Abstract
Breast cancer is the second leading cause of cancer death in women in the United States. Metastasis accounts for the death of ~90 % of these patients, yet the mechanisms underlying this event remain poorly defined. WAVE3 belongs to the WASP/WAVE family of actin-binding proteins that play essential roles in regulating cell morphology, actin polymerization, cytoskeleton remodeling, cell motility, and invasion. Accordingly, we demonstrated previously that WAVE3 promotes the acquisition of invasive and metastatic phenotypes by human breast cancers. Herein, we show that transforming growth factor-β (TGF-β) selectively and robustly induced the expression of WAVE3 in metastatic breast cancer cells, but not in their nonmetastatic counterparts. Moreover, the induction of WAVE3 expression in human and mouse triple-negative breast cancer cells (TNBCs) by TGF-β likely reflects its coupling to microRNA expression via a Smad2- and β3 integrin-dependent mechanism. We further demonstrate the requirement for WAVE3 expression in mediating the initiation of epithelial–mesenchymal transition (EMT) programs stimulated by TGF-β. Indeed, stable depletion of WAVE3 expression in human TNBC cells prevented TGF-β from inducing EMT programs and from stimulating the proliferation, migration, and the formation of lamellipodia in metastatic TNBC cells. Lastly, we observed WAVE3 deficiency to abrogate the outgrowth of TNBC cell organoids in 3-dimensional organotypic cultures as well as to decrease the growth and metastasis of 4T1 tumors produced in syngeneic Balb/C mice. Indeed, WAVE3 deficiency significantly reduced the presence of sarcomatoid morphologies indicative of EMT phenotypes in pulmonary TNBC tumors as compared to those detected in their parental counterparts. Collectively, these findings indicate the necessity for WAVE3 expression and activity during EMT programs stimulated by TGF-β; they also suggest that measures capable of inactivating WAVE3 may play a role in alleviating metastasis stimulated by TGF-β.
Keywords: Breast cancer, EMT, Metastasis, TGF-β, WAVE3
Introduction
Breast cancer is a heterogeneous disease that can be classified into at least five genetically distinct subtypes [1]. Luminal breast cancers that are estrogen receptor positive (ER+) and low grade have the best prognosis, while those that lack expression of hormone receptors (ER-α and progesterone (PR)) and fail to exhibit amplification of ErbB2/HER2 are classified as triple-negative breast cancers (TNBCs), and display the poorest clinical outcomes due to their increased propensity to metastasize and recur [2, 3]. Indeed, metastasis accounts for ~90 % of the mortality observed in breast cancer patients [4]; it is also a multistep process whereby mammary carcinoma cells (i) detach and migrate out of the primary tumor microenvironment, (ii) intravasate into the circulatory system, and (iii) extravasate out of the circulation and invade distant sites of metastasis, at which point they can acquire dormant or actively proliferating phenotypes [5]. Recently, epithelial–mesenchymal transition (EMT) programs have been implicated as potential drivers of breast cancer metastasis in part by eliciting dramatic cytoskeleton remodeling from apical–basolateral polarities characteristic of epithelial cells to the synthesis of actin stress fibers characteristic of mesenchymal cells [6]. Consequently, EMT programs induce immotile mammary epithelial cells (MECs) to acquire invasive and migratory phenotypes, as well as to exhibit cancer stem cell-like and chemoresistant behaviors. We previously established WAVE3 as a critical regulator of actin cytoskeletal remodeling [7–12], doing so by recruitment of the Arp2/3 complex that regulates actin polymerization and enhances lamellipodia formation at the leading edge of migratory cells [13]. Along these lines, aberrant increases in WAVE3 expression enhance the migration and invasion of TNBCs [11, 14], suggesting that therapeutic targeting of WAVE3 or oncogenic signaling pathways coupled to its expression in TNBCs may offer novel inroads to inhibit their metastatic progression.
Transforming growth factor-β (TGF-β) is a multifunctional cytokine that regulates all stages of mammary gland development as well as suppresses the transformation and tumor formation of MECs. However, as mammary tumors continue to develop and progress, TGF-β typically loses its tumor-suppressor function and ultimately acquires tumor-promoting behaviors, which collectively enhance breast cancer proliferation, invasion, and metastasis in part via the stimulation of EMT programs [6, 15]. Indeed, numerous studies have established TGF-β as a master regulator of EMT in a variety of normal and malignant cells and tissues, including those of the breast. Unfortunately, the precise sequence of events that engender the conversion of TGF-β function during mammary tumorigenesis remains incompletely understood, as does a detailed understanding of the molecular mechanisms through which TGF-β induces EMT programs. This knowledge gap is complicated by the ability of TGF-β to activate a bifurcated signaling system that comprises canonical (i.e., Smad2/3/4-dependent) and noncanonical (i.e., Smad2/3/4-independent) signaling inputs, both of which coalesce in promoting EMT reactions stimulated by TGF-β [6, 15].
Despite the documented abilities of TGF-β and WAVE3 to drive the acquisition of EMT and metastatic phenotypes in late-stage breast cancers, it remains completely unknown as to whether TGF-β and WAVE3 function in linear or parallel pathways coupled to breast cancer development and metastatic progression. As such, we sought to examine whether TGF-β is coupled to WAVE3 expression in normal and malignant MECs, and if so, to determine the role of WAVE3 in regulating oncogenic activities of TGF-β and its coupling to EMT and metastasis in TNBCs.
Materials and methods
Cell culture and cDNA constructs
Normal mouse NMuMG cells were obtained from ATCC (Manassas, VA, USA), while their (i) EGFR-transformed and nonmetastatic NME derivatives were described previously [16], and (ii) highly metastatic NME-LM2 derivatives were obtained by ex vivo isolation of pulmonary NME tumor cells, which were subsequently amplified twice through nude mice. Metastatic human MDA-MB-231 cells were purchased from ATCC, while nonmetastatic 67NR, weakly metastatic 4T07, and highly metastatic 4T1 cells were provided by Fred Miller (Wayne State University, Detroit, Michigan, USA). Firefly luciferase-expressing 4T1 cells were described previously [17, 18]. MDA-MB-231 and 4T1 cells rendered deficient in WAVE3 expression were generated by lentiviral-mediated transduction using a scrambled (nonsilencing shRNA) or verified WAVE3 shRNA encoded in pLKO.1-puro from Sigma (Saint Louis MO, USA) as previously described [19, 20]. The extent of WAVE3 deficiency was determined by immunoblotting for WAVE3 as described below.
Semi-quantitative real-time PCR analyses
Total RNA was purified using the RNeasy Plus Mini Kit (QIAGEN, Valencia, CA, USA). Afterward, cDNAs were synthesized using the miScript Reverse Transcription Kit (QIAGEN), and subsequently diluted 10-fold in H2O prior to their use in semi-quantitative real-time PCR reactions that contained 10 μl SsoFast EvaGreen (Bio-Rad, Hercules, CA, USA), 1 μl each of the forward and reverse primers, 3 μl H2O, and 5 μl diluted cDNA. Individual transcript expression levels were analyzed on either a 7500 Fast Real-Time PCR System (Applied Biosystems, Foster City CA, USA) or a MyiQ2 iCycler PCR system (BioRad). Differences in total RNA concentration were normalized to their corresponding GAPDH signals. The human primer sets used were as follows: (a) E-cadherin: forward, 5′-CAT CTTTGTGCCT CCTGAAA; reverse, 5′-TGGGCAGTGT AGGATGTG; (b) N-cadherin: forward, 5′-CCTGCTTAT CCTTGTGCTGA; reverse, 5′-CCTGGTCTTCTTCTCCT CCA; (c) Vimentin: forward 5′-CAAAGC AGGAGTCC ACTGAG; reverse, 5′-TAAGGGCATCCACTTCACAG; and (d) GAPDH: forward, 5′-TCCATGACAACTTTGGT ATTCGT; reverse, 5′-AGTAGAGGCAGGGATGATGTT. Additionally, WAVE3 primer sets were purchased from Qiagen and used as described [14].
Cell migration, invasion, and proliferation assays
Alterations in 4T1 cell migration were assessed by wounding confluent cultures with a micropipette tip, and immediately placing in serum-free medium supplemented with or without TGF-β1 (5 ng/ml). Bright-field images were obtained immediately after wounding, and again at various times thereafter during the ensuing 24 h. The extent of wound closure was quantitated by measuring the wound areas obtained from five independent fields using ImageJ (v1.34s). For invasion assays, modified Boyden chambers were coated with Matrigel (1:10 dilution; BD Biosciences, San Jose, CA, USA) and used to measure the invasiveness of 67NR and 4T1 cells in response to 10 % serum and TGF-β1 (5 ng/ml) as described [21]. Finally, alterations in MDA-MB-231 and 4T1 cell proliferation (10,000 cells/well) were determined by monitoring the incorporation of [3H]thymidine into cellular DNA as described [22].
3-Dimensional (3D) organotypic culture and outgrowth assays
Compliant 3D organotypic cultures were performed using the “on-top” method [23] as described [24]. Briefly, MDA-MB-231 and 4T1 cells were cultured on Cultrex cushions (100 %; Trevigen, Gaithersburg, MD, USA) in complete medium supplemented with 5 % Cultrex. Where indicated, the cells were treated with TGF-β1 (5 ng/ml) for 11 days, during which the medium/Cultrex solution was replaced once every 4 days. Alterations in organoid growth arising from manipulations of WAVE3 expression were quantified by the performance of bioluminescent growth assays as described previously [19]. Briefly, organoid growth rates were detected by the addition of D-luciferin (Gold Biotechnology, St. Louis, MO, USA) to induce bioluminescence, which was quantified on a GloMax-Multi Detection System (Promega, Madison, WI, USA). Cell proliferation was normalized to initial bioluminescent signals that were obtained 18 h after plating.
Immunoblotting analyses
Control (i.e., nonsilencing shRNA) and WAVE3-deficient MDA-MB-231 and 4T1 cells were incubated in the absence or presence of TGF-β1 (5 ng/ml) for varying times over a span of 48 h, at which point they were solubilized in Buffer H/1 % Triton X-100 and prepared for immunoblotting as described [25]. The following primary antibodies were used: (a) anti-WAVE3 (1:500; Cell Signaling, Danvers, MA, USA); (b) anti-phopho-Smad2 (1:1000; Cell Signaling); (c) anti-phospho-Smad3 (1:500; Cell Signaling); (d) anti-Smad2/3 (1:1000; Cell Signaling); (e) anti-phos-pho-p38 MAPK (1:500; Cell Signaling); (f) anti-p38 MAPK (1:1000; Santa Cruz Biotechnology, Dallas, Texas, USA); (g) anti-fibronectin (1:1000; Sigma); (h) anti-vimentin (1:5000; BD Biosciences); (i) anti-β1 integrin (1:1000; Millipore, Billerica, MA, USA); and (j) anti-β3 integrin (1:1000; Cell Signaling).
4T1 tumor growth, metastasis, and IHC analyses
Control (i.e., nonsilencing shRNA) and WAVE3-deficient luciferase-expressing 4T1 cells were engrafted (10,000 cells/mouse) onto the mammary fat pads of female Balb/C mice. The growth and metastasis of primary 4T1 tumors were quantified by weekly bioluminescent imaging of tumor-bearing animals on a Xenogen IVIS-200 (Caliper Life Sciences, Hopkinton, MA, USA) in the Imaging Research Core (Case Comprehensive Cancer Center, Cleveland, OH, USA). Primary tumors were excised 4–5 weeks after inoculation, at which point serial histological sections were prepared by the Tissue Procurement, Histology, & IHC Core (Case Comprehensive Cancer Center). Immunostaining was undertaken to monitor the expression of Ki-67 (1:50; BD Biosciences) as described [26]. The resulting images were captured on an Olympus BH2 microscope outfitted with Spot Advanced software (Diagnostic Instruments Inc., Sterling Heights, MI, USA). For pulmonary outgrowth studies, the aforementioned 4T1 derivatives were injected (5,000 cells/mouse) into the lateral tail vein of female Balb/C mice. Bioluminescence imaging was performed 30 min after inoculation (T0) and biweekly thereafter. Pulmonary tumor development was assessed by normalizing biweekly images to those obtained at T0.
Statistical analyses
Statistical values were defined using an unpaired 2-tailed Student’s t test, where a p value <0.05 was considered to be statistically significant.
Results
WAVE3 expression is upregulated by TGF-β in a manner that correlates with metastatic potential of TNBCs
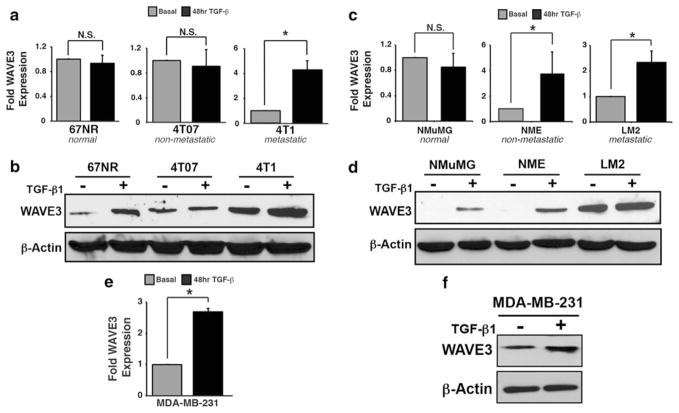
We [8, 9, 12] and others [27, 28] established that the expression and activity of WAVE3 promote carcinoma migration, invasion, and metastasis. Indeed, WAVE3 expression is upregulated dramatically in metastatic human breast cancer cell lines (e.g., MDA-MB-231 and BT-549) as compared to their nonmetastatic counterparts (e.g., MCF7, T47D, and SKBr3) [14]. Along these lines, aberrant WAVE3 expression is associated predominantly with aggressive TNBC subtypes [14]. The murine 4T1 progression series is an established model of TNBC development and metastatic progression and consists of isogenically derived nonmetastatic 67NR, systemically invasive 4T07, and highly metastatic 4T1 cells [29]. RNA profiling of these cell lines indicated that TGF-β significantly upregulated WAVE3 expression in metastatic 4T1 cells, while the same treatment condition elicited only modest upregulation of WAVE3 in the nonmetastatic 67NR and 4T07 cells (Fig. 1a). Similar patterns of WAVE3 protein expression were also observed in 4T1 derivatives stimulated with TGF-β (Fig. 1b). These results indicate that WAVE3 is upregulated by TGF-β in a manner that correlates with metastatic potential. To insure that this correlation was not limited solely to the 4T1 progression series, we also examined the coupling of TGF-β to WAVE3 expression in NMuMG cells, which are readily transformed by EGFR overexpression (termed NME cells [16, 30]), subsequently undergo metastatic progression in response to EMT stimulated by TGF-β, and are termed NME-LM2 cells (M.K. Wendt and W.P. Schiemann, unpublished observation). Similar to our findings obtained in the 4T1 progression series, we observed TGF-β stimulation to induce significant WAVE3 mRNA and protein expression in the transformed NME and NME-LM2 cells, but not in their normal NMuMG counterparts (Fig. 1c, d). Moreover, TGF-β also stimulated WAVE3 mRNA and protein expression in the human MDA-MB-231 cells, which represent an established model for human TNBC (Fig. 1e, f). Collectively, these results indicate that WAVE3 expression is highly upregulated by TGF-β in metastatic TNBC cells.
Fig. 1.
WAVE3 expression is upregulated by TGF-β in a manner that correlates with metastatic potential of TNBCs. Murine 4T1 (a, b) and NME (c, d) breast cancer progression series or human MDA-MB-231 breast cancer cells (e, f) were stimulated with TGF-β1 (5 ng/ml) for 48 h to induce an EMT program. WAVE3 transcript levels were measured by semi-quantitative real-time PCR and normalized to GAPDH (a, c, e), while WAVE3 protein levels were determined by immunoblotting (b, d, f). TGF-β1 treatment upregulated WAVE3 mRNA and protein expression in metastatic 4T1 cells, but not in their nonmetastatic 67NR and 4T07 counterparts (a, b). Similarly, TGF-β also upregulated WAVE3 mRNA and protein in transformed NME and LM2 cells, but not in normal NMuMG cells as measured by semi-quantitative real-time PCR (b, c). Finally, TGF-β induced the synthesis of WAVE3 transcripts and protein in metastatic MDA-MB-231 cells (e, f). All data are representative of at least three independent experiments or are the mean (±SE; n = 3; *p <0.05; Student’s t test)
TGF-β induces WAVE3 expression in a Smad2-and β3 integrin-dependent manner in TNBCs
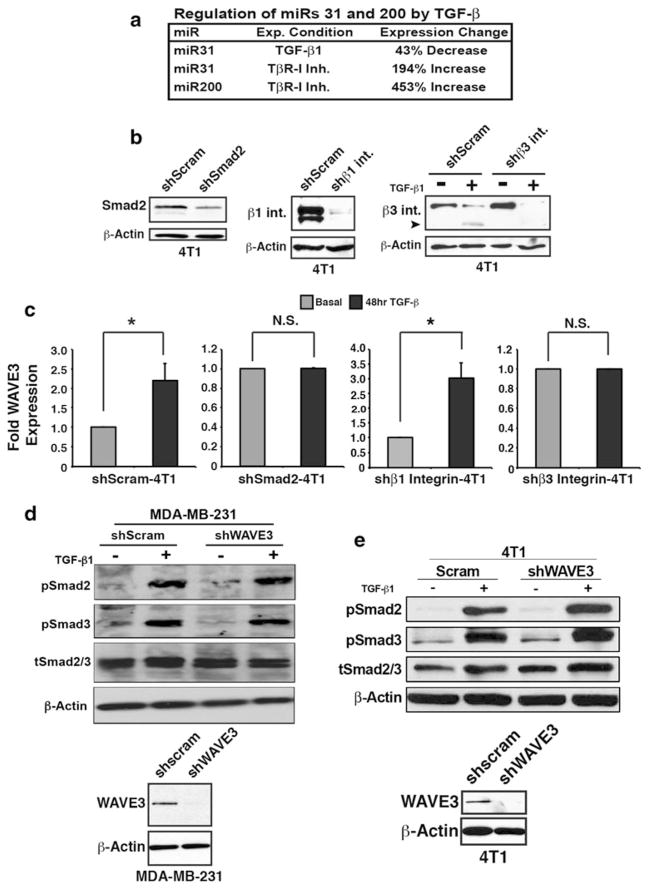
We previously demonstrated that expression of microR-NAs (miRs) 31 and 200 negatively regulates WAVE3 expression in human TNBCs [8, 31]. Along these lines, Fig. 2a shows that TGF-β negatively regulates the expression of these miRs in murine 4T1 cells [26], suggesting that the coupling of TGF-β to WAVE3 may proceed through altered miR-31 and miR-200 expression in TNBCs. Additionally, both canonical (e.g., Smad2/3) and noncanonical (e.g., β1 and β3 integrins, FAK, p38 MAPK, etc.) TGF-β signaling systems are essential in mediating TGF-β stimulation of EMT and metastasis (see [6, 15]). Moreover, β1 and β3 integrins can associate with the TGF-β type-II receptor and promote its activation of p38 MAPK signaling, leading to the induction of EMT programs [22, 32–34]. To further investigate the mechanisms through which TGF-β stimulates WAVE3 expression, we performed semi-quantitative real-time PCR analyses to monitor the synthesis of WAVE3 transcripts in 4T1 cells engineered to express diminished levels of either Smad2, β3 integrin, or β1 integrin (Fig. 2b). As shown in Fig. 2c, 4T1 cells depleted in the expression of either Smad2 or β3 integrin, but not of β1 integrin, and were unable to upregulate WAVE3 mRNA in response to TGF-β. Thus, TGF-β induces WAVE3 expression in part via a Smad2 (canonical) and β3 integrin (noncanonical)-dependent manner.
Fig. 2.
TGF-β induces WAVE3 expression in a Smad2- and β3 integrin-dependent manner in TNBCs. a Manipulating TGF-β signaling in 4T1 organotypic cultures negatively regulates miR-31 and miR-200 expression in metastatic TNBCs. b Knockdown of either Smad2 or β3 integrin, but not β1 integrin in 4T1 cells abrogated the induction of WAVE3 mRNA by TGF-β1 as measured by semi-quantitative real-time PCR, where mRNA signals were normalized to GAPDH (c). MDA-MB-231 (d) or 4T1 (e) cells rendered deficient in WAVE3 expression were stimulated with TGF-β1 (5 ng/ml) for 30 min, at which point the phosphorylation status of either Smad2 or Smad3 was monitored by immunoblot analysis as indicated. Differences in protein loading were determined by reprobing stripped membranes with antibodies against β-actin. All data are representative of three independent experiments or are the mean (±SE; n = 3; *p <0.05; Student’s t test)
We also investigated whether WAVE3 expression and activity were capable of reciprocally regulating those pathways governed by TGF-β. To do so, we measured the phosphorylation status of Smads 2 and 3 in parental (i.e., scrambled shRNA) and WAVE3-deficient human MDA-MB-231 (Fig. 2d) and murine 4T1 (Fig. 2e) cells. Figure 2c also shows that WAVE3 deficiency failed to affect the ability of TGF-β to stimulate the phosphorylation of either Smad2 or Smad3. Similarly, depleting WAVE3 expression in 4T1 cells had no effect on the coupling of TGF-β to the activation of Smad2/3 (Fig. 2e), indicating that WAVE3 deficiency does not alter TGF-β signaling through these cellular pathways. Taken together, these findings indicate that Smad2 and β3 integrin are required for TGF-β to induce WAVE3 expression in TNBCs.
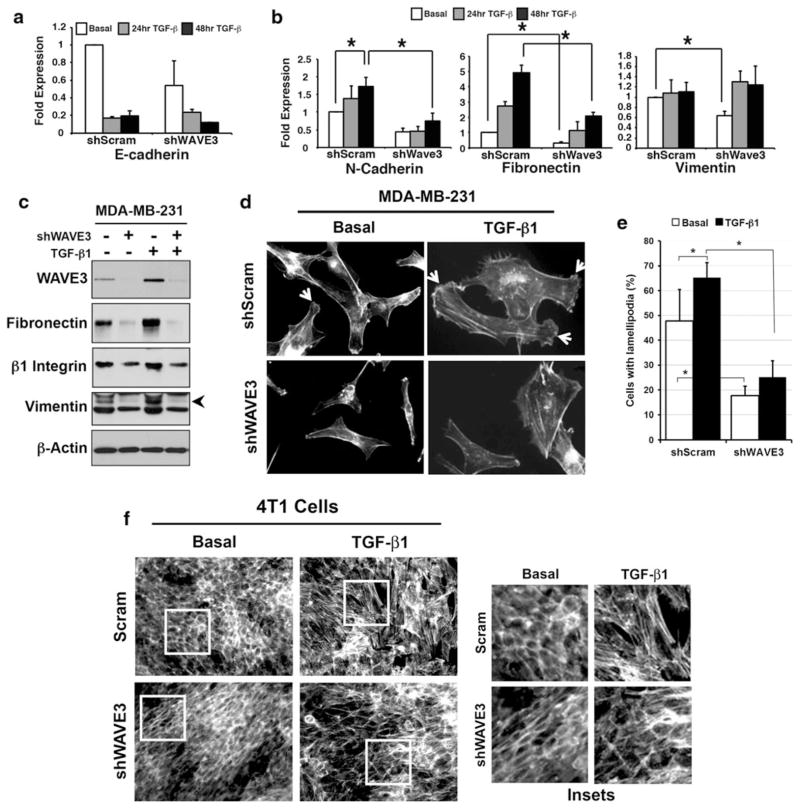
WAVE3 is required for TGF-β-mediated EMT in TNBCs
The ability of TGF-β to promote metastatic progression is strongly linked to its stimulation of EMT programs, whereby polarized MECs acquire a highly motile, apolar fibroblastoid-like phenotype [6]. EMT programs are accompanied by altered molecular profiles that reflect a loss of epithelial cell polarity and gain of mesenchymal morphologies that transpire via the upregulation of fibroblastoid markers (e.g., N-cadherin, fibronectin, and vimentin) [6]. Given the established role of WAVE3 in modulating the actin cytoskeleton [8, 9, 13], we examined the role of WAVE3 in modulating EMT programs stimulated by TGF-β. Although loss of WAVE3 expression failed to alter the loss of E-cadherin expression elicited by TGF-β (Fig. 3a), this same experimental condition prevented TGF-β from inducing the upregulated expression of the mesenchymal markers, N-cadherin, Fibronectin, and Vimentin, as measured by semi-quantitative real-time PCR (Fig. 3b). Additionally, WAVE3 deficiency also elicited a significant reduction in basal levels of vimentin expression in these same MDA-MB-231 derivatives (Fig. 3b). Along these lines, WAVE3 deficiency blocked TGF-β from stimulating fibronectin and vimentin protein expression, a cellular reaction that was not recapitulated for the pan epithelial and mesenchymal marker, β1 integrin (Fig. 3c). Consistent with these findings, WAVE3 deficiency altered the mesenchymal morphologies of metastatic MDA-MB-231 cells (Fig. 3d) and their formation of lamellipodia (Fig. 3e) both before and after their stimulation with TGF-β. Similarly, 4T1 cells treated with TGF-β readily transitioned from an epithelial morphology characterized by cortical actin staining to a mesenchymal morphology with abundant production of actin stress fibers (Fig. 3f). Importantly, depleting WAVE3 expression in these same cells stabilized their cortical actin staining patterns and attenuated their formation of actin stress fibers in response to TGF-β (Fig. 3f). Collectively, these findings indicate that WAVE3 is required for metastatic cells to upregulate the expression of mesenchymal markers required to initiate EMT programs in response to TGF-β.
Fig. 3.
WAVE3 is required for TGF-β-mediated EMT in TNBCs. a, b Control and WAVE3-deficient MDA-MB-231 cells were stimulated to undergo EMT by a 48-h treatment with TGF-β1 (5 ng/ml). Afterward, altered expression of E-cadherin, N-cadherin, fibronectin, or vimentin mRNA was determined by semi-quantitative real-time PCR. Individual transcript signals were normalized to GAPDH. c These same MDA-MB-231 derivatives were also prepared for immunoblot analyses to monitor the expression of fibronectin, vimentin, and β1 integrin as indicated. Differences in protein loading were controlled with anti-β-actin antibodies. d, e Control (i.e., shScram) and WAVE3-deficient MDA-MB-231 cells were seeded on gelatin-coated culture plates (1 μg/ml) and stimulated with TGF-β1 (5 ng/ml) for 48 h. Afterward, cells were fixed and stained for actin structures with Alexa Fluor 568-conjugated phalloidin (d). Arrowheads indicate the presence of lamellipodia membrane protrusions, while differences in lamellipodia formation are shown in panel e, which plots the % of cells with lamellipodia per field. All data are representative of three independent experiments (±SE; n = 3; *p <0.05; Student’s t test). f 4T1 cells were stimulated with TGF-β1 (5 ng/ml) to induce an EMT program. Boxed regions are shown as magnified insets on the right. All data are representative of three independent experiments or the mean (±SE; n = 3; *p <0.05; Student’s t test)
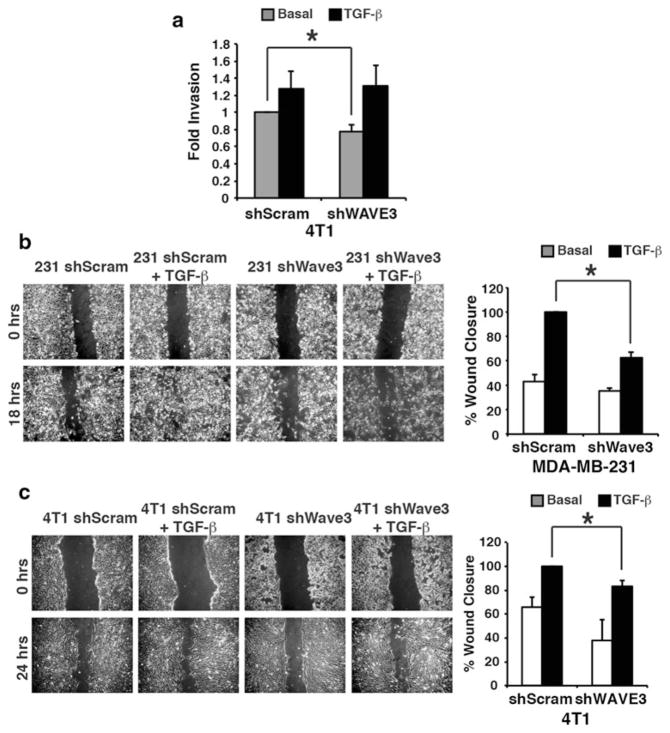
WAVE3 depletion dampens TNBC migration stimulated by TGF-β
A fundamental feature of EMT programs is their ability to promote carcinoma invasion and motility, which are essential processes in the metastatic cascade, which enable breast cancer cells to escape the confines of the primary tumor. Numerous studies have implicated WAVE3 as a crucial component of tumor cell invasion [10–12], a cellular response that has also been attributed to TGF-β in promoting the invasion of 4T1 and MDA-MB-231 cells [35, 36]. Functionally, although decreased WAVE3 expression diminished basal levels of invasion, as has been previously observed [12], depletion of WAVE3 failed to antagonize the ability of TGF-β to induce the invasion of these TNBC cells (Fig. 4a). However, rendering either MDA-MB-231 or 4T1 metastatic cells deficient in WAVE3 significantly reduced their ability to initiate cell migration in response to TGF-β (Fig. 4b, c). Collectively, these findings indicate that WAVE3 is required for cell migration stimulated by TGF-β.
Fig. 4.
WAVE3 depletion abrogates TNBCs’ migration stimulated by TGF-β. a Basal levels of 4T1 cell invasion through a synthetic basic membrane were reduced by inactivation of WAVE3 function, while TGF-β1 (5 ng/ml) stimulation of invasion remained unaffected. Control and WAVE3-deficient MDA-MB-231 (b) or 4T1 (c) cells were induced to migrate into denuded wounds over a 24-h period in the absence or presence of TGF-β1 (5 ng/ml). All data are representative of three independent experiments or are the mean (±SE; n = 3; *p <0.05; Student’s t test)
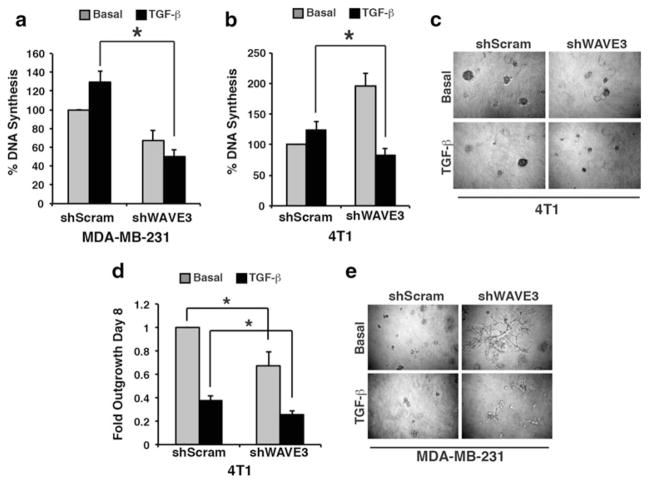
WAVE3 depletion decreases TGF-β-mediated proliferation and 3D outgrowth of TNBCs
Based on the requirement of WAVE3 expression for TGF-β-mediated EMT and migration, we next sought to determine whether WAVE3 expression couples TGF-β to the regulation of MEC proliferation and 3D organotypic outgrowth. In doing so, we initially measured effects of WAVE3 depletion on the rate of DNA synthesis regulated by TGF-β. As expected, TGF-β induced the proliferation of control MDA-MB-231 and 4T1 cells (Fig. 5a, b) [22, 37]. However, when these same cells were rendered deficient in WAVE3 expression, the coupling of TGF-β to cytostasis was restored and led to a dramatic decrease in TGF-β-mediated proliferation (Fig. 5a, b). We also measured differences in the growth of breast cancer organoids formed by these same cells in 3D organotypic cultures, which more closely recapitulate the elastic modulus of the lung microenvironment and mimic metastatic outgrowth in the pulmonary microenvironment [19, 38–40]. We recently demonstrated that TGF-β functions to suppress the growth of late-stage TNBC organoids in compliant 3D organotypic cultures, but to promote their growth when stimulated by TGF-β in rigid 3D organotypic cultures [24, 26, 41]. Interestingly, WAVE3 deficiency significantly repressed the basal growth rates of TNBC organoids in compliant 3D organotypic cultures, a cytostatic event that was further enhanced by inclusion of TGF-β (Fig. 5c, d). Along these lines, WAVE3 deficiency in MDA-MB-231 cells enhanced their formation of branched organoids, a morphology we previously associated with mammary gland differentiation and metastatic dormancy (Fig. 5e) [16, 19]. Collectively, these findings indicate that WAVE3 not only regulates the coupling of TGF-β to EMT programs but may also play a novel role in modulating cell cycle progression in response to TGF-β. Moreover, these findings suggest that WAVE3 deficiency enhances the cytostatic activities of TGF-β, which may serve to prevent the metastatic outgrowth of disseminated TNBC cells.
Fig. 5.
WAVE3 depletion decreases TGF-β-mediated proliferation and 3D outgrowth of TNBCs. The proliferation of control (shScram) or WAVE3-deficient (shWAVE3) expressing MDA-MB-231 (a) or 4T1 (b) cells in response to TGF-β1 (5 ng/ml) as quantitated by a [3H]thymidine incorporation assay. The anti-proliferative activity of TGF-β1 (5 ng/ml) in 4T1 (c, d) and MDA-MB-231 (e) organoids was enhanced by WAVE3 inactivation. The outgrowth of 4T1 organoids in compliant 3D organotypic cultures was quantified by measuring bioluminescent signals 8 days after plating. All data are representative of three independent experiments or are the mean (±SE; n = 3; *p <0.05; Student’s t test)
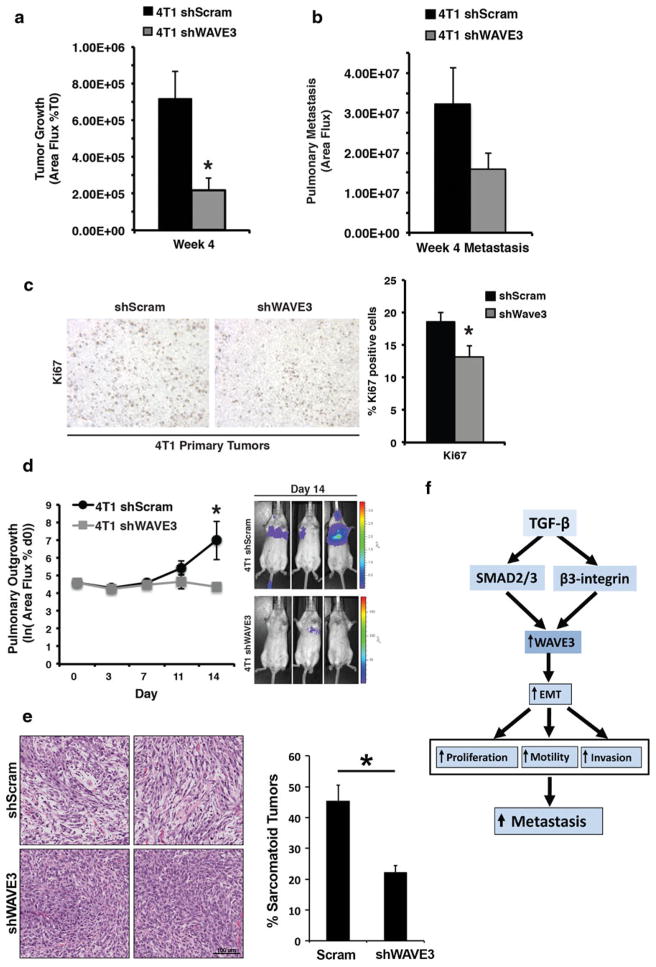
WAVE3 deficiency decreases the growth and metastasis of TNBC tumors in mice
To investigate the role of WAVE3 in TGF-β-mediated tumor growth and metastasis, we orthotopically injected 4T1 cells, which are subject to high levels of autocrine TGF-β signaling [24, 37, 42, 43], into the mammary fat pads of syngeneic Balb/C mice. In this context, WAVE3 deficiency resulted in a significant reduction in primary 4T1 tumor growth and subsequent metastatic dissemination (Fig. 6a, b). In accordance with our demonstration that WAVE3 deficiency elicited an anti-proliferative response in 4T1 cells (Fig. 5), we also observed WAVE3-deficient 4T1 tumors to exhibit significantly lower proliferation indices as compared to their WAVE3-expressing counterparts (Fig. 6c). To further test the supposition that WAVE3 deficiency decreases metastatic outgrowth, we inoculated the same 4T1 derivatives into the lateral tail veins of 4-week-old female Balb/C mice. Initial carcinoma cell seeding and subsequent pulmonary outgrowth of 4T1 cells were subsequently monitored by biweekly bioluminescent imaging. Figure 6d shows that the loss of WAVE3 expression significantly decreased pulmonary tumor burden elicited by 4T1 cells. Importantly, and consistent with our findings that WAVE3 participates in EMT and metastasis stimulated by TGF-β, we found WAVE3 deficiency to significantly reduce the appearance of sarcomatoid morphologies and EMT phenotypes in pulmonary 4T1 tumors (Fig. 6e). Collectively, these findings indicate that WAVE3 enhances the growth and metastatic progression of late-stage TNBC tumors, suggesting that the expression and activity of WAVE3 are an important component of oncogenic TGF-β signaling and its stimulation of breast cancer progression (Fig. 6f).
Fig. 6.
WAVE3 deficiency decreases the growth and metastasis of TNBC tumors in mice. Primary tumor growth (a) and metastasis (b) of control and WAVE3-deficient 4T1 cells engineered to stably express firefly luciferase (Luc) were determined following their engraftment into the mammary fat pads of Balb/C mice (n = 5). c Depletion of WAVE3 inhibits the proliferative capacity of primary 4T1 tumors as measured by Ki67 staining, which was quantified using ImageJ. d These same 4T1 derivatives were also injected into the lateral tail vein for Balb/C mice, whose development of pulmonary tumors was measured by bioluminescence longitudinally every 3 days post-injection (top). Representative bioluminescent signals of pulmonary tumor formation 14 days post-injection are also shown (bottom). Following necropsy, the lungs were stained with H&E and the frequency of sarcomatoid phenotypes in these tissue samples was determined (e). (f) TGF-β upregulation of WAVE3 involves both the canonical (Smad2) and noncanonical (β3 integrin) signaling pathways, leading to the initiation of EMT programs that enhance TNBC cell proliferation, migration, and invasion, which culminates in driving the metastatic dissemination of TNBCs
Discussion
Breast cancer is the second most common cause of cancer death in women in the United States, and of these deaths, ~90 % are due to metastasis. As such, a better understanding of the molecular mechanisms that elicit breast cancer metastasis is necessary for the development of new targeted therapies to improve the clinical course of patients with metastatic disease. It is well known that pathological characteristics, such as positive lymph node status and histological grade, readily contribute to increased risk for metastasis. Moreover, breast cancer can be subcategorized into at least 5 genetically distinct subtypes [1] and perhaps as many as 10 distinct subtypes [44] based on their hormone receptor status (ER-α and PR), amplification of ErbB2/HER2, and distinct genomic landscapes. Interestingly, TNBCs lack expression of ER-α, PR, and HER2, which has significantly impeded the development of targeted therapies against this aggressive breast cancer subtype [45]. Along these line, TNBCs also appear to represent a heterogeneous group that may comprise as many as 6 unique subtypes [46], all of which are highly metastatic and often become resistant to standard-of-care chemotherapeutic agents [45]. The promotion of EMT programs by TGF-β represents an established mechanism capable of driving TNBC metastasis [6]. More recently, elevated expression of WAVE3 in TNBC cell lines has been shown to directly contribute to the increased invasion and metastasis of these cells [14]. In the current study, we observed WAVE3 expression to be induced by TGF-β in both human and mouse TNBC cells, a response to TGF-β that correlated with the metastatic phenotype of these mammary carcinoma cells. These initial observations, coupled with the knowledge that WAVE3 is an established promoter of breast cancer metastasis [14], implicated WAVE3 as a potential mediator of oncogenic TGF-β signaling in TNBCs, thereby providing the impetus to explore the function of WAVE3 during mammary tumorigenesis regulated by TGF-β. As such, the major findings of our study show that (i) the coupling of TGF-β to WAVE3 expression involves both canonical (i.e., Smad2) and non-canonical (i.e., β3 integrin) signaling inputs (Fig. 2); (ii) WAVE3 expression and activity are required for the initiation of EMT programs stimulated by TGF-β (Fig. 3); (iii) WAVE3 deficiency reduced the coupling of TGF-β to cell proliferation and migration, and to TNBC organoid growth in 3D organotypic cultures (Fig. 4, 5); and (iv) loss of WAVE3 function decreased the ability of TGF-β to induce the growth and metastasis of TNBC tumors in mice (Fig. 6). Collectively, our findings have established WAVE3 as a novel effector molecule in the oncogenic TGF-β signaling system and have demonstrated the necessity for WAVE3 during EMT and metastasis programs stimulated by TGF-β.
An intriguing and unexpected finding of the current study was the clear linkage of WAVE3 expression to the regulation of proliferative programs. Precisely how the modulation of the actin cytoskeleton by WAVE3 impacts cell cycle progression remains unknown; however, recent studies do suggest an important role for actin polymerization in regulating cellular pathways and signaling systems coupled to transcriptional and proliferative programs [47, 48]. Interestingly, whereas depletion of WAVE3 failed to significantly alter basal rates of DNA synthesis, this cellular condition did significantly enhance the anti-proliferative activities of TGF-β (Fig. 5a, b). The selectivity of this response suggests that WAVE3 may play a novel and critical role in mediating the switch in TGF-β function from that of a cell cycle suppressor to a promoter of cell cycle progression. In support of this supposition, we recently established that WAVE3 functions to sensitize cancer cells to apoptosis driven by TNF-α (G. Davuluri and K. Sossey-Alaoui, unpublished observation).
Mammary tumor microenvironments play an essential role in governing the growth, metastasis, and chemosensitivity of tumors. Integrins are heterodimeric transmembrane receptors that physically link the extracellular matrix to the actin cytoskeleton, thereby transducing microenvironmental signals into altered gene expression profiles and cell behaviors. Moreover, altered integrin expression profiles are associated with the metastatic progression of breast cancers, including that driven by TGF-β [22, 34, 49]. Mechanistically, oncogenic TGF-β signaling is initiated by the physical interaction of TβR-II with β1 and β3 integrins, which leads to the phosphorylation and activation of FAK, which elicit the recruitment of Src and p130Cas and downstream activation of Rac1, which ultimately enhance the motility and migration of late-stage breast cancers [22, 32–34, 49]. Interestingly, Rac1 can modulate the activity of WAVE3 and promote migratory phenotypes’ carcinoma cells [7]. Upregulation of β1 integrin expression in breast cancer cells has been shown to enhance metastasis, leading to the supposition that β1 integrin-targeted therapies may prove to be effective in reducing metastasis [34, 39, 40]. However, inactivating β1 integrin function elicits a compensatory upregulation of β3 integrin expression that is sufficient to restore the metastatic behavior of late-stage breast cancers (J.G. Parvani and W.P. Schiemann, unpublished observation). Along these lines, upregulated β3 integrin expression is associated with the acquisition of EMT, cancer stem cell-like, and metastatic phenotypes in breast cancers [50]. Accordingly, we established that the simultaneous stimulation of αvβ3 integrin and TGF-β receptors was essential in promoting EMT and invasive phenotypes in normal and malignant MECs, and in stimulating the metastatic progression of TNBCs [22, 32, 33]. Importantly, targeted inactivation of β3 integrin expression abrogates the coupling of TGF-β to breast cancer EMT and pulmonary metastasis [22, 32, 33]. Likewise, we show here that targeted inactivation of β3 integrin, but not that of β1 integrin, also abrogates the expression of WAVE3 in response to TGF-β, thereby implicating WAVE3 as an essential component operant in linking β3 integrin to the oncogenic activities of TGF-β in TNBCs.
In summary, the findings presented herein show that TGF-β strongly induces WAVE3 expression in late-stage human and murine TNBC cells, and that this event correlates with the functional conversion of TGF-β from a suppressor to a promoter of TNBC development and metastatic progression. Collectively, our study implicates upregulated WAVE3 expression as a potential biomarker for TNBC metastasis driven by TGF-β, and shows that therapeutic targeting of WAVE3 may provide an innovative method for selectively restoring the cytostatic activities of TGF-β in late-stage TNBCs.
Acknowledgments
Members of the Sossey-Alaoui and Schiemann laboratories are thanked for critical comments and reading of the manuscript. The expertise and guidance provided by the Athymic Animal and Xenograft Core, the Imaging Research Core, and the Tissue Procurement, Histology, and IHC core of the Case Comprehensive Cancer Center are also gratefully acknowledged. Research support was provided in part by the National Institutes of Health to W.P.S. (CA129359) and E.F.P. (HL073311 and HL HL096062), and by the Department of Defense to K.S.-A. (BC073783) and to M.A.T. (BC093128). Additional support was provided to W.P.S. and K.S.-A. by pilot funds from the Case Comprehensive Cancer Center (P30 CA043703).
Abbreviations
- 3D
3-Dimensional
- EMT
Epithelial–mesenchymal transition
- ER-α
Estrogen receptor-α
- IHC
Immunohistochemistry
- MEC
Mammary epithelial cell
- PR
Progesterone receptor
- TGF-β
Transforming growth factor-β
- TNBC
Triple-negative breast cancer
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
Contributor Information
Molly A. Taylor, Case Comprehensive Cancer Center, Case Western Reserve University, Wolstein Research Building, 2103 Cornell Road, Cleveland, OH 44106, USA
Gangarao Davuluri, Department of Molecular Cardiology, Lerner Research Institute, Cleveland Clinic, Cleveland, OH 44106, USA.
Jenny G. Parvani, Department of Pathology, Case Western Reserve University, Cleveland, OH 44106, USA
Barbara J. Schiemann, Case Comprehensive Cancer Center, Case Western Reserve University, Wolstein Research Building, 2103 Cornell Road, Cleveland, OH 44106, USA
Michael K. Wendt, Case Comprehensive Cancer Center, Case Western Reserve University, Wolstein Research Building, 2103 Cornell Road, Cleveland, OH 44106, USA
Edward F. Plow, Department of Molecular Cardiology, Lerner Research Institute, Cleveland Clinic, Cleveland, OH 44106, USA
William P. Schiemann, Email: wps20@case.edu, Case Comprehensive Cancer Center, Case Western Reserve University, Wolstein Research Building, 2103 Cornell Road, Cleveland, OH 44106, USA
Khalid Sossey-Alaoui, Email: sosseyk@ccf.org, Department of Molecular Cardiology, Lerner Research Institute, Cleveland Clinic, Cleveland, OH 44106, USA, Department of Molecular Cardiology, Lerner Research Institute, Cleveland Clinic, 9500 Euclid Ave., NB-50, Cleveland, OH 44195, USA.
References
- 1.Perou CM, Sorlie T, Eisen MB, van de Rijn M, Jeffrey SS, Rees CA, Pollack JR, Ross DT, Johnsen H, Akslen LA, Fluge O, Pergamenschikov A, Williams C, Zhu SX, Lonning PE, Borresen-Dale AL, Brown PO, Botstein D. Molecular portraits of human breast tumours. Nature. 2000;406(6797):747–752. doi: 10.1038/35021093. [DOI] [PubMed] [Google Scholar]
- 2.Carey L, Winer E, Viale G, Cameron D, Gianni L. Triple-negative breast cancer: disease entity or title of convenience? Nat Rev Clin Oncol. 2010;7(12):683–692. doi: 10.1038/nrclinonc.2010.154. [DOI] [PubMed] [Google Scholar]
- 3.Carey LA. Directed therapy of subtypes of triple-negative breast cancer. Oncologist. 2010;15(Suppl 5):49–56. doi: 10.1634/theoncologist.2010-S5-49. [DOI] [PubMed] [Google Scholar]
- 4.Siegel R, Naishadham D, Jemal CA. Cancer statistics. CA Cancer J Clin. 2012;62(1):10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 5.Valastyan S, Weinberg RA. Tumor metastasis: molecular insights and evolving paradigms. Cell. 2011;147(2):275–292. doi: 10.1016/j.cell.2011.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taylor MA, Parvani JG, Schiemann WP. The pathophysiology of epithelial-mesenchymal transition induced by transforming growth factor-β in normal and malignant mammary epithelial cells. J Mammary Gland Biol Neoplasia. 2010;15(2):169–190. doi: 10.1007/s10911-010-9181-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sossey-Alaoui K. Surfing the big WAVE: insights into the role of WAVE3 as a driving force in cancer progression and metastasis. Semin Cell Dev Biol. 2013;24:287–297. doi: 10.1016/j.semcdb.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sossey-Alaoui K, Downs-Kelly E, Das M, Izem L, Tubbs R, Plow EF. WAVE3, an actin remodeling protein, is regulated by the metastasis suppressor microRNA, miR-31, during the invasion-metastasis cascade. Int J Cancer. 2011;129(6):1331–1343. doi: 10.1002/ijc.25793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sossey-Alaoui K, Li X, Cowell JK. c-Abl-mediated phosphorylation of WAVE3 is required for lamellipodia formation and cell migration. J Biol Chem. 2007;282(36):26257–26265. doi: 10.1074/jbc.M701484200. [DOI] [PubMed] [Google Scholar]
- 10.Sossey-Alaoui K, Li X, Ranalli TA, Cowell JK. WAVE3-mediated cell migration and lamellipodia formation are regulated downstream of phosphatidylinositol 3-kinase. J Biol Chem. 2005;280(23):21748–21755. doi: 10.1074/jbc.M500503200. [DOI] [PubMed] [Google Scholar]
- 11.Sossey-Alaoui K, Ranalli TA, Li X, Bakin AV, Cowell JK. WAVE3 promotes cell motility and invasion through the regulation of MMP-1, MMP-3, and MMP-9 expression. Exp Cell Res. 2005;308(1):135–145. doi: 10.1016/j.yexcr.2005.04.011. [DOI] [PubMed] [Google Scholar]
- 12.Sossey-Alaoui K, Safina A, Li X, Vaughan MM, Hicks DG, Bakin AV, Cowell JK. Down-regulation of WAVE3, a metastasis promoter gene, inhibits invasion and metastasis of breast cancer cells. Am J Pathol. 2007;170(6):2112–2121. doi: 10.2353/ajpath.2007.060975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Takenawa T, Miki H. WASP and WAVE family proteins: key molecules for rapid rearrangement of cortical actin filaments and cell movement. J Cell Sci. 2001;114(Pt 10):1801–1809. doi: 10.1242/jcs.114.10.1801. [DOI] [PubMed] [Google Scholar]
- 14.Kulkarni S, Augoff K, Rivera L, McCue B, Khoury T, Groman A, Zhang L, Tian L, Sossey-Alaoui K. Increased expression levels of WAVE3 are associated with the progression and metastasis of triple negative breast cancer. PLoS ONE. 2012;7(8):e42895. doi: 10.1371/journal.pone.0042895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parvani JG, Taylor MA, Schiemann WP. Noncanonical TGF-β signaling during mammary tumorigenesis. J Mammary Gland Biol Neoplasia. 2011;16(2):127–146. doi: 10.1007/s10911-011-9207-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wendt MK, Smith JA, Schiemann WP. Transforming growth factor-β-induced epithelial-mesenchymal transition facilitates epidermal growth factor-dependent breast cancer progression. Oncogene. 2010;29(49):6485–6498. doi: 10.1038/onc.2010.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wendt MK, Smith JA, Schiemann WP. p130Cas is required for mammary tumor growth and TGF-β-mediated metastasis through regulation of Smad2/3 activity. J Biol Chem. 2009;284(49):31145–31156. doi: 10.1074/jbc.M109.023614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wendt MK, Cooper AN, Dwinell MB. Epigenetic silencing of CXCL12 increases the metastatic potential of mammary carcinoma cells. Oncogene. 2008;27(10):1461–1471. doi: 10.1038/sj.onc.1210751. [DOI] [PubMed] [Google Scholar]
- 19.Wendt MK, Taylor MA, Schiemann BJ, Schiemann WP. Down-regulation of epithelial cadherin is required to initiate metastatic outgrowth of breast cancer. Mol Biol Cell. 2011;22(14):2423–2435. doi: 10.1091/mbc.E11-04-0306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wendt MK, Schiemann WP. Therapeutic targeting of the focal adhesion complex prevents oncogenic TGF-β signaling and metastasis. Breast Cancer Res. 2009;11(5):R68. doi: 10.1186/bcr2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schiemann WP, Blobe GC, Kalume DE, Pandey A, Lodish HF. Context-specific effects of fibulin-5 (DANCE/EVEC) on cell proliferation, motility, and invasion. Fibulin-5 is induced by transforming growth factor-β and affects protein kinase cascades. J Biol Chem. 2002;277(30):27367–27377. doi: 10.1074/jbc.M200148200. [DOI] [PubMed] [Google Scholar]
- 22.Galliher AJ, Schiemann WP. β3 integrin and Src facilitate transforming growth factor-β mediated induction of epithelial-mesenchymal transition in mammary epithelial cells. Breast Cancer Res. 2006;8(4):R42. doi: 10.1186/bcr1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee GY, Kenny PA, Lee EH, Bissell MJ. Three-dimensional culture models of normal and malignant breast epithelial cells. Nat Methods. 2007;4(4):359–365. doi: 10.1038/nmeth1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taylor MA, Amin JD, Kirschmann DA, Schiemann WP. Lysyl oxidase contributes to mechanotransduction-mediated regulation of transforming growth factor-β signaling in breast cancer cells. Neoplasia. 2011;13(5):406–418. doi: 10.1593/neo.101086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schiemann WP, Pfeifer WM, Levi E, Kadin ME, Lodish HF. A deletion in the gene for transforming growth factor β type I receptor abolishes growth regulation by transforming growth factor β in a cutaneous T-cell lymphoma. Blood. 1999;94(8):2854–2861. [PubMed] [Google Scholar]
- 26.Taylor MA, Sossey-Alaoui K, Thompson CL, Danielpour D, Schiemann WP. TGF-β upregulates miR-181a expression to promote breast cancer metastasis. J Clin Invest. 2013;123(1):150–163. doi: 10.1172/JCI64946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ghoshal P, Teng Y, Lesoon LA, Cowell JK. HIF1A induces expression of the WASF3 metastasis-associated gene under hypoxic conditions. Int J Cancer. 2012;131(6):E905–E915. doi: 10.1002/ijc.27631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fernando HS, Sanders AJ, Kynaston HG, Jiang WG. WAVE3 is associated with invasiveness in prostate cancer cells. Urol Oncol. 2010;28(3):320–327. doi: 10.1016/j.urolonc.2008.12.022. [DOI] [PubMed] [Google Scholar]
- 29.Aslakson CJ, Miller FR. Selective events in the metastatic process defined by analysis of the sequential dissemination of subpopulations of a mouse mammary tumor. Cancer Res. 1992;52(6):1399–1405. [PubMed] [Google Scholar]
- 30.Wendt MK, Schiemann BJ, Parvani JG, Lee YH, Kang Y, Schiemann WP. TGF-β stimulates Pyk2 expression as part of an epithelial-mesenchymal transition program required for metastatic outgrowth of breast cancer. Oncogene. 2013;32(16):2005–2015. doi: 10.1038/onc.2012.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sossey-Alaoui K, Bialkowska K, Plow EF. The miR200 family of microRNAs regulates WAVE3-dependent cancer cell invasion. J Biol Chem. 2009;284(48):33019–33029. doi: 10.1074/jbc.M109.034553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Galliher AJ, Schiemann WP. Src phosphorylates Tyr284 in TGF-β type II receptor and regulates TGF-β stimulation of p38 MAPK during breast cancer cell proliferation and invasion. Cancer Res. 2007;67(8):3752–3758. doi: 10.1158/0008-5472.CAN-06-3851. [DOI] [PubMed] [Google Scholar]
- 33.Galliher-Beckley AJ, Schiemann WP. Grb2 binding to Tyr284 in TβR-II is essential for mammary tumor growth and metastasis stimulated by TGF-beta. Carcinogenesis. 2008;29(2):244–251. doi: 10.1093/carcin/bgm245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bhowmick NA, Zent R, Ghiassi M, McDonnell M, Moses HL. Integrin β1 signaling is necessary for transforming growth factor-β activation of p38MAPK and epithelial plasticity. J Biol Chem. 2001;276(50):46707–46713. doi: 10.1074/jbc.M106176200. [DOI] [PubMed] [Google Scholar]
- 35.Farina AR, Coppa A, Tiberio A, Tacconelli A, Turco A, Colletta G, Gulino A, Mackay AR. Transforming growth factor-β1 enhances the invasiveness of human MDA-MB-231 breast cancer cells by up-regulating urokinase activity. Int J Cancer. 1998;75(5):721–730. doi: 10.1002/(sici)1097-0215(19980302)75:5<721::aid-ijc10>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 36.McEarchern JA, Kobie JJ, Mack V, Wu RS, Meade-Tollin L, Arteaga CL, Dumont N, Besselsen D, Seftor E, Hendrix MJ, Katsanis E, Akporiaye ET. Invasion and metastasis of a mammary tumor involves TGF-β signaling. Int J Cancer. 2001;91(1):76–82. doi: 10.1002/1097-0215(20010101)91:1<76::aid-ijc1012>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 37.Neil JR, Schiemann WP. Altered TAB 1:IκB kinase interaction promotes transforming growth factor β-mediated nuclear factor-κB activation during breast cancer progression. Cancer Res. 2008;68(5):1462–1470. doi: 10.1158/0008-5472.CAN-07-3094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barkan D, Kleinman H, Simmons JL, Asmussen H, Kamaraju AK, Hoenorhoff MJ, Liu ZY, Costes SV, Cho EH, Lockett S, Khanna C, Chambers AF, Green JE. Inhibition of metastatic outgrowth from single dormant tumor cells by targeting the cytoskeleton. Cancer Res. 2008;68(15):6241–6250. doi: 10.1158/0008-5472.CAN-07-6849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barkan D, El Touny LH, Michalowski AM, Smith JA, Chu I, Davis AS, Webster JD, Hoover S, Simpson RM, Gauldie J, Green JE. Metastatic growth from dormant cells induced by a Col-I-enriched fibrotic environment. Cancer Res. 2010;70(14):5706–5716. doi: 10.1158/0008-5472.CAN-09-2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shibue T, Weinberg RA. Integrin β1-focal adhesion kinase signaling directs the proliferation of metastatic cancer cells disseminated in the lungs. Proc Natl Acad Sci USA. 2009;106(25):10290–10295. doi: 10.1073/pnas.0904227106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Allington TM, Galliher-Beckley AJ, Schiemann WP. Activated Abl kinase inhibits oncogenic transforming growth factor-β signaling and tumorigenesis in mammary tumors. FASEB J. 2009;23(12):4231–4243. doi: 10.1096/fj.09-138412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hoshino Y, Katsuno Y, Ehata S, Miyazono K. Autocrine TGF-β protects breast cancer cells from apoptosis through reduction of BH3-only protein, Bim. J Biochem. 2011;149(1):55–65. doi: 10.1093/jb/mvq114. [DOI] [PubMed] [Google Scholar]
- 43.Neil JR, Tian M, Schiemann WP. X-linked inhibitor of apoptosis protein and its E3 ligase activity promote transforming growth factor-β-mediated nuclear factor-κB activation during breast cancer progression. J Biol Chem. 2009;284(32):21209–21217. doi: 10.1074/jbc.M109.018374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Curtis C, Shah SP, Chin SF, Turashvili G, Rueda OM, Dunning MJ, Speed D, Lynch AG, Samarajiwa S, Yuan Y, Graf S, Ha G, Haffari G, Bashashati A, Russell R, McKinney S, Group M, Langerod A, Green A, Provenzano E, Wishart G, Pinder S, Watson P, Markowetz F, Murphy L, Ellis I, Purushotham A, Borresen-Dale AL, Brenton JD, Tavare S, Caldas C, Aparicio S. The genomic and transcriptomic architecture of 2,000 breast tumours reveals novel subgroups. Nature. 2012;486(7403):346–352. doi: 10.1038/nature10983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schneider BP, Winer EP, Foulkes WD, Garber J, Perou CM, Richardson A, Sledge GW, Carey LA. Triple-negative breast cancer: risk factors to potential targets. Clin Cancer Res. 2008;14(24):8010–8018. doi: 10.1158/1078-0432.CCR-08-1208. [DOI] [PubMed] [Google Scholar]
- 46.Lehmann BD, Bauer JA, Chen X, Sanders ME, Chakravarthy AB, Shyr Y, Pietenpol JA. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J Clin Invest. 2011;121(7):2750–2767. doi: 10.1172/JCI45014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zipfel PA, Bunnell SC, Witherow DS, Gu JJ, Chislock EM, Ring C, Pendergast AM. Role for the Abi/wave protein complex in T cell receptor-mediated proliferation and cytoskeletal remodeling. Curr Biol. 2006;16(1):35–46. doi: 10.1016/j.cub.2005.12.024. [DOI] [PubMed] [Google Scholar]
- 48.Wang R, Mercaitis OP, Jia L, Panettieri RA, Tang DD. Raf-1, actin dynamics and Abl in human airway smooth muscle cells. Am J Respir Cell Mol Biol. 2012;48(2):172–180. doi: 10.1165/rcmb.2012-0315OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lahlou H, Muller WJ. β1-integrins signaling and mammary tumor progression in transgenic mouse models: implications for human breast cancer. Breast Cancer Res. 2011;13(6):229. doi: 10.1186/bcr2905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lindeman GJ, Visvader JE. Insights into the cell of origin in breast cancer and breast cancer stem cells. Asia Pac J Clin Oncol. 2010;6(2):89–97. doi: 10.1111/j.1743-7563.2010.01279.x. [DOI] [PubMed] [Google Scholar]