Abstract
Forty years ago, when the National Institute on Alcohol Abuse and Alcoholism (NIAAA) was founded, alcoholism was considered an adult disease driven principally by physiological determinants. As NIAAA expanded its research portfolio, new data and insights were obtained that led to an increased focus on underage and young adult drinking. Fostered by interdisciplinary research, etiologic models were developed that recognized the multiplicity of relevant genetic and environmental influences. This shift in conceptualizing alcohol use disorders also was based on findings from large-scale, national studies indicating that late adolescence and early young adulthood were peak periods for the development of alcohol dependence and that early initiation of alcohol use (i.e., before age 15) was associated with a fourfold increase in the probability of subsequently developing alcohol dependence. In recent years, developmental studies and models of the initiation, escalation, and adverse consequences of underage and early young adult drinking have helped us to understand how alcohol use may influence, and be influenced by, developmental transitions or turning points. Major risk and protective factors are being identified and integrated into screening, prevention, and treatment programs to optimize interventions designed to reduce drinking problems among adolescents and young adults. In addition, regulatory policies, such as the minimum drinking age and zero-tolerance laws, are being implemented and evaluated for their impact on public health.
Keywords: Underage drinking, drinking in young adulthood, psychosocial development, development of alcohol disorders, risk factors, protective factors, alcohol effects on brain development, screening among youth, preventive interventions, college drinking, treatment for adolescents and young adults
In 1970, the National Institutes of Health (NIH) established the National Institute on Alcohol Abuse and Alcoholism (NIAAA). At that time, both the general public and the scientific community predominantly regarded alcoholism as a disorder of adulthood, and the major focus of NIH-funded scientific work was on understanding its etiology and finding new treatments for it. Most of the etiological research focused on physiological and clinical analyses in adults, and the drinking behavior of adolescents only appeared in discussions of the epidemiology and sociology of drinking patterns (e.g., Kissin and Begleiter 1972, 1976; Popham 1970).
Simultaneously, but unrelated to the research on the adult psychopathology, a separate scientific community was sensitized to the public concern about an illegal activity—underage drinking—that potentially could result in great personal and societal cost in the form of accidents and loss of life. By the late 1970s, a significant body of research was addressing the critical issue of why most youth only begin drinking in mid- to late adolescence and consume alcohol in small amounts at infrequent intervals and without problems, whereas others begin much earlier, and in some cases progress to consuming near-alcoholic levels within a short time after initiation. At that time, NIAAA’s Division of Epidemiology and Prevention increasingly began to support research addressing these issues, and an important body of theory and research began to articulate the developmental nature of drinking behavior and to identify individual and social contextual factors that regulate it (Blane and Chafetz 1979; Jessor and Jessor 1977; Kandel 1978). This research also started to investigate how the initiation of drinking could be delayed and how the occurrence of problems could be reduced once drinking had begun (Kandel 1989; Robins and Przybeck 1985).
As the developmental window from childhood to early adulthood has been studied over the years, research on early drinking origins to adolescent problems on the one hand and on the origins of alcoholism on the other hand has begun to converge. An NIAAA news release in 2004 (Li 2004) articulates this integration, stating that both alcohol-related problems and alcohol use disorders (AUDs) needed to be understood developmentally because they originate before adulthood; moreover, the highest prevalence of alcohol dependence occurs in youth ages 18–20 (Grant et al. 2004). Since then, research on underage drinking has increasingly crossed disciplines and now involves integrative work on the genetics and neurophysiology of risk that is being tied to behavioral and social environmental science (Clark et al. 2008; Kendler and Prescott 2006; McGue et al. 2001).
Two initiatives in the past decade underscore NIAAA’s recognition of the importance of underage and early adult drinking as a problem area of national significance and also have led directly to the work summarized in this article. One initiative, kicked off in 1998, was the Task Force on College Drinking (NIAAA 2002; also see the article by Hingson, pp. 45–54), which was charged with reviewing the existing research on college drinking as a basis for implementing and evaluating alcohol prevention programs. The other is the Underage Drinking Research Initiative (National Academy of Sciences 2004; also see sidebar), which was formed in 2004 to intensify research, evaluation, and outreach efforts on the underage drinking problem. This initiative is ongoing and has led to the development of the committee on Assessment and Screening for Underage Drinking Risk.
NIAAA’s Underage Drinking Research Initiative.
The National Institute on Alcohol Abuse and Alcoholism’s (NIAAA’s) Underage Drinking Research Initiative was undertaken in response to the convergence of recent scientific advances and the increased public concern about the seriousness of underage drinking and its personal and societal costs. These concerns were expressed cogently both in the 2007 Surgeon General’s Call to Action To Prevent and Reduce Underage Drinking (U.S. Department of Health and Human Services 2007) and by the 2004 report Reducing Underage Drinking: A Collective Responsibility (Bonnie and O’Connell 2004), which was sponsored by the National Research Council and the Institute of Medicine. The focus of this NIAAA initiative is to intensify research, evaluation, and outreach efforts regarding underage drinking. To accomplish this, NIAAA formed an interdisciplinary working group on underage drinking that consisted of NIAAA staff members and a multidisciplinary steering committee. The mission of the steering committee is to stimulate research on underage drinking by drawing upon multiple disciplines (e.g., adolescent development, genetics, neuroscience, prevention, and social policy) to advise NIAAA on future research to improve the prevention and treatment of underage drinking.
Thus far, goals identified by the steering committee have yielded numerous products, including two special issues in scientific journals (i.e., the April 2008 issue of Pediatrics [Suppl. 4] and a 2009 issue of Alcohol Research & Health [Vol. 32]) that summarized existing research and identified important gaps. NIAAA also has established a Web site for the Underage Drinking Initiative (http://www.niaaa.nih.gov/AboutNIAAA/NIAAASponsoredPrograms/underage.htm) that contains updated statistics on underage drinking; updates from the Steering Committee; print publications for parents, teachers, and young people, such as “Keep Kids Alcohol Free: Strategies for Action;” multimedia resources; and other NIAAA-sponsored sites relevant to underage drinking. Other NIAAA-sponsored sites include The Cool Spot (http://www.thecoolspot.gov), an interactive site designed for young people that features FAQs, statistics, and other information about underage drinking, and The Leadership to Keep Children Alcohol Free (http://www.alcoholfreechildren.org), a unique coalition of Governors’ spouses, Federal agencies, and public and private organizations whose focus is on preventing the use of alcohol by children.
References
- Bonnie RJ, O’Connell ME, editors. Reducing Underage Drinking: A Collective Responsibility. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . The Surgeon General’s Call to Action To Prevent and Reduce Underage Drinking. Rockville, MD: U.S. Department of Health and Human Services, Office of the Surgeon General; 2007. [PubMed] [Google Scholar]
This article provides a brief snapshot of the current scientific knowledge about these earliest drinking years. It summarizes the epidemiologic evidence that documents the importance of the adolescent and young adult periods in determining level of alcohol consumption. The article then examines the developmental nature of problem use, explores why the developmental changes of this age period are of particular importance from a public health standpoint, describes the critical nature of timing in the onset of drinking behavior, and explains the manner in which the changes in drinking that occur between age 10 and the early 20s map onto other developmental challenges of this period of life. Finally, the article briefly reviews current knowledge about the risk and protective factors that exist during adolescence and young adulthood and summarizes the screening, prevention, and intervention programs focused on this age-group. Note that although the specific age ranges referenced in different places in this article may vary to some extent contingent on the cited studies, there is consistent agreement regarding the problematic nature of underage and young adult drinking.
Epidemiology of Underage and Young Adult Drinking
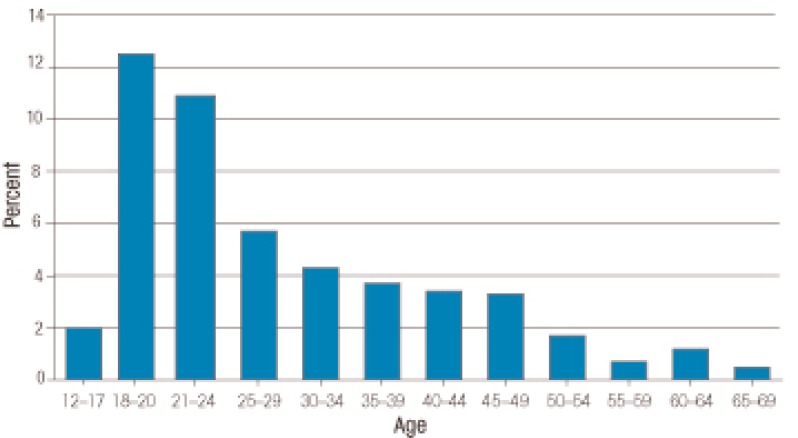
National, large-scale surveys conducted over the past 20 years have provided new insights into the prevalence of alcohol consumption, binge drinking, and AUDs, which have altered the manner in which alcohol use and AUDs are viewed by professionals and lay people alike. For example, data from the NIAAA-funded National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) (Grant et al. 2004) have indicated that the prevalence of past-year alcohol dependence is highest in late adolescence (ages 18–20) and early young adulthood (ages 21–24), with rates declining thereafter (see figure 1). Similar findings have been reported in other national surveys, such as the National Survey of Drug Use and Health (NSDUH), which found that the highest prevalence of lifetime AUDs was reported in late adolescence and early young adulthood (Substance Abuse and Mental Health Services Administration [SAMHSA] 2003, 2004, 2006). For instance, according to the NSDUH, for a variety of population subgroups (i.e., both male and female as well as for White, Black, and Hispanic subjects) the highest rate of AUDs was found in people ages 18–25 years.
Figure 1.
Prevalence of past-year DSM–IV alcohol dependence in the United States.
SOURCE: 18+ years: 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions, 12–17 years: National Survey on Drug Use and Health 2003.
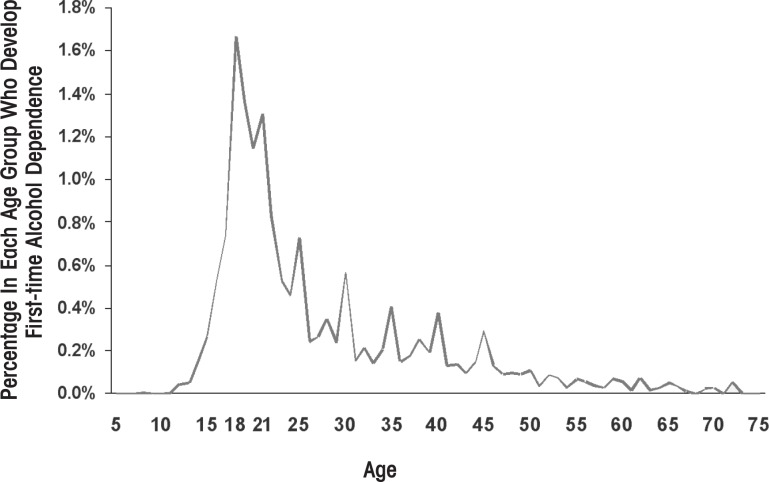
Another way to examine the association between age and AUDs is to evaluate the age at onset of alcohol dependence. This variable is important because an earlier age at onset has been associated with a more severe course of alcoholism, poorer treatment response, and higher relapse rates (Windle and Scheidt 2004). NESARC determined the age at onset of alcohol dependence for a national sample of over 43,000 adults (see figure 2). The findings indicated that onset of first-time alcohol dependence occurred most commonly in late adolescence to early young adulthood, subsequently declining with age.
Figure 2.
Age at onset of DSM–IV alcohol dependence. Data were derived from the 2003 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC).
SOURCE: NIAAA National Epidemiologic Survey on Alcohol and Related Conditions 2003.
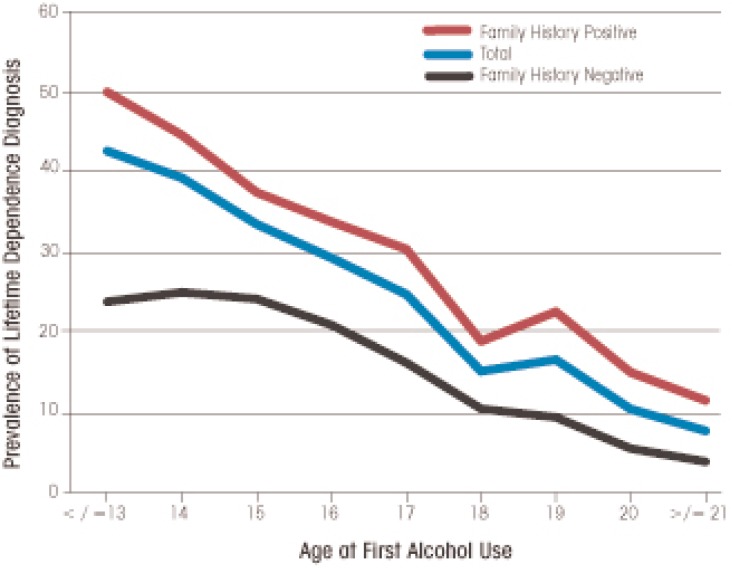
Yet another variable relevant to the association between age, alcohol use, and alcohol dependence is the age of first use of alcohol and its relationship to an important risk factor (i.e., family history of alcoholism). Grant and Dawson (1997) reported that among people who developed alcohol dependence, having a family history of alcoholism (i.e., an alcoholic parent) was significantly associated with an earlier age of first use of alcohol (also see figure 3). For example, among people with alcohol dependence who were family-history positive, almost 60 percent initiated drinking at age 13. By contrast, among people who developed alcohol dependence and were family-history negative, only about 28 percent initiated drinking at age 13. This finding demonstrates that a family history of alcoholism is associated with an earlier age of first use of alcohol, which for many people ultimately evolves into alcohol dependence in later adolescence or young adulthood.
Figure 3.
Association between age at initiation of alcohol use and lifetime dependence (i.e., meeting the DSM–IV criteria for dependence at some point in life). The blue curve represents all respondents, the red curve represents respondents with a family history of alcoholism, and the black curve represents respondents without a family history of alcoholism.
SOURCE: 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions.
The prevalence of AUDs is a valuable indicator of serious alcohol problems during late adolescence and early young adulthood. Another important parameter is the frequency of alcohol consumption and binge drinking among underage drinkers and young adults. In the United States, alcohol consumption occurs in the majority of adolescents (i.e., is statistically normative). According to the 2008 Monitoring the Future Survey (MFS) (Johnston et al. 2009), almost 72 percent of high-school seniors reported consuming alcohol during their lifetime. Moreover, 43 percent had consumed alcohol in the past 30 days, 28 percent reported being drunk in the past 30 days, and 25 percent had been binge drinking1 in the past 2 weeks (see the table). The survey findings allow several conclusions regarding patterns of alcohol use among middle- and high-school students.
Table.
Prevalence (%) of Various Indicators of Alcohol Consumption by Race/Ethnicity, Gender, and School Grade, in 2008.
| Demographic Variables | Alcohol Use in the Past 30 Days | Percentage of Students Reporting Having Been Drunk in Past 30 Days | Having Had Five or More Drinks in a Row in Past 2 Weeks | ||||||
|---|---|---|---|---|---|---|---|---|---|
| School grade | 8th | 10th | 12th | 8th | 10th | 12th | 8th | 10th | 12th |
| Race/ethnicity | |||||||||
| White | 15.2 | 33.3 | 48.6 | 5.5 | 19.2 | 32.7 | 7.8 | 23.5 | 29.9 |
| Black | 12.9 | 20.6 | 28.6 | 3.8 | 8.0 | 14.8 | 5.7 | 11.0 | 10.9 |
| Hispanic | 21.5 | 33.7 | 38.9 | 6.7 | 14.0 | 22.2 | 12.3 | 26.0 | 21.5 |
| Gender | |||||||||
| Total | 15.9 | 28.8 | 43.1 | 5.4 | 14.4 | 27.6 | 8.1 | 16.0 | 24.6 |
| Male | 15.4 | 28.6 | 45.8 | 5.3 | 14.6 | 29.2 | 8.1 | 16.6 | 28.4 |
| Female | 16.4 | 29.0 | 40.9 | 5.4 | 14.3 | 26.2 | 8.0 | 15.4 | 21.3 |
SOURCE: National Institute on Drug Abuse and University of Michigan, Monitoring the Future Surveys (Johnston et al. 2009).
For the three alcohol use indicators (i.e., drinking in the past 30 days, being drunk in the past 30 days, and binge drinking in the past 2 weeks), prevalence increased substantially as teens moved from early to middle and later adolescence.
Whereas younger male and female adolescents were similar in their use of alcohol, older male adolescents were somewhat more likely to be current drinkers and to use alcohol in heavier amounts than were female adolescents in the same grades.
Across grades, Black adolescents reported lower levels of current and heavy alcohol use than did White and Hispanic teens. At younger ages, Hispanic teens were slightly more likely to use alcohol than White teens, but by 12th grade, this relationship had been reversed. This latter finding may be attributable, in part, to higher school dropout rates among Hispanics compared with Whites and Blacks. That is, Hispanic teens who drink at higher rates may be more likely to drop out of school and therefore are not included among seniors in these school-based epidemiologic studies.
Although absolute prevalence rates may differ somewhat, these patterns of alcohol use in terms of age, gender, and race/ethnic group differences obtained in the MFS are consistent with those found in other surveys, including the Centers for Disease Control and Prevention (CDC)-funded Youth Risk Behavior Surveillance Survey and the NSDUH (CDC 2005; Johnston et al. 2009; SAMHSA 2003, 2004, 2006).
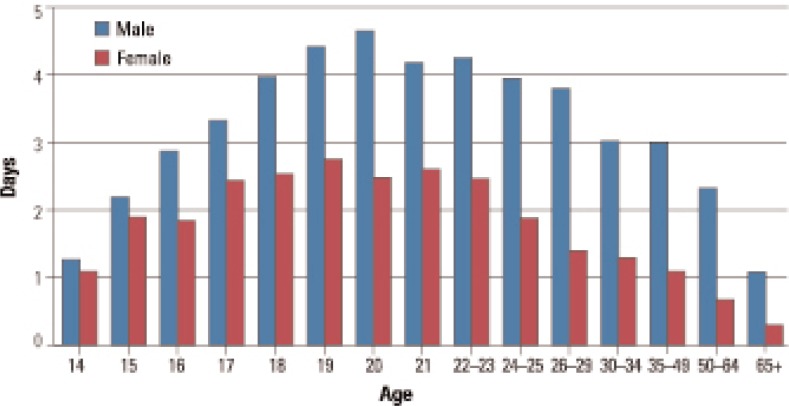
Research studies based on national survey data from both adolescents and adults have indicated that heavier alcohol use distinguishes late adolescents and early young adults from adults. For example, for male and female subjects, binge drinking increased during adolescence, peaked between ages 18 and 25 years, and declined thereafter (see figure 4). Similarly, the MFS indicated that the prevalence of “having been drunk” in the past year increased substantially from 8th grade (12.7 percent) to 12th grade (45.6 percent) and to young adulthood (66.0 percent).
Figure 4.
Number of days in the past 30 days on which drinkers consumed five or more drinks, by age and gender.
SOURCE: Substance Abuse and Mental Health Services Administration, National Survey on Drug Use and Health 2007.
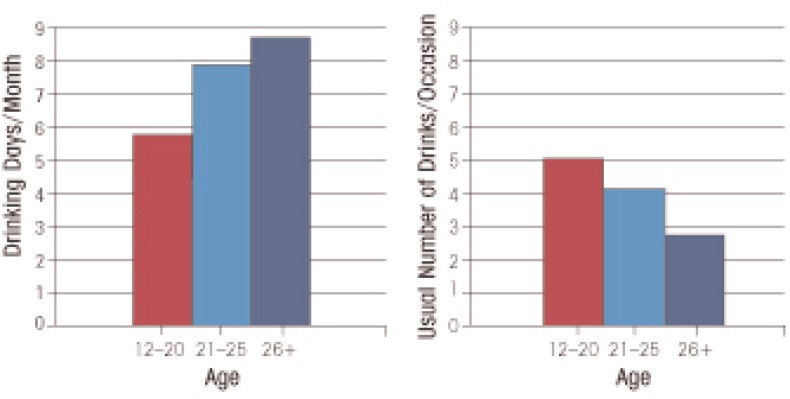
Another measure of drinking patterns during different portions of the life-span is the number of drinking days per month and the usual number of drinks per drinking occasion (see figure 5). Survey data indicate an ordering by age-group of these variables—that is, underage drinkers had the fewest number of drinking days per month but drank the most on the days that they did drink; young adults followed the underage group with fewer drinking days and more drinks per occasion than adults. Thus, compared with adults, underage drinkers and young adults drink on fewer occasions but consume more per occasion. This drinking pattern may be more hazardous to the drinker’s social functioning and physical and mental health.
Figure 5.
Number of drinking days per month and usual number of drinks per occasion for youth (ages 12–20), young adults (ages 21–25), and adults (ages 26 and older).
SOURCE: Substance Abuse and Mental Health Services Administration, National Survey on Drug Use and Health, 2007.
In summary, extant epidemiologic data indicate that the prevalence of alcohol use begins in early adolescence, steadily increases throughout the high school years, reaches a peak in the mid-20s, and begins to decline thereafter. The findings are consistent across different indicators of drinking (e.g., alcohol use, drinking to intoxication, and binge drinking) and across sex and racial/ethnic groups. These age trends also are evident for AUDs, which peak in late adolescence and early young adulthood.
The Developmental Nature of Underage and Young Adult Drinking
The prevalence data on alcohol use and AUDs clearly illustrate that adolescence and early young adulthood are critical for understanding the occurrence of these conditions. In and of themselves, these findings do not necessarily indicate that alcoholism is a developmental disorder. However, data on age of initiation of alcohol use and its relationship to the subsequent development of alcohol dependence provides a strong indication of the developmental nature of AUDs. Grant and Dawson (1997) reported that people who began drinking before age 15 were four times more likely to subsequently become alcohol dependent than people who did not drink alcohol before age 21. Furthermore, the odds of subsequently developing alcohol dependence were reduced by 14 percent with each increasing year of age at first use. This latter finding is the source of intervention programs targeted at delaying the age of initiation of alcohol use.
The significance of earlier initiation as a risk factor for AUDs, in conjunction with other data based on longitudinal studies, has fostered the notion of the developmental nature of underage and young adult drinking, which has been confirmed by other findings. For example, Greenfield and Rogers (1999) reported that adolescents to young adults ages 18–29 were disproportionately represented among the heaviest drinkers. Thus, although this age-group represented only 27 percent of the U.S. population, they accounted for about 45 percent of overall adult drinking. In an analysis of the commercial value of underage drinking, Foster and colleagues (2006) determined that in 2001, the short-term cash value to the alcohol industry from underage drinkers was 22.5 billion dollars, representing 17.5 percent of total consumer expenditures for alcohol beverages.
In a separate study using different data sources, Miller and colleagues (2006) estimated that in 2001, underage drinkers accounted for 16.2 percent of all alcohol sales in the United States. However, the economic costs attributable to alcohol-related youth problems, such as drinking and driving, interpersonal violence, property crimes, and suicide, totaled $61.9 billion (in 2001 dollars). These costs included medical care costs, lost work and other monetary costs, and quality-of-life costs. Hence, underage and young-adult populations clearly are heavy consumers of alcoholic beverages and result in economic costs that are nearly three times higher than the profits of the alcohol industry.
From a public health perspective, it also is important to highlight that the three major causes of death among 12- to 20-year-olds in the United States—unintentional injuries (with motor vehicle crashes accounting for the majority of deaths), homicides, and suicides (Subramanian 2006)—all are associated with alcohol use, especially heavy use. For example, in 2003, motor vehicle crashes were the leading cause of death among 12- to 20-year-olds. In that same year, a report by the National Highway Traffic Safety Administration (Pickrell 2006) indicated that among drivers ages 20 years or younger who were involved in fatal traffic crashes, approximately 20 percent had consumed alcohol at the time of the crash. In addition, the median blood alcohol concentration (BAC) for this age-group ranged from 0.12 to 0.14 percent, well above the legal limit of intoxication (i.e., 0.08 percent) of intoxication.
Finally, higher levels of alcohol use are associated not only with increased mortality but also with a broad range of other problem behaviors, including cigarette and other drug use, deviant behavior, earlier sexual activity and increased risk for sexually transmitted infections (including infection with the human immunodeficiency virus [HIV]), as well as truancy, academic difficulties, and school drop out. These consequences of heavy alcohol use among teenagers and young adults affect not only the drinker but also may adversely impact others via alcohol-related injuries and violence (e.g., victims of adolescent or young adult alcohol-related crashes, campus disruptions, or enhanced aggressive tendencies).
Clearly, the morbidities, mortality, and collateral damage associated with underage and early young adult drinking represent a pervasive public health problem involving the entire population in this age-group. Therefore, appropriate responses also should be targeted at the entire adolescent and young adult population rather than be restricted only to those who meet clinical diagnostic criteria for an AUD.
Developmental Framework for Understanding Underage and Young Adult Drinking
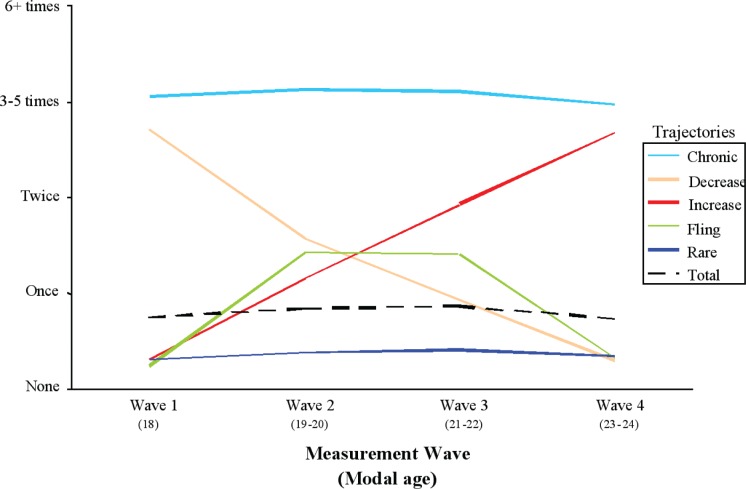
As the findings provided in the previous sections show, drinking behavior and drinking problems change across adolescence and young adulthood, with a clear pattern of age-graded variation. To consider these changes as “maturation”—that is, as a process of emergence and linear growth of alcohol use and alcohol problems—is insufficient because drinking levels across this developmental period vary considerably among individuals. These differences in course have been demonstrated vividly by Schulenberg and colleagues (1996) in their trajectory analysis of a nationally representative sample they had followed through ages 18–22 years. The analysis found that the pattern of binge drinking based on the means of the total sample over the interval does not reflect the pattern for any subset of individuals (see figure 6) but is a composite of five starkly different trajectory courses:
A chronic trajectory of continuously high frequency of binge drinking;
A trajectory with decreasing frequency of binge drinking over time;
A trajectory with increasing frequency of binge drinking over time;
A “fling” trajectory with a transient increase in binge drinking frequency; and
A trajectory of continuously low frequency of binge drinking.
Figure 6.
Different patterns (i.e., trajectories) of binge drinking over time among people ages 18–24. For the studied population as a whole, the overall frequency of binge drinking remained relatively steady at less than one time per 2-week interval. More detailed analysis, however, identified five subgroups of drinkers that differed in how frequency of binge drinking evolved over time.
SOURCE: Schulenberg et al. 1996.
More recent trajectory studies of this age-group continue to support the validity of these trajectory patterns, although class membership percentages vary somewhat as a function of sample age, number of waves of data available, and trajectory class analytic method (Brown et al. 2008; Windle et al. 2005). It is important to note, however, that this variability is occurring during a developmental period when a great deal of life change is occurring. (This will be discussed further below.)
A maturational concept of the development of drinking behaviors does not account for these radically different trajectories, nor is it capable of addressing a variety of major public health concerns about drinking in this and younger age-groups, such as the following:
Why does drinking start when it does?
Why do some youth cross that threshold earlier than others?
How can we explain the fact that some youth begin drinking in mid-to late adolescence in small amounts at infrequent intervals and without problems, and others begin much earlier, with some drinking at near-alcoholic levels within a short time after they start?
Do factors unrelated to alcohol play any significant role in the development of drinking?
To address these questions, researchers have turned to a developmental conceptual model of stability and change that also has served as a powerful guide for investigation in fields as far removed as plant biology, evolutionary biology, and early childhood development. The model emphasizes the importance of studying earlier behaviors and identifying the multilevel processes involved in creating them and the contexts in which they emerge, persist or change, increase or decline (Cicchetti 2006; Masten et al. 2008). Understanding the earlier system of relationships provides clues to continuity, even when no apparent link exists, and discontinuity, even when there appears to be no organismic explanation of it.
Examples of the Utility of the Developmental Framework
The developmental framework described above can be used to probe the causes of, and highlight the critical issues associated with, underage and young adult drinking. This is illustrated here with three examples.
Exploring the Salience of Earlier Behavior for Later Outcomes
One of the major principles of development is that later behavior evolves out of earlier behavior and that the pathway is identifiable, even though the later manifestations may be more differentiated or even changed in structure or appearance (i.e., morphologically changed). For example, there is compelling evidence that a developmental connection exists between behavioral undercontrol in early life and problem drinking and AUD outcomes in late adolescence and early adulthood.
In adolescence and young adulthood, one of the most robust correlates of problem alcohol use is behavioral undercontrol (Zucker et al., in press). Measures of this construct are subsumed under a number of different labels, such as disinhibition, externalizing behavior, aggressiveness, delinquency, conduct problems, and sensation seeking (Brown et al. 1996; Clark et al. 2005; Dubow et al. 2008; Guo et al. 2001; Jessor and Jessor 1977). These measures are positively correlated with one another, tend to operate similarly in their relationships with other variables, and in factor analyses load on the same factor (Bogg and Finn, in press; Donovan and Jessor 1985). Moreover, longitudinal studies have found that behavioral undercontrol in adolescence is a robust predictor of alcohol problems, AUDs, and other substance use disorders in early adulthood (Brown et al. 1996; Clark et al. 2005; Dubow et al. 2008). However, the question is whether this relationship already exists at earlier developmental stages.
The evidence for such a connection in fact is quite strong and has been replicated many times. A recent review (Zucker 2006) identified four longitudinal studies in the general population and two studies with high-risk subjects that found a positive relationship between measures of undercontrol and aggressiveness in early to middle childhood and problem alcohol use in mid-adolescence and severe alcohol problems and AUDs in young adulthood. In two of those studies, undercontrol/disinhibition was identified as early as the preschool years. Another series of four longitudinal studies (Schulenberg and Maggs 2008) reported similar relationships. Without the conceptual framework of developmental theory, it is doubtful that this long chain of relationships would have been uncovered. Yet these relationships are highly significant because they indicate that some central etiologic components that contribute to alcohol problems and AUDs are nonspecific to alcohol. And whatever the underlying predisposition is, it is sufficiently strong to emerge very early in the developmental course. Moreover, the strength of the developmental pathway suggests it should be, to a substantial degree, under genetic control.
Contexts of Alcohol Use and Life Cycle Transitions
Home is the primary source of alcohol in childhood and preadolescence (Donovan and Molina 2008) and one of the primary sources in early adolescence (Centers for Substance Abuse Research 2008). Similarly, associating with peers who already drink is one of the most important proximal causes of drinking onset and problem use during adolescence (Wills and Cleary 1999). Differences in level of use in differing contexts, which in turn make alcohol more or less available, are only part of the way that these drinking environments exert their effects. The presence of alcohol also is a cueing effect, a stimulus for thinking that one could have a drink. Similarly, the fact that someone else already is drinking also acts as a cue because it demonstrates the acceptability of the behavior (Bank et al. 1985).
Lifecycle transitions, such as those occurring during adolescence and young adulthood, also are times of context change, although primarily in relationships and identity rather than in physical contexts. They are points in the life course where the developmental demand is for changes in age-and gender-specified roles. Some of these changes—such as the onset of puberty and parallel onset of adolescence or the onset of parenthood— primarily are driven by biological events, although they typically also have a strong socially prescribed component. Other context changes, such as moving away to college or starting a full-time job, are dictated more by the role demands of the culture. Changes in patterns of alcohol use have been linked to all of these context changes. Some of the changes typically involve increases in alcohol use, such as the move away from home (Stice et al. 1998) and the transition to college (Timberlake et al. 2007). Conversely, some changes, such as the onset of parenthood (Bachman et al. 1996), marriage (Gotham et al. 2003), or the shift from being a college student to full-time employee (Bachman et al. 1996), involve decreased alcohol use. Thus, these transition times pose a significant challenge to the adolescent or young adult not only with respect to the successful adaptation to new life tasks but also with respect to alcohol use. During transitions to contexts typically associated with increasing alcohol use, the challenge is to resist this demand or at least to moderate it so alcohol use does not become excessive (Maggs 1997). During transitions where the demand is for decreasing alcohol use, the challenge is to move from a previously unrestrained pattern of use to one of greater restraint. At the same time, these turning points potentially are useful places for intervention, where a small amount of assistance or guidance can have major impact (see Blomberg 1992; Cunningham et al. 2009). For example, the College Drinking Initiative has been influenced by turning-point transitions in guiding university interventions (NIAAA Research Findings on Underage Drinking and Minimum Legal Drinking Age 2008).
Social Policy Regarding Minimum Legal Drinking Age
One of the most dramatic policy actions of the last generation has been legislation that increased the minimum legal drinking age (MLDA) from 18 to 21 years. Recent advocacy efforts to return to an MLDA of 18 years minimum could suggest that the change had been ineffective. However, scientific evidence unequivocally demonstrates that drinking-and-driving crashes and the resulting loss of life among 18- to 20-year-olds have declined as a result of the legislation, even though the size of the effect varies among States (Shults et al. 2001; Wagenaar and Toomey 2002). Moreover, the influence of this legislation extends to young adults older than 21 years of age, providing an indication of the long-lasting impact of this change. Thus, lower drinking rates persisted in the subsequent 21- to 25-year age-group (O’Malley and Wagenaar 1991). Recent work also has shown lasting differences in drinking outcomes between those living in the era before the MLDA of 21 years was in effect and those who were exposed to the legislation. Even when in their 40s and 50s, people not exposed to the MLDA legislation had higher rates of both AUDs and other substance use disorders than did people who were affected by the legislation (Norberg et al. 2009).
Although the effects of changing the MLDA have been studied the longest, analyses of the effects of the more recent policy changes (i.e., reduction of legal blood alcohol limits and zero-tolerance laws) on adolescents and young adults under age 21 years also show significant reductions in drinking while driving (Wagenaar et al. 2001) and alcohol-related problems (e.g., DUI citations and alcohol-involved fatal crashes) (Voas et al. 2003). All these findings demonstrate that changes in MLDA, lower legal blood alcohol limits, and zero-tolerance laws indeed have had an impact on underage drinking and related problems.
Risk and Protective Factors of Underage and Young Adult Drinking
As young people deal with the challenges and opportunities of adolescence and early adulthood, they are exposed to numerous influences that either increase their risk of developing alcohol-related problems and AUDs or reduce that risk. This section highlights some of these risk and protective factors.
Risk Factors
The inventory of risk factors that increase the likelihood of problem alcohol use in the underage and young adult population is considerable. A comprehensive review of these factors is beyond the scope of this article (for more intensive reviews see Brown et al. 2008; Windle et al. 2008); instead, the discussion will focus on three critical risk issues that are explored in some detail, using them as a vehicle around which to examine the operation or function of specific risks.
Family History
Male children of alcoholics (COAs) are four to nine times more likely to develop alcoholism in adulthood, and female COAs are two to three times more likely than are children without such a family history (Russell 1990; also see figure 3). Approximately 50 percent of that risk is conveyed through genetic factors (Dick and Bierut 2006; McGue 1999). There are a number of pathways through which such genetic risk can be transmitted from parent to child, all of which are relevant in the developmental period discussed here (i.e., adolescence to young adulthood). Some of the risk is conveyed via direct genetic effect on the offspring—that is, genes responsible for relevant characteristics are passed on from parent to child. The relevant characteristics may include structural and functional differences in brain physiology (e.g., variation in spatial memory; [Pulido et al. 2009]), differences in peripheral physiological systems (e.g., intensity of response to alcohol [Schuckit et al. 2004]), and temperament differences (e.g., behavioral undercontrol) that appear very early in life (e.g., Dick et al. 2006, 2009) and which play a major role in the developmental pathway to problematic alcohol and other drug (AOD) use in adolescence and young adulthood. One such temperamental trait is behavioral undercontrol/disinhibition, which already has been discussed in the previous section. It conveys risk through several pathways:
By leading the youngster into relationships with undercontrolled peers who are more likely to be early and heavier alcohol users;
By interfering with normal inhibitory mechanisms, thereby allowing alcohol use to continue even when it reaches problem levels; and
By potentially facilitating use even in circumstances that are likely to cause problems (e.g., engaging in unprotected sex, driving while intoxicated, drinking instead of studying).
However, some genetic risk also is conveyed indirectly, through the behavior of alcoholics as parents. Thus, COAs obviously are exposed to greater alcohol consumption in the home, with its attendant context risks of availability and modeling that were described previously. It is not surprising, therefore, that COAs begin drinking earlier than their non-COA peers, with a small subset beginning even in preadolescence (see figure 3). In fact, the greatest differences in prevalence between COAs and non-COAs occur very early, illustrating the effect of some of the family differences described above. Similarly, COAs are more likely to have been drunk by early adolescence (Wong et al. 2004), and, as described earlier, they are more likely to develop an AUD as they become older.
Furthermore, alcoholic homes are more likely to be high in conflict (Loukas et al. 2001, 2003) and to expose children to spousal violence and parental divorce (Leonard 2002; Roberts and Linney 2000) than homes without an alcoholic parent. This difference may be a direct result of parental intoxication or an indirect result of parental conflict over spousal consumption. High levels of conflict, violence, and divorce also are risk factors for earlier use by offspring and more problematic use once drinking has begun.
Risk Cascades
Although the list of apparently consequential risk factors associated with COA status is long, this does not mean that risk automatically is conferred whenever there is a positive history. Although the relationships between family history and each of these risks are significant, not all alcoholic families share all attributes. For those COAs who experience fewer of these risk elements, the “weight” of the risk burden is lower, as is the probability of a problem outcome. Furthermore, some people without a positive family history also may experience early and heavy exposure to alcohol, family conflict, instability, or life stress. Additionally, the genes that put a person at elevated risk are present not only in alcoholic families, and not all risk factors are familial in nature. For example, neighborhood social disorganization is a non–alcohol-specific and nonfamilial factor that has been shown to affect risk development in adolescence and in later adulthood (Buu et al. 2007, 2009).
In recent years, developmental psychopathologists have suggested that a cascade model of risk accumulation may best characterize how this multiplicity of risk factors develops (Masten et al. 2005). The model proposes that not just simple addition of various risk factors but their sequencing as well as the timing of when they enter the individual’s life determine risk accretion or risk dilution. Thus, exposure to a given risk factor at one time period can create elevated risk, whereas exposure to the same factor at another time may have little impact. Furthermore, each step in the cascade of risk increases the predictive value of the preceding step, and moving out of the cascade subsequently decreases prior risk. A recent cascade analysis by Dodge and colleagues (2009) describes the interplay of seven different risk domains involving the child, parents, and peers, in a transactional process over the course of childhood that culminates in substance use onset. The analysis indicated that not only risk accumulation at each new step of the cascade is important but opportunities for risk offset also are critical because they suggest concrete, phase-specific ways in which intervention programs might interrupt what otherwise would be a sequence of risk potentiation or elevation.
Alcohol Use and Adolescent Brain Development
A recurring theme of this article is that adolescence is a time of increasing alcohol consumption and that consumption typically peaks during the late adolescent to early adult years. This consumption pattern and the problems associated with excessive alcohol use alone would mark this developmental stage as a period of special risk for adverse consequences. This risk, however, is further exacerbated by the fact that adolescence also is a time of major changes in brain structure and function. Neural alterations are taking place particularly in brain areas at the front of the brain that are part of executive and reward systems involved in impulse control and emotional regulation. For example, an area called the dorsolateral prefrontal cortex—which is especially important to decision making and planning—is one of the last brain areas to mature, with structural change continuing through adolescence into early adulthood (Gogtay et al. 2004). Developmental changes related to increasing the development of myelin sheaths around nerve fibers in the central nervous system (i.e., myelogenesis) directly affect impulse and emotional regulation, and there also are gains in the ability to suppress or inhibit irrelevant information (Casey et al. 2002), which in turn are crucial skills in social relationships and in decision-making. Findings primarily obtained in animal studies, but to a limited degree also supported by human cross-sectional studies, suggests that high alcohol (and other drug) consumption during this developmental period may have lasting effects on the maturation of these critical brain areas, inhibiting the development of crucial regulatory and decision-making circuitry (Clark et al. 2008; Spear 2000). Accordingly, the fact that late adolescence/early adulthood often is the time of highest alcohol consumption potentially makes the problem even more serious. Moreover, even within the adolescent period, the highest consumers are likely to be early-onset drinkers, so that exposure to alcohol’s deleterious effects will be earlier, continue longer, and be most severe within a group that already is most vulnerable. Therefore, it is essential that researchers seek to confirm the findings of animal studies in humans, and indeed much of this work now is in progress.
Protective Factors
Like risk factors, protective factors can have functional influences at all levels of analysis from the biological to the broader contextual. Furthermore, although perhaps obvious, individuals, circumstances, and contexts associated with no or only low levels of risk by definition also are protective against a problematic outcome. For example, youth with more effective behavioral control capability are less likely to exhibit problem use in adolescence (Wong et al. 2006). Similarly, at the contextual level, social policies (e.g., zero-tolerance laws) can have a protective influence.
Even more important, however, are those personal or contextual attributes that can provide active insulation against risk. For instance, positive parenting has been associated with a later onset and lower levels of alcohol use among adolescents (Kumpfer and Alvarado 2003). Similarly, involvement with low- or nonusing peers, attending a college with no or low levels of alcohol consumption, or living in a dorm committed to nondrinking all have been related to lower levels of use and problem use (Wechsler and Nelson 2008). Although selection factors are one issue in determining residence (i.e., adolescents who already oppose drinking are most likely to choose a college or dorm committed to abstinence), other research indicates independent effects of context (Cranford et al. 2009). Religious involvement is another area where individual choice and context combine to protect against problem alcohol use. Thus, many studies have reported low-order negative relationships between religious involvement and alcohol use, with some of the effect being attributable to the cultivation of self-control and self-regulatory capacities (McCullough and Willoughby 2009).
A few studies have focused on another potentially highly important area—that is, resilience. Resilience is defined as the ability to avoid a pathological outcome, or achieve a successful one, despite the experience of adversity (Rutter 1987). In theory, biological, psychological, and social characteristics all can contribute to resilience. Despite the importance of this adaptation, very few studies have investigated this area and followed participants into late adolescence to identify problem outcomes. We are aware of only one study, albeit with a small sample, that has investigated biological factors contributing to resilience using functional magnetic resonance imaging (fMRI) to assess brain activity (Heitzeg et al. 2008). The study included COAs ages 16–20 years, who were divided into resilient subjects who had not developed alcohol problems by this time and vulnerable subjects who had developed such problems, as well as non-COA control subjects. The investigators exposed the participants to emotional stimuli and then measured brain activity in various areas. These analyses detected clear differences between resilient and vulnerable subjects in the activation of various brain areas.2 The activation pattern observed in the resilient COAs was consistent with an explanation that resilient youth have greater emotional monitoring capability, which is protective against excessive responding. In contrast, the vulnerable group displayed a pattern consistent with active suppression of affective responses, suggesting a possible deficit in the ability to engage adaptively with emotional stimuli. Clearly, this work is only a beginning effort at understanding the dynamics of resilient capability.
Screening, Prevention, and Treatment Programs for Underage Drinking and Problem Use
Screening
Because of the high rates of alcohol use, binge drinking, and AUDs among underage drinkers and young adults, increasing emphasis has been placed on screening for these difficulties in recent years. The goals of such screening are both to identify current or potential alcohol use problems and to initiate appropriate referral to prevent and treat these problems. Although the goals of screening appear relatively straightforward, the screening of adolescents and young adults for alcohol and other problem behaviors (e.g., other drug use, delinquency) still is in the nascent stages of development, and several issues currently are being addressed. Thus, investigators still need to determine the feasibility of screening for alcohol use in different research settings (e.g., primary-care physician offices, schools, juvenile justice settings), using different modes of administration (e.g., using self-report surveys/questionnaires versus computer-based approaches), using screening tools of different lengths and comprehensiveness (e.g., a few items specifically focusing on alcohol use versus a test battery assessing alcohol use, other drug use, and risk factors), and with different associated costs. For instance, primary-care physicians probably would not be receptive to asking a lengthy set of questions during adolescent checkups; likewise, if a screening survey were administered via a computer, the costs for the computer, software, training of participants completing the survey, and analyses of the data collected would have to be considered.
Currently, several well-developed alcohol screening tests for adolescents are available that have demonstrated high reliability and validity, including the Alcohol Use Disorders Identification Test (AUDIT), Problem-Oriented Screening Instrument for Teenagers (POSIT), and CRAFFT (Knight et al. 2003). These instruments vary in length and have been applied across a variety of adolescent settings. However, some of the feasibility issues discussed above still remain to be explored further, along with other practical issues (e.g., parental consent to administer a screening instrument) and the critical issue of how positive screens can be linked with appropriate referral resources. The health care, educational, and juvenile justice systems in the United States currently are not comprehensively equipped to address the range of adolescent and young adult alcohol use problems. Nevertheless, some recent initial findings from screening and brief intervention studies in hospital emergency rooms (Monti et al. 2007) and college student health centers (Fleming et al. 2010; Schaus et al. 2009) have demonstrated promising findings and may provide a platform for subsequent studies. The issue of screening, referral, and brief interventions is of sufficient prominence that NIAAA has formed a committee on the Assessment and Screening for Underage Drinking Risk as part of the larger Underage Drinking Initiative.
Prevention
The development of successful preventive interventions for underage and early young adult drinking is a challenging task for a variety of reasons, including the multiplicity of risk and protective factors that may vary in their influence across different developmental periods (e.g., early adolescence, young adulthood) and possibly for different sex and/or racial/ethnic groups. Nevertheless, a broad range of alcohol prevention programs have been developed that target different units or levels of analysis (e.g., school, family, individual), with some interventions targeting more than one level of analysis. For example, some intervention programs are school based and rely on social influences (e.g., peer refusal skills) or motivational enhancement principles and youth preference (Brown et al. 2005). Other programs focus on families and rely on strengthening parent–child ties to reduce alcohol use (Spoth et al. 2006). Still, others are aimed at high-risk youth or focus on social policy interventions (e.g., alcohol taxation, minimum legal drinking age, and zero-tolerance laws). Because of space constraints, the discussion here only describes some prominent universal preventive intervention programs.
Universal programs, which include all individuals in a particular population (e.g., all students in a school), are the most widely used form of preventive intervention for underage youth. The most common programs include classroom curricula administered to students within school settings, which may be supplemented with components to change the school-wide climate regarding alcohol use, parent programs, mass media programs, and community-wide interventions. Most universal interventions are based on the social-influence model, which suggests that the primary influences affecting youths’ AOD use behaviors are social factors, such as peer, family, and media influences (Bauman and Ennett 1996). Accordingly, these programs strive both to help adolescents acquire skills that will enable them to effectively resist social pressures (especially peer pressures) to use AODs and to promote social attitudes and norms that oppose AOD use. Most AOD prevention curricula for youth are administered during the late elementary and junior high-school years because AOD use often is initiated in this age period.
In a meta-analysis of 207 universal, school-based AOD prevention programs, Tobler and colleagues (2000) reported that interactive prevention programs (e.g., programs that encouraged social interactions with peers and focused on interpersonal skills, refusal skills, and changes in normative beliefs) yielded stronger outcomes in reducing alcohol use than those that were noninteractive (e.g., teachers providing knowledge to students about the effects of alcohol). Other characteristics of effective programs were a smaller number of participants (e.g., programs with 300 participants were more effective than those with a 1,000 participants), higher intensity (i.e., more delivery hours), and greater comprehensiveness with regard to changes at multiple levels (e.g., individual, parent, school, and community levels).
In a major review of extant preventive interventions focused on underage drinking, Spoth and colleagues (2009) identified 41 intervention studies that demonstrated some evidence of significant effects, or positive changes, in targeted alcohol use behaviors. Some of the most highly visible universal adolescent alcohol use preventive intervention programs were the community-wide Midwestern Prevention Project (Pentz et al. 1989), the community-wide Project Northland (Perry et al. 2000), and the family-focused Iowa Strengthening Families Program (Spoth et al. 2006). Although the specific alcohol outcome variables assessed by these programs have differed to some extent (e.g., delayed drinking initiation or reductions in current alcohol use), each program has reported successes in short- and medium-term posttest evaluations and in some instances in longer-term evaluations. In addition, for some of these programs there has been evidence of the generalizability of the interventions to different ethnic groups.
However, these quite positive and encouraging findings must be tempered by a range of methodological limitations and concerns that have been raised about universal preventive interventions to reduce underage alcohol use. For example, in the review by Spoth and colleagues (2009), only 127 of 400 studies examined provided sufficient data to evaluate the programs, and of these 127 programs, only 41 indicated any evidence of a significant effect. Thus, despite significant advances in the development, implementation, and evaluation of multidomain preventive interventions as well as of policy, legal, and environmentally focused interventions, a number of issues remain to be addressed. These include additional evaluations of the generalizability of findings to nonwhite populations and of the relative contributions of specific components of multidomain interventions, enhancement of dissemination plans, and quality assurance for the implementation of such evidence-based programs.
A review of individual-focused college-based prevention programs from 1999 to 2006 (Larimer and Cronce 2007) provided several important conclusions.
There was no evidence to support the usefulness of information-or knowledge-based prevention approaches; simply providing information about the dangers of drinking was not sufficient to produce any appreciable change in college students’ drinking behaviors.
There was evidence demonstrating the effectiveness of skills-based interventions, such as monitoring the amount of one’s drinking, setting limits on the amount consumed, and avoiding alcohol-related risky situations. Motivational interventions with personalized feedback also yielded positive findings with regard to reductions in alcohol use among college students.
Although significant progress has been made in recent years with regard to individual-focused college drinking prevention programs, additional studies are needed with stronger research designs, appropriate control groups, and retention of participants across the course of studies.
In addition to individual-focused college drinking programs, several policy-based prevention activities have been implemented on campuses to reduce alcohol use and associated problems. These include such policies as establishing alcohol-free residences and campuses, prohibiting beer kegs on campus, prohibiting the self-service of alcohol at campus events, and banning the marketing of alcohol on campus. Findings regarding the impact of these policies are limited, although some studies have demonstrated a reduction in binge drinking in AOD-free residences (Toomey and Wagenaar 2002). Similar to the findings for individual-focused college prevention programs, considerably more research is needed on the impact of university and community policies targeted at reducing alcohol use and alcohol problems among college students. (For more information on college drinking and related problems, see the article by Hingson, pp. 45–54.)
Treatment
A large number of different inpatient and outpatient therapies have been used with underage drinkers, including the 12-step model, behavioral interventions, family therapy, and educational and vocational assistance and rehabilitation. Among the most widely used inpatient approach is the 28-day, group-oriented Minnesota model that uses the 12-step program of recovery (Wheeler and Malmquist 1987). This program includes different components, such as group meetings, educational presentations about alcoholism and associated health and social problems, group counseling, family therapy, and the completion of workbook assignments to instill personal monitoring of progress in the program. The multiple components of this approach are designed to increase personal resources and resolve family problems to increase the prospects of recovery.
Whereas the Minnesota model is based on an inpatient program, most of the existing research on treatment for underage drinkers has been conducted on outpatient programs. Some therapies and approaches, such as cognitive–behavior therapy, have been used with some success to foster recovery among adolescents in treatment (Deas and Clark 2009). However, across these different treatment modalities, effect sizes (i.e., the strength or magnitude of the intervention effect) have been small and the relapse rates within 9 months as high as those of adults (Brown et al. 1994). Finally, although several medications have been approved by the U.S. Food and Drug Administration for the treatment of alcohol dependence in adults, there have been few applications of these medications to adolescents.
Thus, despite the very high rates of alcohol use, binge drinking, and AUDs among underage drinkers, the service delivery system has been lacking in addressing this serious public health issue. Research in the areas of service delivery and treatment has lagged and is compounded by difficulties in addressing the multiple problems (e.g., AOD use, delinquency, academic difficulties) of this high-risk population. Future research in adolescent treatment would benefit from a model that incorporates an understanding of developmental features of adolescence (e.g., critical transitions and the timing and sequence of changes) and of how adolescent assets can be used to increase the magnitude of effects for the treatments, improve the relapse rates, and improve the dissemination of evidenced-based treatments.
Summary and Conclusions
In the 40 years since NIAAA began, the attention to the interval prior to adulthood has steadily increased. Thus, this developmental period has become recognized as an interval during which much of the risk for later alcohol problems and alcoholism begins to emerge, and when the developmental patterning for later disorder begins to consolidate. At the same time, appreciation has deepened about the significance of adolescence and young adulthood as a major playing field in its own right, within which heavy consumption occurs and where great immediate risk exists for damage to self and others. This article has provided a brief overview of research from both of these perspectives, summarizing the epidemiologic evidence, reviewing the importance of social policy as a “shaper” of drinking patterns, and providing a brief snapshot of the many ways that developmental markers both prior to drinking and in the early drinking years can indicate risk for drinking problems and even for emerging AUDs. As described in this overview, over the past 40 years substantial progress has been made in the areas of etiology, screening, preventive interventions, and treatment regarding underage and young adult drinking. The increasing maturity of the field is evidenced by the current interdisciplinary, multilevel research integrating social, behavioral, and biological levels of analysis to understand mechanisms of risk and protection. Furthermore, sophisticated methods of applied research are being used to develop new screening methods for early identification of risk as well as more effective, multisystemic programs for prevention and intervention. Although the past 40 years have provided a rich yield of new research findings on underage and young adult drinking that has been translated into saving many lives, there remain many critical issues to be addressed, which highlight NIAAA’s central role and the need for continued involvement in reducing underage and young adult drinking.
Footnotes
Binge drinking was defined as having five or more drinks in a row.
Resilient subjects showed more activation of the orbital frontal gyrus (OFG) on both sides of the brain as well as in the left insula/putamen than did control and vulnerable subjects. In contrast, the vulnerable group exhibited greater activation of dorsomedial prefrontal cortex and less activation of ventral striatum and extended amygdala, bilaterally, than did either control or resilient groups; moreover, these subjects exhibited more externalizing behavior.
Financial Disclosure
The authors declare that they have no competing financial interests.
References
- Bachman JG, Johnston LD, O’Malley PM, Schulenberg J. Transitions in drug use during late adolescence and young adulthood. In: Graber JA, Brooks-Gunn J, Petersen AC, editors. Transitions Through Adolescence: Interpersonal Domains and Context. Hillsdale, NJ, England: Lawrence Erlbaum Associates; 1996. pp. 111–140. [Google Scholar]
- Bank BJ, Biddle B, Anderson DS, et al. Comparative research on the social determinants of adolescent drinking. Social Psychology Quarterly. 1985;48(2):164–177. [Google Scholar]
- Bauman KE, Ennett ST. On the importance of peer influence for adolescent drug use: Commonly neglected considerations. Addiction. 1996;91:185–198. [PubMed] [Google Scholar]
- Blane HT, Chafetz ME. Youth: Alcohol and Social Policy. New York, NY: Plenum Press; 1979. [Google Scholar]
- Blomberg RD. Lower Legal BAC Limits for Youth: Evaluation of the Maryland 0.02 Law. Washington, DC: U.S. Department of Transportation; 1992. (Report DOT HS–806–807). [Google Scholar]
- Bogg T, Finn PR. A self-regulatory model of behavioral disinhibition in late adolescence: Integrating personality traits, externalizing psychopathology, and cognitive capacity. Journal of Personality. 2010;78(2):441–470. doi: 10.1111/j.1467-6494.2010.00622.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA, Anderson KG, Schulte MT, et al. Facilitating youth self-change through school-based intervention. Addictive Behaviors. 2005;30(9):1797–1810. doi: 10.1016/j.addbeh.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Brown SA, Gleghorn A, Schuckit MA, et al. Conduct disorder among adolescent alcohol and drug abusers. Journal of Studies on Alcohol. 1996;57(3):314–324. doi: 10.15288/jsa.1996.57.314. [DOI] [PubMed] [Google Scholar]
- Brown SA, McGue M, Maggs J, et al. A developmental perspective on alcohol and youths 16 to 20 years of age. Pediatrics. 2008;121(Suppl. 4):S290–S310. doi: 10.1542/peds.2007-2243D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA, Myers MG, Mott MA, Vik PW. Correlates of success following treatment for adolescent substance abuse. Applied Prevention Psychology. 1994;3(2):61–73. [Google Scholar]
- Buu A, DiPiazza C, Wang J, et al. Parent, family, and neighborhood effects on the development of child substance use and other psychopathology from preschool to the start of adulthood. Journal of Studies on Alcohol and Drugs. 2009;70(4):489–498. doi: 10.15288/jsad.2009.70.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buu A, Mansour M, Wang J, et al. Alcoholism effects on social migration and neighborhood effects on alcoholism over the course of 12 years. Alcoholism: Clinical and Experimental Research. 2007;31(9):1545–1551. doi: 10.1111/j.1530-0277.2007.00449.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey BJ, Tottenham N, Fossella J. Clinical, imaging, lesion, and genetic approaches toward a model of cognitive control. Developmental Psychobiology. 2002;40(3):237–254. doi: 10.1002/dev.10030. [DOI] [PubMed] [Google Scholar]
- Center for Substance Abuse Research 45% of young drinkers ages 12 to 14 get alcohol free from adult family members or take from home [article online], 2008. Adapted by CESAR from SAMSHA, Office of Applied Studies, Underage Alcohol Use: Findings from the 2002–2006 National Surveys on Drug Use and Health, 2008. Available at: http://www.oas.samhsa.gov/underage2k8/underage.pdf. Accessed March 10, 2009.
- Centers for Disease Control and Prevention YRBSS: National Youth Risk Behavior Survey: 1991–2005: Trends in the prevalence of alcohol use [article online], 2005. Available at: http://www.cdc.gov/HealthyYouth/yrbs/pdf/trends/2005_YRBS_Alcohol_Use.pdf (03/22/07). Accessed June 15, 2007.
- Cicchetti D. Development and psychopathology. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology. Vol. 1: Theory and Method. 2nd ed. Hoboken, NJ: John Wiley & Sons; 2006. pp. 1–23. [Google Scholar]
- Clark DB, Cornelius JR, Kirisci L, Tarter RE. Childhood risk categories for adolescent substance involvement: A general liability typology. Drug and Alcohol Dependence. 2005;77(1):13–21. doi: 10.1016/j.drugalcdep.2004.06.008. [DOI] [PubMed] [Google Scholar]
- Clark DB, Thatcher DL, Tapert SF. Alcohol, psychological dysregulation, and adolescent brain development. Alcoholism: Clinical and Experimental Research. 2008;32(3):375–385. doi: 10.1111/j.1530-0277.2007.00601.x. [DOI] [PubMed] [Google Scholar]
- Cranford JA, McCabe SE, Boyd CJ, et al. Effects of residential learning communities on drinking trajectories during the first two years of college. Journal on Studies of Alcohol and Drugs. 2009;(Suppl. 16):86–95. doi: 10.15288/jsads.2009.s16.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham RM, Walton MA, Goldstein A, et al. Three-month follow-up of brief computerized and therapist interventions for alcohol and violence among teens. Academic Emergency Medicine. 2009;16(11):1193–1207. doi: 10.1111/j.1553-2712.2009.00513.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deas D, Clark A. Current state of treatment for alcohol and other drug use disorders in adolescents. Alcohol Research & Health. 2009;32(1):76–82. [PMC free article] [PubMed] [Google Scholar]
- Dick DM, Bierut LJ. The genetics of alcohol dependence. Current Psychiatry Reports. 2006;8(2):151–157. doi: 10.1007/s11920-006-0015-1. [DOI] [PubMed] [Google Scholar]
- Dick DM, Bierut L, Hinrichs A, et al. The role of GABARA2 in risk for conduct disorder and alcohol and drug dependence across developmental stages. Behavior Genetics. 2006;36(4):577–590. doi: 10.1007/s10519-005-9041-8. [DOI] [PubMed] [Google Scholar]
- Dick DM, Latendresse SJ, Lansford JE, et al. Role of GABRA2 in trajectories of externalizing behavior across development and evidence of moderation by parental monitoring. Archives of General Psychiatry. 2009;66(6):649–657. doi: 10.1001/archgenpsychiatry.2009.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge KA, Malone PS, Lansford JE, et al. A dynamic cascade model of the development of substance-use onset. Monographs of the Society for Research in Child Development. 2009;74(3):vii–119. doi: 10.1111/j.1540-5834.2009.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donovan JE, Jessor R. Structure of problem behavior in adolescence and young adulthood. Journal of Consulting and Clinical Psychology. 1985;53(6):890–904. doi: 10.1037//0022-006x.53.6.890. [DOI] [PubMed] [Google Scholar]
- Donovan JE, Molina BS. Children’s introduction to alcohol use: Sips and tastes. Alcoholism: Clinical and Experimental Research. 2008;32(1):108–119. doi: 10.1111/j.1530-0277.2007.00565.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubow EF, Boxer P, Huesmann LR. Childhood and adolescent predictors of early and middle adulthood alcohol use and problem drinking: The Columbia County Longitudinal Study. Addiction. 2008;103(Suppl. 1):36–47. doi: 10.1111/j.1360-0443.2008.02175.x. [DOI] [PubMed] [Google Scholar]
- Fleming MF, Balousek SL, Grossberg PM, et al. Brief physician advice for heavy drinking college students: A randomized controlled trial in college health clinics. Journal of Studies on Alcohol and Drugs. 2010;71(1):23–31. doi: 10.15288/jsad.2010.71.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster SE, Vaughan RD, Foster WH, Califano JA. Estimate of the commercial value of underage drinking and adult abusive and dependent drinking to the alcohol industry. Archives of Pediatrics & Adolescent Medicine. 2006;160(5):473–478. doi: 10.1001/archpedi.160.5.473. [DOI] [PubMed] [Google Scholar]
- Gogtay N, Giedd JN, Lusk L, et al. Dynamic mapping of human cortical development during childhood through early adulthood. The Proceedings of the National Academy of Sciences of the United States of America. 2004;101(21):8174–8179. doi: 10.1073/pnas.0402680101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotham HJ, Sher KJ, Wood PK. Alcohol involvement and developmental task completion during young adulthood. Journal of Studies on Alcohol. 2003;64(1):32–42. doi: 10.15288/jsa.2003.64.32. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: Results from the National Longitudinal Alcohol Epidemiologic Survey. Journal of Substance Abuse. 1997;9:103–110. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Age of onset of drug use and its association with DSM-IV drug abuse and dependence: Results from the National Longitudinal Alcohol Epidemiologic Survey. Journal of Substance Abuse. 1998;10(2):163–173. doi: 10.1016/s0899-3289(99)80131-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, et al. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug and Alcohol Dependence. 2004;74(3):223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003;71(1):7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Greenfield TK, Rogers JD. Who drinks most of the alcohol in the U.S.? The policy implications. Journal of Studies on Alcohol. 1999;60:78–89. doi: 10.15288/jsa.1999.60.78. [DOI] [PubMed] [Google Scholar]
- Guo J, Hawkins JD, Hill KG, Abbott RD. Childhood and adolescent predictors of alcohol abuse and dependence in young adulthood. Journal of Studies on Alcohol. 2001;62(6):754–762. doi: 10.15288/jsa.2001.62.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heitzeg MM, Nigg JT, Yau WY, et al. Affective circuitry and risk for alcoholism in late adolescence: Differences in frontostriatal responses between vulnerable and resilient children of alcoholic parents. Alcoholism: Clinical and Experimental Research. 2008;32(3):414–426. doi: 10.1111/j.1530-0277.2007.00605.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HHS Press Office Acting Surgeon General Issues National Call to Action on Underage Drinking. 2007. [article online], Available at: http://www.hhs.gov/news/press/2007pres/20070306.html. Accessed May 6, 2010.
- Jessor R, Jessor SL. Problem Behavior and Psychosocial Development: A Longitudinal Study of Youth. New York, NY: Academic Press; 1977. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future National Survey Results on Drug Use, 1975–2008: Volume I, Secondary School Students. Bethesda, MD: National Institute on Drug Abuse; 2009. (NIH Publication No. 09–7402). [Google Scholar]
- Kandel DB, editor. Longitudinal Research on Drug Use: Empirical Findings and Methodological Issues. Washington, DC: Hemisphere; 1978. [Google Scholar]
- Kandel DB. Issues of sequencing of adolescent drug use and other problem behaviors. Drugs and Society. 1989;3:59–80. [Google Scholar]
- Kendler KS, Prescott CA. Genes, Environment, and Psychopathology: Understanding the Causes of Psychiatric and Substance Use Disorders. New York, NY: Guilford Press; 2006. [Google Scholar]
- Kissin B, Begleiter H, editors. The Biology of Alcoholism: Volumes 1–3. New York: Plenum; 1972. [Google Scholar]
- Kissin B, Begleiter H, editors. The Biology of Alcoholism: Volumes 4–5. New York: Plenum; 1976. [Google Scholar]
- Knight JR, Sherritt L, Harris SK, et al. Validity of brief alcohol screening tests among adolescents: A comparison of the AUDIT, POSIT, CAGE, and CRAFFT. Alcoholism: Clinical and Experimental Research. 2003;27(1):67–73. doi: 10.1097/01.ALC.0000046598.59317.3A. [DOI] [PubMed] [Google Scholar]
- Kumpfer KL, Alvarado R. Family-strengthening approaches for the prevention of youth problem behaviors. American Psychologist. 2003;58(6–7):457–465. doi: 10.1037/0003-066X.58.6-7.457. [DOI] [PubMed] [Google Scholar]
- Larimer ME, Cronce JM. Identification, prevention, and treatment revisited: Individual-focused college drinking prevention strategies 1999–2006. Addictive Behaviors. 2007;32(11):2439–2468. doi: 10.1016/j.addbeh.2007.05.006. [DOI] [PubMed] [Google Scholar]
- Leonard KE. Alcohol and substance abuse in marital violence and child maltreatment. In: Wekerle C, Wall AM, editors. The Violence and Addiction Equation: Theoretical and Clinical Issues in Substance Abuse and Relationship Violence. New York, NY: Brunner-Routledge; 2002. pp. 194–219. [Google Scholar]
- Li TK. Alcohol Abuse Increases, Dependence Declines Across Decade Young Adult Minorities Emerge As High-Risk Subgroups. Jun 10, 2004. NIH News. [Google Scholar]
- Loukas A, Fitzgerald HE, Zucker RA, von Eye A. Parental alcoholism and co-occurring antisocial behavior: Prospective relationships to externalizing behavior problems in their young sons. Journal of Abnormal Child Psychology. 2001;29(2):91–106. doi: 10.1023/a:1005281011838. [DOI] [PubMed] [Google Scholar]
- Loukas A, Zucker RA, Fitzgerald HE, Krull JL. Developmental trajectories of disruptive behavior problems among sons of alcoholics: Effects of parent psychopathology, family conflict, and child undercontrol. Journal of Abnormal Psychology. 2003;112(1):119–131. [PubMed] [Google Scholar]
- Maggs JL. Alcohol use and binge drinking as goal-directed action during the transition to post-secondary education. In: Schulenberg J, Maggs JL, Hurrelmann K, editors. Health Risks and Developmental Transitions During Adolescence. New York, NY: Cambridge University Press; 1997. pp. 345–371. [Google Scholar]
- Masten AS, Faden VB, Zucker RA, Spear LP. Underage drinking: A developmental framework. Pediatrics. 2008;121(Suppl. 4):S235–S251. doi: 10.1542/peds.2007-2243A. [DOI] [PubMed] [Google Scholar]
- Masten AS, Roisman GI, Long JD, et al. Developmental cascades: Linking academic achievement and externalizing and internalizing symptoms over 20 years. Developmental Psychology. 2005;41(5):733–746. doi: 10.1037/0012-1649.41.5.733. [DOI] [PubMed] [Google Scholar]
- McCullough ME, Willoughby BL. Religion, self-regulation, and self-control: Associations, explanations, and implications. Psychological Bulletin. 2009;135(1):69–93. doi: 10.1037/a0014213. [DOI] [PubMed] [Google Scholar]
- McGue M, Iacono WG, Legrand LN, et al. Origins and consequences of age at first drink: I. associations with substance-use disorders, disinhibitory behavior and psychopathology, and P3 amplitude. Alcoholism: Clinical and Experimental Research. 2001;25(8):1156–1165. [PubMed] [Google Scholar]
- McGue M. The behavioral genetics of alcoholism. Current Directions in Psychological Science. 1999;8:109–115. [Google Scholar]
- Miller TR, Levy DT, Spicer RS, Taylor DM. Societal costs of underage drinking. Journal of Studies on Alcohol. 2006;67(4):519–528. doi: 10.15288/jsa.2006.67.519. [DOI] [PubMed] [Google Scholar]
- Monti PM, Barnett NP, Colby SM, et al. Motivational interviewing versus feedback only in emergency care for young adult problem drinking. Addiction. 2007;102(8):1234–1243. doi: 10.1111/j.1360-0443.2007.01878.x. [DOI] [PubMed] [Google Scholar]
- National Academy of Sciences 2004. Report brief: Reducing underage drinking: A collective responsibility [article online], Available at: http://www.iom.edu/Object.File/Master/19/780/ReducingUnderageDrinking.pdf (03/22/07). Accessed March 10, 2007.
- National Institute on Alcohol Abuse and Alcoholism Changing the culture of campus drinking [article online], 2002. Alcohol Alert. Oct, 2002. Available at: http://pubs.niaaa.nih.gov/publications/aa58.htm. Accessed March 10, 2006.
- National Institute on Alcohol Abuse and Alcoholism Research findings on underage drinking and the minimum legal drinking age [article online] 2008. Available at: http://www.niaaa.nih.gov/AboutNIAAA/NIAAASponsoredPrograms/drinkingage.htm. Accessed January 10, 2009.
- Norberg KE, Bierut LJ, Grucza RA. Long-term effects of minimum drinking age laws on past-year alcohol and drug use disorders. Alcoholism: Clinical and Experimental Research. 2009;33(12):2180–2190. doi: 10.1111/j.1530-0277.2009.01056.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Malley PM, Wagenaar AC. Effects of minimum drinking age laws on alcohol use, related behaviors and traffic crash involvement among American youth: 1976–1987. Journal of Studies on Alcohol. 1991;52(5):478–491. doi: 10.15288/jsa.1991.52.478. [DOI] [PubMed] [Google Scholar]
- Pentz MA, Dwyer JH, MacKinnon DP, et al. A multi-community trial for primary prevention of adolescent drug abuse: Effects on drug use prevalence. JAMA: Journal of the American Medical Association. 1989;261:3259–3266. [PubMed] [Google Scholar]
- Perry CL, Williams CL, Komro KA, et al. Project Northland high school interventions: Community action to reduce adolescent alcohol use. Health Education & Behavior. 2000;27:29–49. doi: 10.1177/109019810002700105. [DOI] [PubMed] [Google Scholar]
- Pickrell TM. Driver alcohol involvement in fatal crashes by age group and vehicle type [article online] 2006. Available at: www.nrd.nhtsa.dot.gov/pdf/nrd-30/NCSA/RNotes/2006/810598.pdf. Accessed August 30, 2007.
- Popham RE, editor. Alcohol and Alcoholism. Toronto, Canada: University of Toronto Press/Addiction Research Foundation; 1970. [Google Scholar]
- Pulido C, Anderson KG, Armstead AG, et al. Family history of alcohol-use disorders and spatial working memory: Effects on adolescent alcohol expectancies. Journal of Studies on Alcohol and Drugs. 2009;70(1):87–91. doi: 10.15288/jsad.2009.70.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts LJ, Linney KD. Alcohol problems and couples: Drinking in an intimate relational context. In: Schmaling KB, Sher TG, editors. The Psychology of Couples and Illness: Theory, Research, and Practice. Washington, DC: American Psychological Association; 2000. pp. 269–310. [Google Scholar]
- Robins LN, Przybeck TR. Age of onset of drug use as a factor in drug and other disorders. In: Jones C, Battjes R, editors. Etiology of Drug Abuse: Implications for Prevention. Rockville, MD: National Institute on Drug Abuse (NIDA); 1985. pp. 178–192. (NIDA Research Monograph56). [PubMed] [Google Scholar]
- Russell M. Prevalence of alcoholism among children of alcoholics. In: Windle M, Searles JS, editors. Children of Alcoholics: Critical Perspectives. New York, NY: Guilford Press; 1990. pp. 9–38. [Google Scholar]
- Rutter M. Psychosocial resilience and protective mechanisms. American Journal of Orthopsychiatry. 1987;57(3):316–331. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- Schaus JF, Sole ML, McCoy TP, et al. Alcohol screening and brief intervention in a college student health center: A randomized controlled trial. Journal of Studies on Alcohol and Drugs. 2009;(Suppl. 16):131–141. doi: 10.15288/jsads.2009.s16.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuckit MA, Smith TL, Anderson KG, Brown SA. Testing the level of response to alcohol: Social information processing model of alcoholism risk: A 20-year prospective study. Alcoholism: Clinical and Experimental Research. 2004;28(12):1881–1889. doi: 10.1097/01.alc.0000148111.43332.a5. [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, Maggs JL. Destiny matters: Distal developmental influences on adult alcohol use and abuse. Addiction. 2008;103(Suppl. 1):1–6. doi: 10.1111/j.1360-0443.2008.02172.x. [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, O’Malley PM, Bachman JG, et al. Getting drunk and growing up: Trajectories of frequent binge drinking during the transition to young adulthood. Journal of Studies on Alcohol. 1996;57(3):289–304. doi: 10.15288/jsa.1996.57.289. [DOI] [PubMed] [Google Scholar]
- Shults RA, Elder RW, Sleet DA, et al. Reviews of evidence regarding interventions to reduce alcohol-impaired driving. American Journal of Preventive Medicine. 2001;21(Suppl. 4):66–88. doi: 10.1016/s0749-3797(01)00381-6. [DOI] [PubMed] [Google Scholar]
- Spear LP. The adolescent brain and age-related behavioral manifestations. Neuroscience and Biobehavioral Reviews. 2000;24(4):417–463. doi: 10.1016/s0149-7634(00)00014-2. [DOI] [PubMed] [Google Scholar]
- Spoth R, Greenberg M, Turrisi R. Overview of preventive interventions addressing underage drinking. Alcohol Research & Health. 2009;32(1):53–66. [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Shin C, Guyll M, et al. Universality of effects: An examination of the comparability of long-term family intervention effects on substance use across risk-related subgroups. Prevention Science. 2006;7:209–224. doi: 10.1007/s11121-006-0036-3. [DOI] [PubMed] [Google Scholar]
- Stice E, Myers MG, Brown SA. Relations of delinquency to adolescent substance use and problem use: A prospective study. Psychology of Addictive Behaviors. 1998;12(2):136–146. [Google Scholar]
- Subramanian R. Motor vehicle traffic crashes as a leading cause of death in the United States [article online] 2003. Traffic Safety Facts Research Note. Available at: http://www-nrd.nhtsa.dot.gov/pdf/nrd-30/NCSA/RNotes/2006/810568.pdf. Accessed March 27, 2007.
- Substance Abuse and Mental Health Services Administration, Office of Applied Studies. National Survey on Drug Use and Health, [article online], 2006. Available at: http://www.drugabusestatistics.samhsa.gov/nsduh.htm. Accessed March 23, 2007.
- Substance Abuse and Mental Health Services Administration, Office of Applied Studies . Results from the 2002 National Survey on Drug Use and Health: National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2003. (NHSDA Series H–22, DHHS publication no. SMA 03–3836). [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Results from the 2003 National Survey on Drug Use and Health: National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2004. (Office of Applied Studies, NSDUH Series H–25, DHHS publication no. SMA 04–3964). [Google Scholar]
- Timberlake DS, Hopfer CJ, Rhee SH, et al. College attendance and its effect on drinking behaviors in a longitudinal study of adolescents. Alcoholism: Clinical and Experimental Research. 2007;31(6):1020–1030. doi: 10.1111/j.1530-0277.2007.00383.x. [DOI] [PubMed] [Google Scholar]
- Tobler NS, Roona MR, Ochshorn P, et al. School-based adolescent drug prevention programs: 1998 meta-analysis. Journal of Primary Prevention. 2000;20:275–336. [Google Scholar]
- Toomey TL, Wagenaar AC. Environmental policies to reduce college drinking: Options and research findings. Journal of Studies on Alcohol. 2002;(Suppl. 14):193–205. doi: 10.15288/jsas.2002.s14.193. [DOI] [PubMed] [Google Scholar]
- Voas RB, Tippetts AS, Fell JC. Assessing the effectiveness of minimum legal drinking age and zero tolerance laws in the United States. Accident Analysis and Prevention. 2003;35(4):579–587. doi: 10.1016/s0001-4575(02)00038-6. [DOI] [PubMed] [Google Scholar]
- Wagenaar AC, Toomey TL. Effects of minimum drinking age laws: Review and analyses of the literature from 1960 to 2000. Journal of Studies on Alcohol. 2002;(Suppl. 14):206–225. doi: 10.15288/jsas.2002.s14.206. [DOI] [PubMed] [Google Scholar]
- Wagenaar AC, O’Malley PM, LaFond C. Lowered legal blood alcohol limits for young drivers: Effects on drinking, driving, and driving-after-drinking behaviors in 30 states. American Journal of Public Health. 2001;91(5):801–804. doi: 10.2105/ajph.91.5.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler H, Nelson TF. What we have learned from the Harvard School of Public Health College Alcohol Study: Focusing attention on college student alcohol consumption and the environmental conditions that promote it. Journal of Studies on Alcohol and Drugs. 2008;69(4):481–490. doi: 10.15288/jsad.2008.69.481. [DOI] [PubMed] [Google Scholar]
- Wheeler K, Malmquist J. Treatment approaches in adolescent chemical dependency. Pediatric Clinics of North America. 1987;34(2):437–447. doi: 10.1016/s0031-3955(16)36225-3. [DOI] [PubMed] [Google Scholar]
- Wills TA, Cleary SD. Peer and adolescent substance use among 6th–9th graders: Latent growth analyses of influence versus selection mechanisms. Health Psychology. 1999;18(5):453–463. doi: 10.1037//0278-6133.18.5.453. [DOI] [PubMed] [Google Scholar]
- Windle M, Scheidt DM. Alcoholic subtypes: Are two sufficient? Addiction. 2004;99(12):1508–1519. doi: 10.1111/j.1360-0443.2004.00878.x. [DOI] [PubMed] [Google Scholar]
- Windle M, Mun EY, Windle RC. Adolescent-to-young adulthood heavy drinking trajectories and their prospective predictors. Journal of Studies on Alcohol. 2005;66(3):313–322. doi: 10.15288/jsa.2005.66.313. [DOI] [PubMed] [Google Scholar]
- Windle M, Spear LP, Fuligni AJ, et al. Transitions into underage and problem drinking: Developmental processes and mechanisms between 10 and 15 years of age. Pediatrics. 2008;121(Suppl. 4):S273–S289. doi: 10.1542/peds.2007-2243C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MM, Brower KJ, Fitzgerald HE, Zucker RA. Sleep problems in early childhood and early onset of alcohol and other drug use in adolescence. Alcoholism: Clinical and Experimental Research. 2004;28(4):578–587. doi: 10.1097/01.alc.0000121651.75952.39. [DOI] [PubMed] [Google Scholar]
- Wong MM, Nigg JT, Zucker RA, et al. Behavioral control and resiliency in the onset of alcohol and illicit drug use: A prospective study from preschool to adolescence. Child Development. 2006;77(4):1016–1033. doi: 10.1111/j.1467-8624.2006.00916.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker RA. Alcohol use and the alcohol use disorders: A developmental-biopsychosocial systems formulation covering the life course. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology. 2nd ed. New York: Wiley; 2006. pp. 620–656. Vol. 3. Risk, Disorder and Adaptation. [Google Scholar]
- Zucker RA, Nigg J, Heitzeg M. Parsing the undercontrol/disinhibition pathway to substance use disorders: A multilevel developmental problem. Child Development Perspectives. 2010 doi: 10.1111/j.1750-8606.2011.00172.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]