Abstract
Among cluster analytic studies of the personality profiles associated with bulimia nervosa, a group of individuals characterized by emotional lability and behavioral dysregulation (i.e., a dysregulated cluster) has emerged most consistently. However, previous studies have all been cross-sectional and mostly used clinical samples. This study aimed to replicate associations between the dysregulated personality cluster and bulimic symptoms and related characteristics using a longitudinal, population-based sample. Participants were females assessed at ages 17 and 25 from the Minnesota Twin Family Study, clustered based on their personality traits. The Dysregulated cluster was successfully identified at both time points and was more stable across time than either the Resilient or Sensation Seeking clusters. Rates of bulimic symptoms and related behaviors (e.g., alcohol use problems) were also highest in the dysregulated group. Findings suggest that the dysregulated cluster is a relatively stable and robust profile that is associated with bulimic symptoms.
Keywords: personality cluster, bulimic behaviors, stability
Women with bulimia nervosa (BN) tend to exhibit very heterogeneous personality characteristics (Westen, Thompson-Brenner, & Peart, 2006). One approach to this dilemma is to use cluster analytic techniques to identify subgroups of women with similar personality profiles. The identification of separate “personality types” can help researchers formulate hypotheses about the etiology of eating disorders and possibly inform treatment decisions as personality type membership might impact the effectiveness of treatments. Indeed, studies have indicated that clustering provides incremental validity over and above eating disorder diagnoses in terms of predicting disordered eating symptoms, adaptive functioning, and illness severity (Thompson-Brenner & Westen, 2005; Westen & Harnden-Fischer, 2001).
Different studies using the profiling approach have been relatively consistent with regard to finding similar personality clusters of women with eating disorders (Claes et al., 2006; Espelage, Mazzeo, Sherman, & Thompson, 2002; Goldner, Srikameswaran, Schroeder, Livesley, & Birmingham, 1999; Thompson-Brenner & Westen, 2005; Thompson-Brenner, Eddy, Satir, Boisseau, & Westen, 2008; Wagner et al., 2006; Westen & Harnden-Fischer, 2001; Wildes et al., 2011; Wonderlich et al, 2005). One of the most consistent clusters is the dysregulated profile (e.g., emotionally dysregulated/undercontrolled cluster; Westen & Harnden-Fischer, 2001), characterized by high impulsivity and behavioral dysregulation. This cluster has been identified across different samples, with different personality measures (Claes et al., 2006; Goldner et al., 1999; Espelage et al., 2002; Wildes et al., 2011), and in different developmental periods (Thompson-Brenner et al., 2008; Westen & Harnden-Fischer, 2001). Notably, in several studies, the dysregulated cluster exhibited higher rates of bulimic behaviors compared to the other clusters (Claes et al., 2006; Perkins, Slane & Klump, in preparation; Westen & Harnden-Fischer, 2001; Wildes et al., 2011), suggesting that the dysregulated cluster is particularly salient for understanding BN.
Despite the frequent replication of the dysregulated cluster, there are some limitations of past research. First, although the dysregulated cluster has been identified among samples of adolescents and adults with eating disorders, the longitudinal stability of cluster membership from adolescence into adulthood is largely unknown. There have been a few studies examining cluster stability in population-based samples of adolescents with findings that personality profiles were “relatively unstable” during this time (Meeus, Van de Schoot, Klimstra, & Branje, 2011). However, not only have studies not examined stability into adulthood, but they have also not included information about associations with BN across time. Knowledge of whether there is longitudinal stability into adulthood, and information about associations with bulimic pathology across development, would provide much needed justification for efforts aimed at examining etiological associations between personality clusters and BN (e.g., Wonderlich et al., 2005). Second, all previous cluster analytic studies examining BN have used clinical samples of women. Replications in population-based samples would suggest that findings are generalizable and informative for non-clinical levels of bulimic behaviors, which are far more common in the population than eating disorder diagnoses (Neumark-Sztainer & Hannan, 2000).
Given all of the above, we conducted a longitudinal, population-based study of associations between the dysregulated cluster and bulimic behaviors in a large sample of females followed from late adolescence into young adulthood. We first identified the dysregulated cluster at each developmental period and examined its stability across the transition from adolescence into young adulthood. We then examined associations between the cluster and BN symptoms as well as several characteristics that have been found to be associated with BN and the dysregulated cluster (i.e., alcohol use disorder symptoms, depressive and anxiety symptoms, behavioral disinhibition, and DSM-IV diagnoses). Cross-sectional as well as longitudinal associations were evaluated in these analyses in order to assess the invariance of associations across development.
METHOD
Participants
Participants included an archival, convenience sample of female twins from the Minnesota Twin Family Study (MTFS). The MTFS is a population-based, longitudinal study of same-sex female twins and their parents. A detailed description of study recruitment and assessments can be found elsewhere (Iacono, Carlson, Taylor, Elkins, & McGue, 1999). The current study used cross-sectional and longitudinal data from two cohorts in the MTFS. Both cohorts were assessed at ages 17 (M = 17.87; SD = 0.74) and 25 (M = 25.04; SD = 0.69) years, but they began the studies at different ages and times. Cohort 1 began the study when they were 11 years old, whereas cohort 2 began the study at age 17. Due to some missing data at each time point as well as removal of outliers prior to data analysis, sample sizes differed across the age groups as follows: 1,264 females at age 17 and 1,184 females at age 25.1
Measures
Multidimensional Personality Questionnaire
The Multidimensional Personality Questionnaire (MPQ; Tellegen, 1982) was used to assess personality characteristics at ages 17 and 25. The MPQ is a198-item self-report, true-false questionnaire measuring personality characteristics on 11 facet scales. These scales include Well Being, Social Potency, Achievement, Social Closeness, Stress Reaction, Alienation, Aggression, Control, Harm Avoidance, Traditionalism, and Absorption. Internal consistency for the MPQ scales are usually acceptable with alphas for the 11 primary scales ranging from .76 to .90 (Tellegen, 1982). One-month test-retest stability coefficients ranged from .82 to .92 (Tellegen, 1982). In the present sample, internal consistency ranged from .79 to .91, depending on the facet scale examined. Notably, the MPQ is useful for examining personality in population-based samples, as it was developed and standardized with nonclinical groups (Krueger, Caspi, & Moffitt, 2000). Further, in previous research, MPQ measured personality traits have shown moderate stability from adolescence into adulthood (Blonigen, Carlson, Hicks, Krueger, & Iacono, 2008; Hopwood et al., 2011; McGue, Bacon, & Lykken, 1993; Roberts, Caspi, & Moffitt, 2001).
Bulimia Nervosa Symptoms
Bulimic behaviors were assessed at both time points using the Minnesota Eating Behavior Survey (MEBS; von Ranson, Klump, Iacono, & McGue, 2005)2 This 30-item true/false self-report questionnaire assesses overall levels of eating pathology as well as specific disordered eating symptoms including body dissatisfaction (i.e., dissatisfaction with one’s size or shape), binge eating (i.e., thoughts about overeating or the tendency to binge eat) compensatory behaviors (i.e., the use of compensatory behaviors such as self-induced vomiting, diuretics, etc. for weight loss), and weight preoccupation (i.e., preoccupation with dieting, thinness, and weight). Given the low prevalence BN (i.e., 1–3%; American Psychiatric Association, 2000), the MEBS was utilized as it maximized variability within the sample.
The internal consistency of the MEBS subscales has been shown to be adequate in samples of females ages 17 (α = .65–.89) and 20 years old (α = .68–89) (Klump, McGue, & Iacono, 2000; von Ranson et al., 2005) in previous studies. The MEBS demonstrated an ability to differentiate between normal control participants and individuals with eating disorders (von Ranson et al., 2005). Concurrent validity was also demonstrated through significant correlations (r = .68–.72) between the MEBS subscales (i.e., Weight Preoccupation and Body Dissatisfaction) and similar subscales (i.e., Shape concerns and Weight Concerns subscales) from the Eating Disorders Examination Questionnaire (von Ranson et al., 2005).
Alcohol Use Disorder Symptoms
Alcohol abuse and dependence symptoms (i.e., alcohol use disorder [AUD] symptoms) were assessed at both ages using the Substance Abuse Module (SAM) from the Composite International Diagnostic Interview (Robins, Babor, & Cottler, 1987). A composite score of all symptoms (e.g., recurrent alcohol-related legal problems, tolerance, and withdrawal) was used in analyses. The SAM is a well-established, semi-structured interview measure that has been used in field trials for the development of the DSM (Cottler et al, 1995; Spitzer, Williams, & Gibbon, 1987). The SAM shows excellent inter-rater reliability (Cottler, Robins, & Hezler, 1989), with an average kappa reliability of 0.92 for individual alcohol abuse and dependence symptoms. Further, kappa values from the MTFS assessment of AUD diagnoses using the SAM were excellent (all kappa’s > .90).
Depressive Symptoms
Symptoms of major depressive disorder (MDD) were assessed using the Structured Clinical Interview for the DSM-III-R (Spitzer et al., 1987). Symptom counts at both time points were included in analyses. Notably, kappa reliabilities for the MTFS major depressive disorder diagnoses were excellent (range = .82 to .89).
Trait Anxiety
The Trait Anxiety scale from the State-Trait Anxiety Inventory (Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983) was used to assess an individual’s typical level of anxiety at both time points. Psychometric properties of the scale are adequate in young adults. Alpha coefficients for high school and college females were .90 and .91, respectively (Spielberger et al., 1983) in previous studies. Test-retest reliability ranged from .65 to .77 for high school and college females over intervals between 20–104 days (Spielberger et al., 1983). Importantly, the Trait Anxiety scale was not administered at age 25 for the 17-year-old cohort; thus, the sample size for these data is smaller at that age.
Behavioral Disinhibition Scale
The Behavioral Disinhibition (BD) scale is composed of 12 items from the Socialization scale of the California Personality Inventory (CPI; Gough, 1957). BD is characterized as a tendency towards difficulties with impulse control, including lack of foresight, poor negative mood regulation, and a need for instant gratification (Hicks, unpublished data). Participants completed this scale at age 17, but not at age 25. Internal consistency of the BD scale was adequate (α = .68; Hicks, unpublished data).
Diagnoses
Eating disorder (i.e., anorexia nervosa [AN] and BN), AUDs, and major depressive disorder (MDD) diagnoses were assessed using DSM-III R and DSM-IV (except for AUD and MDD at age 17) criteria at both time points. Specifically, AN and BN were assessed using the Eating Disorders Structured Clinical Interview (EDSCI). The EDSCI is a semi-structured interview based on Module H of the Structured Clinical Interview for DSM Axis I Disorders (SCID; Spitzer et al., 1987). BN diagnoses were coded as absent, probable, and definite based on symptoms endorsed. A definite diagnosis was given if the subject met full diagnostic criteria for BN. A probable diagnosis was given if the participant was one symptom short of a full diagnosis, but still had at least subclinical levels of binge eating (i.e., binges on an amount of food that is larger than an average meal and purging or non-purging behaviors such as excessive exercise and/or frequency of these behaviors [e.g., twice a week for two months instead of twice per week for three months]). Similar to previous research in population-based samples (e.g., Bienvenu et al., 2000), probable and definite diagnoses were combined to indicate that a diagnosis was present.
The best estimates of lifetime BN diagnoses and symptoms were assessed at age 17. That is, at this age, both the twin’s mother and the twin herself reported on all BN symptoms, and we coded a symptom as present if either the mother or twin indicated that it was present. At age 25, consensual estimates could not be used since the twin’s mother did not report on symptoms at this time point. Thus, symptoms and diagnoses at age 25 were based on twin report only and include symptoms present over the earlier three to four years. Notably, BN symptoms tend to develop in late adolescence and young adulthood and typically persist for at least several years (American Psychiatric Association, 2000). Thus, it can be expected that the majority of women with BN symptoms between ages 17 and 20 will have BN symptoms present between ages 20 and 25, assessed at the age 25 time point. Importantly, reliability of BN diagnoses and symptoms was good with kappa values ranging from .64 to 1.00.
Alcohol dependence included both probable (i.e., two full symptoms of dependence) and definite (i.e., three or more full symptoms of dependence) diagnoses. Alcohol Abuse only included definite diagnoses, as only one symptom of abuse is needed to meet full diagnostic criteria. Definite (five or more full symptoms of depression plus impairment) and probable (four full symptoms of depression, with one of the symptoms being depressed mood or anhedonia, plus impairment) and were combined to indicate the presence of a diagnosis of major depressive disorder. Notably, kappa reliabilities for the MTFS major depressive disorder diagnoses were excellent (range = .82 to .89).
Procedures for Diagnostic Interviews
Eating disorder, AUD and MDD symptoms and diagnoses were assessed by trained bachelor’s and master’s level clinicians. Each symptom assigned was discussed in a clinical case conference with at least two advanced clinical psychology doctoral students. Discrepancies that emerged during the case conference were clarified by listening to interview audiotapes or re-contacting study participants. Symptoms were counted as present if they qualified for clinical significance in both frequency and severity.
Statistical Analyses
Cluster analysis was used as the primary analytic method as the majority of previous studies examining clusters in eating disorder samples used this approach (Claes et al., 2006; Espelage et al., 2002; Goldner et al., 1999; Westen & Harnden-Fischer, 2001). Further, studies using latent profile analysis in eating disorder samples have replicated the dysregulated cluster and resulted in cluster solutions that are comparable to studies using cluster analysis (Wagner et al., 2006; Wonderlich et al, 2005).
Two steps were conducted to prepare the data for the cluster analytic procedures. First, the 11 facet scales from the MPQ were transformed to z-scores (within age with cohorts combined) to account for differences in the normative level and variance of each scale. Standardization of the variables is recommended when using continuous variables that should be considered equally (i.e., have the same case weight) in the cluster analysis (Wishart, 2006). If variables are left unstandardized prior to cluster analysis, scales with greater standard deviations will have a larger impact on the estimated proximity (i.e., similarity value; Hair, Black, Babin, Anderson, & Tatham, 2006). Second, outliers (i.e., z-scores of 3.29 or greater; Tabachnick & Fidell, 2007) were removed because such extreme scores can distort results (Hair et al., 2006). Cluster analyses were then conducted separately at both time points with the MPQ facet scales using the program ClustanGraphics 8.06 (Wishart, 2006).
Several steps were taken to determine the best cluster solution. First, cluster analysis was conducted using increases in sum of squares (i.e., Ward’s method; Ward, 1963), a hierarchical method which minimizes the squared Euclidean distances among each item in a cluster and typically creates somewhat compact clusters (Wishart, 2006). Second, two measures for determining the “best cut” or optimum number of clusters, were examined. ClustanGraphics offers the upper tail t test and tree validation as two methods for determining the best solution. As clusters are agglomerated, the upper tail t test inspects the difference in fusion value size during each step (Wishart, 2006). A significantly large change as two clusters are combined (as indicated by the fusion value) suggests decreasing similarity/homogeneity of the agglomerated clusters. Thus, the best solution, as indicated by the upper tail t test, is the cluster number prior to the initial significant increase in the fusion values.
Tree validation was also used in determining which cluster solution provides the most optimum fit to the dataset. This method compares the tree (i.e., dendogram) for the current dataset with multiple trees generated using random permutation of the data. Tree validation attempts to reject the hypothesis that the data do not have structure or are distributed randomly. This method seeks cluster solutions that represent the largest deviation from randomness, as indicated by the greatest absolute difference score. This score is determined by subtracting the randomly estimated fusion statistic from the fusion statistic that is estimated using the data (e.g., |ESSData – ESSRandom| = Absolute Difference; Wishart, 2006).
After determining the best cluster solution at each time point, multivariate analysis of variance (MANOVA) was used to characterize clusters on MPQ facets. Significant multivariate effects were examined using univariate analysis of variance (ANOVA). Findings provide information about which MPQ facet scales typify each of the clusters. Stability of clusters across ages 17 and 25 was examined by calculating Cohen’s (1960) kappa coefficient (k). A k coefficient between .21 and .40 signifies fair stability of cluster membership, between .40 and .59 is moderate, .60 to .79 is substantial, and a kappa greater than .75 is excellent (Landis & Koch, 1977). The Reliable Change Index (RCI; Christensen & Mendoza, 1986; Jacobson & Truax, 1991) was used to identify how frequently the facet scales increased, decreased, or remained the same across time for each cluster across time. Reliable Change is calculated by subtracting scores at age 17 from scores at age 25 and dividing by the standard error of the difference between the two scores. Correlates of cluster members were examined at each time point to determine whether cluster membership relates to eating pathology and related conditions. Specifically, MANOVAs was used to evaluate whether there are significant differences between groups on bulimic behaviors, mood, and symptom count variables. Significant multivariate effects were examined using ANOVA to determine which groups were significantly different on each variable.3
RESULTS
Cluster Analysis of the MPQ and Cluster Comparisons
Overall, findings indicated that the best fit for the cluster analyses was a four-cluster solution at age 17 and a three-cluster solution at age 25. For example, jumps in fusion values in the best-cut analysis occurred at the four and three-cluster solution, respectively, where it was significant at p < .05 on an upper tail t test for the 17 (t (19) = 2.65) and 25-year-old samples (t (14) = 4.91).4 Tree validation results also indicated that the four-cluster solution was the best fit at age 17, and the three-cluster solution was the best fit at age 25, as the absolute differences (i.e., absolute deviations between the random fusion statistic and estimated fusion statistic) were 25.50 and 38.7 at ages 17 and 25, respectively. These large absolute difference scores suggest that there is a high departure from randomness in the four cluster solution at age 17 and the three cluster solution at age 25 (i.e., clusters at each time point are created based on patterns in the data).
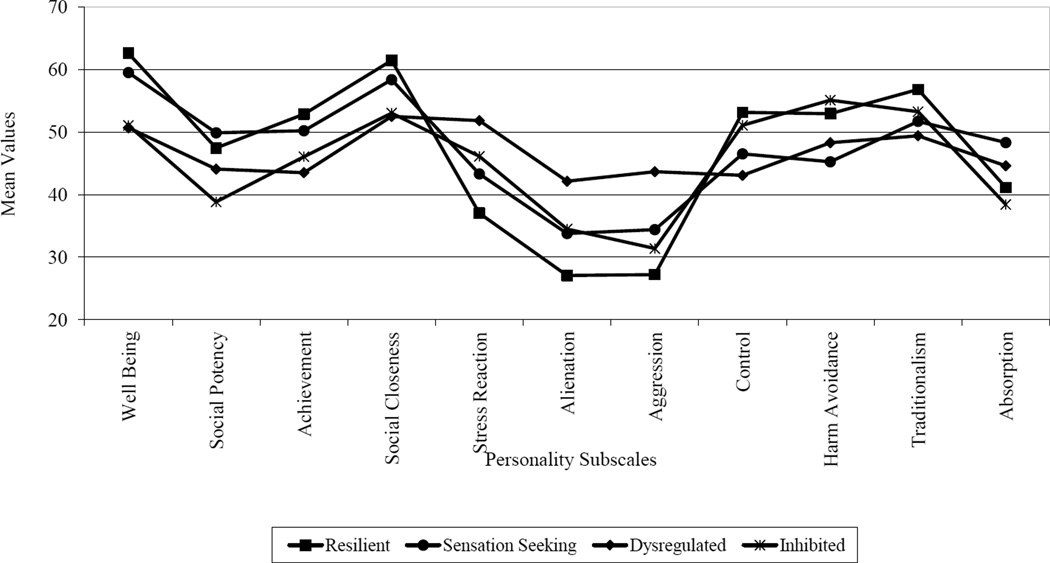
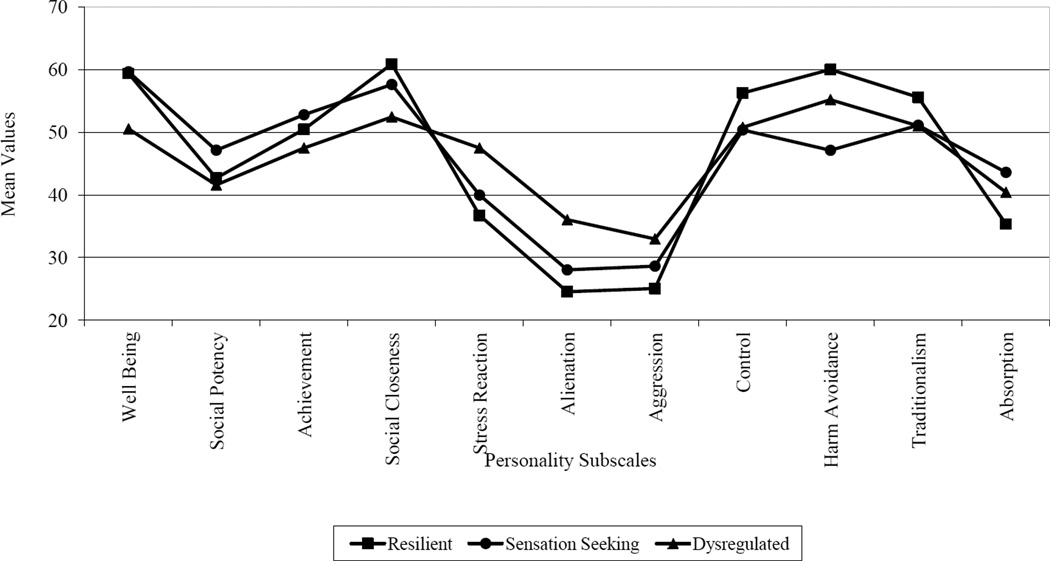
Examination of cluster differences revealed that Dysregulated, Resilient, and Sensation Seeking clusters were identified at each age, whereas an additional Inhibited cluster was identified at age 17 only (see Table 1 and Figure 1 and Figure 2). It should be noted that cluster names were based on predominant descriptors of each group based on characteristic personality traits in conjunction with conventions in the existing literature and do not necessarily indicate pathology. Specifically, the Dysregulated cluster had the highest levels of Stress Reaction, Alienation and Aggression, indicating increased anxiety, feelings of betrayal, and physical and interpersonal aggressiveness compared to the other clusters. In addition, the Dysregulated cluster had the lowest levels of Achievement and Traditionalism, suggesting they reported decreased levels of ambition and endorsement of moral values compared to the other groups. This group also had the lowest scores on Well Being and Social Closeness at both time points compared to other clusters, suggesting that this group experiences low levels of happiness and is uncomfortable in social interactions. Lastly, this group had the lowest Control score at age 17 and the second lowest at age 25 compared to the other groups, indicating that they may exhibit impulsive and rebellious behavior. Following expectations, this cluster is characterized as more interpersonally aggressive, emotionally labile, and impulsive than the other clusters and included 21% (268/1264) and 37% (437/1184) of women at ages 17 and 25, respectively.
Table 1.
Means of Three- and Four-Cluster Solutions for Multidimensional Personality Questionnaire (MPQ) Facet Scales at Ages 17 and 25
| Age 17 | Age 25 | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Resilient Cluster 1 (n=257, 20%) |
Sensation Seeking Cluster 2 (n=398, 32%) |
Dysregulated Cluster 3 (n=268, 21%) |
Inhibited Cluster 4 (n=341, 27%) |
F value |
Pairwise Contrast |
Resilient Cluster 1 (n=375, 32%) |
Sensation Seeking Cluster 2 (n=372, 31%) |
Dysregulated Cluster 3 (n=437, 37%) |
F value |
Pairwise Contrast |
||||||||
| M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | |||||
| Well Being | 0.83 | 0.63 | 0.45 | 0.75 | −0.64 | 0.85 | −0.60 | 0.81 | 278.22 | 1>2>3&4 | 0.43 | 0.78 | 0.47 | 0.72 | −0.67 | 0.82 | 286.14 | 1&2>3 |
| Social Potency | 0.28 | 0.93 | 0.57 | 0.89 | −0.13 | 0.75 | −0.77 | 0.79 | 166.47 | 2>1>3>4 | −0.11 | 1.00 | 0.42 | 0.96 | −0.24 | 0.89 | 52.03 | 2>1&3 |
| Achievement | 0.58 | 0.98 | 0.25 | 0.93 | −0.56 | 0.71 | −0.25 | 0.93 | 89.88 | 1>2>4>3 | 0.05 | 0.95 | 0.36 | 1.04 | −0.33 | 0.84 | 53.92 | 2>1>3 |
| Social Closeness | 0.63 | 0.84 | 0.26 | 0.85 | −0.45 | 0.93 | −0.39 | 0.94 | 99.41 | 1>2>3&4 | 0.54 | 0.79 | 0.14 | 0.86 | −0.49 | 0.92 | 151.44 | 1>2>3 |
| Stress Reaction | −0.82 | 0.80 | −0.15 | 0.85 | 0.77 | 0.82 | 0.15 | 0.89 | 161.74 | 3>4>2>1 | −0.57 | 0.82 | −0.22 | 0.89 | 0.59 | 0.81 | 205.97 | 3>2>1 |
| Alienation | −0.86 | 0.70 | −0.09 | 0.81 | 0.88 | 0.89 | −0.00 | 0.81 | 206.36 | 3>2&4>1 | −0.70 | 0.57 | −0.26 | 0.86 | 0.74 | 0.77 | 402.25 | 3>2>1 |
| Aggression | −0.81 | 0.57 | 0.02 | 0.83 | 1.09 | 0.81 | −0.33 | 0.70 | 314.45 | 3>2>4>1 | −0.63 | 0.59 | −0.10 | 0.87 | 0.55 | 0.96 | 207.03 | 3>2>1 |
| Control | 0.65 | 1.01 | −0.23 | 0.81 | −0.69 | 0.84 | 0.37 | 0.83 | 136.53 | 1>4>2>3 | 0.53 | 0.90 | −0.26 | 1.06 | −0.20 | 0.81 | 87.02 | 1>2&3 |
| Harm Avoidance | 0.29 | 0.95 | −0.49 | 0.97 | −0.18 | 0.94 | 0.51 | 0.77 | 87.06 | 4>1>3>2 | 0.62 | 0.71 | −0.71 | 0.86 | 0.13 | 0.87 | 252.60 | 1>3>2 |
| Traditionalism | 0.64 | 1.00 | −0.14 | 0.98 | −0.50 | 0.81 | 0.10 | 0.86 | 71.73 | 1>4>2>3 | 0.48 | 0.89 | −0.18 | 1.08 | −0.20 | 0.81 | 65.98 | 1>2&3 |
| Absorption | −0.24 | 1.01 | 0.52 | 0.95 | 0.13 | 0.75 | −0.53 | 0.88 | 90.35 | 2>3>1>4 | −0.50 | 0.93 | 0.39 | 1.04 | 0.04 | 0.78 | 90.08 | 2>3>1 |
Note. Sample sizes vary across age due to missing data. Z-scores are presented for ease of cluster comparisons. Boldface indicates significantly higher or lower scores on a facet scale compared to the other clusters at that time point. Age 17 Wilks’s λ =.18, F33 = 87.66, p<0.001; age 25 Wilks’s λ = .27, F22 = 99.06, p <0.001.
Figure 1.
Means of MPQ Facet Scales Across Resilient (n = 257), Sensation Seeking (n = 398), Dysregulated (n = 268), and Inhibited (n = 341) Clusters at 17-years-old.
Figure 2.
Means of MPQ Facet Scales Across Resilient (n = 375), Sensation Seeking (n = 372), and Dysregulated (n = 437) Clusters at 25-years-old.
At ages 17 and 25, 20% (257/1264) and 32% (375/1184) of women, respectively fell within the Resilient cluster. The Resilient cluster largely resembled clusters identified in previous studies that were labeled “Resilients” or “High-Functioning” (Claes et al., 2006; Thompson-Brenner & Westen, 2005). This cluster is characterized by high levels of social closeness, cautiousness, and moral standards as well as low anxiety, feelings of alienation, and aggression. The Sensation Seeking cluster contained 32% (398/1264) of women at age 17 and 31% (372/1184) of the sample at age 25. This cluster contains women with high levels of social dominance and a preference for novel and thrilling activities.
The Inhibited cluster was only present at age 17 with 27% (341/1264) of women falling within this cluster. Women in this cluster expressed a preference for safe activities over risky ones, prefer being alone and not being the center of attention, and are not very imaginative. Although this cluster is similar to the Inhibited/Anxious and Avoidant/Depressed groups found in previous research (Thompson-Brenner et al., 2008; Wagner et al., 2006), we did not expect it to represent a fourth and separate cluster at either age. However, given that changes in traits from adolescence to adulthood tend to follow a pattern of “increased maturity” (Caspi, Roberts, & Shiner, 2005) or changes in directions that seem to facilitate the performance of adult roles (e.g., increases in traits like Achievement, and decreases in traits as Aggression; Donnellan, Conger, & Burzette, 2007), it seems to make sense that there are different cluster groups represented at these two age groups.
Cluster Membership Stability
A Cohen’s (1960) k coefficient of .31 indicated fair stability of cluster membership across the first three clusters (i.e., Dysregulated, Resilient, and Sensation Seeking) from ages 17 to 25.5 The majority of women (55%; 435/797) remained within the same cluster across time, with the Dysregulated cluster being the most stable. Roughly 67% (145/217) of women originally classified in the Dysregulated cluster at age 17 remained in that cluster at age 25, with only 10% moving to the Resilient cluster and 23% moving to the Sensation Seeking cluster. Movement from other clusters to the Dysregulated cluster was also relatively uncommon, as only 23% of women moved from one of the other two clusters (i.e., Resilient or Sensation Seeking) at age 17 to the Dysregulated cluster at age 25. However, a larger percentage of women (i.e., 41%, see footnote 3) in the Inhibited cluster moved into the Dysregulated cluster at age 25. Overall then, 50% of women originally in the Resilient or Sensation Seeking groups moved to another group, whereas only 33% of women in the Dysregulated cluster moved to another cluster, again suggesting that cluster membership stability was greater for the Dysregulated relative to the other clusters.
The RCI was used to determine the pattern of change from age 17 to age 25 within each possible cluster grouping at 17 and 25 (e.g., Dysregulated to Sensation Seeking). As shown in Table 2, although 45% of women changed cluster membership across time, most of the MPQ traits that characterized these women remained stable or otherwise reflected changes in sensible ways (e.g., women who transited from Dysregulated to Resilient declined in Aggression and Alienation). Thus, patterns of underlying trait change are consistent with cluster membership stability and change.
Table 2.
Frequency of MPQ facet change across time from age 17 cluster membership to age 25 cluster membership
| SS→SS (n = 167) | SS→Resilient (n = 85) | SS→Dysregulated (n = 97) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Facet | ↓ | Stable | ↑ | ↓ | Stable | ↑ | ↓ | Stable | ↑ |
| Well Being | 19 (11%) | 122 (73%) | 26 (16%) | 8 (9%) | 66 (78%) | 11 (13%) | 33 (34%) | 61 (63%) | 3 (3%) |
| Social Potency | 18 (11%) | 144 (86%) | 5 (3%) | 18 (21%) | 64 (75%) | 3 (4%) | 21 (22%) | 74 (76%) | 2 (2%) |
| Achievement | 15 (9%) | 112 (67%) | 40 (24%) | 7 (8%) | 64 (75%) | 14 (17%) | 10 (10%) | 78 (80%) | 9 (9%) |
| Social Closeness | 20 (12%) | 122 (73%) | 25 (15%) | 11 (13%) | 54 (64%) | 20 (24%) | 26 (27%) | 62 (64%) | 9 (9%) |
| Stress Reaction | 29 (17%) | 122 (73%) | 16 (10%) | 33 (39%) | 51 (60%) | 1 (1%) | 12 (12%) | 67 (69%) | 18 (19%) |
| Alienation | 54 (32%) | 108 (65%) | 5 (3%) | 48 (57%) | 37 (44%) | 0 | 8 (8%) | 84 (87%) | 5 (5%) |
| Aggression | 32 (19%) | 132 (79%) | 3 (2%) | 27 (32%) | 58 (68%) | 0 | 8 (8%) | 89 (92%) | 0 |
| Control | 6 (4%) | 115 (69%) | 46 (27%) | 2 (2%) | 46 (54%) | 37 (44%) | 3 (3%) | 73 (75%) | 21 (22%) |
| Harm Avoidance | 15 (9%) | 111 (67%) | 41 (25%) | 1 (1%) | 50 (59%) | 34 (40%) | 4 (4%) | 63 (65%) | 30 (31%) |
| Traditionalism | 37 (22%) | 101 (61%) | 29 (17%) | 11 (13%) | 52 (61%) | 22 (26%) | 20 (21%) | 64 (66%) | 13 (13%) |
| Absorption | 51 (31%) | 107 (64%) | 9 (5%) | 46 (54%) | 34 (40%) | 5 (6%) | 39 (40%) | 51 (53%) | 7 (7%) |
| Overall N Mean (S | D) 1.8 (1.4) | 7.7 (2.1) | 1.5 (1.4) | 2.5 (1.3) | 6.7 (1.9) | 1.7 (1.3) | 1.9 (1.4) | 7.8 (1.9) | 1.2 (1.2) |
| Resil ient→SS (n= 73) | Resilient→Resilient (n = 123) | Resilient→ Dysregulate d (n = 35) | |||||||
| ↓ | Stable | ↑ | ↓ | Stable | ↑ | ↓ | Stable | ↑ | |
| Well Being | 14 (19%) | 56 (77%) | 3 (4%) | 18 (15%) | 102 (83%) | 3 (2%) | 16 (46%) | 19 (54%) | 0 |
| Social Potency | 3 (4%) | 64 (88%) | 6 (8%) | 20 (16%) | 96 (78%) | 7 (6%) | 4 (11%) | 30 (86%) | 1 (3%) |
| Achievement | 8 (11%) | 53 (73%) | 12 (16%) | 15 (12%) | 94 (76%) | 14 (11%) | 12 (34%) | 18 (51%) | 5 (14%) |
| Social Closeness | 23 (32%) | 41 (56%) | 9 (12%) | 23 (19%) | 87 (71%) | 13 (11%) | 17 (49%) | 17 (49%) | 1 (3%) |
| Stress Reaction | 7 (10%) | 55 (75%) | 11 (15%) | 18 (15%) | 95 (77%) | 10 (8%) | 0 | 25 (71%) | 10 (29%) |
| Alienation | 10 (14%) | 52 (71%) | 11 (15%) | 15 (12%) | 105 (85%) | 3 (2%) | 0 | 26 (74%) | 9 (26%) |
| Aggression | 4 (6%) | 68 (93%) | 1 (1%) | 1 (1%) | 121 (98%) | 1 (1%) | 1 (3%) | 29 (83%) | 5 (14%) |
| Control | 9 (12%) | 48 (66%) | 16 (22%) | 4 (3%) | 103 (84%) | 16 (13%) | 5 (14%) | 26 (74%) | 4 (11%) |
| Harm Avoidance | 8 (11%) | 57 (78%) | 8 (11%) | 2 (2%) | 92 (75%) | 29 (24%) | 6 (17%) | 21 (60%) | 8 (23%) |
| Traditionalism | 23 (32%) | 42 (58%) | 8 (11%) | 23 (19%) | 85 (69%) | 15 (12%) | 17 (49%) | 17 (49%) | 1 (3%) |
| Absorption | 13 (18%) | 51 (70%) | 9 (12%) | 49 (40%) | 64 (52%) | 10 (8%) | 8 (23%) | 24 (69%) | 3 (9%) |
| Overall N Mean (SD) | 1.7 (1.5) | 8.0 (1.7) | 1.3 (1.3) | 1.5 (1.4) | 8.4 (1.6) | 1.0 (1.0) | 2.5 (1.7) | 7.1 (2.4) | 1.3 (1.4) |
| Dysregulated→SS (n = 50) | Dysregulated→Resilient (n = 22) | Dysreg→Dysreg (n = 145) | |||||||
| ↓ | Stable | ↑ | ↓ | Stable | ↑ | ↓ | Stable | ↑ | |
| Well Being | 1 (2%) | 29 (58%) | 20 (40%0 | 0 | 10 (46%) | 12 (55%) | 25 (17%) | 99 (68%) | 21 (15%) |
| Social Potency | 5 (10%) | 44 (88%) | 1 (2%) | 5 (23%) | 16 (73%) | 1 (5%) | 18 (12%) | 120 (83%) | 7 (5%) |
| Achievement | 2 (4%) | 28 (56%) | 20 (40%) | 1 (5%) | 14 (64%) | 7 (32%) | 13 (9%) | 97 (67%) | 35 (24%) |
| Social Closeness | 4 (8%) | 28 (56%) | 18 (36%) | 0 | 13 (59%) | 9 (41%) | 27 (19%) | 89 (61%) | 29 (20%) |
| Stress Reaction | 27 (54%) | 23 (46%) | 0 | 14 (64%) | 8 (36%) | 0 | 35 (24%) | 101 (70%) | 9 (6%) |
| Alienation | 29 (58%) | 21 (42%) | 0 | 17 (77%) | 5 (23%) | 0 | 39 (27%) | 102 (70%) | 4 (3%) |
| Aggression | 27 (54%) | 23 (46%) | 0 | 16 (73%) | 6 (27%) | 0 | 59 (41%) | 86 (59%) | 0 |
| Control | 0 | 30 (60%) | 20 (40%) | 0 | 11 (50%) | 11 (50%) | 2 (1%) | 94 (65%) | 49 (34%) |
| Harm Avoidance | 4 (8%) | 31 (62%) | 15 (30%) | 0 | 9 (41%) | 13 (59%) | 3 (2%) | 86 (59%) | 56 (39%) |
| Traditionalism | 6 (12%) | 31 (62%) | 13 (26%) | 1 (5%) | 9 (41%) | 12 (55%) | 13 (9%) | 98 (68%) | 34 (23%) |
| Absorption | 12 (24%) | 31 (62%) | 7 (14%) | 10 (46%) | 10 (46%) | 2 (9%) | 42 (29%) | 93 (64%) | 10 (7%) |
| Overall N Mean (SD) | 2.3 (1.4) | 6.3 (2.2) | 2.3 (1.6) | 2.9 (1.1) | 5.0 (1.5) | 3.0 (1.4) | 1.9 (1.5) | 7.3 (2.2) | 1.9 (1.3) |
| Inhibited→SS (n = 49) | Inhibited→Resilient (n = 121) | Inhibited→Dysreg (n = 119) | |||||||
| ↓ | Stable | ↑ | ↓ | Stable | ↑ | ↓ | Stable | ↑ | |
| Well Being | 1 (2%) | 30 (61%) | 18 (37%) | 3 (3%) | 82 (68%) | 36 (30%) | 14 (12%) | 88 (74%) | 17 (14%) |
| Social Potency | 2 (4%) | 39 (80%) | 8 (16%) | 10 (8%) | 105 (87%) | 6 (5%) | 5 (4%) | 103 (87%) | 11 (9%) |
| Achievement | 1 (2%) | 34 (69%) | 14 (29%) | 7 (6%) | 88 (73%) | 26 (22%) | 7 (6%) | 92 (77%) | 20 (17%) |
| Social Closeness | 4 (8%) | 26 (53%) | 19 (39%) | 5 (4%) | 71 (59%) | 45 (37%) | 21 (18%) | 79 (66%) | 19 (16%) |
| Stress Reaction | 15 (31%) | 33 (67%) | 1 (2%) | 41 (34%) | 76 (63%) | 4 (3%) | 19 (16%) | 85 (71%) | 15 (13%) |
| Alienation | 15 (31%) | 34 (69%) | 0 | 61 (50%) | 60 (50%) | 0 | 18 (15%) | 94 (79%) | 7 (6%) |
| Aggression | 6 (12%) | 43 (88%) | 0 | 21 (17%) | 100 (83%) | 0 | 7 (6%) | 108 (91%) | 4 (3%) |
| Control | 4 (8%) | 39 (80%) | 6 (12%) | 2 (2%) | 78 (65%) | 41 (34%) | 4 (3%) | 103 (87%) | 12 (10%) |
| Harm Avoidance | 4 (8%) | 42 (86%) | 3 (6%) | 1 (1%) | 92 (76%) | 28 (23%) | 7 (6%) | 92 (77%) | 20 (17%) |
| Traditionalism | 10 (20%) | 34 (69%) | 5 (10%) | 16 (13%) | 77 (64%) | 29 (23%) | 29 (24%) | 78 (66%) | 12 (10%) |
| Absorption | 10 (20%) | 29 (59%) | 10 (20%) | 34 (28%) | 75 (62%) | 12 (10%) | 20 (17%) | 88 (74%) | 11 (9%) |
| Overall N Mean (SD) | 1.7 (1.3) | 7.7 (1.8) | 1.7 (1.2) | 1.7 (1.4) | 7.4 (1.9) | 1.9 (1.4) | 1.3 (1.2) | 8.4 (1.7) | 1.2 (1.3) |
Note. SS = Sensation Seeking; Dysreg = Dysregulated.
Associations with BN Behaviors and Related Behaviors
As expected, the Dysregulated group had the highest levels of bulimic behaviors at both time points, suggesting that these behaviors are most strongly associated with this type of personality profile. Moreover, this association is stable across time (see Table 3). Specifically, at age 17, the univariate analyses indicated that the MEBS total score and binge eating scores were highest among the Dysregulated group, whereas at age 25, this was the case for MEBS total score, body dissatisfaction, and compensatory behaviors. The Resilient cluster had the lowest levels of bulimic behaviors at both time points.
Table 3.
Comparisons between correlates at ages 17 and 25
| Age 17 | Age 25 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Resilient Cluster 1 |
Sensation Seeking Cluster 2 |
Dysregulated Cluster 3 |
Inhibited Cluster 4 |
F(df) | P | Resilient Cluster 1 |
Sensation Seeking Cluster 2 |
Dysregulated Cluster 3 |
F(df) | P | |
| MEBS Total Score | 5.03 | 5.96 | 7.93 | 6.92 | 6.55 | <001 | 5.59 | 6.33 | 8.63 | 26.42 | <001 |
| (4.92)a | (5.03)ab | (5.85)c | (6.10)bc | (3, 597) | (4.69)a | (5.60)a | (5.81)b | (2, 889) | |||
| Binge Eating | 0.64 | 0.92 | 1.66 | 1.13 | 12.18 | <001 | -- | -- | -- | -- | -- |
| (1.03)a | (1.27)ab | (1.61)o | (1.46)b | (3, 597) | |||||||
| Body Dissatisfaction | -- | -- | -- | -- | -- | -- | 2.17 | 2.20 | 3.24 | 23.96 | <001 |
| (2.05)a | (2.19)a | (2.27)b | (2, 889) | ||||||||
| Compensatory Beh. | -- | -- | -- | -- | -- | -- | .13 | .27 | .30 | 6.13 | .002 |
| (−46). | (.72)b | (.70)b | (2, 890) | ||||||||
| Trait Anxiety | 30.02 | 34.40 | 41.07 | 37.20 | 95.12 | <001 | 29.28 | 31.94 | 38.56 | 81.80 | <001 |
| (5.29)a | (6.62)b | (7.41)d | (7.75)c | (3, 1005) | (5.83)a | (6.10)b | (8.03)c | (2, 490) | |||
| Behavioral Dis. | 1.40 | 2.63 | 3.81 | 1.70 | 83.52 | <001 | -- | -- | -- | -- | -- |
| (1.38)a | (1.97)b | (2.50)c | (1.67)a | (3, 1191) | |||||||
| Depressive Sxs. | -- | -- | -- | -- | -- | -- | 0.56 | 0.91 | 1.56 | 20.49 | <001 |
| (1.64)a | (2.16)a | (2.66)b | (2, 1171) | ||||||||
| Alcohol composite | 0.18 | 0.46 | 0.95 | 0.23 | 18.87 | <001 | -- | -- | -- | -- | -- |
| (0.63)a | (1.32)b | (2.08)c | (0.89)ab | (3, 1227) | |||||||
Note. Results are from follow-up ANOVA analyses of correlates that were significant in the original MANOVA analyses (Age 17 Wilks sλ =.58,F30= 9.46, P<0.001; age 25 Wilks’s λ =.66, F18= 6.76,p<0.001). MEBS = Minnesota Eating Behavior Survey; Beh. = Behaviors; Dis. = Disinhibition; Sxs. = Symptoms. Depressive Symptoms represents DSM-III-R symptoms of major depressive disorder. Alcohol composite consists of DSM-III-R alcohol abuse and dependence symptoms combined. Raw scores (means and standard deviations) shown for descriptive purposes. Significant differences between clusters are identified by different subscript letters.
Findings for the other variables matched expectations. The Dysregulated group had the highest mean levels of AUD symptoms and behavioral disinhibition scores at age 17, as well as the highest levels of anxiety at both time points, and depressive symptoms at age 25. Although the mean alcohol composite score was the highest among the Dysregulated cluster at age 25, the p value in the overall MANOVA was above .01, so the post-hoc ANOVA was not conducted. However, the p value was .021 suggesting a trend in cluster differences in the alcohol composite at age 25, indicating some consistency in this relation across time. Similar to the other findings for associated variables, the Sensation Seeking cluster had the second highest levels of related symptoms, and the Resilient cluster had the lowest.
Diagnoses across Clusters
As expected, the Dysregulated cluster had the highest frequency of BN, alcohol abuse, and alcohol dependence at age 17 (see Table 4). This was also true at age 25, although the Sensation Seeking group had two women with BN versus one in the Dysregulated group. In contrast, AN was greatest in the Inhibited group at age 17; however, at age 25, the frequency of AN was highest in the Dysregulated cluster. MDD was higher in the Sensation Seeking group at age 17, but similar to AN frequencies, was highest in the Dysregulated cluster at age 25. Findings suggest that the Dysregulated group is becoming worse over time with regard to psychopathology.
Table 4.
Comparisons between Clusters on Diagnoses
| Age 17 | Age 25 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Resilient Cluster 1 |
Sensation Seeking Cluster 2 |
Dysregulated Cluster 3 |
Inhibited Cluster 4 |
Full Sample | Resilient Cluster 1 |
Sensation Seeking Cluster 2 |
Dysregulated Cluster 3 |
Full Sample | |
| Combined Number of Probable and Definite Diagnoses | |||||||||
| Anorexia Nervosa | 4 (2.5%) | 2 (1.1%) | 4 (3.8%) | 14 (7.7%) | 24 (1.9%) | 2 (0.7%) | 5 (1.7%) | 7 (2.2%) | 14 (1.2%) |
| Bulimia Nervosa | 0 | 2 (0.5%) | 4 (1.5%) | 2 (0.6%) | 8 (0.6%) | 1 (0.3%) | 2 (0.5%) | 1 (0.2%) | 4 (0.4%) |
| Major Depressive D/O | 24 (9%) | 58 (15%) | 53 (20%) | 48 (14%) | 183 (14%) | 23 (6%) | 38 (10%) | 70 (16%) | 131 (11%) |
| Alcohol Abuse | 17 (7%) | 46 (12%) | 49 (18%) | 17 (5%) | 129 (10%) | 24 (9%) | 51 (14%) | 81 (19%) | 156 (13%) |
| Alcohol Dependence | 3 (1.2%) | 28 (7%) | 34 (13%) | 15 (4%) | 80 (6.3%) | 11 (3%) | 24 (7%) | 28 (6%) | 63 (5.3%) |
| BN Symptoms | .10 (.53) | .17 (.81) | .34 (1.10) | .17 (.78) | -- | .12 (.77) | .22 (.94) | .13 (.66) | -- |
Note. D/O = Disorder; BN = Bulimia Nervosa. Percentages, shown in parentheses, indicate the number of individuals with probable and definite diagnoses divided by the total number of participants in each cluster. All diagnoses are DSM-IV with the exception of age 17 diagnoses of MDD, alcohol abuse, and alcohol dependence which are DSM-IIIR. Standard deviations are indicated in parentheses for BN symptoms.
DISCUSSION
The current investigation is the first to examine associations between the dysregulated cluster and BN symptoms and associated conditions in a longitudinal, population-based sample of girls followed from late adolescence into young adulthood. Notably, the dysregulated cluster, present in all previous cluster analytic examinations of women with eating disorders, was identified in this population-based sample during late adolescence as well as adulthood. In addition, findings indicated that the Dysregulated group was the most stable cluster in longitudinal analyses and this group had the highest levels of bulimic behaviors as well as known correlates of BN including alcohol use problems, behavioral disinhibition, anxiety, and depressive symptoms. Further, the majority of these relations remained stable across time. Overall, findings support continued efforts to link this personality profile with eating pathology.
It is notable that the clusters identified in the present study correspond well to those identified in samples of women with eating disorders. For example, the Resilient cluster largely resembled clusters identified in previous studies that were labeled “Resilients” or “High-Functioning” (Claes et al., 2006; Thompson-Brenner & Westen, 2005). In addition, the Inhibited cluster is similar to the Inhibited/Anxious and Avoidant/Depressed groups found in previous research (Thompson-Brenner et al., 2008; Wagner et al., 2006). Lastly, the Dysregulated cluster corresponded to other dysregulated clusters, such as the Emotionally Dysregulated/Undercontrolled group (Westen & Harnden-Fischer, 2001) and the Dysregulated group (Thompson-Brenner & Westen, 2005). The Sensation Seeking group corresponded with previously identified clusters the least; however, it is somewhat similar to Impulsive clusters identified in earlier studies (e.g., Wagner et al., 2006). In sum, findings suggest that the personality clusters of women with eating disorders do not differ greatly from the present, population-based sample that was not selected for eating pathologies. The differences between samples may therefore be found in the degree of personality pathology and difficulties associated with these traits, rather than major discrepancies in their overall personality styles. Therefore, the present findings apply to a range of pathology from normal to abnormal.
The current study expanded on extant research by being the first to use a longitudinal sample to examine stability of cluster membership and associations with bulimic pathology from adolescence into adulthood. Importantly, the Dysregulated cluster was the most stable across time with 33% of Dysregulated 17 year olds moving into another cluster at age 25 (compared to 47% in the next most stable cluster). Nevertheless, findings indicated only fair stability (Cohen’s k =.31) of clusters overall, which may be accounted for, in part, by developmental changes in personality traits. Findings corroborate some previous population-based studies of adolescents, which generally found personality profiles to be “unstable” (see review in Meeus et al., 2011). For example, one study indicated that only 38% of the samplemaintained the same personality profile over three years during adolescence (initial assessment age range = 11–15 years old; van Aken & Dubas, 2004). Importantly, however, movement in these population-based studies was typically from the “undercontrolled” and “overcontrolled” groups to the resilient cluster. Although, in the present study, the greatest movement was not to the Resilient group for any clusters except the Inhibited group, all groups demonstrated a “functional maturity” in mean levels of traits (Blonigen et al., 2008). That is, personality research has indicated a “trend toward growth and maturity” (Donnellan et al., 2007) across time, with increases in traits that facilitate success in adult roles such as worker, committed partner, and parent and decreases in traits that negatively impact role performance (e.g., increases in self-control and decreases in negative affectivity). Indeed, in the present sample, there were overall increases in traits such as Well Being and Achievement, and decreases traits such as Stress Reaction and Aggression, from ages 17 to 25 (see Table 1). Further, as shown in Table 2, most of the women who changed clusters across time followed a pattern of growth and maturity.
One of the largest longitudinal cluster changes in the present study was the movement of the Inhibited cluster at age 17 into the other three clusters at age 25. The majority of Inhibited 17 year olds moved into either the Resilient (i.e., 42%) or Dysregulated (i.e., 41%) group at age 25. By contrast, the smallest number of women (only 17%) moved to the Sensation Seeking cluster. It is unclear why this pattern of movement occurred across time for the Inhibited cluster; however, comparisons between the characteristic traits of each cluster may provide some insight. That is, the Inhibited group is characterized largely by low Social Potency (i.e., low levels of persuasiveness, decisiveness, influence over others) and high Harm Avoidance (i.e., avoidance of risky activities). Although the Dysregulated and Resilient groups do not closely resemble the Inhibited group, they are not really opposite of the cluster either. That is, many of the mean levels of traits in the Inhibited group fall between those of the Dysregulated and Resilient groups. Thus, slight increases or decreases in mean levels of the traits in the Inhibited group across development could lead to a closer resemblance to the Dysregulated (e.g., an increase in social alienation and anxiety) or Resilient (e.g., an increase in social acceptance and coping) clusters. In contrast, the Sensation Seeking cluster, a group with the highest Social Potency and lowest Harm Avoidance at both time points, appears to have the opposite personality profile of the Inhibited group. Given these differences, it is perhaps not surprising that the smallest movement occurred between these clusters.
The correlates of the Dysregulated cluster were largely similar to those reported in previous research. Bulimic behaviors were present in all clusters, as expected given the heterogeneity of the disorder, with the highest mean levels of each symptom present in the Dysregulated group (Claes et al., 2006; Perkins et al., in preparation; Westen & Harnden-Fischer, 2001; Wildes et al., 2011) compared to the other clusters. This supports the idea that the dysregulated cluster may be more strongly associated with bulimic pathology, particularly given that women with anorexia nervosa, restricting type are sometimes absent from this cluster (Westen and Harnden-Fischer, 2001). With regard to psychological conditions and behaviors associated with bulimic behaviors, findings also followed expectations with the Dysregulated cluster having the highest level of AUD symptoms and trait anxiety at age 17 and 25 (although not significantly at age 25), suggesting that these correlates are also stable longitudinally. This group also had significantly higher behavioral disinhibition at age 17 and significantly higher depressive symptoms at age 25 than the other clusters. In sum, findings support primary goals of the present paper. That is, the longitudinal stability of the clusters and their correlates, particularly, for the Dysregulated cluster, provides some support for research aimed at examining etiological associations between personality clusters and BN (e.g., Wonderlich et al., 2005). Further, since the present study used a population-based sample, findings appear to be generalizable and informative for the more common, non-clinical levels of BN behaviors (Neumark-Sztainer & Hannan, 2000).
With regard to diagnostic frequencies, it was not surprising that the Dysregulated group had the greatest percentage of BN, MDD, and AUD diagnoses at both time points (with the exception of BN at age 25). This corroborated previous cluster analytic studies of women with eating disorders which found greater numbers of women with these diagnoses in the Dysregulated group compared to other clusters (Claes et al., 2006; Thompson-Brenner & Westen, 2005; Wonderlich et al, 2005). Interestingly, AN was greatest in the Inhibited group at age 17. This supports some previous research suggesting that women with AN are characterized as having high harm avoidance (Klump et al., 2000b). Notably, AN was highest in the Dysregulated cluster at age 25, which further supports findings that women with eating disorders are heterogeneous with regard to personality (Vitousek & Manke, 1994). This may stem, in part, from the high diagnostic cross-over rate in eating disorders (Eddy et al., 2008). Of note, the overall prevalence rates of these disorders (see “full sample” in Table 4) corresponded to those of women in population-based studies (e.g., BN 1.3%, subthreshold AN 1.5%, MDD 17%, Alcohol Abuse 11.5%, Alcohol Dependence 8.0%; Hasin, Goodwin, Stinson, & Grant, 2005; Hasin, Stinson, Ogburn, & Grant, 2007; Swanson, Crow, Le Grange, Swendsen, & Merikangas, 2011). Nonetheless, the Dysregulated group does appear to be the cluster with not only the most psychopathology, but also increasing levels across time. Thus, although there is a trait-level trend towards growth and maturity among each cluster, some individuals in the Dysregulated cluster are likely remaining “dysregulated” and perhaps becoming more so across time. Furthermore, findings suggest that the Dysregulated personality may be risk factor for several different forms of psychopathology.
Although the present study was the first to identify and examine the stability of the dysregulated cluster longitudinally within a population-based sample, it was not without limitations. First, only two time points were included in the study with a fairly large range between the ages. Although the archival data set utilized in the present study included assessments at age 20, only one cohort completed the MPQ during that assessment. Given that clusters can be sample-dependent (Rapkin & Luke, 1993), clustering was not conducted on this partial sample for comparison with the full sample. Nevertheless, if the data were available on the full sample, it would have been informative to examine the stability of the clusters across several time points to determine whether it is more or less stable across different stages of development. Second, it is unclear whether the clusters identified in the present study would have been replicated in this population-based sample of women using a different measure of personality such as a Big Five-based measure (e.g., Costa & McCrae, 1992). However, there is some evidence that there is a hierarchical relationship between normal and abnormal personality traits as measured by a variety of personality models (Markon, Krueger, & Watson, 2005). Nonetheless, if similar profiles were indicated using alternate measures, it would provide further support that the clusters identified in eating disorder samples can be replicated in population-based samples.
Overall, the current study indicated that the dysregulated cluster is a robust personality profile that is present in adolescence and adulthood and is relatively stable across time. Importantly, the dysregulated cluster may represent a high risk personality profile that would be fruitful to examine in etiologic research concerning BN. This supports extant research suggesting that this personality style may be a risk factor for BN (Lilenfeld et al. 1998; Wonderlich & Mitchell, 2001). Indeed, given higher rates of bulimic behaviors, alcohol use, depressive symptoms, and anxiety in this cluster compared to other groups, this risk profile appears to cut across diagnostic boundaries and may aid in understanding the etiologic basis of a diverse range of phenotypes.
Acknowledgments
This work was supported by National Institute on Alcohol Abuse and Alcoholism grant R01 AA009367. Address correspondence to Jennifer D. Slane, University of Michigan Addiction Research Center, Rachel Upjohn Building, 4250 Plymouth Road, Office 2433, Ann Arbor, MI 48109-2700; E-mail: slane@msu.edu
Data for this project were collected at the University of Minnesota.
This article was accepted under the editorship of Robert F. Krueger and John Livesley. From Department of Psychiatry, University of Michigan (J. D. S.); Department of Psychology, Michigan State University (K. L. K., M. B. D.); and Department of Psychology, University of Minnesota (M. M., W. G. I.).
Footnotes
Of the women included in the cluster analysis at age 17, 178 were lost to follow-up at age 25. Further, 98 women were included in the cluster analysis at age 25 who were not assessed at age 17. There were only two significant differences between the group that dropped out at age 17 and those that remained in the sample. The group that dropped out after the assessment at 17 was slightly older (M = 18.01 compared to 17.85) and had lower levels of Traditionalism (M = 52.34 compared to 52.72). The effect sizes of these differences were very small (Cohen’s d = .06 and .10, respectively), thus, we did not find it necessary to make adjustments to the analyses.
The Minnesota Eating Behavior Survey (MEBS; previously known as the Minnesota Eating Disorder Inventory (M-EDI)) was adapted and reproduced by special permission of Psychological Assessment Resources, Inc., 16204 North Florida Avenue, Lutz, Florida 33549, from the Eating Disorder Inventory (collectively, EDI and EDI-2) by Garner, Olmstead, Polivy, Copyright 1983 by Psychological Assessment Resources, Inc. Further reproduction of the MEBS is prohibited without prior permission from Psychological Assessment Resources, Inc.
Due to the large number of tests, a conservative Type I error rate of .01 was used for the multivariate analysis of variance tests.
Due to the non-independence of twin data, analyses were also run separately with a random selection of twins from each pair at age 17 and at age 25. Findings for both groups of twins corresponded to those of the entire sample (data not shown.), i.e., a 4-cluster solution was best at age 17, and a 3-cluster solution was best at age 25.
Because the kappa statistic requires a symmetric two-way table with matching variable values at both time points, individuals falling within the fourth, Inhibited cluster at age 17 were excluded from kappa analyses of cluster stability. However, among the Inhibited group, 42% (121/289) moved to the Resilient cluster at age 25, 17% (49/289) moved to the Sensation Seeking cluster, and 41% (119/289) moved to the Dysregulated cluster.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders - 4th Ed - Text Revision. Washington, D.C.: American Psychiatric Association; 2000. [Google Scholar]
- Bienvenu OJ, Samuels JF, Riddle MA, Hoehn-Saric R, Liang K, Cullen BA, et al. The relationship of obsessive-compulsive disorder to possible spectrum disorders: Results from a family study. Biological Psychiatry. 2000;28:287–293. doi: 10.1016/s0006-3223(00)00831-3. [DOI] [PubMed] [Google Scholar]
- Blonigen DM, Carlson MD, Hicks BM, Krueger RF, Iacono WG. Stability and change in personality traits from late adolescence to early adulthood: A longitudinal twin study. Journal of Personality. 2008;76:229–266. doi: 10.1111/j.1467-6494.2007.00485.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, Roberts BW, Shiner RL. Personality development: Stability and change. Annual Review of Psychology. 2005;56:453–484. doi: 10.1146/annurev.psych.55.090902.141913. [DOI] [PubMed] [Google Scholar]
- Claes L, Vandereycken W, Luyten P, Soenens B, Pieters G, Vertommen H. Personality prototypes in eating disorders based on the Big Five Model. Journal of Personality Disorders. 2006;20:401–416. doi: 10.1521/pedi.2006.20.4.401. [DOI] [PubMed] [Google Scholar]
- Christensen L, Mendoza JL. A method of assessing change in a single subject: An alteration of the RC index. Behavior Therapy. 1986;17:305–308. [Google Scholar]
- Cohen J. A coefficient of agreement for nominal scales. Educational and Psychological Measurement. 1960;20:37–46. [Google Scholar]
- Costa PT, Jr., McCrae RR. Revised NEO Personality Inventory (NEO-PR I) and the Five Factor Inventory (NEO-FFI): Professional Manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- Cottler LB, Schuckit MA, Helzer JE, Crowley T, Woody G, Nathan P, Hughes J. The DSM-IV field trial for substance use disorders: Major results. Drug and Alcohol Dependence. 1995;38:59–69. doi: 10.1016/0376-8716(94)01091-x. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Robins LN, Helzer JE. The reliability of the Composite International Diagnostic Interview Substance Abuse Module (CIDI-SAM) – A comprehensive substance abuse interview. British Journal of Addiction. 1989;84:801–814. doi: 10.1111/j.1360-0443.1989.tb03060.x. [DOI] [PubMed] [Google Scholar]
- Donnellan MB, Conger RD, Burzette RG. Personality development from late adolescence to young adulthood: Differential stability, normative maturity, and evidence for the maturity-stability hypothesis. Journal of Personality. 2007;75:237–264. doi: 10.1111/j.1467-6494.2007.00438.x. [DOI] [PubMed] [Google Scholar]
- Eddy KT, Dorer DJ, Franko DL, Tahilani K, Thompson-Brenner H, Herzog DB. Diagnostic crossover in anorexia nervosa and bulimia nervosa: Implications for DSM-V. American Journal of Psychiatry. 2008;165:245–250. doi: 10.1176/appi.ajp.2007.07060951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espelage DL, Mazzeo SE, Sherman R, Thompson R. MCMI-II profiles of women with eating disorders: A cluster analytic investigation. Journal of Personality Disorders. 2002;16:453–463. doi: 10.1521/pedi.16.5.453.22127. [DOI] [PubMed] [Google Scholar]
- Goldner EM, Srikameswaran S, Schroeder ML, Livesley WJ, Birmingham CL. Dimensional assessment of personality pathology in patients with eating disorders. Psychiatry Research. 1999;85:151–159. doi: 10.1016/s0165-1781(98)00145-0. [DOI] [PubMed] [Google Scholar]
- Gough HG. Manual for the California Psychological Inventory. Palo Alto, CA: Consulting Psychologists Press; 1957. [Google Scholar]
- Hair JF, Black WC, Babin BJ, Anderson RE, Tatham RL. Multivariate Data Analaysis. 6th Ed. New Jersey: Pearson; 2006. [Google Scholar]
- Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: Results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Archives of General Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, Correlates, Disability, and Comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hicks BM. Preliminary evaluation of behavioral disinhibition phenotypes for the GEDI Project. unpublished [Google Scholar]
- Hopwood CJ, Donnellan MB, Blonigen DM, Krueger RF, McGue MG, et al. Genetic and environmental influences on personality trait stability and growth during the transition to adulthood: A three-wave longitudinal study. Journal of Personality and Social Psychology. 2011;100:545–556. doi: 10.1037/a0022409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacono WG, Carlson SR, Taylor J, Elkins IJ, McGue M. Behavioral disinhibition and the development of substance-use disorders: findings from the Minnesota Twin Family Study. Developmental Psychopathology. 1999;11:869–900. doi: 10.1017/s0954579499002369. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Klump KL, Bulik CM, Pollice C, Halmi KA, Fichter MM, Berrettini WH, et al. Temperament and character in women with anorexia nervosa. The Journal of Nervous and Mental Disease. 2000a;188:559–567. doi: 10.1097/00005053-200009000-00001. [DOI] [PubMed] [Google Scholar]
- Klump KL, McGue M, Iacono WG. Age differences in genetic and environmental influences on eating attitudes and behaviors in preadolescent and adolescent female twins. Journal of Abnormal Psychology. 2000b;109:239–251. [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE. Epidemiological personology: The unifying role of personality in population-based research on problem behaviors. Journal of Personality. 2000;68:967–998. doi: 10.1111/1467-6494.00123. [DOI] [PubMed] [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- Lilenfeld LR, Kaye WH, Greeno CG, Merikangas KR, Plotnicov K, Pollice C, et al. Psychiatric disorders in women with bulimia nervosa and their first-degree relatives: Effects of comorbid substance dependence. International Journal of Eating Disorders. 1998;22:253–264. doi: 10.1002/(sici)1098-108x(199711)22:3<253::aid-eat4>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Markon KE, Krueger RF, Watson D. Delineating the structure of normal and abnormal personality: An integrative hierarchical approach. Journal of Personality and Social Psychology. 2005;88:139–157. doi: 10.1037/0022-3514.88.1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGue M, Bacon S, Lykken DT. Personality stability and change in early adulthood: A behavioral genetic analysis. Developmental Psychology. 1993;29:96–109. [Google Scholar]
- Meeus W, Van de Schoot R, Kimistra T, Branje S. Change and stability and links with adjustment and relationships: A five-wave longitudinal study. Developmental Psychology. 2011;47:1181–1195. doi: 10.1037/a0023816. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Hannan PJ. Weight-related behaviors among adolescent girls and boys: Results from a national survey. Archives of Pediatric Adolescent Medicine. 2000;154:569–77. doi: 10.1001/archpedi.154.6.569. [DOI] [PubMed] [Google Scholar]
- Perkins PS, Slane JD, Klump KL. Personality clusters and family relationships in women with eating pathology. in preparation doi: 10.1016/j.eatbeh.2013.05.007. [DOI] [PubMed] [Google Scholar]
- Rapkin BD, Luke DA. Cluster analysis in community research: Epistemology and practice. American Journal of Community Psychology. 1993;21:247–277. [Google Scholar]
- Roberts BW, Caspi A, Moffitt TE. The Kids Are Alright: Growth and stability in personality development from adolescence to adulthood. Journal of Personality and Social Psychology. 2001;81:670–683. [PubMed] [Google Scholar]
- Robins LN, Babor TF, Cottler LB. Composite International Diagnostic Interview: Expanded substance abuse module. St Louis, MO: Washington University Department of Psychiatry; 1987. [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene RE, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory (Form Y): (“self-evaluation questionnaire”) Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M. Structured Clinical Interview for DSM III-R (SCID) New York: New York State Psychiatric Institute, Biometrics Research; 1987. [Google Scholar]
- Swanson SA, Crow SJ, Le Grange D, Swendsen J, Merikangas KR. Prevalence and correlates of eating disorders in adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. Archives of General Psychiatry. 2011;68:714–723. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics – Fifth Edition. Boston, MA: Allyn & Bacon; 2007. [Google Scholar]
- Tellegen A. Brief manual for the Multidimensional Personality Questionnaire. Unpublished manuscript, University of Minnesota, Minneapolis; 1982. [Google Scholar]
- Thompson-Brenner H, Westen D. A naturalistic study of psychotherapy for bulimia nervosa, part 1: Comorbidity and therapeutic outcome. The Journal of Nervous and Mental Disease. 2005;193:573–584. doi: 10.1097/01.nmd.0000178843.81100.eb. [DOI] [PubMed] [Google Scholar]
- Thompson-Brenner H, Eddy KT, Satir DA, Boisseau CL, Westen D. Personality subtypes in adolescents with eating disorders: Validation of a classification approach. The Journal of Child Psychology and Psychiatry. 2008;49:170–180. doi: 10.1111/j.1469-7610.2007.01825.x. [DOI] [PubMed] [Google Scholar]
- van Aken MAG, Dubas JS. Personality type, social relationships, and problem behavior in adolescence. European Journal of Developmental Psychology. 2004;1:331–348. [Google Scholar]
- von Ranson KM, Klump KL, Iacono WG, McGue M. The Minnesota Eating Behavior Survey: A brief measure of disordered eating attitudes and behaviors. Eating Behaviors. 2005;6:373–392. doi: 10.1016/j.eatbeh.2004.12.002. [DOI] [PubMed] [Google Scholar]
- Vitousek K, Manke F. Personality variables and disorders in anorexia nervosa and bulimia nervosa. Journal of Abnormal Psychology. 1994;103:137–147. doi: 10.1037//0021-843x.103.1.137. [DOI] [PubMed] [Google Scholar]
- Wagner A, Barbarich-Marsteller NC, Frank GK, Bailer UF, Wonderlich SA, Crosby RD, et al. Personality traits after recovery from eating disorders: Do subtypes differ? International Journal of Eating Disorders. 2006;39:276–284. doi: 10.1002/eat.20251. [DOI] [PubMed] [Google Scholar]
- Ward JH. Hierarchical grouping to optimize an objective function. Journal of the American Statistical Association. 1963;58:236–244. [Google Scholar]
- Westen D, Harnden-Fischer J. Personality profiles in eating disorders: Rethinking the distinction between Axis I and Axis II. American Journal of Psychiatry. 2001;158:547–562. doi: 10.1176/appi.ajp.158.4.547. [DOI] [PubMed] [Google Scholar]
- Westen D, Thompson-Brenner H, Peart J. Personality and eating disorders. In: Wonderlich S, Mitchell JE, Zwaan Md, Steiger H, editors. Annual Review of Eating Disorders Part II - 2006. Oxford: Radcliffe Publishing; 2006. [Google Scholar]
- Wildes JE, Marcus MD, Crosby RD, Ringham RM, Dapelo MM, Gaskill JA, et al. The clinical utility of personality subtypes in patients with anorexia nervosa. Journal of Consulting and Clinical Psychology. 2011;5:665–674. doi: 10.1037/a0024597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wishart D. Clustan Graphics Primer: A Guide to Cluster Analysis. Fourth Edition. Edinburgh: Clustan Ltd; 2006. [Google Scholar]
- Wonderlich SA, Crosby R, Joiner T, Peterson CB, Bardone-Cone A, Klein M, et al. Personality subtyping and bulimia nervosa: Psychopathological and genetic correlates. Psychological Medicine. 2005;35:647–657. doi: 10.1017/s0033291704004234. [DOI] [PubMed] [Google Scholar]
- Wonderlich SA, Mitchell JE. The role of personality in the onset of eating disorders and treatment implications. Psychiatric Clinics of North America. 2001;24:249–258. doi: 10.1016/s0193-953x(05)70221-5. [DOI] [PubMed] [Google Scholar]