole et al, 2008). Missing data did not exceed 2.5% for any item. In common with many population surveys, the sample had more women (62.2% vs 53.2%), more respondents with university degrees (22.5% vs 15.2%), fewer from non-white ethnic backgrounds (1.7% vs 7.9%), and fewer aged over 70 (29.7% vs 34.2%) than the UK population in this age range (ONS, 2001; NISRA, 2004; ONS, 2005; ONS, 2011).
Anticipating waiting for >2 weeks to seek medical advice was highest for persistent cough (48.1%), whereas for breast changes and rectal bleeding, only 8.2% and 7.4% anticipated waiting for >2 weeks. As an indicator of internal consistency, those who thought it would be difficult to see a doctor anticipated waiting significantly longer for all three warning signs (P<0.01: see Table 1). Table 1 also shows a trend towards greater anticipated time to help-seeking in younger people, and in those from white and more educated backgrounds. The education effect was significant for all three warning signs (P<0.05), the age effect was significant for persistent cough and rectal bleeding (P<0.001), and the ethnicity effect reached statistical significance for persistent cough only (P<0.001).
Table 1. Demographic and health-care correlates of anticipated time to help-seeking (>2 weeks) for each cancer warning sign.
|
Anticipated time to help-seeking >2 weeks % (n) |
|||
|---|---|---|---|
| Persistent cough | Rectal bleeding | Breast changes (women only) | |
| All respondents (n=6965) |
48.1 (3351) |
7.4 (515) |
8.2 (351) |
|
Gender | |||
| Female (n=4330) | 51.2 (2145)a | 7.1 (306) | 8.2 (351) |
| Male (n=2635) |
47.9 (1206) |
8.0 (209) |
N/A |
|
Age | |||
| 50–59 (n=2346) | 56.5 (1291)b | 9.8 (229)b | 8.6 (123) |
| 60–69 (n=2356) | 52.7 (1293) | 7.6 (192) | 8.6 (133) |
| 70+ (n=2067) |
38.6 (757) |
4.6 (93) |
7.3 (94) |
|
Marital status | |||
| Married/cohabiting (n=3787) | 51.9 (1914)b | 7.5 (283) | 7.3 (152)c |
| Single/divorced/separated (n=3144) |
47.6 (1424) |
7.4 (229) |
9.1 (197) |
|
Ethnicity | |||
| White (n=6830) | 50.1 (3298)c | 7.5 (504) | 8.2 (346) |
| Not White (n=117) |
38.3 (44) |
8.8 (10) |
6.5 (4) |
|
Education | |||
| Degree or above (n=1569) | 60.3 (921)b | 8.8 (137)c | 10.8 (90)a |
| Below degree (n=5224) |
47.0 (2363) |
7.1 (369) |
7.6 (252) |
|
Region | |||
| England (n=2360) | 50.7 (1153)c | 7.1 (165) | 6.9 (100)c |
| Wales (n=2298) | 51.4 (1142) | 7.3 (167) | 9.9 (135) |
| Northern Ireland (n=2307) |
47.7 (1056) |
8.0 (183) |
8.0 (116) |
|
Health-care access | |||
| Easy (n=5785) | 49.0 (2739)a | 7.0 (402)a | 7.4 (259)b |
| Difficult (n=1101) | 54.6 (575) | 9.7 (106) | 12.0 (87) |
Note: Totals vary due to missing data.
X2, P<0.01.
X2, P<0.001.
X2, P<0.05.
The warning sign that was most well recognised was ‘unexplained lump or swelling' (96.6%), followed by ‘unexplained bleeding' (89.7%), and ‘persistent cough or hoarseness' (69.5%). Table 2 shows that recognition tended to be lower for men, older people, and those from ethnic minority and less-educated groups. These effects were significant for all three warning signs (P<0.05), although the absolute differences were sometimes small.
Table 2. Recognition that warning signs might indicate cancer.
|
Recognition of cancer warning signs % (n) |
|||
|---|---|---|---|
| Persistent cough or hoarseness | Unexplained bleeding | Unexplained lump or swelling | |
| All respondents (n=6965) |
69.5 (4838) |
89.7 (6248) |
96.6 (6727) |
|
Gender | |||
| Female (n=4330) | 73.1 (3163)a | 91.6 (3966)a | 96.9 (4197)b |
| Male (n=2635) |
63.6 (1675) |
86.6 (2282) |
96.0 (2530) |
|
Age | |||
| 50–59 (n=2346) | 69.3 (1626)c | 90.2 (2117)c | 97.5 (2288)a |
| 60–69 (n=2536) | 71.5 (1814) | 90.6 (2297) | 97.1 (2463) |
| 70+ (n=2067) |
67.1 (1387) |
88.0 (1818) |
94.8 (1960) |
|
Marital status | |||
| Married/cohabiting (n=3787) | 69.5 (2632) | 90.2 (3414) | 97.0 (3675)b |
| Single/divorced/separated (n=3144) |
69.4 (2181) |
89.3 (2805) |
96.0 (3019) |
|
Ethnicity | |||
| White (n=6830) | 69.7 (4758)b | 89.9 (6141)a | 96.7 (6607)a |
| Not White (n=117) |
59.0 (69) |
79.5 (93) |
88.9 (104) |
|
Education | |||
| Degree or above (n=1569) | 73.9 (1159)a | 92.5 (1451)a | 97.8 (1534)c |
| Below degree (n=5224) |
68.2 (3563) |
89.2 (4660) |
96.3 (5032) |
|
Region | |||
| England (n=2360) | 68.8 (1623) | 89.6 (2113) | 96.5 (2277) |
| Wales (n=2298) | 68.4 (1571) | 89.3 (2051) | 96.5 (2218) |
| Northern Ireland (n=2307) | 71.3 (1644) | 90.4 (2084) | 96.7 (2232) |
Note: Totals vary due to missing data.
X2, P<0.001.
X2, P<0.05.
X2, P<0.01.
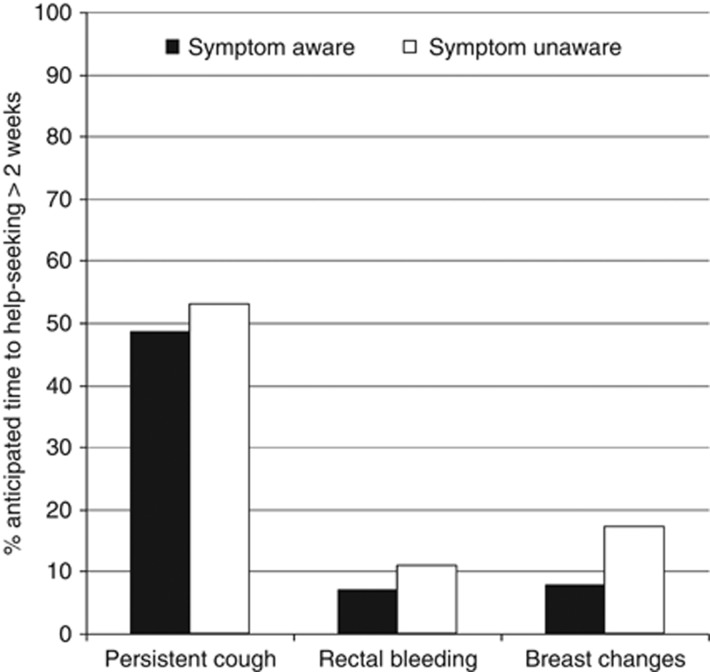
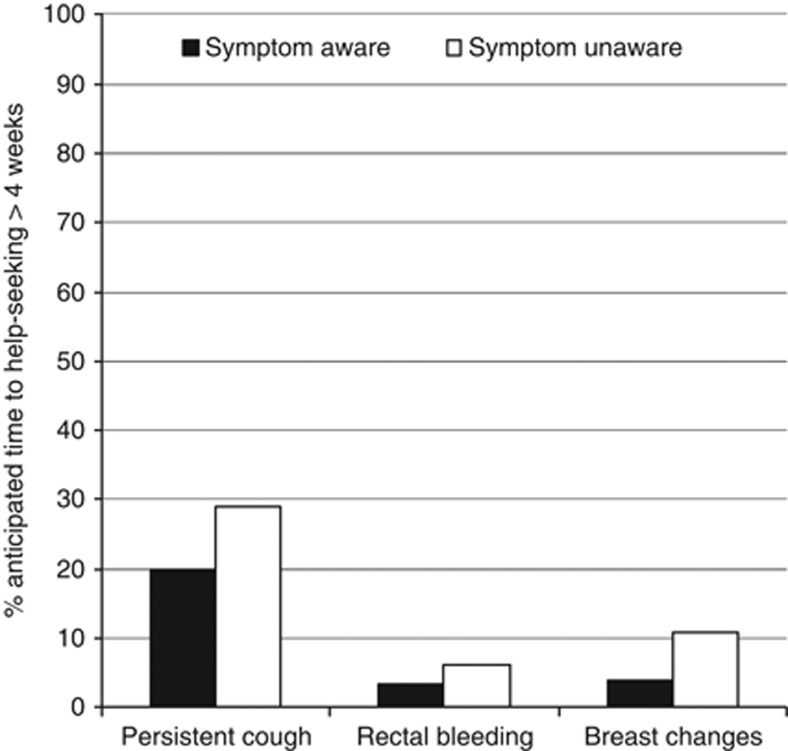
Figure 1 shows that for each symptom, anticipating >2 weeks delay was more common in those who did not recognise the associated warning sign (persistent cough: χ2 (1)=12.10, P=0.001; rectal bleeding: χ2 (1)=14.66, P<0.001; breast changes: χ2 (1)=13.78, P<0.001). We repeated the analyses using anticipated time to help-seeking of >4 weeks, where although the absolute numbers were lower, the patterns were the same (Figure 2).
Figure 1.
Recognition and anticipating >2 weeks before help-seeking for each related symptom (persistent cough/hoarseness, unexplained bleeding, and unexplained lump or swelling).
Figure 2.
Recognition and anticipating >4 weeks before help-seeking for each related symptom (persistent cough/hoarseness, unexplained bleeding, and unexplained lump or swelling).
Multivariable logistic regression analyses (see Table 3) demonstrated that recognition of each warning sign was associated with delay independent of demographic variables and difficulty of access: breast changes (OR=2.45, 1.47–4.08), rectal bleeding (OR=1.77, 1.36–2.30), and persistent cough (OR=1.30, 1.17–1.46). The analyses were repeated using a delay interval of >4 weeks and the odds ratios were similar or higher, and significant in all cases.
Table 3. Predictors of anticipating >2 weeks before help-seeking for a potential warning sign of cancer.
|
Persistent cough (n=6447) |
Rectal bleeding (n=6622) |
Breast changes (n=4097) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |
|
Gender | |||||||||
| Male | 1.00 | – | – | 1.00 | – | – | – | – | – |
| Female |
1.24 |
1.11–1.38 |
0.000 |
0.89 |
0.74–1.08 |
0.232 |
– |
– |
– |
|
Age group | |||||||||
| 50–59 | 1.00 | – | – | 1.00 | – | – | 1.00 | – | – |
| 60–69 | 0.90 | 0.80–1.01 | 0.076 | 0.78 | 0.64–0.96 | 0.021 | 1.04 | 0.80–1.35 | 0.794 |
| 70+ |
0.52 |
0.46–0.59 |
0.000 |
0.44 |
0.34–0.58 |
0.000 |
0.79 |
0.58–1.07 |
0.132 |
|
Marital status | |||||||||
| Married/cohabiting | 1.00 | – | – | 1.00 | – | – | 1.00 | – | – |
| Single/divorced/separated |
0.93 |
0.84–1.03 |
0.166 |
1.14 |
0.94–1.38 |
0.178 |
1.27 |
1.01–1.61 |
0.044 |
|
Ethnicity | |||||||||
| White | 1.00 | – | – | 1.00 | – | – | 1.00 | – | – |
| Not White |
0.44 |
0.29–0.67 |
0.000 |
0.86 |
0.41–1.80 |
0.696 |
0.51 |
0.16–1.66 |
0.264 |
|
Education | |||||||||
| Degree or above | 1.00 | – | – | 1.00 | – | – | 1.00 | – | – |
| Below degree |
0.61 |
0.54–0.68 |
0.000 |
0.83 |
0.67–1.03 |
0.085 |
0.68 |
0.52–0.89 |
0.004 |
|
Ease of seeing doctor | |||||||||
| Easy | 1.00 | – | – | 1.00 | – | – | 1.00 | – | – |
| Difficult |
1.20 |
1.04–1.37 |
0.010 |
1.37 |
1.09–1.72 |
0.007 |
1.61 |
1.24–2.10 |
0.000 |
|
Recognise symptom? | |||||||||
| Yes | 1.00 | – | – | 1.00 | – | – | 1.00 | – | – |
| No | 1.30 | 1.17–1.46 | 0.000 | 1.77 | 1.36–2.30 | 0.000 | 2.45 | 1.47–4.08 | 0.001 |
Abbreviations: OR=odds ratio; 95% CI=95% confidence interval.
The addition of cancer experience (self or close other) did not change the associations.
Discussion
This is the first large-scale, population-based study to examine associations between anticipated time to help-seeking for a potential cancer symptom and recognition of the related warning sign. For each symptom, individuals who did not recognise the related warning sign were more likely to say they would wait for >2 weeks before visiting the doctor. The association was independent of a range of demographic variables and perceived difficulty of health-care access, and was the same using a longer delay interval as the cutoff. These results confirm findings from an earlier study, using a similar measure (the CAM: Stubbings et al, 2009), which found an association between a general awareness score aggregated across nine warning signs and time for help-seeking across symptoms (Robb et al, 2009). The observation from clinical samples that recognition of a symptom as possibly a warning sign is related to prompt help-seeking is therefore visible ‘in anticipation' in a community sample (Ramirez et al, 1999; Smith et al, 2005; Macdonald et al, 2006; Mitchell et al, 2008; Singh et al, 2010).
There are methodological issues that limit the interpretation of the results. Associations between warning sign recognition and anticipated time to help-seeking may be artificially inflated owing to shared method variance. The cross-sectional design precludes any assumption of causality: individuals who tend to be rapid help-seekers may know more about cancer warning signs. To unequivocally demonstrate causation requires an intervention design that modifies recognition and shows effects on symptom presentation. There are also limitations with the measures. Using ‘recognition' of warning signs as the indicator of awareness (rather than recall of warning signs) may overestimate awareness; but given that in everyday life, the challenge for the individual is to recognise that a symptom they are experiencing may be a sign of cancer, recognition has been argued to be the most appropriate measure (Waller et al, 2004). Awareness is also likely to be more complex than a simple yes/no: a person may ‘know' that a lump can indicate cancer but their belief about how a lump should feel, or the broader context such as other symptoms and general health, may contribute to help-seeking decisions (Rauscher et al, 2010). This might help to explain why a significant proportion (48%) of those recognising a persistent cough still anticipated waiting over 2 weeks, which was markedly reduced when using a 4-week cutoff (20%). As cough is a common symptom it is unlikely to cause immediate alarm. The key issue is not the symptom itself, but the persistence and this may have been interpreted differently by different respondents. Time to help-seeking was hypothetical (how soon would you visit the doctor if…), and hypothetical intentions do not always translate into action (Sheeran, 2002). However, finding that the rating of difficulty in accessing a doctor was associated with anticipated time to help-seeking gave some reassurance of internal consistency.
Some of the findings associated with the demographic factors were not predicted; in particular, the tendency for people with more education to report greater delay. In a previous study, we found that higher SES respondents were more likely to say that being too busy was a barrier to seeking medical help (Robb et al, 2009). Future research to examine the help-seeking decision processes in relation to factors such as age, sex, ethnicity, and SES would be valuable.
In terms of strengths, the level of specificity between warning sign and anticipated help seeking should produce a more accurate estimate of the association than the aggregated scores used in previous community studies, because both awareness and time taken to seek help vary across warning signs (Linsell et al, 2008; Macleod et al, 2009). The large sample size made it possible to control for multiple confounding variables and therefore produce a more robust result. The older age of the respondents meant that the likelihood of cancer was higher and therefore predictors of earlier diagnosis are more salient.
These results support UK policy initiatives that include awareness-raising as part of the strategy to promote early diagnosis. However, more work is needed to identify the most cost-effective ways to promote recognition of early warning signs, particularly in disadvantaged populations, and to do it without provoking anxiety or increasing inappropriate help-seeking.
Acknowledgments
We would like to thank Anna Carluccio, Colin Gardiner, Julia Pye, Laura Thomas, and Chris Marshall of IPSOS Mori for coordinating the fieldwork. Kate Aldersey, Martine Bomb, Catherine Foot, Donia Sadik and Emily Fulleylove of Cancer Research UK for managing the programme. ICBP Programme Board: Ole Andersen, Søren Brostrøm, Heather Bryant, David Currow, Anna Gavin, Gunilla Gunnarsson, Jane Hanson, Todd Harper, Stein Kaasa, Nicola Quin, Linda Rabeneck, Michael A Richards, Michael Sherar, Bob Thomas. Academic Reference Group: Neil Aaronson, David Cella, Henrik Møller, Keith Petrie, Liesbeth Van Osch. Funding provided by ICBP Programme Board and supporting Module 2 committees and advisers in the UK. NI study and NI Cancer Registry funded by Public Health Agency for Northern Ireland. Funding for the Welsh arm of this study was provided by Tenovus and the Welsh Government. Professor Jane Wardle is supported by Cancer Research UK. These analyses were carried out with funding from the Department of Health Policy Research Unit in Cancer Awareness, Screening, and Early Diagnosis. The Policy Research Unit in Cancer Awareness, Screening, and Early Diagnosis receives funding for a research programme from the Department of Health Policy Research Programme. It is a collaboration between researchers from seven institutions (Queen Mary University of London, University College London, King's College London, London School of Hygiene and Tropical Medicine, Hull York Medical School, Durham University, and Peninsula Medical School). The views expressed are those of the authors and not necessarily those of the NHS, or the Department of Health.
The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding source.
References
- Allgar VL, Neal RD. Delays in the diagnosis of six cancers: analysis of data from the National Survey of NHS Patients: Cancer. Br J Cancer. 2005;92 (11:1959–1970. doi: 10.1038/sj.bjc.6602587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapple A, Ziebland S, McPherson A. Qualitative study of men's perceptions of why treatment delays occur in the UK for those with testicular cancer. Br J Gen Pract. 2004;54 (498:25–32. [PMC free article] [PubMed] [Google Scholar]
- CR-UK 2010. International Cancer Benchmarking Partnership. Retrieved 21 March 2013 from http://www.cancerresearchuk.org/cancer-info/spotcancerearly/ICBP .
- CR-UK 2012. Spotting The Signs of Cancer for Men. Retrieved 21 March 2013 from http://publications.cancerresearchuk.org/downloads/product/HM_AP_SCE_Male_July_2013.pdf .
- CR-UK 2012. Spotting The Signs of Cancer for Women. Retrieved 21 March 2013 from http://publications.cancerresearchuk.org/downloads/product/HM_AP_SCE_Female_July_2013.pdf .
- Cuthbertson SA, Goyder EC, Poole J. Inequalities in breast cancer stage at diagnosis in the Trent region, and implications for the NHS Breast Screening Programme. J Public Health (Oxf) 2009;31 (3:398–405. doi: 10.1093/pubmed/fdp042. [DOI] [PubMed] [Google Scholar]
- Forbes LJ, Atkins L, Thurnham A, Layburn J, Haste F, Ramirez AJ. Breast cancer awareness and barriers to symptomatic presentation among women from different ethnic groups in East London. Br J Cancer. 2011;105 (10:1474–1479. doi: 10.1038/bjc.2011.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes LJ, Simon AE, Warburton F, Boniface D, Brain KE, Dessaix A, Donnelly C, Haynes K, Hvidberg L, Lagerlund M, Lockwood G, Tishelman C, Vedsted P, Vigmostad MN, Ramirez AJ, Wardle J. Differences in cancer awareness and beliefs between Australia, Canada, Denmark, Norway, Sweden and the UK (the International Cancer Benchmarking Partnership): do they contribute to differences in cancer survival. Br J Cancer. 2013;108 (2:292–300. doi: 10.1038/bjc.2012.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grunfeld EA, Ramirez AJ, Hunter MS, Richards MA. Women's knowledge and beliefs regarding breast cancer. Br J Cancer. 2002;86 (9:1373–1378. doi: 10.1038/sj.bjc.6600260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linsell L, Burgess CC, Ramirez AJ. Breast cancer awareness among older women. Br J Cancer. 2008;99 (8:1221–1225. doi: 10.1038/sj.bjc.6604668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lockwood-Rayermann S, Donovan HS, Rambo D, Kuo CW. Women's awareness of ovarian cancer risks and symptoms. Am J Nurs. 2009;109 (9:36–45. doi: 10.1097/01.NAJ.0000360309.08701.73. [DOI] [PubMed] [Google Scholar]
- Macdonald S, Macleod U, Campbell NC, Weller D, Mitchell E. Systematic review of factors influencing patient and practitioner delay in diagnosis of upper gastrointestinal cancer. Br J Cancer. 2006;94 (9:1272–1280. doi: 10.1038/sj.bjc.6603089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macleod U, Mitchell ED, Burgess C, Macdonald S, Ramirez AJ. Risk factors for delayed presentation and referral of symptomatic cancer: evidence for common cancers. Br J Cancer. 2009;101 (Suppl 2:S92–S101. doi: 10.1038/sj.bjc.6605398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaffery K, Wardle J, Waller J. Knowledge, attitudes, and behavioral intentions in relation to the early detection of colorectal cancer in the United Kingdom. Prev Med. 2003;36 (5:525–535. doi: 10.1016/s0091-7435(03)00016-1. [DOI] [PubMed] [Google Scholar]
- Mitchell E, Macdonald S, Campbell NC, Weller D, Macleod U. Influences on pre-hospital delay in the diagnosis of colorectal cancer: a systematic review. Br J Cancer. 2008;98 (1:60–70. doi: 10.1038/sj.bjc.6604096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichols BS, Misra R, Alexy B. Cancer detection: how effective is public education. Cancer Nurs. 1996;19 (2:98–103. doi: 10.1097/00002820-199604000-00003. [DOI] [PubMed] [Google Scholar]
- NISRA 2004. Theme Table 1. Demography: people, family and households. Retrieved 21 March 2013 from http://www.nisra.gov.uk/archive/census/2001/theme/theme_tables.pdf .
- O'Toole J, Sinclair M, Leder K. Maximising response rates in household telephone surveys. BMC Med Res Methodol. 2008;8:71. doi: 10.1186/1471-2288-8-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olesen F, Hansen RP, Vedsted P. Delay in diagnosis: the experience in Denmark. Br J Cancer. 2009;101 (Suppl 2:S5–S8. doi: 10.1038/sj.bjc.6605383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ONS 2001. Census 2001 National Report for England and Wales Part 1. Retrieved 21 March 2013 from http://www.ons.gov.uk/ons/rel/census-2001-national-report-for-england-and-wales/national-report-for-england-and-wales-part-1/index.html?format=hi-vis .
- ONS 2005. Focus on Ethnicity and Identity Data. Retrieved 21 March 2013 from http://www.ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77-50846 .
- ONS 2011. Population Estimates for UK, England and Wales, Scotland and Northern Ireland, Mid-2010. Retrieved 21 March 2013 from http://www.ons.gov.uk/ons/publications/re-reference-tables.html?edition=tcm%3A77-231847 .
- Palmer RC, Schneider EC. Social disparities across the continuum of colorectal cancer: a systematic review. Cancer Causes Control. 2005;16 (1:55–61. doi: 10.1007/s10552-004-1253-3. [DOI] [PubMed] [Google Scholar]
- Park A, Clery E. British Social Attitudes, 27th Report. National Centre for Social Research; 2010. [Google Scholar]
- Paul C, Girgis A, Wakefield M, Greenbank S, Beckman K, White V, Slevin T, Rogers C, Jalleh G. Cancer-Related Knowledge & Practices: Recommended Survey Items. Version 1 Newcastle. The Public Health Committee of The Cancer Council Australia: New South Wales, Australia; 2006. [Google Scholar]
- Ramirez AJ, Westcombe AM, Burgess CC, Sutton S, Littlejohns P, Richards MA. Factors predicting delayed presentation of symptomatic breast cancer: a systematic review. Lancet. 1999;353 (9159:1127–1131. doi: 10.1016/s0140-6736(99)02142-x. [DOI] [PubMed] [Google Scholar]
- Rauscher GH, Ferrans CE, Kaiser K, Campbell RT, Calhoun EE, Warnecke RB. Misconceptions about breast lumps and delayed medical presentation in urban breast cancer patients. Cancer Epidemiol Biomarkers Prev. 2010;19 (3:640–647. doi: 10.1158/1055-9965.EPI-09-0997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards MA. The national awareness and early diagnosis initiative in England: assembling the evidence. Br J Cancer. 2009;101 (Suppl 2:S1–S4. doi: 10.1038/sj.bjc.6605382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizzo L, Brick JM, Park I. A minimally intrusive method for sampling persons in random digit dial surveys. Public Opin Quarterly. 2004;68 (2:267–274. [Google Scholar]
- Robb K, Stubbings S, Ramirez A, Macleod U, Austoker J, Waller J, Hiom S, Wardle J. Public awareness of cancer in Britain: a population-based survey of adults. Br J Cancer. 2009;101 (Suppl 2:S18–S23. doi: 10.1038/sj.bjc.6605386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roetzheim RG, Pal N, Tennant C, Voti L, Ayanian JZ, Schwabe A, Krischer JP. Effects of health insurance and race on early detection of cancer. J Natl Cancer Inst. 1999;91 (16:1409–1415. doi: 10.1093/jnci/91.16.1409. [DOI] [PubMed] [Google Scholar]
- Sheeran P. Intention-behavior relations: a conceptual and empirical review. Eur Rev Soc Psychol. 2002;12 (1:1–36. [Google Scholar]
- Simon AE, Forbes LJ, Boniface D, Warburton F, Brain KE, Dessaix A, Donnelly M, Haynes K, Hvidberg L, Lagerlund M, Petermann L, Tishelman C, Vedsted P, Vigmostad MN, Wardle J, Ramirez AJ. An international measure of awareness and beliefs about cancer: development and testing of the ABC. BMJ Open. 2012;2 (6:e001758. doi: 10.1136/bmjopen-2012-001758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh H, De CC, Shu E, Fradette K, Latosinsky S, Pitz M, Cheang M, Turner D. Wait times from presentation to treatment for colorectal cancer: a population-based study. Can J Gastroenterol. 2010;24 (1:33–39. doi: 10.1155/2010/692151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith LK, Pope C, Botha JL. Patients' help-seeking experiences and delay in cancer presentation: a qualitative synthesis. Lancet. 2005;366 (9488:825–831. doi: 10.1016/S0140-6736(05)67030-4. [DOI] [PubMed] [Google Scholar]
- Stubbings S, Robb K, Waller J, Ramirez A, Austoker J, Macleod U, Hiom S, Wardle J. Development of a measurement tool to assess public awareness of cancer. Br J Cancer. 2009;101 (Suppl 2:S13–S17. doi: 10.1038/sj.bjc.6605385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The American Association of Public Opinion Research 2011. Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys.
- Waller J, McCaffery K, Wardle J. Measuring cancer knowledge: comparing prompted and unprompted recall. Br J Psychol. 2004;95 (2:219–234. doi: 10.1348/000712604773952430. [DOI] [PubMed] [Google Scholar]
- Waller J, Robb K, Stubbings S, Ramirez A, Macleod U, Austoker J, Hiom S, Wardle J. Awareness of cancer symptoms and anticipated help seeking among ethnic minority groups in England. Br J Cancer. 2009;101 (Suppl 2:S24–S30. doi: 10.1038/sj.bjc.6605387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods LM, Rachet B, Coleman MP. Origins of socio-economic inequalities in cancer survival: a review. Ann Oncol. 2006;17 (1:5–19. doi: 10.1093/annonc/mdj007. [DOI] [PubMed] [Google Scholar]
- Yu ES, Kim KK, Chen EH, Brintnall RA. Breast and cervical cancer screening among Chinese American women. Cancer Pract. 2001;9 (2:81–91. doi: 10.1046/j.1523-5394.2001.009002081.x. [DOI] [PubMed] [Google Scholar]