Abstract
Introduction:
To examine the extent to which cigarette smoking in adolescence is associated with maladaptive versus adaptive coping behaviors in adulthood.
Method:
The data came from a longitudinal study of New Zealand adolescents followed into adulthood at age 32 years. Using structural equation modeling (SEM), we examined the predictive association between daily smoking of cigarettes and symptoms of tobacco dependence from 18 to 26 years of age and later coping at age 32 years. We included pathways from childhood family disadvantage in addition to both adolescent stress–worry and adult coping in the model.
Results:
SEM revealed that cigarette smoking had a small but direct inverse effect on later adaptive coping (−.14) and a direct effect on maladaptive coping (.23) independent of the relationships between adolescent coping and stress–worry and later adult coping.
Conclusions:
The findings are consistent with the hypothesis that tobacco smoking may inhibit the development of self-efficacy or one’s ability to act with appropriate coping behaviors in any given situation.
INTRODUCTION
It is well established that smokers have higher rates of mental health problems such as depression and anxiety than the general population (Degenhardt, Lynskey, & Hall, 2000; Fergusson, Goodwin, & Horwood, 2003; McGee & Williams, 2006; Morrell & Cohen, 2006). The direction of causality indicates that there is a modest association between smoking and subsequent increases in psychological distress, including depressed mood (Carter, ven der Deen, Wilson, & Blakely, 2012). Those smokers who have unsuccessfully tried to quit also show very high levels of distress (Sung, Prochaska, Ong, Shi, & Max, 2011; van der Deen, Carter, Wilson, & Collings, 2011). The reason why smoking leads to poorer mental health is not immediately clear. However, one possibility is that smoking interferes in some way with the development of adaptive coping skills that might help reduce stress and worry in the face of life’s adversities. In this study, we address the question of whether a history of smoking tobacco leads to the development of more maladaptive coping strategies and fewer adaptive ones in adulthood.
High stress levels are associated with the initiation of smoking among young people. For example, among clinic attendees aged 12–21 years, nearly three quarters stated that they progressed from initiation to regular smoking because they felt stressed; a third stated that smoking helped them deal with problems (Siqueira, Diab, Bodian, & Rolnitzky, 2000). Among young New Zealand (NZ) adolescents aged 13 years, friendship and wanting to join in were given as the two most frequent reasons to begin smoking, followed by relaxation and helping to stop worrying about things, both of which were rated more highly than image as a reason to smoke (Stanton, Mahalski, McGee, & Silva 1993). There is some evidence to indicate that this association between smoking and stress may be stronger among adolescent girls than among boys (Booker et al., 2007; Byrne & Mazanov, 2003), although not all studies have found this gender difference (Wills, Sandy, & Yaeger, 2002).
Although cigarette smoking may be a response to dealing with stress, there is a parallel body of research in adolescence to suggest that smoking is related to more “negative” coping strategies, such as distraction and denial, and the use of less restraint or use of aggression. Conversely, nonsmoking is associated with more positive or adaptive coping, including seeking adult support and behavioral coping (Sussman et al., 1993; Vollrath, 1998). Despite being regarded as a way to deal with stress, smoking remains a relatively weak coping mechanism (Koval & Peterson, 1999).
Much of this research on stress, coping, and tobacco smoking in adolescence has relied, at least in part, on cross-sectional studies (Siqueira et al., 2000; Sussman et al., 1993), making it difficult to identify causal directions among stress, coping, and smoking. Other research has relied on short-term longitudinal studies that followed young smokers from initiation to sustained smoking over several years (e.g., Byrne & Mazanov, 2003; Koval & Peterson, 1999; McGee & Stanton, 1993; Wills et al., 2002). However, rates of daily smoking in these studies of adolescents can be relatively low, leading to a reliance on weaker definitions of smoking such as “ever smoked and not quit.”
Nicotine dependence may develop relatively quickly in young smokers (Guo, McGee, Reeder, & Gray, 2010), so that although stress and the relaxing effects of tobacco may foster the initiation of smoking, it may be the addictive process that maintains smoking in the longer term. For example, in our study of young NZ smokers, although feelings of relaxation were correlated with smoking at age 13 years, this relaxing effect of smoking was not especially predictive of continued smoking from 13 to 15 years of age (McGee & Stanton, 1993). This may simply reflect the development of nicotine dependence among these 15-year-old adolescents who were smoking daily. What remains unexamined is whether sustained smoking into adulthood interferes with the healthy development of adaptive coping strategies such as planning and use of emotional and other support. Parrott (1999), for example, has argued that if an individual uses cigarettes to deal with adverse moods in stressful situations, the underlying problem causing the distress can be left unresolved. He hypothesizes that this results in smokers failing to tackle problems directly, leaving them to use less effective methods for handling negative life events. There is strong evidence that smokers cite subjective distress as a cue for smoking, and experimental manipulations indicate that stressful tasks and anxiety increase smoking, especially among younger individuals (Rose, Ananda, & Jarvik, 1983). Etter, Bergman, Humair, and Perneger (2000) estimate that as much as 25% of cigarette consumption is likely to be in response to negative affect, including stress, worry, and boredom. A consequence is that continually lighting up in response to negative affect leaves the sources of stress, worry, and boredom unaddressed.
We were unable to find any longitudinal studies that examined the potential long-term effect of sustained smoking on the development of adult coping behaviors. What little longitudinal research there is in this area has examined coping-related variables in relation to later quitting behaviors (see Cengelli, O’Loughlin, Lauzon, & Cornuz, 2012, for a recent review). In this study, we report a follow-up of a sample of NZ adolescents to identify the longer term consequences of smoking into the young adult years for coping skills at age 32 years. We also examine the relative contribution to later coping, from early childhood disadvantage, experience of stress and worry in adolescence, and adolescent coping. These three additional variables are potentially related to both the development of smoking and the development of particular styles of coping behaviors in later life. Given the possibility of multiple pathways to adult coping, structural equation modeling (SEM) was considered the most appropriate way to examine the development of adult coping styles from these earlier variables. If our hypothesis is correct, tobacco smoking should independently predict more maladaptive coping and fewer adaptive coping strategies in adulthood.
Finally, evidence suggests that there may be gender-based differences in the relationships between stress-and-coping and later smoking (Byrne & Mazanov, 2003; Strine et al., 2012). Given differences between adolescent boys and girls both in terms of experienced distress (Byrne & Mazanov, 2003; McGee & Stanton, 1992), coping behaviors (Nada Raja, McGee, & Stanton, 1992), and rates of smoking in NZ (Stanton, 1995), we also examine gender-based differences in the relationships between smoking and coping in later adulthood..
METHOD
Participants
The Dunedin Multidisciplinary Health and Development Study (DMHDS) is a longitudinal study of a cohort of 1,037 people born in Dunedin NZ between April 1, 1972, and March 31, 1973. The participants were enrolled and assessed initially at age 3 years and then reassessed at 5, 7, 9, 11, 13, 15, 18, 21, 26, 32, and, most recently, at age 38 years (2010–2012) on a variety of health, behavior, and background measures. Participants, and in earlier phases their parents, gave signed consent and were invited to attend the research unit for a full day of assessments as close as possible to their birthdays. In total, 964 participants completed an interview on wellbeing and coping styles at age 32 years, representing 95% of the 1,015 participants known to be alive and eligible for assessment. More than 90% of the participants identified themselves as being of “New Zealand/European” ethnicity. Although comparable with other community-based samples from Western societies, the sample is underrepresentative of Maori (tangata whenua–the indigenous people of the land) and Pacific peoples (Poulton et al., 2006). Every assessment phase of the DMHDS has been subject to ethical approval from the Ethics Committee attached to the Otago Regional District Health Board.
Measures and Procedure
“Cigarette smoking” has been assessed throughout the DMHDS since age 9 years (McGee & Stanton, 1993; Stanton et al., 1993). For the present study, we used two kinds of smoking data to indicate persistent and high levels of tobacco smoking into the early adult years, namely, daily smoking (defined by self-report of “usually smoking every day”) and symptoms of tobacco dependency. The frequency of daily smoking rose rapidly, from only a handful smoking at least one cigarette daily at age 13 years to 15% smoking daily at age 15 years, then to 31%, 35%, and 39% at ages 18, 21, and 26 years, and a slight decline to 35% at age 32 years. Women reported significantly more daily smoking than men at every age. There was high continuity between daily smoking at age 15 years and at later ages (Stanton, 1995), and smoking also persisted across the early adult years, with 80% of those reporting smoking at age 21 years still smoking at age 32 years (Welch & McGee, 2010).
Owing to this strong persistence of smoking over time, preliminary SEM analysis of the smoking variables was carried out to identify a stable latent variable for smoking. Daily smoking itself did not form an especially stable latent variable. Consequently, we explored combining daily smoking with reports of symptoms of tobacco dependence. Tobacco dependence based on the Diagnostic & Statistical Manual of Mental Disorders–3rd Edition Revised (DSM-III-R) was assessed at ages 18, 21, and 26 years (Reeder, Williams, McGee & Poulton, 2001; Stanton, 1995). An 11-item measure of dependence included assessment of desire to smoke, unsuccessful attempts to quit smoking, giving up activities to smoke, smoking despite health and other problems, withdrawal symptoms during cessation attempts, and smoking to avoid such symptoms. Initial modeling indicated that daily smoking at age 18, in combination with the tobacco dependence scores at ages 21 and 26 years did form a stable latent variable. This also had the effect that the smoking variable was temporally separated from the stress-and-coping measures assessed at age 15 years.
“Coping behaviors” at age 32 years were assessed using the Brief COPE inventory that assesses problem-focused coping responses and those directed toward aspects of the situation other than the stressor per se (Carver, 1997). Each coping strategy was assessed using two items, rated on a four-point Likert-type scale, ranging from 1 = haven’t using the been doing this at all to 4 = I’ve been doing this a lot. Responses were summed to produce subscale scores for each participant. Active coping, Planning, Positive reframing, Using emotional support, and Using instrumental support were selected to indicate adaptive coping strategies. Scales representing maladaptive coping strategies were Venting, Denial, Behavioral disengagement, and Self-blame. These groupings were based upon a principal-components analysis of the various subscales and examination of the pattern of intercorrelations among them (Olsson, McGee, Nada-Raja, & Williams, 2012). The Brief COPE also includes a subscale assessing the use of alcohol and other drugs to help deal with problems. In the analysis, we tested the overall model both including and excluding this scale, given the potential relationship between using alcohol and other drugs (as well as tobacco) to cope. The remaining subscales of Acceptance, Humor, and Religion did not correlate with the other subscales to justify inclusion in the two groupings.
“Coping at age 15 years” was not formally assessed by a single scale. However, several measures had been used to assess different aspects of adolescent coping, and these were combined to form a stable latent variable. These measures included the Communication subscale of a shortened version of the Inventory of Parent and Peer Attachment (IPPA: Armsden & Greenberg, 1987; Nada Raja et al., 1992). Four items assessed perceived levels of communication with each of parents and peers, with items rated on a four-point Likert-type scale of 1 = almost never or never, 2 = sometimes, 3 = often, and 4 = almost always or always. Sample items include I tell my parents about my problems and troubles, and I like to get my friends point of view on things I’m concerned about. Coefficient alpha for the parent and peer scales were .82 and .80, respectively, indicating high internal consistency. A subscale assessing aspects of negative coping was formed from three items included as part of the mental health interview (see McGee et al., 1990). These were as follows: try not to think or talk about your problems, don’t talk to anyone when you feel upset, and use drugs or alcohol to make you feel better (with responses for each item scored as 1 = yes or 0 = no).
“Stress and worry” at age 15 years were measured with two scales. The first, called the Feel Bad scale, consists of 20 items describing commonly occurring events and situations that adolescents might experience (Lewis, Siegel, & Lewis, 1984). Sample items include feeling left out of things, not getting along with your teacher, and fighting with your parents about house rules. Each item is rated for frequency over the past year on a five-point scale, ranging from 0 = never, 1 = one or two times, 2 = sometimes, 3 = often, and 4 = all the time. If the frequency of an item is rated 1 or above, the item is also rated for intensity of stress experiences (i.e., “how did it make you feel”), with 0 = not bad, 1 = a little bad, 2 = pretty bad, 3 = really bad, and 4 = terrible. Coefficient alpha for the distress ratings was .79 (McGee & Stanton, 1992). The factor structure of the scale indicated three main distress subscales identified as self-esteem, competence, and parents; these were used in the present study. The second scale consisted of the diagnostic items for overanxiety disorder taken from a shortened version of the Diagnostic Interview Schedule for Children–Child version XXIII, based on DSM-III criteria (DISC-C: McGee et al., 1990). These items were included as part of a mental health interview at age 15 years, with each item coded as 0 = no, 1 = sometimes, and 2 = yes. The eight items assessed worry about various future and past events, schoolwork, making mistakes in front of others, others laughing at you, and other concerns. Coefficient alpha for the worry scale was .71.
“Family disadvantage” during childhood was indicated by three separate indices measuring socioeconomic status, family climate of mental health, and parent–child interaction practices. These indices and the measures used to derive them are fully described by McGee, Williams, and Nada-Raja (2001). In brief, an index of socioeconomic disadvantage from 5 to 9 years of age was constructed from data on the child’s father having a semiskilled or unskilled job; the child’s mother being 20 years or younger at first pregnancy; the mother having no formal educational qualifications beyond high school level; and single parenting, mainly relevant to the mother. Family climate of mental health from 5 to 9 years of age was defined by an index assessing low within-family social support at ages 7 and 9; high levels of maternal depression when the child was aged 5, 7, or 9 years; parental separation up to age 9; and other adverse family circumstances (e.g., family violence or father’s mental ill health) reported by the parents. Finally, harsh parent–child interaction from 3 to 9 years of age was identified by four items including maternal rejection observed during psychometric testing when the child was aged 3, parental reports of low egalitarianism at ages 5 or 7, parental reports of high authoritarianism at ages 5 or 7, and a measure of lax inconsistent discipline at ages 7 or 9 years.
Statistical Analyses
SEM was performed in STATA software (STATA Corporation, 2005). Individual measurement models were constructed for each of the latent indicators used in the analysis and then assembled into a developmental model testing the relative contribution of family disadvantage, stress or worry, early coping, and smoking pathways to both adaptive and maladaptive coping styles in adulthood. Path coefficients are presented as standardized estimates. A standardized estimate expresses the proportion of a SD change in one variable due to a 1 SD change in a second variable. Gender-based differences were investigated by fitting a model in which all the parameters were constrained to be equal and using score tests (Lagrange multiplier tests) and Wald tests to examine whether the parameters assumed to be equal across groups should be relaxed. Goodness of fit for the SEM was assessed by the Tucker–Lewis index (TLI), comparative fit index (CFI), and the root mean squared error of approximation (RMSEA).
Standardized effects were examined among six developmentally ordered latent variables:
Level of family disadvantage in childhood, indicated by the indices of socioeconomic disadvantage, family climate of mental health, and harsh parent–child interaction. A high score indicated greater levels of disadvantage.
Adolescent coping, indicated by the two parent and peer communication subscales from the IPPA, as well as the negative coping subscale. A high score indicated more positive coping.
Adolescent stress–worry, indicated by the feel bad distress intensity subscales for self-esteem, competence, and parents, in addition to the measure of adolescent worry from the DISC-C. A high score indicated more reported stress and worry.
Cigarette smoking in late adolescence and early adulthood, indicated by daily smoking at age 18 and high tobacco dependence scores at ages 21 and 26 years.
Adaptive coping styles in adulthood, indicated by the brief COPE subscales for active coping, planning, positive reframing, and using emotional and instrumental support. A high score indicated greater use of adaptive coping styles.
Maladaptive coping styles, indicated by the brief COPE subscales for venting, denial, behavioral disengagement, self-blame, and substance use. A high score indicated greater use of maladaptive coping styles.
RESULTS
SEM was conducted on data from 961 participants, giving an overall response rate of 94.5%. Figure 1 shows the best-fitting model of the relationship among childhood disadvantage, adolescent tobacco smoking, stress, and parent attachment, and later adult coping. The latent variable loadings for observed variables are presented in Table 1. The fit of the overall model was acceptable, with CFI = .899, TLI = .882, and RMSEA = .050. The factor loadings for the latent variables suggested that the various measures were contributing significantly to each latent variable.
Figure 1.
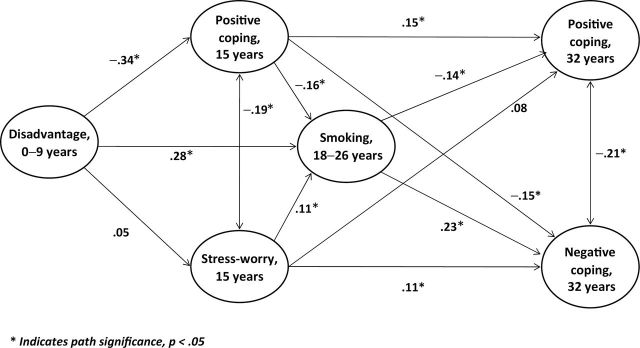
Pathways from adolescent smoking to adult coping styles.
Table 1.
First-Order Latent Variable Loadings for Observed Variables in the Model
| Latent variable | Observed variable | Age, y | Estimate | SE |
|---|---|---|---|---|
| Family disadvantage | Socioeconomic conditions | 0–9 | .626 | .061 |
| Family climate | 0–9 | .350 | .049 | |
| Harsh parenting | 0–9 | .334 | .046 | |
| Adolescent coping | Parent communication | 15 | .700 | .041 |
| Peer communication | 15 | .464 | .038 | |
| Negative coping | 15 | −.547 | .038 | |
| Adolescent stress–worry | Self-esteem | 15 | .884 | .020 |
| Parents | 15 | .642 | .024 | |
| Competence | 15 | .622 | .025 | |
| Worry | 15 | .533 | .028 | |
| Tobacco smoking | Dependence at 21 years | 21 | .910 | .013 |
| Dependence at 26 years | 26 | .796 | .016 | |
| Daily 18 years | 18 | .764 | .017 | |
| Adaptive coping | Planning | 32 | .840 | .022 |
| Active coping | 32 | .749 | .023 | |
| Positive reframing | 32 | .515 | .028 | |
| Instrumental Support | 32 | .381 | .032 | |
| Emotional support | 32 | .306 | .034 | |
| Maladaptive coping | Disengagement | 32 | .761 | .041 |
| Denial | 32 | .526 | .035 | |
| Self-blame | 32 | .362 | .036 | |
| Venting | 32 | .225 | .039 | |
| Substance use | 32 | .280 | .039 |
Note. SE = standard error.
Childhood Disadvantage, Coping, and Stress–Worry
The direct (unmediated) standardized estimates of the effects of childhood disadvantage on adolescent coping and stress–worry were −.34 and .05, respectively, whereas the direct effect of disadvantage on daily smoking was .28. That is, childhood disadvantage was inversely related to adolescent coping and positively related to later smoking. Stress–worry had a small direct effect on smoking, with a path coefficient of .11, whereas coping at age 15 years had a small inverse effect, with –.16, respectively.
From Smoking to Later Coping
Smoking in turn had a direct inverse effect on later adaptive coping (−.14) and a direct effect on maladaptive coping (.23). Some small but parallel effects of adolescent coping and stress–worry on later coping were also evident. Stress–worry predicted later maladaptive coping (.11) but not adaptive coping. Adolescent coping had a direct effect on adaptive coping (.15) and an inverse effect on maladaptive coping (−.15). Exclusion of the substance use subscale of the Brief COPE did not substantially alter these findings.
Further Model Evaluations
The two strongest paths in the model lead from early childhood disadvantage to coping in adolescence and later smoking, and the total effect of disadvantage on later smoking was .33, including both the direct path and the indirect paths through coping and stress–worry. We examined the extent to which the effect of tobacco smoking on later adult coping reflects these associations between childhood disadvantage and smoking. The total effect of childhood disadvantage on positive coping at age 32 years through these indirect paths was −.13, p < .05, an effect size of the same order as the direct path from smoking to positive coping at age 32 years. However, this latter path remained independent of any effect of early disadvantage, suggesting that the effect on coping is smoking related; smoking is not simply acting as a marker for earlier disadvantage.
A separate question is the extent to which there are male–female differences in the associations among the latent variables for men and women in the structural part of the model. Although the likelihood ratio test [LR test (44) = 138.34, p < .001] suggested that there were differences in some of the model parameters, the differences in parameters estimating the associations among the latent variables were not significant. The score tests indicated that the differences in the models could be attributed to differences in the means of some of the variables rather than their associations with the latent variable. It was, therefore, concluded that the model as it stood applied to both men and women.
Finally, we compared the participants with available data and who were included in the model with those having incomplete data. There were no significant differences between the two groups in terms of either smoking at age 18 or age 26 years (p > .05). Given that smoking was the central variable under investigation, we believe it is unlikely that missing data introduced any significant source of bias in the overall model.
DISCUSSION
The findings of this study are consistent with the hypothesis that the onset of persistent tobacco smoking from midadolescence to early adulthood at age 21 years is associated with more-frequent use of maladaptive coping skills in dealing with problems and less-frequent use of adaptive coping skills in later adulthood. These associations do not appear to be due to prior relationships between family disadvantage and smoking, or either the experience of stress and worry in adolescence, or poorer coping in adolescence among those who smoke tobacco. The relationship between tobacco smoking and coping held for both men and women.
There has been a lack of long-term studies investigating the predictive association between smoking and later coping. Short-term follow-up studies in adolescence have sought to describe the causal direction of this relationship, especially in the context of adolescent stress predicting the uptake of cigarette smoking (Byrne & Mazanov, 2003; McGee & Stanton, 1993; Wills et al., 2002). Our results are consistent with the view that tobacco smoking may inhibit the development of self-efficacy or the confidence in one’s ability to act in a given situation (Etter et al., 2000). As Parrott (1999) points out, because of its addictive nature, smoking becomes a highly overlearned behavior. Elsewhere, we have estimated that the young smokers in our sample would have smoked on average about 25,000 cigarettes from the ages of 15–21 years; by age 32, for the 8 in every 10 who continued smoking daily, they would have smoked a staggering 66,000 cigarettes each (Welch & McGee, 2010). Perhaps 25% of these cigarettes were smoked in response to negative affect, including stress, worry, and boredom (Etter et al., 2000).
The study also confirms previous associations between family disadvantage in childhood and later smoking in the Dunedin study (McGee & Williams, 2006). Indeed, this is the strongest effect we observed in the model, attesting to the strength of the relationship between early disadvantage and smoking in late adolescence and early adulthood. Recent research has noted the association between childhood poverty and what has been called elevated allostatic load, a marker of elevated physiological stress mobilized in response to persistent demands from the environment to act (Evans & Kim, 2012). Tobacco smoking is clearly a highly visible and often modeled way to deal with this stress (Koval & Peterson, 1999). However, as our study suggests, smoking may preclude the development of more adaptive styles of coping, perhaps even more so in the presence of poorer coping in adolescence, which itself is an outcome of early disadvantage. Nevertheless, it is important not to overstate these associations. It needs to be acknowledged that although statistically significant, the sizes of these effects of smoking on later coping are relatively small. Tobacco smoking may just be one way of coping with the vagaries of everyday life, but it is not the only way and it certainly does not explain all patterns of adult coping.
A particular strength of the Dunedin study has remained the consistently high participation rates from childhood to adulthood. So in the current study, the SEM was analyzed using data from 961 participants, representing 95% of the sample known to be alive at age 32 years. Furthermore, those with missing data did not differ significantly from those included in the model on tobacco smoking. Over the years, the study has collected a rich variety of prospective information on participants, allowing a detailed study of smoking behaviors over time. Where psychological constructs such as stress, worry, and coping have been assessed, we have used valid and reliable instruments based on the current literature at the time of assessment. The sample is community based and broadly representative of the NZ population, although somewhat underrepresentative of Maori and Pacific peoples. One potential weakness in the current study is the lack of a broader measure of coping skills at age 15, prior to the development of persistent tobacco smoking. Nevertheless, we had access to measures of parent and peer communication at that age and the use of alcohol or other drugs to feel better, measures that mirror the instrumental and emotional support subscales and the alcohol–drug subscale of the Brief COPE. Finally, it should be noted that the goodness-of-fit indices were still slightly below accepted standards. For example, CFI = .899 still falls just short of the often recommended cutoff of .90, although there remains debate about the stringency of recommended cutoffs (see Marsh, Hau, & Wen, 2004). Our intention in this study was to test a quite specific model concerning the relationships between tobacco smoking and later coping. One interpretation of the findings is that this model should be seen as exploratory to allow hypothesis generation to inform further replication and extension. For example, do other forms of substance use such as alcohol and cannabis dependence have similar effects on the development of patterns of adult coping?
In the Introduction, we highlighted the well-documented association between tobacco smoking and poor mental health. Our findings contribute to a partial explanation of this relationship, in that some of the poor mental health shown by smokers may be explained by their less well-developed adaptive coping skills arising because of their addiction. The addictive nature of smoking explains the difficulty experienced by many smokers in quitting, but the process of quitting also requires coping skills in the face of withdrawal, again skills that have not been developed. Finally, the results may point to some mental health gains to be made as tobacco smoking declines. This may be especially so among young people where the teaching of adaptive coping skills would no longer have to compete with tobacco as an alternative source of stress reduction.
FUNDING
The research described in this study was supported by the Health Research Council of NZ, with additional support from grants from the Antisocial and Violent Behavior Branch of the U.S. National Institutes of Mental Health. Dr. Craig A. Olsson is supported by an Australian Research Council Fellowship.
DECLARATION OF INTERESTS
None declared.
ACKNOWLEDGMENTS
The authors are indebted to the many people who have contributed to this research effort over the years. We thank Professor Richie Poulton for his comments on the manuscript. Our thanks go to those enrolled in the DMHDS, their parents, and study investigators for their long-term commitment to this research effort.
REFERENCES
- Armsden G. C., Greenberg M. T. (1987). The inventory of parent and peer attachment: Individual differences and their relationship to psychological well-being in adolescence. Journal of Youth and Adolescence, 16, 427–454.10.1007/BF02202939 [DOI] [PubMed] [Google Scholar]
- Booker C. L., Unger J. B., Azen S. P., Baezconde-Garbanati L., Lickel B., Johnson C. A. (2007). Stressful life events and smoking behaviors in Chinese adolescents: A longitudinal analysis. Nicotine & Tobacco Research, 9, 1085–1094.10.1080/14622200701491180 [DOI] [PubMed] [Google Scholar]
- Byrne D. G., Mazanov J. (2003). Adolescent stress and future smoking behaviour: A prospective investigation. Journal of Psychosomatic Research, 54, 313–321.10.1016/s0022-3999(02)00411-7 [DOI] [PubMed] [Google Scholar]
- Carter K. N., ven der Deen F. S., Wilson N., Blakely T. (2012). Smoking uptake is associated with increased psychological distress: Results of a national longitudinal study. Tobacco Control, 1–6.10.1136/tc.2012–050614 [DOI] [PubMed] [Google Scholar]
- Carver C. S. (1997). You want to measure coping but your protocol’s too long: Consider the brief COPE. International Journal of Behavioral Medicine, 4, 92–100.10.1207/s15327558ijbm0401_6 [DOI] [PubMed] [Google Scholar]
- Cengelli S., O’Loughlin J., Lauzon B., Cornuz J. (2012). A systematic review of longitudinal population-based studies on the predictors of smoking cessation in adolescent and young smokers. Tobacco Control, 21, 355–36210.1136/tc. 2011–044149 [DOI] [PubMed] [Google Scholar]
- Degenhardt L., Lynskey M., Hall W. (2000). Cohort trends in the age of initiation of drug use in Australia. Australian & New Zealand Journal of Public Health, 24, 421–426.10.1111/J.1467-842x.2000.tb01605x [DOI] [PubMed] [Google Scholar]
- Etter J. F., Bergman M. M., Humair J. P., Perneger T. V. (2000). Development and validation of a scale measuring self-efficacy of current and former smokers. Addiction, 95, 901–913.10.1046/j.1360-0443.2000.9569017.x [DOI] [PubMed] [Google Scholar]
- Evans G. W., Kim P. (2012). Childhood poverty and young adults’ allostatic load: The mediating role of childhood cumulative risk exposure. Psychological Science, 23, 979–983.1177/0956797612441218 [DOI] [PubMed] [Google Scholar]
- Fergusson D. M., Goodwin R. D., Horwood L. J. (2003). Major depression and cigarette smoking: Results of a 21-year longitudinal study. Psychological Medicine, 33, 1357–1367.10.1017/s0033291703008596 [DOI] [PubMed] [Google Scholar]
- Guo H., McGee R., Reeder A. I., Gray A. (2010). Smoking behaviours and contextual influences on adolescent nicotine dependence. Australian & New Zealand Journal of Public Health, 34, 502–507.10.1111/j/1753-6405.2010.00597.x [DOI] [PubMed] [Google Scholar]
- Koval J. J., Peterson L. L. (1999). Stress-coping and other psychosocial risk factors: A model for smoking in grade 6 students. Addictive Behaviors, 24, 207–218.10.1016/s0306-4603(98)00037-9 [DOI] [PubMed] [Google Scholar]
- Lewis C. E., Siegel J. M., Lewis M. A. (1984). Feeling bad: Exploring sources of distress among pre-adolescent children. American Journal of Public Health, 74, 117–122.10.2105/AJPH.74.2.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh H. W., Hau K. T., Wen Z. (2004). In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Structural Equation Modeling, 11, 320–341.10.1207/s15328007sem1103_2 [Google Scholar]
- McGee R., Feehan M., Williams S., Partridge F., Silva P. A., Kelly J. (1990). DSM-III disorders in a large sample of adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 29, 611–619.10.1097/ 00004583-1990070000-00016 [DOI] [PubMed] [Google Scholar]
- McGee R., Stanton W. R. (1992). Sources of distress among New Zealand adolescents. Journal of Child Psychology and Psychiatry, 33, 999–1010.10.1111/j.1469-76101992.tb00921x [DOI] [PubMed] [Google Scholar]
- McGee R., Stanton W. R. (1993). A longitudinal study of reasons for smoking in adolescence. Addiction, 88, 265–271.10.1111/j.1360-0443.1993.tb00810.x [DOI] [PubMed] [Google Scholar]
- McGee R., Williams S. (2006). Predictors of persistent smoking and quitting among women smokers. Addictive Behaviors, 31, 1711–1715.10.1016/ j.addbeh.2005.12.008 [DOI] [PubMed] [Google Scholar]
- McGee R., Williams S., Nada-Raja S. (2001). Low self-esteem and hopelessness in childhood and suicidal ideation in early adulthood. Journal of Abnormal Child Psychology, 29, 281–291.10.1023/A:1010353711369 [DOI] [PubMed] [Google Scholar]
- Morrell H. E. R., Cohen L. M. (2006). Cigarette smoking, anxiety, and depression. Journal of Psychopathology and Behavioral Assessment, 28, 281–295.10.1007/s10862-005-9011-8 [Google Scholar]
- Nada Raja S., McGee R., Stanton W. R. (1992). Perceived attachments to parents and peers and psychological well-being in adolescence. Journal of Youth and Adolescence, 21, 471–485.10.1007/BF01537898 [DOI] [PubMed] [Google Scholar]
- Olsson C., McGee R., Nada-Raja S., Williams S. (2012). A 32-year longitudinal study of child and adolescent pathways to well-being in adulthood. Journal of Happiness Studies, 1–15.10.1007/s10902-012-9369-8 [Google Scholar]
- Parrott A. C. (1999). Does cigarette smoking cause stress? American Psychologist, 54, 817–820.10.1037/0003- 066x.54.10.817 [DOI] [PubMed] [Google Scholar]
- Poulton R., Hancox R., Milne B., Baxter J., Scott K., Wilson N. (2006). The Dunedin Multidisciplinary Health and Development Study: Are its findings consistent with the overall New Zealand population? New Zealand Medical Journal, 199, U2002 Retrieved from http://journal.nzma.org.nz/journal/119–1235/ [PubMed] [Google Scholar]
- Reeder A. I., Williams S., McGee R., Poulton R. (2001). Nicotine dependence and attempts to quit or cut down among young adult smokers. The New Zealand Medical Journal, 114, 403–406 [PubMed] [Google Scholar]
- Rose J. E., Ananda S., Jarvik M. E. (1983). Cigarette smoking during anxiety-provoking and monotonous tasks. Addictive Behaviors, 8, 353–359.10.1016/0306-4603(83)90035–7 [DOI] [PubMed] [Google Scholar]
- Siqueira L., Diab M., Bodian C., Rolnitzky L. (2000). Adolescents become smokers: The roles of stress and coping methods. Journal of Adolescent Health, 27, 399–408.10.1016/s1054-139x(00)00167-1 [DOI] [PubMed] [Google Scholar]
- Stanton W. R. (1995). DSM-III-R tobacco dependence and quitting during late adolescence. Addictive Behaviors, 20, 595–603.10.1016/0306-4603-(95)00019-9 [DOI] [PubMed] [Google Scholar]
- Stanton W. R., Mahalski P., McGee R., Silva P. A. (1993). Reasons for smoking or not smoking in early adolescence. Addictive Behaviors, 18, 321–329.10.1016/0306-4603(93)90033–6 [DOI] [PubMed] [Google Scholar]
- STATA Corporation (2005). Stata statistical software [computer program], release 10.1. College Station, TX: Stata Corporation [Google Scholar]
- Strine T. W., Edwards V. J., Dube S. R., Wagenfeld M., Dhingra S., Prehn A. W, … Croft J. B. (2012). The mediating sex-specific effect of psychological distress on the relationship between adverse childhood experiences and current smoking among adults. Substance Abuse Treatment, Prevention, and Policy, 7, 30.10.1186/1747-597X-7–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung H., Prochaska J. J., Ong M. K., Shi Y., Max W. (2011). Cigarette smoking and serious psychological distress: A population-based study of California adults. Nicotine & Tobacco Research, 13, 1183–1192.10.1093/ntr/ntr148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sussman S., Brannon B. R., Dent C. W., Hansen W. B., Johnson C. A., Flay B. (1993). Relations of coping effort, perceived stress, and cigarette smoking among adolescents. International Journal of the Addictions, 28, 599–612 Retrieved from http://informahealthcare.com [DOI] [PubMed] [Google Scholar]
- van der Deen F. S., Carter K. N., Wilson N., Collings S. (2011). The association between failed quit attempts and increased levels of psychological distress in smokers in a large New Zealand cohort. BMC Public Health, 11, 598.10.1186/1471-2458-11-598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vollrath M. (1998). Smoking, coping and health behavior among university students. Psychology & Health, 13, 431–441.10.1080/08870449808407301 [Google Scholar]
- Welch D., McGee R. (2010). Breath holding predicts reduced smoking intake but not quitting. Open Addiction Journal, 3, 39–42.10.2174/1874941001003010039 [Google Scholar]
- Wills T. A., Sandy J. M., Yaeger A. M. (2002). Stress and smoking in adolescence: A test of directional hypotheses. Health Psychology, 21, 122–130.10.1037/0278-6133.21.2.12 [PubMed] [Google Scholar]


