Abstract
An estimated 80% of sexually active young women in the United States use hormonal contraceptives during their reproductive years. Associations between hormonal contraceptive use and mood disturbances remain understudied, despite the hypothesis that estrogen and progesterone play a role in mood problems. In this study, we used data from 6,654 sexually active nonpregnant women across 4 waves of the National Longitudinal Study of Adolescent Health (1994–2008), focusing on women aged 25–34 years. Women were asked about hormonal contraceptive use in the context of a current sexual partnership; thus, contraceptive users were compared with other sexually active women who were using either nonhormonal contraception or no contraception. Depressive symptoms were assessed with the Center for Epidemiologic Studies Depression Scale. At ages 25–34 years, hormonal contraceptive users had lower mean levels of concurrent depressive symptoms (β = −1.04, 95% confidence interval: −1.73, −0.35) and were less likely to report a past-year suicide attempt (odds ratio = 0.37, 95% confidence interval: 0.14, 0.95) than women using low-efficacy contraception or no contraception, in models adjusted for propensity scores for hormonal contraceptive use. Longitudinal analyses indicated that associations between hormonal contraception and depressive symptoms were stable. Hormonal contraception may reduce levels of depressive symptoms among young women. Systematic investigation of exogenous hormones as a potential preventive factor in psychiatric epidemiology is warranted.
Keywords: adolescent, depression, gender, hormonal contraception, oral contraceptives, suicide
Editor's note: An invited commentary on this article appears on page 1389, and the authors’ response appears on page 1392.
An estimated 80% of sexually active women in the United States use hormonal contraception, most typically oral contraceptives, to prevent pregnancy (1). In addition to providing effective pregnancy prevention, hormonal contraception offers many health benefits (2–4), though its use remains a risk factor for venous thromboembolism and other vascular disease outcomes (5).
Little research has focused on the association of hormonal contraceptive use with mental health outcomes, such as depressive symptoms, and more severe manifestations of mood disturbance, such as suicide attempts. Approximately 17% of women experience major depression during their lifetime, with incidence being highest during the reproductive years (6), and many more experience depressive symptoms that do not necessarily cross the threshold to a diagnosis but may be disabling (7, 8). While a role for hormones such as estrogen and progesterone in the etiology of depressive symptoms has been hypothesized (9–11), the association remains inadequately understood. Clinical studies have indicated that precipitous changes in estrogen levels may trigger depressive episodes among women at risk for depression, particularly during the late luteal phase of the menstrual cycle and during postpartum and perimenopausal periods (12, 13), and that women with major depression generally have lower estradiol levels than controls (14, 15). Given that hormonal contraception methods introduce synthetic estrogen and progestin and modulate the physiological cycle, an examination of the role of hormonal contraception in mood problems is warranted.
Few population-based studies have evaluated the association between hormonal contraceptive use and depressive symptoms. Among 3 population-based studies conducted within the last 15 years, 2 found no consistent evidence of an association (positive or negative) between hormonal contraceptive use and depressive symptoms (16, 17), while a recent population-based study in Finland found that hormonal contraceptive use reduced levels of depressive symptoms (18). A recent study of long-term mortality based on oral contraceptive use found an increase in violent deaths, including suicide, among oral contraceptive users compared with nonusers (19), although 2 other large studies found no increase in suicide risk for oral contraceptive use (20, 21). To our knowledge, no studies have examined oral contraceptive use in relation to suicide attempts, which are more common and have different risk factors than completed suicide (22). Thus, there remains limited evidence regarding potential associations between hormonal contraceptive use and depressive symptoms or suicidality, despite widespread use of these methods for pregnancy prevention and other outcomes.
In the present study, we utilized data from a nationally representative US longitudinal study to investigate the association between contraceptive use and depressive symptoms, as well as suicide attempts. First, we compared women who were using various forms of hormonal and nonhormonal contraception with women who were using no contraception with regard to various dimensions of health, including exercise, body mass index, smoking, and engagement with health professionals. Second, we tested the association between contraceptive use and concurrent depressive symptoms, as well as past-year suicide attempts, while controlling for health-related dimensions that varied across contraceptive users. We used traditional adjustment as well as propensity score adjustment to control for sources of confounding. Lastly, we examined longitudinally whether hormonal contraceptive use predicted depressive symptoms/suicide attempts and whether depressive symptoms/suicide attempts predicted hormonal contraceptive use.
MATERIALS AND METHODS
Sample
Data were drawn from the National Longitudinal Study of Adolescent Health (23), an ongoing nationally representative study designed to address health, behaviors, and relationships. The study began with approximately 90,000 adolescents aged 12–21 years who were sampled at school in 1994–1995; approximately 20,000 of these adolescents underwent in-depth home interviews and longitudinal follow-up. Follow-up interviews were conducted in 1996 (wave 2), 2001–2002 (wave 3), and 2007–2008 (wave 4).
The present study focused on the subset of participants who completed a wave 4 interview in 2007–2008, at ages 25–34 years. Figure 1 outlines the exclusion criteria for the present sample. Women who were not sexually active in the past year were not asked about contraceptive use; thus, we did not include them in the analytical sample. The sample size for analysis was 6,654.
Figure 1.
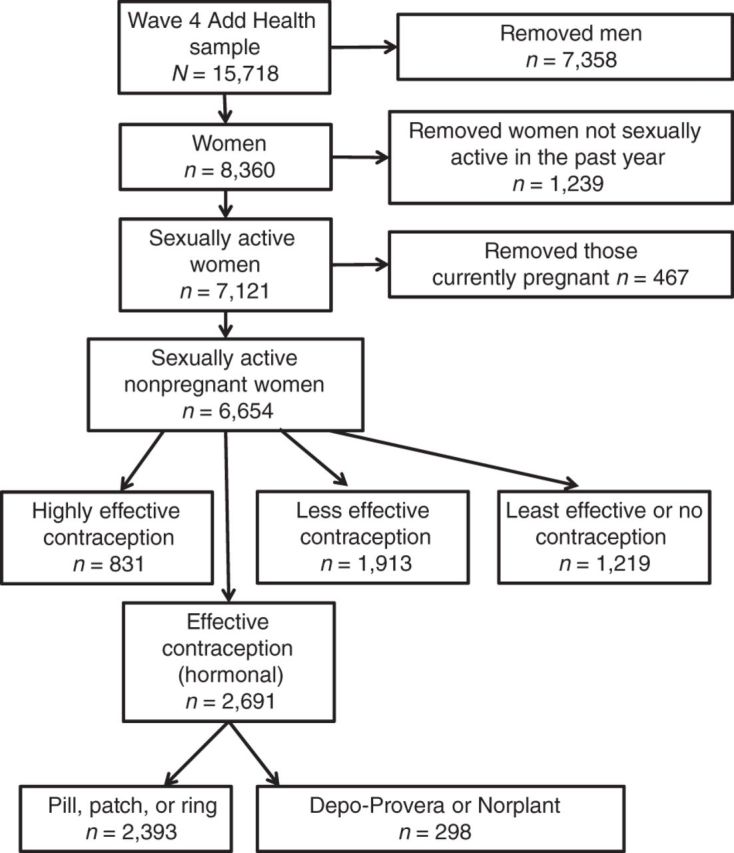
Selection of the study sample from participants in the wave 4 interview (ages 25–34 years) of the National Longitudinal Study of Adolescent Health (Add Health), 2007–2008.
Measures
Contraceptive use in wave 4
Women who had had a sex partner in the past year were asked whether they used any form of birth control or disease prevention. We divided the sample into groups based on World Health Organization categories of contraception effectiveness (24).
The first group included women using methods that are rated as highly effective, and included vasectomy, intrauterine devices (IUDs), and tubal ligation (n = 831; 12.5%). We did not have information on use of hormonal IUDs versus nonhormonal IUDs; however, hormonal IUDs would probably comprise a small proportion of total IUD use in this sample, which was already low (4.5%). A second category included methods rated as effective; these included combination hormonal contraceptives in the form of the contraceptive pill, patch, or ring (n = 2,393; 36.0%). We analyzed women using known progestin-only forms of contraception (i.e., Depo-Provera (Pfizer Inc., New York, New York) or Norplant (Wyeth Pharmaceuticals, Radnor, Pennsylvania)) separately (n = 298; 4.5%) and report results separately from those for the pill, patch, and ring group. Among women who did not use a highly effective or effective method, a third category included women who used condoms, a diaphragm, a vaginal sponge, or the withdrawal method (n = 1,913; 28.8%). Among women who did not use any of the above methods, a fourth category included the least effective contraceptive methods: periodic abstinence, spermicides, and contraceptive film (n = 91; 1.4%). Finally, 17.0% (n = 1,128) of women in the sample did not report any contraceptive use with a current partner. Because of low prevalence, women using the least effective contraceptive methods were combined with women using no contraception.
Contraceptive use in waves 1–3
In waves 1 and 2, women were asked whether they were currently taking birth control pills (wave 1: 8.2%; wave 2: 8.6%). We note that the wave 1 and 2 interviews were conducted between 1994 and 1996, before the contraceptive patch and ring formulations were introduced. We did not have information on known progestin-only forms of contraception in waves 1 and 2. However, fewer than 2% of women have ever used these forms of contraception (25); thus, while there may have been some women in the referent group who were using a hormonal form of contraception, the number is unlikely to have been appreciable.
In wave 3, questions on contraceptive use mirrored the wave 4 measures. We included anyone using a pill, patch, or ring and users of known progestin-only products as hormonal contraceptive users (50.4%). We created dichotomous indicators for these hormonal contraceptive users versus all other women. As noted above, information on hormonal IUDs was not included, but the number of women using these devices was probably negligible.
Depressive symptoms and suicide attempts in waves 1–4
The presence of depressive symptoms during the past 7 days was assessed in all waves using the Center for Epidemiologic Studies Depression Scale (CES-D) (26, 27). In waves 1 and 2, the 20-item CES-D Scale was used, with each item scored 0–3, for a maximum score of 60. In waves 3 and 4, the 10-item CES-D Scale was used, with each item scored 0–3, for a maximum score of 30. Both the 10-item and the 20-item CES-D have well-documented reliability and validity (26–28). In waves 3 and 4, a CES-D score greater than or equal to 11 was considered a high level of depressive symptoms (29). In each wave, respondents were also asked how many times they had attempted suicide in the past year (dichotomized at 1 or more attempts).
Other covariates
We assessed a range of covariates for capturing information on the health and lifestyles of sexually active women. All covariates included are shown in Table 1. Demographic factors included age, race/ethnicity, education, and parity. Relationship factors included past-year monogamy and total lifetime number of vaginal sex partners. Health-related factors included current body mass index (weight (kg)/height (m)2), derived using weight and height measured by the interviewer at the time of the interview or imputed with self-report data when measured data were unavailable; participation in any individual sports during the past week (e.g., running or jogging); visiting a dentist during the last 2 years; undergoing a routine checkup by a physician during the last 2 years; and current smoking status. We also included the centrality of religion to the respondent, given that religion may be important in the decision to use contraceptives (30, 31) and is also associated with depression (32).
Table 1.
Distributions of Sociodemographic Characteristics, Relationship Factors, and Health Behaviors Among Sexually Active Nonpregnant Women Aged 25–34 Years in a Nationally Representative US Sample, National Longitudinal Study of Adolescent Health, 2007–2008
| Characteristic | Effectiveness of Contraceptive Method |
Significance Testb | Degrees of Freedom | P Value | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Highly Effective (n = 831) |
Effective (Hormonal)a (n = 2,393) |
Less Effective (n = 1,913) |
Least Effective or None Used (n = 1,219) |
||||||||
| % | Mean | % | Mean | % | Mean | % | Mean | ||||
| Sociodemographic factors | |||||||||||
| Age, years | 28.8 | 28.2 | 28.5 | 28.7 | 11.4 | 3 | <0.01 | ||||
| Parity (any children) | 91.7 | 38.5 | 55.8 | 61.6 | 76.8 | 3 | <0.01 | ||||
| Highest level of education completed | |||||||||||
| Less than high school | 9.5 | 3.0 | 6.9 | 13.3 | 32.4 | 6 | <0.01 | ||||
| High school | 72.5 | 44.1 | 62.6 | 68.4 | |||||||
| College or more | 17.9 | 52.9 | 30.5 | 18.3 | |||||||
| Race/ethnicity | |||||||||||
| Non-Hispanic | 75.8 | 75.2 | 58.4 | 69.5 | 6.1 | 9 | <0.01 | ||||
| White | |||||||||||
| American Indian, Alaska Native, Asian, or Pacific Islander | 3.2 | 3.5 | 5.1 | 3.3 | |||||||
| Black | 11.7 | 10.3 | 23.7 | 13.0 | |||||||
| Hispanic | 9.3 | 10.9 | 12.8 | 14.2 | |||||||
| Relationship factors | |||||||||||
| In a monogamous sexual partnership | 81.8 | 76.2 | 66.0 | 80.0 | 10.6 | 3 | <0.01 | ||||
| Lifetime no. of vaginal sex partners | 9.6 | 9.0 | 9.6 | 10.5 | 1.1 | 3 | 0.36 | ||||
| Health behaviors and other indicators of interest | |||||||||||
| Body mass indexc | 29.0 | 26.9 | 29.5 | 31.4 | 27.0 | 3 | <0.01 | ||||
| Any individual sports (e.g., running) in the past week | 18.2 | 29.3 | 17.9 | 18,3 | 12.8 | 3 | <0.01 | ||||
| Undergoing a routine checkup by a physician in the past 2 years | 82.7 | 87.8 | 81.0 | 76.0 | 10.7 | 3 | <0.01 | ||||
| Visiting a dentist in the last 2 years | 58.0 | 67.4 | 55.4 | 50.6 | 14.0 | 3 | <0.01 | ||||
| Smoking status | |||||||||||
| Regular smoker (≥1 cigarette on ≥25 days in past month) | 34.2 | 16.0 | 26.1 | 32.9 | 9.8 | 6 | <0.01 | ||||
| Occasional smoker (≥1 cigarette on ≥1 day but <25 days in past month) | 7.7 | 13.9 | 12.8 | 12.0 | |||||||
| Nonsmoker (no cigarettes in past month) | 58.1 | 70.1 | 61.1 | 55.2 | |||||||
| Importance of religion | |||||||||||
| Not important | 12.6 | 15.5 | 11.1 | 10.1 | 1.6 | 9 | 0.12 | ||||
| Somewhat important | 32.9 | 33.9 | 30.2 | 32.9 | |||||||
| Extremely important | 41.5 | 39.6 | 46.2 | 45.2 | |||||||
| More important than anything else | 12.9 | 10.9 | 12.4 | 11.8 | |||||||
| History of depression, suicide attempts, and hormonal birth control use | |||||||||||
| Mean depression scored | |||||||||||
| Wave 1 | 10.4 | 8.5 | 10.0 | 10.8 | 12.2 | 3 | <0.01 | ||||
| Wave 2 | 9.2 | 3.7 | 7.0 | 13.0 | 10.6 | 3 | <0.01 | ||||
| Wave 3 | 5.2 | 4.6 | 5.2 | 5.7 | 6.9 | 3 | <0.01 | ||||
| Any past-year suicide attempt | |||||||||||
| Wave 1 | 7.7 | 5.5 | 6.0 | 8.3 | 1.3 | 3 | 0.27 | ||||
| Wave 2 | 9.0 | 3.7 | 6.7 | 5.8 | 5.3 | 3 | <0.01 | ||||
| Wave 3 | 1.8 | 2.6 | 2.3 | 4.5 | 1.3 | 3 | 0.29 | ||||
| Reported hormonal birth control use at a past interviewe | 53.0 | 68.5 | 48.5 | 51.1 | 19.2 | 3 | <0.01 | ||||
Abbreviation: CES-D, Center for Epidemiologic Studies Depression Scale.
a “Hormonal birth control” included contraceptive pills, patches, and ring formulations. Users of Depo-Provera (Pfizer Inc., New York, New York) and Norplant (Wyeth Pharmaceuticals, Radnor, Pennsylvania) were analyzed separately; demographic information for this group is available upon request.
b Chi-square test for categorical covariates; t test for continuous covariates.
c Weight (kg)/height (m)2.
d Depression score in waves 1 and 2 was measured with the 20-item CES-D (possible range of scores, 0–60). Depression score in wave 3 was measured with the 10-item CES-D (possible range of scores, 0–30).
e Hormonal birth control assessed in waves 1 and 2 included oral contraceptives only. Hormonal birth control assessed in wave 3 included pills, patches, rings, Depo-Provera, and Norplant.
Statistical analysis
First, we examined whether women using various forms of contraception or no contraception (4-level categorical variable) varied with regard to health-related covariates. We used chi-square tests for categorical outcomes and t tests for continuous outcomes. We created a propensity score using the binary variable of hormonal contraceptive use versus none as the outcome. Covariates used to create the propensity score included health-related covariates as well as design variables (study stratum (geographic area), primary sampling unit, and sample weight), as is recommended for propensity score analysis in complex surveys (33). We examined the distribution of contraception categories within quintiles of the propensity score for sufficient sample sizes to conduct the analysis and controlled for propensity score in additional regression models (34). Second, we tested whether women differed with regard to wave 4 depression symptoms, a high level of depressive symptoms, and past-year suicide attempts based on wave 4 contraceptive use. Women using the least effective contraceptives or no contraceptives were designated the referent group. Linear regression was used for depressive symptoms and logistic regression for high levels of depressive symptoms and past-year suicide attempts. Results of regression analyses were first unadjusted and then adjusted for all of the health-related variables listed in Table 1; analyses were also carried out with adjustment for propensity score. In addition, analyses of depression outcomes were also controlled for prior-wave highest depression score, and analyses of suicide attempts were also controlled for any prior suicide attempt. Users of known progestin-only products were analyzed separately. Third, longitudinal associations were assessed examining wave 3 hormonal contraceptive use (versus all other wave 3 respondents), wave 4 hormonal contraceptive use (versus all other wave 4 respondents), and high levels of depressive symptoms and past-year suicide attempts in both wave 3 and wave 4—all with logistic regression models. Analyses were conducted using SAS-callable (SAS Institute Inc., Cary, North Carolina) SUDAAN (RTI International, Research Triangle Park, North Carolina) and incorporated design weights.
RESULTS
Differences between women based on contraceptive use
Table 1 indicates that contraception-use groups in this sample differed with regard to all covariates studied except for the importance of religion in their lives, lifetime number of sexual partners, and wave 1 and wave 3 suicide attempts. In general, women using hormonal contraceptives were younger than women in other groups, less likely to have children, more likely to have a college degree, more likely to engage in individual sports (e.g., running), more likely to engage in positive health behaviors such as undergoing a routine physician's checkup and visiting the dentist, less likely to be a regular smoker, and more likely to have used hormonal contraception in the past. Women using hormonal contraceptives also had a lower mean body mass index than other groups and a lower depression score in each prior interview.
Using these covariates as well as design variables, we created a propensity score using a binary indicator of hormonal contraceptive use versus none as the outcome. Figure 2 shows the distribution of propensity scores in users and nonusers of hormonal contraceptives. Table 2 shows the percentage of women in each contraception-use category in each quintile of the propensity score; for example, 74.5% of women with the highest propensity to use hormonal birth control (propensity score >0.83) actually used hormonal birth control, and 10.4% of women with the lowest propensity to use hormonal birth control (propensity score <0.39) actually used hormonal birth control. The smallest cell size was the number of women with a propensity score greater than 0.83 who used highly effective birth control (n = 34), and cell sizes for the remainder of the contraception categories in the >0.83 category were substantially larger. The mean cell size across all propensity score quintiles and contraception categories was 202 women. Given the sufficient sample size in each of these cells, we used propensity score as a control variable in the regression modeling described below.
Figure 2.
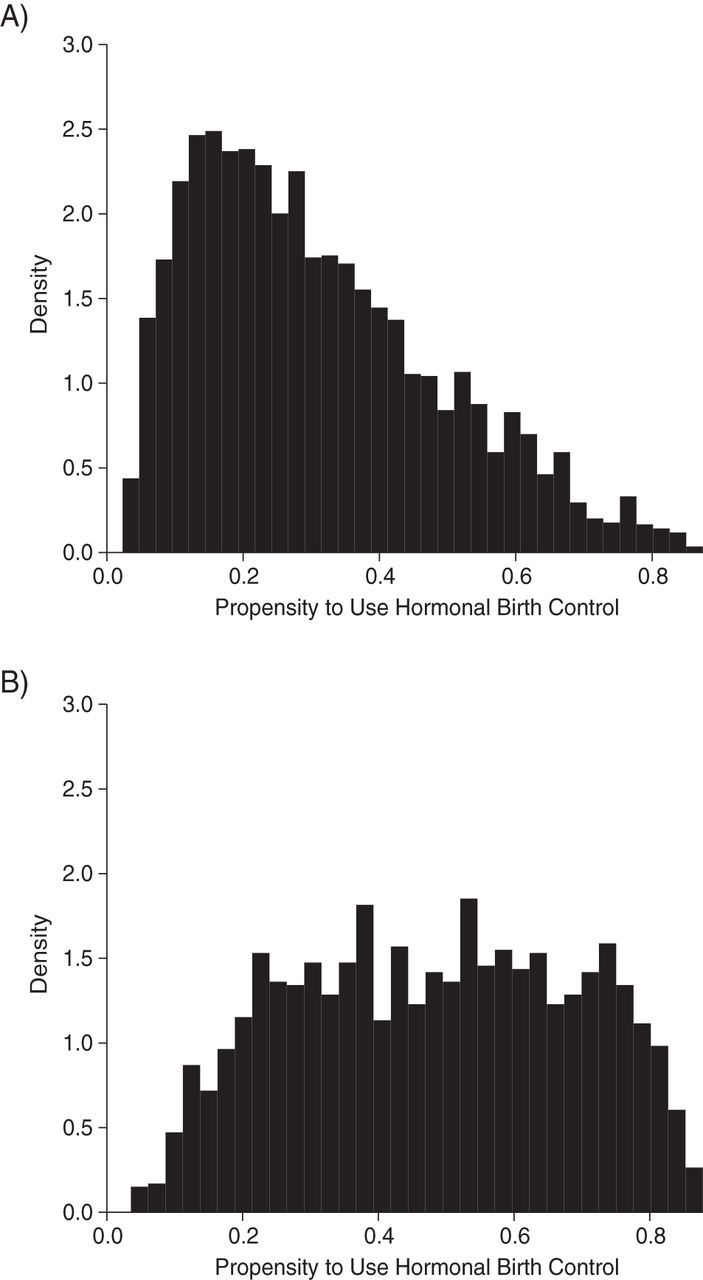
Distribution of propensity scores among users (A) and nonusers (B) of hormonal birth control aged 25–34 years in a nationally representative sample of sexually active nonpregnant US women, National Longitudinal Study of Adolescent Health, 2007–2008.
Table 2.
Distribution of Women Aged 25–34 Years Into Contraception Categories (%) by Quintile of Propensity Score,a National Longitudinal Study of Adolescent Health, 2007–2008
| Effectiveness of Contraceptive Method |
||||
|---|---|---|---|---|
| Quintile of Propensity Score | Highly Effective (n = 831) | Effective (Hormonal) (n = 2,393) | Less Effective (n = 1,913) | Least Effective or None Used (n = 1,310) |
| 5 (>0.83) | 4.2 | 74.5 | 15.1 | 6.2 |
| 4 (0.72–0.83) | 8.0 | 49.0 | 27.5 | 15.5 |
| 3 (0.58–0.71) | 12.4 | 35.9 | 32.6 | 19.2 |
| 2 (0.39–0.57) | 17.4 | 22.7 | 33.2 | 26.8 |
| 1 (<0.39) | 18.0 | 10.4 | 41.0 | 30.6 |
a Propensity to use hormonal contraceptives. Covariates included in the propensity score included study stratum (geographic area), primary sampling unit, sample weight, age, education, race/ethnicity, smoking, parity, monogamy (dichotomous indicator) and number of sex partners in the past year (continuous measure), importance of religion, regular engagement in an individual sport (e.g., running or jogging), body mass index, visiting the dentist in the last 2 years, undergoing a routine checkup by a physician in the last 2 years, prior use of hormonal birth control, prior depressive symptoms, and prior suicide attempts.
Association between hormonal contraceptive use and depression and suicide attempts
When adjusted for propensity score, hormonal contraceptive users had lower mean levels of past-week depressive symptoms (β = −1.04, 95% confidence interval (CI): −1.73, −0.35), lower odds of high levels of depressive symptoms (odds ratio (OR) = 0.68, 95% CI: 0.49, 0.94), and lower odds of past-year suicide attempts (OR = 0.37, 95% CI: 0.14, 0.95). These results held when we adjusted for propensity score as a continuous variable (Table 3), a 5-level categorical quintile variable (results not shown), or a subset within each quintile (direction and magnitude were the same, although power was reduced in some quintiles; results not shown).
Table 3.
Association Between Hormonal Contraceptive Use and Depressive Symptoms in a Nationally Representative US Sample of Sexually Active Nonpregnant Women Aged 25–34 Years, National Longitudinal Study of Adolescent Health, 2007–2008
| Measure of Depressive Symptoms and Effectiveness of Contraceptive Method | No. of Women | Mean Value | β | OR | 95% CI | Adjusted βa | Adjusted ORa | 95% CI | Propensity Scoreb | 95% CI |
|---|---|---|---|---|---|---|---|---|---|---|
| Past-week CES-D depression score (continuous) | ||||||||||
| Highly effectivec | 831 | 6.65 | −0.67 | −1.53, 0.19 | −0.38 | −1.06, 0.30 | −0.89 | −1.68, 0.04 | ||
| Effective (hormonal)d | 2,393 | 5.61 | −1.71* | −2.37, −1.05 | −0.71* | −1.30, −0.11 | −1.04* | −1.73, −0.35 | ||
| Less effectivee | 1,913 | 6.90 | −0.42 | −1.12, 0.27 | −0.24 | −0.86, 0.39 | −0.39 | −1.08, 0.29 | ||
| Least effective or none usedf | 1,310 | 7.32 | 0 | Referent | 0 | Referent | 0 | Referent | ||
| High past-week depression score (CES-D score ≥11) | ||||||||||
| Highly effective | 831 | 20.10 | 0.80 | 0.53, 1.20 | 0.91 | 0.61, 1.35 | 0.74 | 0.50, 1.09 | ||
| Effective (hormonal) | 2,393 | 14.35 | 0.53* | 0.39, 0.72 | 0.81 | 0.58, 1.14 | 0.68* | 0.49, 0.94 | ||
| Less effective | 1,913 | 21.88 | 0.89 | 0.65, 1.22 | 0.99 | 0.70, 1.41 | 0.89 | 0.65, 1.22 | ||
| Least effective or none used | 1,310 | 23.94 | 1 | Referent | 1 | Referent | 1 | Referent | ||
| Any suicide attempt in the past year | ||||||||||
| Highly effective | 831 | 3.59 | 1.71 | 0.65, 4.50 | 1.30 | 0.45, 3.91 | 1.32 | 0.48, 3.58 | ||
| Effective (hormonal) | 2,393 | 0.67 | 0.31* | 0.12, 0.82 | 0.38* | 0.15, 0.97 | 0.37* | 0.14, 0.95 | ||
| Less effective | 1,913 | 2.49 | 1.17 | 0.53, 2.59 | 1.18 | 0.55, 2.55 | 1.20 | 0.54, 2.68 | ||
| Least effective or none used | 1,310 | 3.11 | 1 | Referent | 1 | Referent | 1 | Referent |
Abbreviations: CES-D, Center for Epidemiologic Studies Depression Scale; CI, confidence interval; OR, odds ratio.
* P < 0.05.
a Results were adjusted for age, education, race/ethnicity, smoking, parity, past-year monogamy, lifetime number of vaginal sex partners, importance of religion, regular engagement in an individual sport (e.g., running or jogging), body mass index, visiting the dentist in the last 2 years, going to a physician for a routine checkup in the last 2 years, and prior use of hormonal birth control. Analyses of depression outcomes were also controlled for prior wave highest depression score; analyses of suicide attempts were also controlled for any prior suicide attempt.
b Propensity to use hormonal contraceptives.
c Included vasectomy, intrauterine devices, and tubal ligation.
d Included combination hormonal contraceptives in the form of the contraceptive pill, patch, or ring. Women using known progestin-only forms of contraception (i.e., Depo-Provera (Pfizer Inc., New York, New York) or Norplant (Wyeth Pharmaceuticals, Radnor, Pennsylvania)) were analyzed separately.
e Included condoms, diaphragms, vaginal sponges, and the withdrawal method.
f Included periodic abstinence, spermicides, and contraceptive film.
Results were similar when covariates were controlled in the regression rather than propensity score (Table 3), although the confidence interval for hormonal contraceptive users was wide for high depression levels (OR = 0.81, 95% CI: 0.58, 1.14).
Users of progestin-only hormonal contraceptives
We analyzed the 298 women using hormonal contraceptive formulations that are known to contain progestin only (i.e., Depo-Provera or Norplant) separately from women using other hormonal contraceptives. In fully controlled models, women using progestin-only contraception had significantly lower levels of depressive symptoms than women using the lowest-efficacy contraceptives or no contraceptives (β = −1.3, 95% CI: −2.4, −0.2). Results were consistently protective for high levels of depressive symptoms, although the finding was not significant (OR = 0.7, 95% CI: 0.4, 1.2), and results were not significant or protective for suicide attempts (OR = 1.6, 95% CI: 0.4, 6.1). Women using progestin-only contraceptives did not have significantly different levels of depression symptoms than women using other forms of hormonal contraception (β = −0.3, 95% CI −1.2, 0.6).
Longitudinal associations between hormonal contraceptive use and depression
In Figure 3, we dichotomize contraceptive users into women using hormonal contraceptives (pill, patch, ring, or progestin-only) and all other women, and we show all associations between hormonal contraceptive use and high depression scores across 2 waves of data. There were protective associations between hormonal contraceptive use and high depression scores when both were measured at the wave 3 interview (ages 18–28 years) (OR = 0.76, 95% CI: 0.57, 1.02) and when both were measured at the wave 4 interview (ages 25–34 years) (OR = 0.83, 95% CI: 0.63, 0.98).
Figure 3.
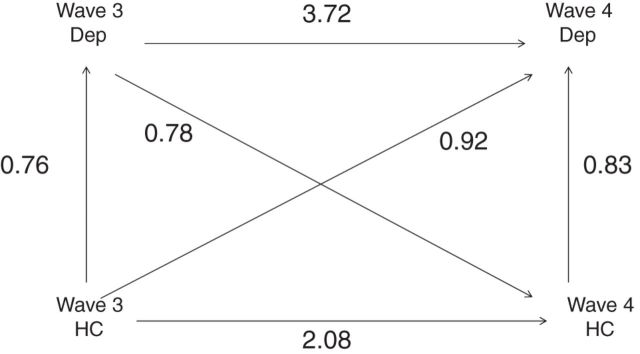
Adjusted odds ratios (ORs) for the association between hormonal contraceptive (HC) use and past-week high depression score (Dep) among nonpregnant women aged 18–34 years with a current sex partner in 2 study waves, National Longitudinal Study of Adolescent Health, 2001–2008. For OR = 0.76, P = 0.06; for OR = 3.72, OR = 0.83, and OR = 2.08, P < 0.05. Wave 3 logistic regression analyses adjusted for race/ethnicity, wave 3 education, age, parity, past-year monogamy, lifetime number of vaginal sex partners, importance of religion, regular engagement in an individual sport (e.g., running or jogging), body mass index, visiting a dentist in the last 2 years, smoking, wave 1 or 2 highest depression score, and wave 1 or 2 use of hormonal birth control. Wave 4 logistic regression analyses adjusted for race/ethnicity and wave 4 age, education, smoking, parity, past-year monogamy, lifetime number of vaginal sex partners, importance of religion, regular engagement in an individual sport (e.g., running or jogging), body mass index, visiting a dentist in the last 2 years, undergoing a routine checkup by a physician in the last 2 years, wave 1, 2, or 3 high depression, and wave 1, 2, or 3 use of hormonal birth control. A high depression score was defined as a score greater than or equal to 11 on the 10-item Center for Epidemiologic Studies Depression Scale.
We then repeated this longitudinal analysis with past-year suicide attempts as the outcome (Figure 4). While hormonal contraceptive use was not protective against suicide attempts at the wave 3 interview (ages 18–28 years), it was protective against suicide attempts at the wave 4 interview (ages 25–34 years) (OR = 0.31, 95% CI: 0.15, 0.66).
Figure 4.
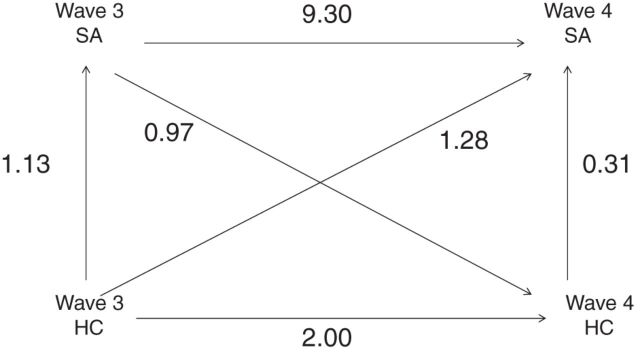
Adjusted odds ratios (ORs) for the association between hormonal contraceptive (HC) use and past-year suicide attempts (SA) among nonpregnant women aged 18–34 years with a current sex partner in 2 study waves, National Longitudinal Study of Adolescent Health, 2001–2008. For OR = 9.30, OR = 0.31, and OR = 2.00, P < 0.05. Wave 3 logistic regression analyses adjusted for race/ethnicity, wave 3 education, age, parity, past-year monogamy, lifetime number of vaginal sex partners, importance of religion, regular engagement in an individual sport (e.g., running or jogging), body mass index, visiting a dentist in the last 2 years, smoking, wave 1 or 2 suicide attempts, and wave 1 or 2 use of hormonal birth control. Wave 4 logistic regression analyses adjusted for race/ethnicity and wave 4 age, education, smoking, parity, past-year monogamy, lifetime number of vaginal sex partners, importance of religion, regular engagement in an individual sport (e.g., running or jogging), body mass index, visiting a dentist in the last 2 years, undergoing a routine checkup by a physician in the last 2 years, wave 1, 2, or 3 suicide attempts, and wave 1, 2, or 3 use of hormonal birth control. A high depression score was defined as a score greater than or equal to 11 on the 10-item Center for Epidemiologic Studies Depression Scale.
DISCUSSION
In the present study, we found a protective association between hormonal contraceptive use and depressive symptoms, as well as suicide attempts, in a population-based sample of young, sexually active US women. These associations persisted even after controlling for all measured factors related to health and lifestyle, including prior depressive symptoms and hormonal contraceptive use. The study documented this effect among these women at 2 different life stages, once in the early 20s and once in the late 20s/early 30s. The protective association with depressive symptoms was found for women using combination estrogen/progesterone formulations as well as among users of progestin-only contraceptives.
These results could have arisen because hormonal contraception reduces or stabilizes levels of depressive symptoms, but they should be interpreted in the context of evidence that women with depressive symptoms are less likely to start and adhere to hormonal contraception regimens. Almost one-third of women who begin using hormonal contraceptives discontinue use within 1 year (35–39). Previous clinical research has documented that women with a history of depression are less likely to choose exogenous hormone use as a contraception method (40) and are more likely to discontinue use even if they begin using hormonal contraceptives (37, 41–46). Further, women who perceive a negative mood effect of hormonal contraceptives are more likely to discontinue use (47, 48). Women who discontinue use of oral contraceptives because of side effects are less likely to restart (49). Thus, hormonal contraceptive users at any time point may be overselected for less depression than nonusers of hormonal contraceptives. Indeed, odds ratios were in the direction of women with high depression scores being less likely to subsequently use hormonal contraception (Figure 3). However, controlling for past depressive symptoms, the protective association of hormonal contraceptives with depressive symptoms and suicide attempts remained robust. Nevertheless, the associations presented here are likely to at least partially reflect a nonadherence effect related to depressed mood. This underscores the importance of identification and treatment of women with depression in order to promote health in other domains, such as reproductive health and medication adherence.
Existing literature on hormonal contraception and depression has been primarily confined to small, unrepresentative samples. Among these smaller studies, few cohesive findings have emerged. Daily diary studies have produced conflicting results, with some finding no mood differences across the cycle when comparing users with nonusers (50–52) and some finding improvement in mood (53), as well as clinically significant positive affect (54) and sexual desire (55, 56), and others finding heightened negative mood (37, 49, 57) and negative reaction to stressors (58). A consistent finding in the literature is that there is less variation in mood among women taking hormonal contraceptives (reviewed by Oinonen and Mazmanian (59)), which corresponds to clinical research showing that women who experience severe mood problems during the menstrual cycle (e.g., premenstrual dysphoric disorder) demonstrate improvement on hormonal contraceptives due to a more stable mood across the cycle (60–63). In that context, our findings show strong and robust associations, with hormonal contraceptive users being at substantially reduced risk for depressed mood in one of the largest population-based studies to have examined this issue in the literature.
Estrogen has widespread effects on the brain and behavior through direct and indirect genomic and nongenomic actions (see McEwen et al. (64) for a detailed review). Estrogen receptors have been found in the hypothalamus, amygdala, hippocampus, and prefrontal cortex and in autonomic centers of the brain stem. In these regions, estrogen receptors are detectable in neuronal cell bodies, dendrites, presynaptic terminals, mitochondria, and glial cells. Through these receptors, estrogens modulate neuroplastic processes as well the activity of the major neurotransmitter and neuromodulator systems, including the cholinergic, noradrenergic, serotonergic, dopaminergic, glutamatergic, neuropeptide Y, and opioidergic systems, as well as brain-derived neurotrophic factor and second messenger pathways—all of which have been implicated in the pathophysiology of mood disorders (64). Through such mechanisms, estrogen may exert mood-regulating effects in oral contraceptive users. In addition, through its effects on the hippocampus and hypothalamus, estrogen modulates the activity and reactivity of the hypothalamic-pituitary-adrenal axis, which in turn is implicated in the pathophysiology of depression and mood regulation (64). Further, exogenous estrogen can affect cortisol responses and hypothalamic-pituitary-adrenal activity, which are both implicated in the regulation of mood (64). For example, Kirschbaum et al. (65) documented that free salivary cortisol responses to a laboratory-generated psychosocial stressor were lowest among hormonal contraceptive users as compared with men as well as women in the luteal and follicular phases, while total cortisol responses did not differ between groups, suggesting a higher level of cortisol-binding globulin in the hormonal contraceptive users. Recent evidence also indicates substantially increased cortisol-binding globulin among hormonal contraceptive users compared with noncompliant users (66). By binding free cortisol, cortisol-binding globulin inactivates the hormone's effects, leading to a reduced biologically active portion of circulating cortisol. A reduction of bioactive cortisol in hormonal contraceptive users could potentially be neuroprotective under conditions of chronic stress, thereby reducing depression risk.
Little research has examined the role of exogenous hormone use in suicidality, and existing research has focused on mortality from suicide rather than suicide attempts. Hannaford et al. (19) documented a suggestive increase in the risk of suicide mortality among oral contraceptive users, although mortality could occur long after use rather than concurrently, and results are not consistent with those of other large cohort studies (20, 21). Risk factors for attempted suicide differ substantially from risk factors for completed suicide (22); thus, different associations with hormonal contraceptive use are likely. Emerging evidence suggests that women in the late luteal phase of the menstrual cycle may be at heightened risk for suicide attempts and severe suicide attempts (67, 68); thus, hormonal contraceptive use may prove to be a useful adjunct in stabilizing mood among women with suicidal ideation.
Several limitations of this study are notable. While we were able to control for a wide range of factors associated with the decision to use hormonal contraceptives, residual confounding as an explanation for these results cannot be ruled out because of the study's observational design. The decision to use a particular type of contraception is not randomly distributed; women in stable partnerships may choose a method with more stability, such as sterilization, an IUD, or a hormonal method, although available data indicate that barrier protection remains a popular choice among women in stable partnerships (25, 69). In this sample, women in monogamous relationships chose barrier protection less frequently than hormonal contraception. Thus, relationship factors such as partnership stability and overall health-care utilization may be related to both hormonal contraceptive decisions and levels of depressive symptoms. These differences underscore our analytical plan to examine different groups of contraceptive users; among users of highly effective methods (e.g., sterilization, IUD), we found no association with depressive symptoms or suicide attempts, suggesting that partnership stability does not explain the relationships observed here. Further, we also controlled for a monogamous partnership in the past year. Nevertheless, continued research in study samples with comprehensive information on the stability and satisfaction of sexual partnerships would enhance our ability to make causal inferences about these associations.
Further, we did not have information on the hormonal contraceptive formulations used by women in this study. Estrogen and progestin doses vary by formulation, and such information would be helpful in establishing the specificity of this association, as well as potential dose-response. We also did not have information on whether IUDs contained hormones. However, assuming that these users would be expected to have lower levels of depressive symptoms, this potential misclassification would bias the users of highly effective contraceptives towards lower levels of depressive symptoms than we report. Data on synthetic estrogen and progestin dose are also critical as a next step in this research, so that a potential dose-response or threshold can be established.
Finally, our results are generalizable only to sexually active women, because questions regarding contraceptive use were asked in the context of current partnerships. Women who are not in sexual relationships may be using hormonal contraception for a variety of reasons.
In summary, these results, notwithstanding limitations of study design and measurement, warrant further investigation of the potentially protective effects of hormonal contraceptives on mood in epidemiologic studies. Depression remains one of the most disabling health conditions worldwide (70), and it disproportionately affects women. Given the widespread prevalence of hormonal contraceptive use among young women in the United States and worldwide, systematic investigation of the role of exogenous hormones (including potential dose-response relationships) in regulating mood, as well as the role of mood in predicting nonadherence to hormonal contraceptive regimens, is warranted.
ACKNOWLEDGMENTS
Author affiliations: Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, New York (Katherine M. Keyes, Keely Cheslack-Postava, Carolyn Westhoff, Michelle Haloossim, Kate Walsh, Karestan Koenen); Department of Obstetrics and Gynecology, Mailman School of Public Health, Columbia University, New York, New York (Carolyn Westhoff); and Center for Human and Health Sciences, Institute of Medical Psychology, Charité–Universitätsmedizin Berlin, Berlin, Germany (Christine M. Heim).
All authors contributed equally to the work.
This research was supported in part by the National Institute of Alcohol Abuse and Alcoholism (grant K01AA021511 to K.M.K.), the New York State Psychiatric Institute (funding for K.M.K.), the Columbia University Department of Epidemiology (funding for K.M.K.), and the National Institute of Mental Health (grant T32-13043 to K.C.P.).
The funding organizations played no role in the design and conduct of the study; the collection, management, analysis, and interpretation of the data; or the preparation, review, and approval of the manuscript.
Conflict of interest: none declared.
REFERENCES
- 1.Chandra A, Martinez GM, Mosher WD, et al. Fertility, family planning, and reproductive health of U.S. women: data from the 2002 National Survey of Family Growth. Vital Health Stat 23. 2005;(25):1–160. [PubMed] [Google Scholar]
- 2.Kaunitz AM. Oral contraceptive health benefits: perception versus reality. Contraception. 1999;59(suppl 1):29S–33S. doi: 10.1016/s0010-7824(98)00135-8. [DOI] [PubMed] [Google Scholar]
- 3.King J. Noncontraceptive uses of hormonal contraception. J Midwif Wom Health. 2011;56(6):628–635. doi: 10.1111/j.1542-2011.2011.00118.x. [DOI] [PubMed] [Google Scholar]
- 4.Maguire K, Westhoff C. The state of hormonal contraception today: established and emerging noncontraceptive health benefits. Am J Obstet Gynecol. 2011;205(suppl 4):S4–S8. doi: 10.1016/j.ajog.2011.06.056. [DOI] [PubMed] [Google Scholar]
- 5.Shufelt CL, Bairey Merz CN. Contraceptive hormone use and cardiovascular disease. J Am Coll Cardiol. 2009;53(3):221–231. doi: 10.1016/j.jacc.2008.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hasin DS, Goodwin RD, Stinson FS, et al. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 7.Rushton JL, Forcier M, Schectman RM. Epidemiology of depressive symptoms in the National Longitudinal Study of Adolescent Health. J Am Acad Child Adolesc Psychiatry. 2002;41(2):199–205. doi: 10.1097/00004583-200202000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Wight RG, Sepulveda JE, Aneshensel CS. Depressive symptoms: how do adolescents compare with adults? J Adolesc Health. 2004;34(4):314–323. doi: 10.1016/j.jadohealth.2003.05.003. [DOI] [PubMed] [Google Scholar]
- 9.McEwen BS. Invited review: estrogens effects on the brain: multiple sites and molecular mechanisms. J Appl Physiol. 2001;91(6):2785–2801. doi: 10.1152/jappl.2001.91.6.2785. [DOI] [PubMed] [Google Scholar]
- 10.Schmidt PJ, Nieman LK, Danaceau MA, et al. Differential behavioral effects of gonadal steroids in women with and in those without premenstrual syndrome. N Engl J Med. 1998;338(4):209–216. doi: 10.1056/NEJM199801223380401. [DOI] [PubMed] [Google Scholar]
- 11.Joffe H, Cohen LS. Estrogen, serotonin, and mood disturbance: where is the therapeutic bridge? Biol Psychiatry. 1998;44(9):798–811. doi: 10.1016/s0006-3223(98)00169-3. [DOI] [PubMed] [Google Scholar]
- 12.Payne JL. The role of estrogen in mood disorders in women. Int Rev Psychiatry. 2003;15(3):280. doi: 10.1080/0954026031000136893. [DOI] [PubMed] [Google Scholar]
- 13.Cohen LS, Soares CN, Vitonis AF, et al. Risk for new onset of depression during the menopausal transition: the Harvard study of moods and cycles. Arch Gen Psychiatry. 2006;63(4):385–390. doi: 10.1001/archpsyc.63.4.385. [DOI] [PubMed] [Google Scholar]
- 14.Young EA, Midgley AR, Carlson NE, et al. Alteration in the hypothalamic-pituitary-ovarian axis in depressed women. Arch Gen Psychiatry. 2000;57(12):1157–1162. doi: 10.1001/archpsyc.57.12.1157. [DOI] [PubMed] [Google Scholar]
- 15.Harlow BL, Wise LA, Otto MW, et al. Depression and its influence on reproductive endocrine and menstrual cycle markers associated with perimenopause: the Harvard Study of Moods and Cycles. Arch Gen Psychiatry. 2003;60(1):29–36. doi: 10.1001/archpsyc.60.1.29. [DOI] [PubMed] [Google Scholar]
- 16.Duke JM, Sibbritt DW, Young AF. Is there an association between the use of oral contraception and depressive symptoms in young Australian women? Contraception. 2007;75(1):27–31. doi: 10.1016/j.contraception.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 17.Joffe H, Cohen LS, Harlow BL. Impact of oral contraceptive pill use on premenstrual mood: predictors of improvement and deterioration. Am J Obstet Gynecol. 2003;189(6):1523–1530. doi: 10.1016/s0002-9378(03)00927-x. [DOI] [PubMed] [Google Scholar]
- 18.Toffol E, Heikinheimo O, Koponen P, et al. Hormonal contraception and mental health: results of a population-based study. Hum Reprod. 2011;26(11):3085–3093. doi: 10.1093/humrep/der269. [DOI] [PubMed] [Google Scholar]
- 19.Hannaford PC, Iversen L, Macfarlane TV, et al. Mortality among contraceptive pill users: cohort evidence from Royal College of General Practitioners’ Oral Contraception Study. BMJ. 2010;340:c927. doi: 10.1136/bmj.c927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Colditz GA. Oral contraceptive use and mortality during 12 years of follow-up: the Nurses’ Health Study. Ann Intern Med. 1994;120(10):821–826. doi: 10.7326/0003-4819-120-10-199405150-00002. [DOI] [PubMed] [Google Scholar]
- 21.Vessey M, Painter R, Yeates D. Mortality in relation to oral contraceptive use and cigarette smoking. Lancet. 2003;362(9379):185–191. doi: 10.1016/S0140-6736(03)13907-4. [DOI] [PubMed] [Google Scholar]
- 22.Nock MK, Borges G, Bromet EJ, et al. Suicide and suicidal behavior. Epidemiol Rev. 2008;30:133–154. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harris KM. Chapel Hill, NC: Carolina Population Center, University of North Carolina at Chapel Hill; 2009. The National Longitudinal Study of Adolescent Health (Add Health), Waves I & II, 1994–1996; Wave III, 2001–2002; Wave IV, 2007–2009 [machine-readable data file and documentation] [Google Scholar]
- 24.Trussell J. Contraceptive efficacy. In: Hatcher RA, Trussell J, Nelson J, et al., editors. Contraceptive Technology: Nineteenth Revised Edition. New York, NY: Ardent Media; 2007. pp. 19–41. [Google Scholar]
- 25.Mosher WD, Jones J. Use of contraception in the United States: 1982–2008. Vital Health Stat 23. 2010;(29):1–44. [PubMed] [Google Scholar]
- 26.Andresen EM, Malmgren JA, Carter WB, et al. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- 27.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 28.Boey KW. Cross-validation of a short form of the CES-D in Chinese elderly. Int J Geriatr Psychiatry. 1999;14(8):608–617. doi: 10.1002/(sici)1099-1166(199908)14:8<608::aid-gps991>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 29.Bradley KL, Bagnell AL, Brannen CL. Factorial validity of the Center for Epidemiological Studies Depression 10 in adolescents. Issues Ment Health Nurs. 2010;31(6):408–412. doi: 10.3109/01612840903484105. [DOI] [PubMed] [Google Scholar]
- 30.Brewster KL, Cooksey EC, Guilkey DK, et al. The changing impact of religion on the sexual and contraceptive behavior of adolescent women in the United States. J Marriage Fam. 1998;60(2):493–504. [Google Scholar]
- 31.Goldscheider C, Mosher WD. Patterns of contraceptive use in the United States: the importance of religious factors. Stud Fam Plann. 1991;22(2):102–115. [PubMed] [Google Scholar]
- 32.Westgate CE. Spiritual wellness and depression. J Counsel Develop. 1996;75(1):26–35. [Google Scholar]
- 33.Little RJ, Vartivarian S. On weighting the rates in non-response weights. Stat Med. 2003;22(9):1589–1599. doi: 10.1002/sim.1513. [DOI] [PubMed] [Google Scholar]
- 34.Austin PC. The performance of different propensity-score methods for estimating relative risks. J Clin Epidemiol. 2008;61(6):537–545. doi: 10.1016/j.jclinepi.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 35.Rosenberg MJ, Waugh MS, Long S. Unintended pregnancies and use, misuse and discontinuation of oral contraceptives. J Reprod Med. 1995;40(5):355–360. [PubMed] [Google Scholar]
- 36.Ali M, Cleland JL. Contraceptive discontinuation in six developing countries: a cause-specific analysis. Int Fam Plann Perspect. 1995;21(3):92–97. [Google Scholar]
- 37.Hall KS, White KO, Rickert VI, et al. Influence of depressed mood and psychological stress symptoms on perceived oral contraceptive side effects and discontinuation in young minority women. Contraception. 2012;86(5):518–525. doi: 10.1016/j.contraception.2012.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Westhoff CL, Heartwell S, Edwards S, et al. Oral contraceptive discontinuation: do side effects matter? Am J Obstet Gynecol. 2007;196(4):412.e1–412.e6. doi: 10.1016/j.ajog.2006.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nelson AL, Westhoff C, Schnare SM. Real-world patterns of prescription refills for branded hormonal contraceptives: a reflection of contraceptive discontinuation. Obstet Gynecol. 2008;112(4):782–787. doi: 10.1097/AOG.0b013e3181875ec5. [DOI] [PubMed] [Google Scholar]
- 40.Garbers S, Correa N, Tobier N, et al. Association between symptoms of depression and contraceptive method choices among low-income women at urban reproductive health centers. Matern Child Health J. 2010;14(1):102–109. doi: 10.1007/s10995-008-0437-y. [DOI] [PubMed] [Google Scholar]
- 41.Herzberg BN, Draper KC, Johnson AL, et al. Oral contraceptives, depression, and libido. BMJ. 1971;3(5773):495–500. doi: 10.1136/bmj.3.5773.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Borgstrom A, Odlind V, Ekselius L, et al. Adverse mood effects of combined oral contraceptives in relation to personality traits. Eur J Obstet Gynecol Reprod Biol. 2008;141(2):127–130. doi: 10.1016/j.ejogrb.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 43.Borgstrom A, Kask K, Gulinello M, et al. Patients with adverse mood effects from combined oral contraceptives have lower levels of prepulse inhibition than healthy controls. Psychoneuroendocrinology. 2008;33(4):487–496. doi: 10.1016/j.psyneuen.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 44.Ernst U, Baumgartner L, Bauer U, et al. Improvement of quality of life in women using a low-dose desogestrel-containing contraceptive: results of an observational clinical evaluation. Eur J Contracept Reprod Health Care. 2002;7(4):238–243. [PubMed] [Google Scholar]
- 45.Robinson SA, Dowell M, Pedulla D, et al. Do the emotional side-effects of hormonal contraceptives come from pharmacologic or psychological mechanisms? Med Hypoth. 2004;63(2):268–273. doi: 10.1016/j.mehy.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 46.Westhoff C, Truman C, Kalmuss D, et al. Depressive symptoms and Norplant contraceptive implants. Contraception. 1998;57(4):241–245. doi: 10.1016/s0010-7824(98)00022-5. [DOI] [PubMed] [Google Scholar]
- 47.Sanders SA, Graham CA, Bass JL, et al. A prospective study of the effects of oral contraceptives on sexuality and well-being and their relationship to discontinuation. Contraception. 2001;64(1):51–58. doi: 10.1016/s0010-7824(01)00218-9. [DOI] [PubMed] [Google Scholar]
- 48.Wiebe ER, Brotto LA, MacKay J. Characteristics of women who experience mood and sexual side effects with use of hormonal contraception. J Obstet Gynaecol Can. 2011;33(12):1234–1240. doi: 10.1016/S1701-2163(16)35108-8. [DOI] [PubMed] [Google Scholar]
- 49.Kalmuss D, Koenemann S, Westhoff C, et al. Prior pill experiences and current continuation among pill restarters. Perspect Sex Reprod Health. 2008;40(3):138–143. doi: 10.1363/4013808. [DOI] [PubMed] [Google Scholar]
- 50.O'Connell K, Davis AR, Kerns J. Oral contraceptives: side effects and depression in adolescent girls. Contraception. 2007;75(4):299–304. doi: 10.1016/j.contraception.2006.09.008. [DOI] [PubMed] [Google Scholar]
- 51.Walker A, Bancroft J. Relationship between premenstrual symptoms and oral contraceptive use: a controlled study. Psychosom Med. 1990;52(1):86–96. doi: 10.1097/00006842-199001000-00007. [DOI] [PubMed] [Google Scholar]
- 52.Graham CA, Sherwin BB. A prospective treatment study of premenstrual symptoms using a triphasic oral contraceptive. J Psychosom Res. 1992;36(3):257–266. doi: 10.1016/0022-3999(92)90090-o. [DOI] [PubMed] [Google Scholar]
- 53.Sadler C, Smith H, Hammond J, et al. Lifestyle factors, hormonal contraception, and premenstrual symptoms: The United Kingdom Southampton Women's Survey. J Womens Health (Larchmt) 2010;19(3):391–396. doi: 10.1089/jwh.2008.1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Almagor M, Ben-Porath YS. Mood changes during the menstrual cycle and their relation to the use of oral contraceptive. J Psychosom Res. 1991;35(6):721–728. doi: 10.1016/0022-3999(91)90123-6. [DOI] [PubMed] [Google Scholar]
- 55.Heiman JR, Rupp H, Janssen E, et al. Sexual desire, sexual arousal and hormonal differences in premenopausal US and Dutch women with and without low sexual desire. Horm Behav. 2011;59(5):772–779. doi: 10.1016/j.yhbeh.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 56.Nappi RE, Albani F, Tonani S, et al. Psychosexual well-being in women using oral contraceptives containing drospirenone. Funct Neurol. 2009;24(2):71–75. [PubMed] [Google Scholar]
- 57.Halbreich U, Kahn LS. Role of estrogen in the aetiology and treatment of mood disorders. CNS Drugs. 2001;15(10):797–817. doi: 10.2165/00023210-200115100-00005. [DOI] [PubMed] [Google Scholar]
- 58.Rubino-Watkins MF, Doster JA, Franks S, et al. Oral contraceptive use: implications for cognitive and emotional functioning. J Nerv Ment Dis. 1999;187(5):275–280. doi: 10.1097/00005053-199905000-00002. [DOI] [PubMed] [Google Scholar]
- 59.Oinonen KA, Mazmanian D. To what extent do oral contraceptives influence mood and affect? J Affect Disord. 2002;70(3):229–240. doi: 10.1016/s0165-0327(01)00356-1. [DOI] [PubMed] [Google Scholar]
- 60.Freeman EW, Kroll R, Rapkin A, et al. Evaluation of a unique oral contraceptive in the treatment of premenstrual dysphoric disorder. J Womens Health Gend Based Med. 2001;10(6):561–569. doi: 10.1089/15246090152543148. [DOI] [PubMed] [Google Scholar]
- 61.Freeman MP. Depression and hormonal contraception. JAMA. 2001;286(6):671–672. doi: 10.1001/jama.286.6.671. [DOI] [PubMed] [Google Scholar]
- 62.Felthous AR, Robinson DB, Conroy RW. Prevention of recurrent menstrual psychosis by an oral contraceptive. Am J Psychiatry. 1980;137(2):245–246. doi: 10.1176/ajp.137.2.245. [DOI] [PubMed] [Google Scholar]
- 63.Joffe H, Petrillo LF, Viguera AC, et al. Treatment of premenstrual worsening of depression with adjunctive oral contraceptive pills: a preliminary report. J Clin Psychiatry. 2007;68(12):1954–1962. doi: 10.4088/jcp.v68n1218. [DOI] [PubMed] [Google Scholar]
- 64.McEwen BS, Akama KT, Spencer-Segal JL, et al. Estrogen effects on the brain: actions beyond the hypothalamus via novel mechanisms. Behav Neurosci. 2012;126(1):4–16. doi: 10.1037/a0026708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kirschbaum C, Kudelka BM, Gaab J, et al. Impact of gender, menstrual cycle phase, and oral contraceptives on the activity of the hypothalamus-pituitary-adrenal axis. Psychosom Med. 1999;61(2):154. doi: 10.1097/00006842-199903000-00006. [DOI] [PubMed] [Google Scholar]
- 66.Westhoff CL, Petrie KA, Cremers S. Using changes in binding globulins to assess oral contraceptive compliance. Contraception. 2012;87(2):176–181. doi: 10.1016/j.contraception.2012.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Baca-Garcia E, Diaz-Sastre C, Ceverino A, et al. Suicide attempts among women during low estradiol/low progesterone states. J Psychiatr Res. 2010;44(4):209–214. doi: 10.1016/j.jpsychires.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 68.Sein Anand J, Chodorowski Z, Ciechanowicz R, et al. The relationship between suicidal attempts and menstrual cycle in women. Przeglad Lekarski. 2005;62(6):431–433. [PubMed] [Google Scholar]
- 69.Gemzell-Danielsson K, Cho S, Inki P, et al. Use of contraceptive methods and contraceptive recommendations among health care providers actively involved in contraceptive counseling—results of an international survey in 10 countries. Contraception. 2012;86(6):631–638. doi: 10.1016/j.contraception.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 70.Ustün TB, Ayuso-Mateos JL, Chatterji S, et al. Global burden of depressive disorders in the year 2000. Br J Psychiatry. 2004;184:386–392. doi: 10.1192/bjp.184.5.386. [DOI] [PubMed] [Google Scholar]


