Abstract
Background/Objectives
Comorbidity is common among patients with heart failure (HF). Heart failure with preserved left ventricular ejection fraction (HF-P) is increasing in prevalence, accounting for a substantial proportion of clinical cases of HF but whether patterns of comorbidity and multiple morbidity differ from those of patients with HF with reduced left ventricular ejection fraction (HF-R) has not been examined. We examined whether the total burden of comorbidity and pattern of co-occurring conditions varies in patients with HF-P or HF-R.
Design
Cross sectional cohort study.
Setting
Four participating health plans within the National Heart, Lung and Blood Institute-sponsored Cardiovascular Research Network.
Measurements
The sample consisted of all members ≥65 years with HF based on hospital discharge and ambulatory visit diagnoses. Patients with ejection fraction ≥50%, were classified as having HF-P. Presence of cardiac and non-cardiac comorbidities was obtained from health plan administrative databases.
Results
We identified 23,435 patients with HF and EF information; 53% (12,407) had confirmed HF-P (mean age = 79.6 years; 60% women). More than 3/4 of the sample had 3 or more co-occurring conditions in addition to HF. One half of the sample had 5 or more co-occurring conditions. Patients with HF-P had a slightly higher burden of comorbidity than those with HF-R (mean = 4.5 vs 4.4; p=.002). Patterns of how specific conditions co-occurred did not vary in patients with preserved or reduced systolic function.
Conclusion
There is a high degree of comorbidity and multiple morbidity in patients with HF. The burden and pattern of comorbidity in patients with HF varies only slightly in patients with preserved or reduced systolic function.
Keywords: Heart Failure, Comorbidity, Multi-morbidity, epidemiology
INTRODUCTION
With the aging of the U.S. population, the number of persons with multiple chronic medical conditions has increased dramatically.1 Multiple morbidity can make clinical decision-making and disease management challenging, and may increase the risk for adverse outcomes including unnecessary hospitalizations, adverse drug events, and functional decline, with overall increases in the costs of medical care.2, 3 A recent report indicated that the one quarter of patients with multiple chronic conditions account for nearly two thirds of healthcare spending in the U.S.,4 highlighting the financial impact that this very high risk population exerts on our healthcare system.
Heart failure (HF) disproportionately affects the elderly and carries a very high burden of comorbidity.5 Nearly one half of patients with HF have five additional comorbid conditions present, and the rates of comorbidities in patients with HF have steadily increased over the past 2 decades.5, 6 Increasing numbers of patients diagnosed with HF have preserved left ventricular ejection fraction (HF-P).7 Although there are a limited number of studies on HF-P, HF patients presenting with preserved ejection fraction are typically older and are more likely to be female than are patients presenting with HF and reduced left ventricular ejection fraction (HF-R).7–9 Differences in the occurrence of specific comorbidities between patients with HF and preserved or reduced left ventricular systolic function have been reported. In general, patients with HF-P tend to have higher rates of hypertension and atrial fibrillation, and patients with HF-R tend to have higher rates of prior myocardial infarction.7–9 Despite the high burden of comorbidity among patients with HF, the co-occurrence of multiple chronic conditions has not been well characterized and has not been compared in patients with HF-P vs. HF-R.
Although understanding rates of specific conditions that co-occur with HF and preserved or reduced systolic function is important, with the increasing age of the HF population, it is becoming more important to also characterize patterns of comorbidity in these patients. The overall burden and patterns of cardiac and non cardiac comorbidities may influence clinical decision-making in these patients, especially when the evidence base around treatment decisions is limited.
In the present study, we describe the patterns of comorbidity (how multiple conditions co-occurred) in a large, multi-center, community-based cohort of older adults with heart failure and assess if patterns differ according to whether HF is with preserved or reduced left ventricular systolic function and according to age.
METHODS
Source Population
This study is based on data from the NHLBI-sponsored Cardiovascular Research Network’s (CVRN)10 PRESERVE study. The PRESERVE study is a large, multi-center community based study of patients with HF that is examining differences in predictors of, and outcomes associated with, HF-P as compared to HF-R. The source population included patients from 4 health plans who participate in the CVRN. Sites included Kaiser Permanente of Northern California, Kaiser Permanente Colorado, Kaiser Permanente Northwest (NW Oregon and SW Washington State) and Fallon Community Health Plan (Central MA). These 4 sites provide care for an ethnically and socio-demographically diverse population and to commercially insured individuals as well as patients insured by Medicare, Medicaid, state-specific gap programs and other financing arrangements. Each of these sites has developed a Virtual Data Warehouse (VDW) which served as the primary source of data for subject identification and characterization.11
The institutional review boards at participating sites approved the study and waiver of consent was obtained due to the nature of the study.
Study Population
The study population included 37,054 patients aged ≥21 years with diagnosed HF between January 1, 2005 and December 31, 2008. Diagnosis of HF was based on either having been hospitalized with a primary discharge diagnosis of HF and/or having ≥3 ambulatory visits coded for HF with at least one being with a cardiologist. The following International Classification of Disease, 9th Edition (ICD-9) codes to identify HF: 398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 428.0, 428.1, 428.21, 428.22, 428.23, 428.30, 428.31, 428.32, 428.33, 428.40, 428.41, 428.42, 428.43, and 428.9. Prior studies have shown a positive predictive value of >95% for admissions with a primary discharge diagnosis of HF based on these codes when compared to chart review and Framingham clinical criteria.12–14 Our sample included both incident and prevalent cases of HF. We defined prevalent HF as having any hospitalization or ambulatory HF diagnosis before the index date.
Assessments of Left Ventricular Systolic Function
Information on quantitative and/or qualitative assessments of left ventricular systolic function were abstracted from results of echocardiograms, nuclear imaging, and left ventriculography from health plan databases and complemented by manual review of electronic health records. We defined preserved ejection fraction as either left ventricular ejection fraction ≥50% and/or a physician’s qualitative determination of normal or preserved ejection fraction; reduced ejection fraction was defined as left ventricular ejection fraction <50%. When multiple studies were available, we used results nearest to the date of diagnosis of HF during the study period.
Selection of Comorbidities
Information on coexisting illnesses at the time of HF diagnosis was based on diagnoses and procedures mapped to relevant ICD-9 codes.15 Following the approach used in previous work,16–18 we focused on the most common co-existing conditions in the cohort, defined as those with a prevalence rate of >3%. Conditions included in the present analysis included: hypertension, dyslipidemia, visual impairment, lung disease, atrial fibrillation/atrial flutter, aortic valvular disease, cerebrovascular disease (includes ischemic stroke, transient ischemic attack and cerebrovascular disease), diabetes mellitus, hearing impairment, coronary heart disease (CHD, includes myocardial infarction and unstable angina), depression, dementia, peripheral arterial disease, cancer, thromboembolic disorder, gastrointestinal hemorrhage, ventricular fibrillation/ventricular tachycardia, based on previously described ICD-9 and CPT procedure codes.15 (See appendix for full list of ICD-9 codes used to identify comorbidities) Based on laboratory values, we also included the presence of anemia (hemoglobin <13.0 g/L in men and <12.0 g/L in women).
The Charlson Deyo- Comorbidity index, a weighted sum of medical conditions (scored 0–37) with higher scores representing more comorbidity, was also calculated.19
Statistical Analysis
The comorbidities were summed to provide a description of the average number of comorbidities in the entire cohort and stratified by LVEF. We report age and sex adjusted prevalence rates for comorbidites stratified by preserved and reduced left ventricular systolic function. We report the most frequently occurring (>10% in overall sample) combinations of two and three conditions stratified by age and left ventricular systolic function category. We also compared to observed prevalence of commonly occurring combinations of conditions with the expected prevalence [calculated as (prevalence of comorbidity A) x (prevalence of comorbidity B)17]. The interpretation of these descriptive statistics, and their ratio (observed prevalence/expected prevalence) reflects, in part, how related the conditions are to one another. We used the ratio of observed to expected prevalence to put the co-occurrence of conditions into context with respect to how more or less they are occurring than would be expected. Observed and expected prevalence rates would be equal if the conditions were independent and occurred as often as expected by chance alone. Observed prevalence is higher than expected prevalence when there is a physiologic link between the conditions and the conditions co-occur more often than would be expected by chance.
RESULTS
We identified 23,435 adults ≥65 years with HF between 2005 and 2008 with left ventricular systolic function data available. The mean age of the sample was 78.9 years (range 65 – 106 years), 48.6% were women and 80% were White. (Table 1) Approximately half of the sample (12,407; 52.9%) had HF-P.
Table 1.
Baseline Characteristics (Demographics and Comorbidities) Overall and According to Left Ventricular Ejection Fraction Category.
| Overall Sample N = 23,435 |
Preserved Ejection Fraction N = 12,407 |
Reduced Ejection Fraction N = 11,028 |
P Value | |
|---|---|---|---|---|
| Demographic variables | ||||
| Age, mean (standard deviation) | 73.7±12.4 | 75.6±11.6 | 71.8±12.8 | <0.001 |
| Age, n (%) | ||||
| 65 – 74 | 7,274 (31.0) | 3,413 (27.5) | 3,861(35.0) | <0.001 |
| 75 −84+ | 10,405 (44.4) | 5,584 (45.0) | 4,821(43.7) | |
| 85+ | 5,756 (24.6) | 3,410 (27.5) | 2,346 (21.3) | |
| Female gender, n (%) | 11,389 (48.6) | 7,409 (61.2) | 3,980 (36.1) | <0.001 |
| Race, % | ||||
| White | 18,580 (79.3) | 9,925 (80.0) | 8,655 (78.4) | |
| Black | 1,404(5.99) | 691(5.57) | 713(6.47) | |
| Other | 1,264(5.39) | 699(5.63) | 565(5.12) | |
| Unknown | 2,187(9.33) | 1,092(8.8) | 1,095(9.93) | <0.001 |
| Number of Comorbidities | ||||
| Mean (standard deviation) | 4.5 (2.2) | 4.5 (2.2) | 4.4 (2.2) | 0.002 |
| Median (25%, 75%) | 4 (3,6) | 4 (3,6) | 4 (3,6) | |
| Charlson Score (range 0–37) | ||||
| Mean (standard deviation) | 2.4 (2.1) | 2.5 (2.1) | 2.4 (2.1) | <0.001 |
| Median (25%, 75%) | 2.0 (1,3) | 2.0 (1,4) | 2.0 (1,4) | |
| Medical History of Comorbidities, (%)a | ||||
| Hypertension | 58.9 | 58.5 | 59.5 | 0.12 |
| Anemia | 55.8 | 59.8 | 52.1 | <0.001 |
| Dyslipidemia | 44.6 | 43.0 | 46.8 | <0.001 |
| Visual Impairments | 43.2 | 43.0 | 43.3 | 0.65 |
| Lung Diseaseb | 30.9 | 32.6 | 28.9 | <0.001 |
| Atrial Fibrillation / Atrial Flutter | 25.3 | 28.2 | 22.1 | <0.001 |
| Aortic Valvular Disease | 22.9 | 24.1 | 21.6 | <0.001 |
| Cerebrovascular Diseasec | 22.8 | 23.0 | 22.4 | 0.28 |
| Hearing Impairment | 21.7 | 22.7 | 20.3 | <0.001 |
| Diabetes Mellitus | 19.2 | 19.3 | 19.1 | 0.71 |
| CHD (AMI/Unstable Angina) | 18.9 | 16.1 | 22.4 | <0.001 |
| Depression | 17.5 | 17.7 | 17.2 | 0.32 |
| Dementia | 13.8 | 13.9 | 13.4 | 0.27 |
| Peripheral Arterial Disease | 9.8 | 9.9 | 9.5 | 0.31 |
| Cancer | 7.8 | 8.3 | 7.4 | 0.012 |
| Thromboembolic Disorderd | 6.9 | 6.8 | 7.3 | 0.14 |
| Gastrointestinal hemorrhage | 5.8 | 6.5 | 5.0 | <0.001 |
| V. Fibrillation / V. Tachycardia | 3.1 | 1.7 | 4.3 | <0.001 |
Age and sex adjusted prevalence rates;
Based on inpatient primary discharge diagnosis or outpatient diagnosis 490–496; 518
Includes ischemic stroke, transient ischemic attack, and cerebrovascular disease;
Based on inpatient primary discharge diagnoses: 440.0, 444.1, 444.21, 444.22, 444.81, 444.89, 557.0, 557.1, 557.9
We examined overall comorbidity burden in two ways: 1.The Charlson-Deyo Comorbidity Index and 2. a simple count of previously described conditions. Comorbidity burden as assessed by the Charlson-Deyo Comorbidity Index differed significantly by whether HF was with preserved or reduced systolic function (mean Charlson score 2.5 vs 2.4; p<0.001). (Table 1) When we examined comorbidity burden as a count of conditions, we found a high burden of comorbidity in the cohort. On average, patients with HF had 4.5 additional comorbidities. Women had a significantly higher burden of comorbidity than men (mean of 4.5 vs. 4.4 additional comorbidities; p<0.001). Patients with HF-P had an average of 4.5 additional comorbidities while patients with HF-R had an average of 4.4 comorbidities (p=<0.001). The average number of comorbidities did not vary significantly by gender among patients with HF-P (women: 4.6, men: 4.5, p=0.11) but women with HF-R had significantly more comorbidities than men with HF-R (4.4 vs. 4.3, p=0.016).
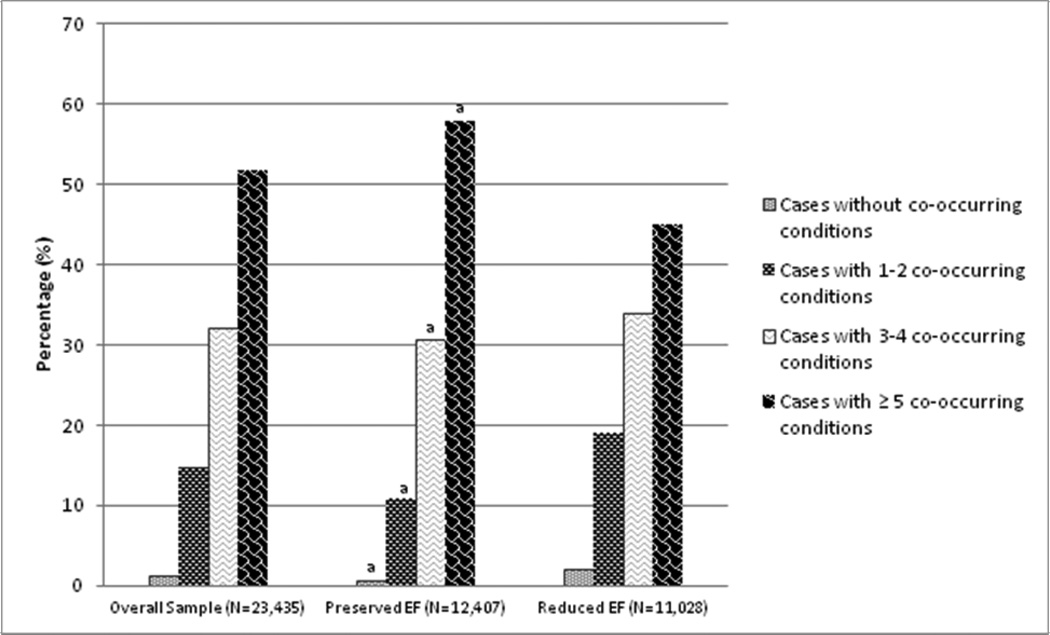
Less than 2% of older patients with HF had no co-occurring conditions, approximately 15% had 1–2 additional diseases in addition to HF, one third had 3–4 additional diseases and approximately one half had five or more additional conditions in addition to HF. (Figure 1) Using the condition count approach, the degree of comorbidity burden differed significantly among patients with HF-P vs. HF-R. Specifically, patients with HF-P were significantly less likely than those with HF-R to have 1–2 co-occurring conditions (11% vs 19%) and 3–4 co-occurring conditions (30% vs. 34%) but were significantly more likely to have 5 or more co-occurring conditions (58% vs 45%, all age and sex adjusted p values were <0.001). (Figure 1)
Figure 1. Degree of comorbidity and multi-morbidity in patients with heart failure.
Legend: Note: EF: Ejection Fraction
aAge and sex adjusted p<0.0001 when compared to Reduced EF
aAdjusted for age and sex p< 0.05 when compared to Reduced EF
bAdjusted for age and sex p<<0.0001 when compared to Reduced EF
We also examined the age and sex-adjusted occurrence of specific comorbidities. Hypertension, anemia, dyslipidemia and visual impairments were the most common comorbidities, experienced by approximately one half of the cohort. Several comorbidities that are not typically considered in the context of studies of HF patients were present in >10% of the population including hearing impairment (21.7%), depression (17.5%) and dementia (13.8%).
In general, most of the comorbidities we examined were significantly more likely to be present in patients with HF-P than they were in those with HF-R when adjusted for age and sex. (Table 1) Several cardiac and vascular disease-related conditions were significantly more likely to be present in patients with HF-P as compared to those with HF-R such as: atrial fibrillation/atrial flutter (28.2% vs.22.1%), aortic valvular disease (24.1% vs.21.6% all p’s <0.001). In addition, comorbidities less frequently considered in HF patients were also more common in patients with HF-P than in those with HF-R including anemia (59.8 vs. 52.1), cancer (8.3% vs.7.4%) and hearing impairment (22.7% vs.20.3%, all p’s<0.05). Dyslipidemia, CHD, and ventricular fibrillation/ventricular tachycardia were more commonly present in patients with HF-R than in those with HF-P. (Table 1) The prevalence of several comorbidities (hypertension, visual impairments, cerebrovascular disease, diabetes, and peripheral arterial disease) did not differ according to whether left ventricular systolic function was preserved or reduced.
Prevalence of the most frequently co-occurring comorbidity combinations (those occurring in >10% of the cohort) are reported for the total sample and also stratified by left ventricular systolic function, age and sex in Table 2. For a number of the comorbidity pairs, the ratio of observed to expected prevalence was >1.0 (data not shown), indicating that the comorbidities examined co-occurred at a rate higher than expected by chance alone. For example, diabetes and hypertension co-occurred in 14.2% of the cohort, 25% more often than expected. Hypertension and dyslipidemia occurred in nearly one third of the sample, 21% more often than expected. In most cases, this was not unexpected given that many of the comorbidities examined are vascular or cardiac-related conditions.
Table 2.
Prevalence of most frequent groups of co-occurring conditions with heart failure stratified by left ventricular ejection fraction category and age. (N=23,435)
| Overall Sample |
Left Ventricular Ejection Fraction |
Age, Years | Gender | |||||
|---|---|---|---|---|---|---|---|---|
| Comorbidity Group | N=23,435 | Preserved n=12,407 |
Reduced n=11,028 |
65–74 n=7,274 |
75–84 n=10,405 |
≥85 n=5,756 |
Male n=12,04 7 |
Female n=11,38 9 |
| Anemia & Hypertension | 32.1 | 34.6 | 29.3 | 29.2 | 32.5 | 35.1 | 28.6 | 35.9 |
| Hypertension & Dyslipidemia |
31.7 | 30.0 | 33.7 | 35.6 | 32.0 | 26.3 | 33.2 | 30.2 |
| Visual Impairment & Hypertension |
29.8 | 29.6 | 30.0 | 30.1 | 31.1 | 27.1 | 30.5 | 29.1 |
| Anemia & Dyslipidemia | 24.7 | 26.0 | 23.3 | 23.8 | 24.4 | 26.3 | 21.3 | 28.3 |
| Anemia & Vision Impairment | 23.2 | 25.3 | 20.8 | 20.9 | 23.8 | 24.9 | 20 | 26.5 |
| Visual Impairment & Dyslipidemia |
22.6 | 21.4 | 24.1 | 24.7 | 23.2 | 18.9 | 23.3 | 21.9 |
| Hypertension & Lung Disease | 19.8 | 20.4 | 19.1 | 21.4 | 20.9 | 16.0 | 20.1 | 19.5 |
| Hypertension & Visual Impairment & Dyslipidemia |
17.7 | 16.9 | 18.7 | 19.4 | 18.3 | 14.5 | 18.4 | 17 |
| Hypertension & Anemia & Dyslipidemia |
17.5 | 18.1 | 16.8 | 17.5 | 17.5 | 17.3 | 15.9 | 19.2 |
| Anemia & Lung Disease | 17.1 | 19.5 | 14.5 | 15.7 | 17.8 | 17.8 | 14.5 | 20 |
| Hypertension & Anemia & Visual Impairment |
15.9 | 17.2 | 14.5 | 14.7 | 16.4 | 16.6 | 14.1 | 17.9 |
| Visual Impairment & Lung Disease |
15.2 | 15.4 | 14.8 | 16.3 | 16.1 | 12.0 | 15.2 | 15.1 |
| Dyslipidemia & Lung Disease | 15.1 | 14.9 | 15.2 | 17.4 | 15.6 | 11.2 | 15.1 | 15.1 |
| Aortic Valvular Disease & Hypertension |
14.8 | 15.4 | 14.2 | 13.8 | 16.4 | 13.4 | 14.7 | 15 |
| Stroke & Hypertension | 14.7 | 14.4 | 15.0 | 13.4 | 15.8 | 14.2 | 15.5 | 13.9 |
| Atrial Fibrillation/Flutter & Anemia |
14.5 | 17.7 | 11.0 | 38.7 | 14.9 | 19.5 | 12 | 17.2 |
| Atrial Fibrillation/Flutter & Hypertension |
14.5 | 16.2 | 12.5 | 11.5 | 15.4 | 16.6 | 13.6 | 15.4 |
| Diabetes & Hypertension | 14.2 | 13.8 | 14.7 | 17.3 | 14.3 | 10.1 | 15.2 | 13.1 |
| Anemia & Stroke | 14.0 | 15.5 | 12.3 | 11.4 | 14.4 | 16.4 | 12.4 | 15.6 |
| Diabetes & Dyslipidemia | 13.4 | 13.0 | 14.0 | 16.6 | 13.0 | 10.2 | 14 | 12.8 |
| Hearing Impairment & Hypertension |
13.3 | 13.9 | 12.6 | 10.3 | 14.0 | 15.7 | 14.4 | 12.1 |
| Anemia & Aortic Valvular Disease |
12.9 | 14.7 | 10.9 | 10.1 | 14.0 | 14.6 | 10.9 | 15 |
| Anemia & Hearing Impairment | 12.3 | 14.2 | 10.2 | 7.4 | 12.7 | 17.9 | 11.1 | 13.7 |
| Anemia & Visual Impairment & Dyslipidemia |
12.1 | 12.6 | 11.5 | 11.7 | 12.3 | 12.2 | 10.6 | 13.7 |
| CHD & Hypertension | 12.1 | 9.8 | 14.6 | 13.7 | 12.3 | 9.5 | 13.6 | 10.5 |
| Anemia & CHD | 11.9 | 10.5 | 13.5 | 12.1 | 12.3 | 11.1 | 11.6 | 12.3 |
| Visual Impairment & Aortic Valvular Disease |
11.5 | 11.8 | 11.1 | 10.6 | 12.7 | 10.2 | 11.2 | 11.7 |
| Depression & Hypertension | 11.4 | 11.7 | 11.1 | 12.7 | 11.9 | 9.0 | 9.9 | 13.1 |
| Stroke & Dyslipidemia | 11.4 | 11.2 | 11.7 | 10.6 | 12.0 | 11.3 | 11.5 | 11.2 |
| Hypertension & Dyslipidemia & Lung Disease |
11.3 | 11.2 | 11.5 | 13.3 | 11.9 | 7.7 | 11.6 | 11 |
| Visual Impairment & Diabetes | 11.0 | 11.0 | 11.0 | 12.8 | 11.4 | 8.0 | 11.6 | 10.4 |
| Hypertension & Visual Impairment & Lung Disease |
11.0 | 11.2 | 10.7 | 11.8 | 11.7 | 8.5 | 11.1 | 10.8 |
| Hypertension & Diabetes & Dyslipidemia |
10.9 | 10.4 | 11.3 | 13.9 | 10.5 | 7.6 | 11.4 | 10.2 |
| CHD & Dyslipidemia | 10.8 | 8.6 | 13.3 | 12.3 | 10.6 | 9.4 | 11.6 | 10 |
| Stroke & Visual Impairment | 10.8 | 10.7 | 10.9 | 9.6 | 11.9 | 10.3 | 11.2 | 10.3 |
| Hypertension & Anemia & Lung Disease |
10.8 | 12.0 | 9.5 | 10.2 | 11.6 | 10.1 | 9.5 | 12.2 |
| Anemia & Diabetes | 10.7 | 11.7 | 9.6 | 10.8 | 11.0 | 10.1 | 9.8 | 11.7 |
| Atrial Fibrillation/Flutter & Visual Impairment |
10.7 | 11.9 | 9.3 | 8.7 | 11.6 | 11.5 | 9.9 | 11.5 |
| Atrial Fibrillation/Flutter & Dyslipidemia |
10.7 | 11.9 | 9.2 | 9.4 | 11.2 | 11.4 | 9.8 | 11.6 |
| Aortic Valvular Disease & Dyslipidemia |
10.7 | 11.9 | 9.2 | 11.2 | 12.5 | 9.6 | 11.2 | 11.6 |
| Anemia & Depression | 10.5 | 11.9 | 8.8 | 10.1 | 10.8 | 10.4 | 7.3 | 13.8 |
| Visual Impairment & Hearing Impairment |
10.2 | 10.3 | 10.2 | 7.8 | 11.1 | 11.9 | 10.9 | 9.5 |
In general, prevalence of comorbidity pairs were similar among patients with preserved and reduced systolic function. (Table 2) Although the prevalence of a number of comorbidity pairs increased with age in many cases, this pattern was not evident across all pairs. (Table 2) In a number of cases, prevalence rates of the comorbidity pairs was highest in the youngest age group, likely reflecting a survivor bias (e.g., 38.7% of those 65–74 years, compared with 19.5% of those ≥85 years, had atrial fibrillation/atrial flutter and anemia). In general, the prevalence of comorbidity pairs was higher in women than in men, particularly when anemia was one of the comorbidities (Table 2). The combinations of comorbidities that were higher in prevalence among men than women typically included either hypertension or diabetes.
There were also several sets of comorbidity triads that occurred in more than 10% of the sample. (Table 2) For example, hypertension, visual impairment and dyslipidemia occurred in 17.7% of the cohort, 56% more often than expected; anemia, visual impairment and dyslipidemia occurred in 12%, 12% more often than expected; and hypertension, diabetes and dyslipidemia occurred in 17.7% of the cohort, more than 60% as often as expected.
DISCUSSION
We found a slightly higher rate of comorbidity and multi-morbidity among patients with HF-P, but few differences in the way that groups of conditions clustered together in patients with HF-P vs. HF-R. These findings add to the growing literature on the complex older patient, and the often narrow focus on a single medical condition (e.g., HF) that characterizes specialty care and many disease management programs.1, 2, 16, 20, 21
Increasing attention has been given to the ever growing numbers of older persons with multiple coexisting chronic medical conditions, and this is now recognized as a critical issue in the care of older patients, both at the individual and population levels.1 Comorbidity is especially important in chronic conditions with increasing survival rates, such as HF, where rates of comorbidity are increasing.6 Comorbidity in patients with HF increases the risk for hospitalization, polypharmacy and death.6, 22–24 Importantly, both cardiac and non-cardiac comorbidity is high in patients with HF and both are associated poor outcomes.22, 23, 25–27The majority of studies of comorbidity in patients with HF have focused on the group of HF patients as a whole or have stratified comorbidity rates by age.6, 23, 25, 26 Patterns of the co-occurrence of additional comorbidities have not been compared in patients with HF with preserved and reduced systolic function.
Characterizing multiple conditions that frequently co-occur in patients HF-P and HF-R may help explain differences in treatment and inform the design of clinical trials and of clinical guidelines that are directly relevant to these complex patients. Understanding how chronic conditions co-occur in patients with HF would also be helpful in the composition and training of providers in the medical home for HF.28 Complex comorbidity is also associated with adverse drug events caused by drug-drug interactions.29 Review of medications and potential for drug-drug or drug-disease interactions are important components of quality improvement initiatives in patients with multiple co-existing conditions. Since many of the commonly occurring comorbidity groups identified were non-intuitive (i.e., combination of cardiovascular and non-cardiovascular comorbidity), potentially important drug-drug and drug-disease interactions may be overlooked, particularly when prescribed by multiple providers.
A recent meta-analysis of 31 studies including nearly 42,000 patients found that, compared to patients with HF-R, patients with HF-P were older, more often female and more likely to have a history of hypertension and atrial fibrillation and were less likely to have a history of myocardial infarction and diabetes.30 Non-cardiac comorbidities were not assessed and total comorbidity burden (presence of multiple comorbidities) was not reported in this meta-analysis. Because patients with HF-P are, on average, older than those with HF-R, we hypothesized that patients with preserved EF would have higher comorbidity burden. We found that there was a slightly higher overall comorbidity burden in patients with HF-P, but that the occurrence of several non-cardiac comorbidities, such as anemia and hearing impairment were significantly higher among patients with HF-P after age and sex adjustment. These results likely reflect the demographics of the group and are similar to the findings from a recent study which examined comorbidity in HF stratified by age: older patients had significantly more non-cardiac comorbidities than younger patients.25
We also examined which comorbidities most commonly co-occurred in the cohort. We found that the most common pairs of co-occurring conditions included cardiovascular and non-cardiovascular comorbidities. For instance, hypertension and dyslipidemia co-occurred in nearly one third of the cohort and hypertension and visual impairment co-occurred in more than one quarter of the cohort. In general, the comorbidity pairs occurred at rates higher than would be expected by chance. In general, results were similar in patients with HF-P and HF-R, but prevalence of comorbidity pairs did not uniformly increase with age.
Our findings suggest a lack of variability in the overall burden of comorbidity and in the co-occurrence of specific conditions in patients with HF-P vs. HF-R. Factors other than comorbidity are the likely drivers of clinical differences observed between these two discrete patient groups, perhaps reflecting pathophysiologic differences between the two conditions.7, 8, 30
Our results are strengthened by the large, ethnically diverse study sample that included HF patients cared for in a variety of clinical and geographically diverse practice settings. We used a standardized data resource with extensive health care utilization information, including outpatient visits as well as health plan and non health plan hospitalizations. Although we had extensive standardized electronic diagnosis and procedure data with which to characterize comorbidity, we do not have data on a few potentially important comorbidities including obesity and arthritis. In addition, were limited in our ability to identify comorbidities based on laboratory values and thus have missing data for potentially important comorbidities defined by lab values, such as renal function. Several of the comorbidities included in our study were likely under-reported in administrative data, such as dementia and depression, thus our estimates may be conservative.31, 32 In addition, due to the large cohort size, some associations may have been statistically, but not clinically, significant. Although our findings represent four geographically diverse health plans, our findings may not be generalizable to uninsured populations.
Clinical care of patients with multi-morbidity is complex. These patients are often excluded from clinical trials, resulting in a lack of information on which to base clinical decision-making. When guidelines do exist for co-occurring conditions, they are typically focused on a single additional condition,33 not multiple co-occurring conditions as is frequently the case in patients with HF.6 In addition, guidelines for treatment of specific co-occurring conditions may conflict with each other or it may be difficult to implement treatments simultaneously. Understanding which sets of conditions most commonly co-occur with heart failure may help identify candidate groups for clinical trials to better understand HF treatment in the setting of other conditions. Future risk prediction work should consider not just single comorbidities but also the co-occurrence of multiple comorbidities. Our study revealed a number of conditions that frequently co-occur in patients, with HF with both preserved and reduced left ventricular systolic function, representing large and clinically challenging subgroups of patients with HF, to which future research efforts deserve to be directed.
ACKNOWLEDGMENTS
This study was conducted within the Cardiovascular Research Network, a consortium of research organizations affiliated with the HMO Research Network and sponsored by the National Heart Lung and Blood Institute (NHLBI) (U19 HL91179–01). This study was funded by 1RC1HL099395 from the National Heart Lung and Blood Institute. Dr. Saczynski was supported in part by funding from the National Institute on Aging (K01AG33643). Drs. Saczynski, McManus, Goldberg and Gurwitz were supported in part by funding from the NHLBI (U01HL105268).
Sponsor’s Role: The sponsor had no role in the design, methods, subject recruitment, data collections, analysis and preparation of paper.
Appendix A
Study Comorbidity Definitions.
| Comorbidity | Codes | Algorithm |
|---|---|---|
| Hypertension | ICD-9 codes: 401.X, 402.X, 403.X, 404.X, 405.X |
>= 2 outpatient diagnoses of hypertension or >= 1 outpatient diagnosis of hypertension plus >1 anti-hypertensive drug prescription fill within one year of outpatient diagnosis |
| Dyslipidemia | ICD-9 code 272 AHFS Therapeutic Class: 240604, 240605, 240606, 240608, 240692, 562400, 800000, 880800 |
>=1 prescription for lipid-lowering drug or >=1 outpatient diagnosis of dyslipidemia |
| Visual Impairments | ICD-9 codes 360–379.99 | |
| Lung Disease | ICD-9 Codes: 490, 491, 492, 493, 494, 495, 496, 518 |
inpatient primary discharge or outpatient diagnosis |
| Cerebrovascular | ICD-9 Codes: 430, 431, 432, 432.0, | Based on inpatient (principal discharge) and ED diagnosis |
| Disease | 432.1, 432.9, 433.X1, 434.X1, 435.X, 436.0, 438.X |
|
| Diabetes Mellitus | ICD-9 code 250.X | Identified based on pharmacy information and/or inpatient and /or outpatient diagnosis. Primary inpatient discharge diagnoses AND/OR >= 2 outpatient diagnoses AND/OR >=1 dispensed prescription for an antidiabetic drug Exclusion criteria: Patient diagnosed with gestational diabetes within 8 months from inpatient or outpatient diagnoses of DM (ICD-9 codes for gestational diabetes: 648.80, 648.81, 648.82, 648.83, 648.84, 790.21, 790.22, 790.29) AND/OR Women only receiving Metformin or Thiazolidinedione with no inpatient or outpatient diagnosis of DM within 2 years. |
| Hearing Impairment | ICD-9 codes 387 – 389.99 | |
| CHD (AMI/Unstable Angina) | ICD-9 codes: 410.X, 411.X, 414.X | Principal discharge diagnosis or Principal discharge diagnosis ICD-9 code of 411.x, or the combination of a principal discharge diagnosis ICD-9 code 414.x plus a secondary discharge diagnosis ICD-9 code 411.x |
| Dementia | ICD-9 Codes 290, 294, 331, 292.2, 292.82 |
Based only on outpatient diagnosis |
| Cancer | Systemic Cancer from Cancer Registry (all malignancies other than non-melanoma skin cancers) | |
| Thromboembolic Disorder |
ICD-9 Codes 440.0, 444.1, 444.21, 444.22, 444.81, 444.89, 557.0, 557.1, 557.9 |
Identified based on inpatient primary discharge diagnosis |
| Gastrointestinal Hemorrhage |
ICD-9 Codes 455.2, 455.5, 455.8, 456.0, 456.20, 530.7, 530.82, 531.00, 531.01, 531.20, 531.21, 531.40, 531.41, 531.60, 531.61 , 532.00, 532.01, 532.20, 532.21, 532.40, 532.41, 532.60, 532.61, 533.00, 533.01, 533.20, 533.21, 533.40, 533.41, 533.60, 533.61, 534.00, 534.01, 534.20, 534.21, 534.40, 534.41 , 534.60, 534.61, 535.01, 535.11, 535.21, 535.31, 535.41, 535.51, 535.61, 537.83, 562.02, 562.03, 562.12, 562.13, 568.81, 569.3, 569.85, 578.0, 578.1, 578.9 |
Identified based on inpatient primary discharge diagnosis |
Footnotes
Conflict of Interest: The authors have no conflicts to report (please see attached grid)
Author Contributions:
Ms. Ogarek: analysis and interpretation of data, revising manuscript critically for important intellectual content, and final approval of the version to be published.
Drs. Saczynski, Go, Magid, Smith, McManus, Allen, Goldberg and Gurwitz: conception and design, drafting the article or revising paper critically for important intellectual content and final approval of the version to be published.
REFERENCES
- 1.Parekh AK, Barton MB. The challenge of multiple comorbidity for the US health care system. JAMA. 2010;303:1303–1304. doi: 10.1001/jama.2010.381. [DOI] [PubMed] [Google Scholar]
- 2.Vogeli C, Shields AE, Lee TA, et al. Multiple chronic conditions: prevalence, health consequences, and implications for quality, care management, and costs. J Gen Intern Med. 2007;22(Suppl 3):391–395. doi: 10.1007/s11606-007-0322-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wolff JL, Starfield B, Anderson G. Prevalence, expenditures, and complications of multiple chronic conditions in the elderly. Arch Intern Med. 2002;162:2269–2276. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]
- 4.Anderson G. Chronic conditions: Making the case for ongoing care. Johns Hopkins University; [Google Scholar]
- 5.Liu L. Changes in cardiovascular hospitalization and comorbidity of heart failure in the United States: Findings from the National Hospital Discharge Surveys 1980–2006. Int J Cardiol. 2011;149:39–45. doi: 10.1016/j.ijcard.2009.11.037. [DOI] [PubMed] [Google Scholar]
- 6.Wong CY, Chaudhry SI, Desai MM, et al. Trends in comorbidity, disability, and polypharmacy in heart failure. Am J Med. 2011;124:136–143. doi: 10.1016/j.amjmed.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Owan TE, Hodge DO, Herges RM, et al. Trends in Prevalence and Outcome of Heart Failure with Preserved Ejection Fraction. N Engl J Med. 2006;355:251–259. doi: 10.1056/NEJMoa052256. [DOI] [PubMed] [Google Scholar]
- 8.Bhatia RS, Tu JV, Lee DS, et al. Outcome of heart failure with preserved ejection fraction in a Population-Based Study. N Engl J Med. 2006;355:260–269. doi: 10.1056/NEJMoa051530. [DOI] [PubMed] [Google Scholar]
- 9.Lee TA, Shields AE, Vogeli C, et al. Mortality rate in veterans with multiple chronic conditions. J Gen Intern Med. 2007;22(Suppl 3):403–407. doi: 10.1007/s11606-007-0277-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Go AS, Yang J, Gurwitz JH, et al. Comparative effectiveness of different beta-adrenergic antagonists on mortality among adults with heart failure in clinical practice. Arch Intern Med. 2008;168:2415–2421. doi: 10.1001/archinternmed.2008.506. [DOI] [PubMed] [Google Scholar]
- 11.Magid DJ, Gurwitz JH, Rumsfeld JS, et al. Creating a research data network for cardiovascular disease: The CVRN. Expert Rev Cardiovasc Ther. 2008;6:1043–1045. doi: 10.1586/14779072.6.8.1043. [DOI] [PubMed] [Google Scholar]
- 12.Go AS, Lee WY, Yang J, et al. Statin therapy and risks for death and hospitalization in chronic heart failure. JAMA. 2006;296:2105–2111. doi: 10.1001/jama.296.17.2105. [DOI] [PubMed] [Google Scholar]
- 13.Go AS, Yang J, Ackerson LM, et al. Hemoglobin level, chronic kidney disease, and the risks of death and hospitalization in adults with chronic heart failure: The Anemia in Chronic Heart Failure: Outcomes and Resource Utilization (ANCHOR) Study. Circulation. 2006;113:2713–2723. doi: 10.1161/CIRCULATIONAHA.105.577577. [DOI] [PubMed] [Google Scholar]
- 14.McKee PA, Castelli WP, McNamara PM, et al. The natural history of congestive heart failure: the Framingham study. N Engl J Med. 1971;285:1441–1446. doi: 10.1056/NEJM197112232852601. [DOI] [PubMed] [Google Scholar]
- 15.Go AS, Chertow GM, Fan D, et al. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 16.Boyd CM, Ritchie CS, Tipton EF, et al. From bedside to bench: summary from the American Geriatrics Society/National Institute on Aging Research Conference on Comorbidity and Multiple Morbidity in Older Adults. Aging Clin Exp Res. 2008;20:181–188. doi: 10.1007/bf03324775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marengoni A, Rizzuto D, Wang H-X, et al. Patterns of chronic multimorbidity in the elderly population. J Am Geriatr Soc. 2009;57:225–230. doi: 10.1111/j.1532-5415.2008.02109.x. [DOI] [PubMed] [Google Scholar]
- 18.Marengoni A, Winblad B, Karp A, et al. Prevalence of chronic diseases and multimorbidity among the elderly population in Sweden. Am J Public Health. 2008;98:1198–1200. doi: 10.2105/AJPH.2007.121137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 20.McCall N, Cromwell J. Results of the Medicare Health Support disease-management pilot program. N Engl J Med. 2011;365:1704–1712. doi: 10.1056/NEJMsa1011785. [DOI] [PubMed] [Google Scholar]
- 21.Yancik R, Ershler W, Satariano W, et al. Report of the national institute on aging task force on comorbidity. J Gerontol A Biol Sci Med Sci. 2007 Mar;62(3):275–280. doi: 10.1093/gerona/62.3.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ahluwalia SC, Gross CP, Chaudhry SI, et al. Impact of Comorbidity on Mortality Among Older Persons with Advanced Heart Failure. J Gen Intern Med. 2011 Nov 18; doi: 10.1007/s11606-011-1930-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Braunstein JB, Anderson GF, Gerstenblith G, et al. Noncardiac comorbidity increases preventable hospitalizations and mortality among Medicare beneficiaries with chronic heart failure. J Am Coll Cardiol. 2003;42:1226–1233. doi: 10.1016/s0735-1097(03)00947-1. [DOI] [PubMed] [Google Scholar]
- 24.Masoudi FA, Krumholz HM. Polypharmacy and comorbidity in heart failure. BMJ. 2003;327:513–514. doi: 10.1136/bmj.327.7414.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ahluwalia SC, Gross CP, Chaudhry SI, et al. Change in comorbidity prevalence with advancing age among persons with heart failure. J Gen Intern Med. 2011;26:1145–1151. doi: 10.1007/s11606-011-1725-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boyd CM, Leff B, Wolff JL, et al. Informing clinical practice guideline development and implementation: Prevalence of coexisting conditions among adults with coronary heart disease. J Am Geriatr Soc. 2011;59:797–805. doi: 10.1111/j.1532-5415.2011.03391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lang CC, Mancini DM. Non-cardiac comorbidities in chronic heart failure. Heart. 2007;93:665–671. doi: 10.1136/hrt.2005.068296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Konstam MA, Greenberg B. Transforming health care through the medical home: The example of heart failure. J Cardiac Failure. 2009;15:736–738. doi: 10.1016/j.cardfail.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 29.Obreli-Neto PR, Nobili A, de Oliveira Baldoni A, et al. Adverse drug reactions caused by drug-drug interactions in elderly outpatients: A prospective cohort study. Eur J Clin Pharmacol. 2012 May 30; doi: 10.1007/s00228-012-1309-3. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 30.Meta-analysis Global Group in Chronic Heart Failure (MAGGIC) The survival of patients with heart failure with preserved or reduced left ventricular ejection fraction: An individual patient data meta-analysis. Eur Heart J. 2012;33:1750–1757. doi: 10.1093/eurheartj/ehr254. [DOI] [PubMed] [Google Scholar]
- 31.Glasser M, Stearns JA, de Kemp E, et al. Dementia and depression symptomatology as assessed through screening tests of older patients in an outpatient clinic. Fam Pract Res J. 1994;14:261–272. [PubMed] [Google Scholar]
- 32.Joray S, Wietlisbach V, Bula CJ. Cognitive impairment in elderly medical inpatients: detection and associated six-month outcomes. Am J Geriatr Psychiatry. 2004;12:639–647. doi: 10.1176/appi.ajgp.12.6.639. [DOI] [PubMed] [Google Scholar]
- 33.Boyd CM, Darer J, Boult C, et al. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: Implications for pay for performance. JAMA. 2005;294:716–724. doi: 10.1001/jama.294.6.716. [DOI] [PubMed] [Google Scholar]