Abstract
Background
Sun exposure, especially during childhood, is the most important preventable risk factor for skin cancer, yet few effective interventions to reduce exposure exist.
Purpose
To test the effectiveness of a partially tailored mailed intervention based on the Precaution Adoption Process Model, delivered in the spring over 3 years to parents and children.
Design
RCT, with data collection through telephone interviews of parents and skin exams of children at baseline (Summer 2004) and annually (Summer 2005–2007). The control group received no intervention.
Setting/participants
Families recruited in the Denver CO area, through private pediatric clinics, a large MCO, and community settings. Children born in 1998 were aged approximately 6 years at baseline; 867 children met inclusion criteria; analysis is reported for 677 white, non-Hispanic participants at highest risk for skin cancer.
Main outcome measures
Primary outcomes were parent-reported child sun protection behaviors. Secondary outcomes included parents' risk perception, and perceived effectiveness of and barriers to prevention behaviors, stage of change, reported sunburns, and observed tanning and nevus development. The longitudinal mixed-model analysis was conducted between 2008 and 2011.
Results
The intervention group reported more use of protective clothing and hats, shadeseeking, sunscreen and midday sun avoidance; fewer sunburns; more knowledge of the risk of skin cancer; higher perceived effectiveness of sun protection and stage of change; and lower perception of barriers to sun protection (all p<0.05). The intervention group had fewer nevi ≥2 mm in 1 year of the study, 2006 (p=0.03). No differences were found in tanning or nevi <2 mm.
Conclusions
The level of behavior change associated with this single-modality intervention is not likely sufficient to reduce skin cancer risk. However, the intervention shows promise for inclusion in longer-term, multicomponent interventions that have sufficient intensity to affect skin cancer incidence.
Trial registration
This study is registered at www.clinicaltrials.gov NCT01464957.
Introduction
Skin cancer incidence is increasing dramatically and is largely caused by sun exposure.1–3 Exposure in childhood is particularly important for risk.4,5 Prevention efforts have focused on minimizing ultraviolet (UV) exposure through a combination of avoiding the midday sun, wearing clothing and hats, seeking shade, and using sunscreen. Although studies show widespread sunscreen use, the use of other sun protection strategies has lagged.6 Interventions are particularly needed to promote the use of hats and clothing, which a recent study showed may be more effective than sunscreen in reducing skin cancer risk.7
Interventions in single settings have been effective for improving the UV protection of children, including: school-based programs;8–16 programs at swimming pools and zoos;17–19 programs in pediatric care settings;20–22 and multimedia computer programs.23,24 The most-successful interventions for changing sun protection behaviors of parents and children have been community-wide, multicomponent approaches.25,26 However, research is needed to inform evidence-based decision-making about effective components for comprehensive interventions, particularly for children approaching adolescence, when their responsibility for preventive behaviors increases. Effective interventions are needed that promote behavior change to both parents and children and encourage family communication about sun protection.
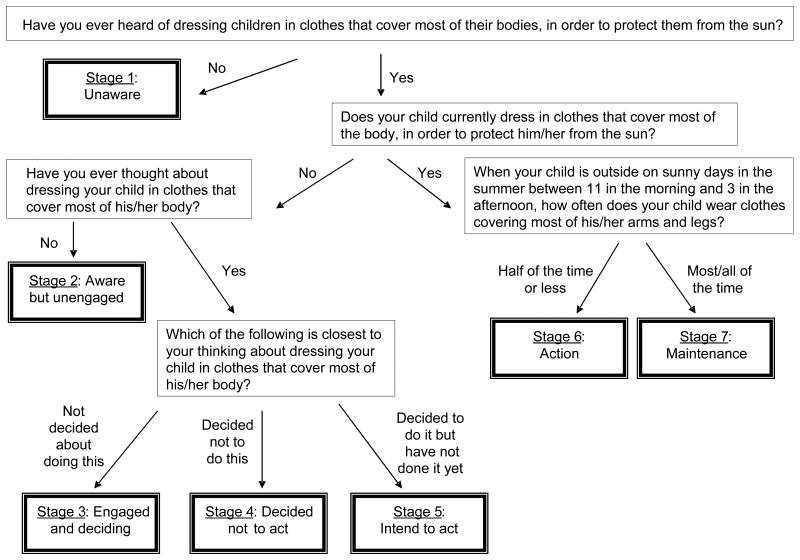
This study evaluated the effectiveness of a partially tailored newsletter intervention, supplemented by sun protection resources, mailed to parents and children as the children aged from 6 to 9 years. The intervention was based on the Precaution Adoption Process Model (PAPM), a stage theory of health behavior change.27 The model is depicted in Figure 1 as applied in this study for adoption of protective clothing. Movement through seven stages is hypothesized to be influenced by cognitive mediators, including: knowledge of risk, personalization of risk, perception of risk severity, perception of effectiveness of preventive strategies, and perception of barriers to prevention strategies.27 It was hypothesized that the intervention would result in changes in PAPM cognitive mediators, PAPM stage of change, sun protection behaviors, sunburns, tanning and development of nevi.
Figure 1. Precaution Adoption Process Model (PAPM) applied to use of clothing for sun protection.
Method
Study Design
This study was a longitudinal RCT. Parent/child dyads were enrolled in 2003/2004, completed baseline measures in Summer 2004, and were randomized by computer to two groups, intervention or no-intervention control, in equal proportions in Spring 2005. Outcome assessments were conducted using annual telephone interviews of parents (cognitive outcomes, sun protection behaviors, and sun exposure experiences) and annual skin exams of children (total body nevus counts and tanning). The study was reviewed and approved by the Colorado Multiple IRB and the Kaiser Permanente of Colorado IRB. Parents provided written informed consent, and beginning at age 7 years, children provided written assent for participation.
Recruitment
Children born between January 1 and September 30 of 1998 were eligible. Recruitment was conducted in Fall 2003 and Winter 2004 through pediatric offices, a large MCO, and community sites in the greater Denver CO area. Information on the study was distributed, and interested parents were asked to contact the study office. On initial contact, an interviewer explained the study and administered an enrollment interview, which included an assessment of phenotypes related to skin cancer risk. Parents whose children had dark skin color, dark eye color, and dark hair color were informed that the program may be of minimal benefit because of low skin cancer risk. There was no racial or gender bias in the distribution of study information or the selection of participants; all responding families were invited to participate.
Intervention
The intervention, developed by the study team, consisted of three sets of educational newsletters about skin cancer and sun protection, and related sun protection resources such as a swim shirt, sun hat, sunscreen, and backpack. Newsletters were mailed to families in April and May at approximately 2-week intervals each year. In 2005, parents were sent four newsletters. In 2006, parents received four newsletters, and children received one. Parents received three project newsletters in 2007 and children received two.
Each year, the sequencing of newsletters addressed movement through PAPM stages. The first parent newsletter in each annual series presented general information about skin cancer and its causes (Stages 1 and 2). The second newsletter was designed to personalize risk perception (Stage 3) by providing tailored information about risk factors specific to each child, which included, as relevant to the child, family history of skin cancer, at-risk phenotype (hair, eye, and skin color; freckling; tendency to burn/tan), and high number of moles. Tailoring utilized information provided by parents at enrollment or observed during skin exams. Parents of children with low-risk racial backgrounds (black and Asian) were informed of the child's low risk and about types of skin cancer not caused by sun exposure.
Subsequent newsletters each year discussed the effectiveness of sun protection strategies for reducing children's risk and ways to overcome barriers to those strategies (PAPM Stages 5, 6 and 7). Shade, sunscreen, clothing/hats, and midday sun avoidance were each discussed, with the latter two emphasized. The choice to emphasize clothing/hats and sun avoidance was based on the high reported use of sunscreen in this and other populations,6 and unclear evidence at that time that sunscreen is protective against skin cancer.28
Parent testimonials conveyed positive social norms. Interactive features such as a self-assessment of skin cancer risk and a tanning quiz were included.29 Parent newsletters were 1–4 pages and approximately 500–1500 words, and were written at a 6th-grade, or below, reading level. Newsletters for children were complementary to the parent newsletters but could be used by children without parent involvement. They included age-appropriate information and activities (e.g., word searches, crossword puzzles, and matching games) about the sun, skin cancer, and sun protection.17,30 All newsletters were pilot-tested multiple times (with intervening revisions) in focus-group settings with parents and children who were the same age as the study cohort.
The control group received a letter each spring inviting them to complete data collection. All participants who attended skin exams during a given summer (both study groups) received a letter informing them of the average nevus count among children examined in that year and the nevus count for their child.
Measurement
Parent interviews
Telephone interviews were administered by trained interviewers using a computer-assisted telephone interviewing (CATI) system and a call protocol that included up to 20 attempts to reach each family. Interviewers were monitored throughout data collection, and were blinded to intervention status. Each year, the primary caregiver for the child was interviewed (95% female). Participants received $25.00 for completing each 20–30 minute interview. Enrollment interviews were conducted between November 2003 and July 2004. The baseline and follow-up interviews were conducted between June and September of 2004, 2005, 2006 and 2007, with the timing of interviews balanced across the two study groups.
The enrollment interview collected household income, parent's education and child's race/ethnicity. Child phenotype measures were based on previous studies and included skin color, hair color, eye color, and skin sensitivity to the sun (tendency to burn and tan when exposed for 1 hour at the beginning of summer with no protection).31–33 The interviews were the source for all self-reported outcomes.
Regarding sun protection, parents were asked to think about sunny days during the current summer when their child is outside for 15 minutes or longer between 11:00 a.m. and 3:00 p.m. and indicate the frequency with which the child: (1) wears clothes covering most of the arms and legs, (2) stays in the shade; (3) wears a hat; and (4) uses sunscreen. Responses were recorded on a 5-point Likert scale (1=never; 2=not very often; 3=about half the time; 4=most of the time; 5=all of the time).34 Parents were also asked how many days per week the child is usually outside between 11:00 a.m. and 3:00 p.m. for more than 15 minutes during the current summer, and on those days, how long the child is outside. Responses were used to estimate weekly outside hours during midday (range=0–24). Scores were rescaled to 1–5 for consistency with the other four behavioral measures.
A composite measure of sun protection behavior was created by summing scores on the five behavior variables, with higher scores reflecting more-frequent sun protection behavior.15,17 Parents were asked whether their child had any severe sunburns (defined as blistering) or other sunburns each year. Due to low frequency, both measures were dichotomized as none versus any.
Cognitive mediators of sun protection behavior, based on the PAPM, were developed for the study. Risk factor knowledge was measured by asking parents whether 11 different factors increased, decreased, or had no impact on the chance of someone getting skin cancer. Number of correct answers was assessed. For perceived melanoma risk, parents were asked: “Thinking about your child, what you do now, and where you live, how likely do you think [CHILD] is to get melanoma over [HIS/HER] whole life?” Responses were recorded on a scale from 1 (no chance at all) to 7 (certain to happen).
For melanoma severity, parents were asked four questions about the difficulty of treating melanoma skin cancer (e.g., “How easy or hard do you think it is for doctors to treat a typical case of melanoma?”) and the likelihood of dying from melanoma skin cancer (e.g., “Among those who get melanoma skin cancer how common do you think it is to die from it?”). Responses to questions were recorded on a 5-point scale with higher values reflecting greater perceived severity, and averaged together to form an overall measure of perceived melanoma severity (score range =1–5; Cronbach's alpha=0.76).
Parents rated the effectiveness of five sun protection behaviors in reducing their child's risk of skin cancer. Responses were on a scale ranging from 0 (not at all effective) to 10 (extremely effective), and averaged together to form a composite measure of perceived effectiveness (score range=0–10; Cronbach's alpha = 0.76). To assess perceived barriers to sun protection, parents were asked how much they agreed or disagreed with eight statements such as: “You find it difficult to keep a hat on your child.” Responses were recorded on a scale ranging from 1 (strongly disagree) to 4 (strongly agree), and averaged together to form a composite measure of perceived barriers (score range=1–4; Cronbach's alpha=0.59). Higher scores reflect greater perceived barriers.
The PAPM stage of change was assessed for the two sun protection behaviors emphasized in the intervention: clothing and midday sun avoidance (Figure 1). Deviating from previous applications of the PAPM model,27 frequency rather than duration of behavior was used to distinguish between Stages 6 (Action) and 7 (Maintenance) because most participants who practiced each behavior reported doing so for more than 6 months, but many did not consistently engage in the behavior. It was reasoned that the behaviors were more stable if consistently practiced.
Process evaluation measures
To assess intervention exposure, parents in both groups were asked where they had heard or seen information on skin cancer or sun protection. Parents who mentioned the newsletters were asked a series of questions about their use of the newsletters and accompanying resources.
Skin Exams
Exams were conducted each summer between mid-June and mid-September (balanced across the study groups) by a team of four to seven healthcare providers who received annual training from the study's lead dermatologist (JGM). Skin exam staff members were blind to intervention status. The entire body (except scalp, genitals and buttocks) was examined for nevi. Additional detail about exam procedures is available elsewhere.33,35–38
Nevi were classified as < 2mm or ≥ 2mm.32 Each year, between 34 and 66 children were examined separately by two providers to determine inter-rater reliability for nevus counts (calculated yearly using the intraclass correlation). Values ranged from 0.80 to 0.89. Tanning was measured using a Chroma Meter CR-400. Base skin color was measured five times on the unexposed, upper inner arm, and degree of tanning was calculated as the difference in L- dimension39 values in this area and the exposed lateral forearm.
Data Analysis
The analysis was conducted between 2008 and 2011. Parental reports of the frequency with which their child uses long clothing, hats, shade, sunscreen and midday sun avoidance served as the primary outcomes. Secondary outcomes included tanning, nevus counts, sunburns and PAPM mediators. Power calculations performed prior to study commencement indicated that a sample size of 315 per group at the final follow-up (2007) would provide 90% power to detect a 0.7-point difference between groups in the overall frequency of sun protection and a 2.6-point difference in the number of moles, using a two-tailed significance test with alpha = 0.05.
All models of intervention effectiveness were based on the longitudinal outcomes of the study. Linear, generalized linear and nonlinear mixed models were used to account for correlated observations within a child over time,40 using SAS/STAT 9.2 software. SAS PROC MIXED was used to analyze all continuous and ordinal outcomes and counts of nevi <2 mm (natural log– transformed). Dichotomous outcomes were analyzed using the SAS PROC GLIMMIX procedure for generalized mixed models. Perceived sun protection effectiveness and the two PAPM stage variables were assumed to follow a multinomial distribution and were analyzed using SAS PROC NLMIXED. Scores for perceived sun protection effectiveness were grouped into quartiles (0–7.9, 8–8.9, 9–9.8, and 9.9–10) to correct for a strong negative skew.
Analyses of intervention effectiveness used an intention-to-treat approach and were conducted using all study participants (n=848) and separately for the subset of white non-Hispanic participants (n=677). With the results being similar, results are reported for the white non-Hispanic subgroup due to significantly higher risk for skin cancer.41 For each outcome, all participants who provided data at one or more time points between 2004 and 2007 were included and used to estimate overall average and annual group differences during the 2005–2007 post-intervention period compared with the baseline in 2004. Follow-up year (2005–2007) and the intervention group * year interaction were considered fixed effects. Time was a repeated measures factor and study participant was a random effect.
For all models it was assumed that groups were equal at baseline due to randomization.42 Annual group differences were obtained by testing each group * year interaction against zero. The overall difference between groups across the follow-up period compared to the baseline was obtained by taking the average of the three (2005–2007) interaction effects.
Results
Participation Rates
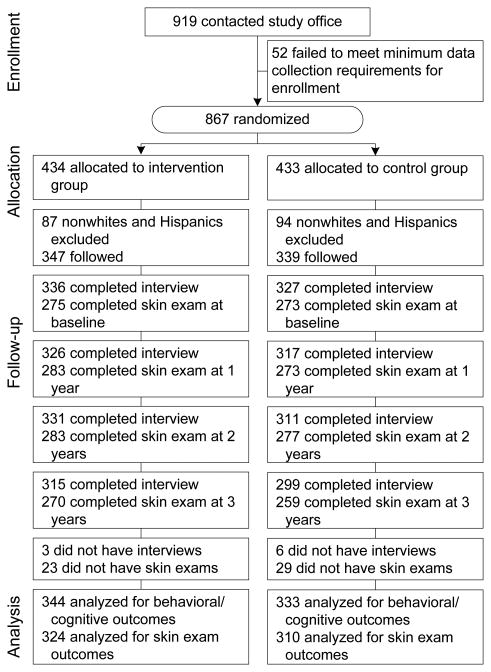
Figure 2 presents the CONSORT chart. Of 919 families that indicated interest, 867 (94%) were enrolled and completed some portion of the baseline data collection; of these, 677 white, non-Hispanic children were utilized in the present analysis. Participation in data collection was comparable between study groups throughout the follow-up period (2005–2007). Completion of interviews was 90%–97%, and completion of skin exams was 77%–82%. There were no consistent differences across years in the composition of respondents by demographic and phenotypic characteristics, study group assignment, and baseline sunscreen use (Appendix A, available online at www.ajpmonline.org). Overall, nine families provided no interview data and 52 provided no skin exam data; these families were dropped from the analysis.
Figure 2. Study flow diagram for randomized trial of stage-based mailed intervention.
Demographic and phenotypic characteristics did not differ between study groups (Table 1). A difference in baseline sunscreen use favors the control group. A total of 53% of participating children were girls. The sample had high levels of education and income, with 75% of parents having a college education or higher and 36% of households earning $100,000 or more.
Table 1. Sociodemographic characteristics by intervention status, white non-Hispanic Colorado children aged 6 years, 2004, %.
| Characteristic | All (N=686) | Control (n=339) | Intervention (n=347) | p-value* |
|---|---|---|---|---|
| Gender | ||||
| Male | 47.5 | 47.5 | 47.6 | 0.99 |
| Female | 52.5 | 52.5 | 52.4 | |
| Parent education | ||||
| Less than college | 24.9 | 24.8 | 25.1 | 0.93 |
| College or higher | 75.1 | 75.2 | 74.9 | |
| Household income | ||||
| Less than $75,000 | 37.0 | 38.0 | 36.1 | 0.84 |
| $75,000–$99,999 | 27.3 | 27.3 | 27.2 | |
| $100,000 or higher | 35.7 | 34.7 | 36.7 | |
| Hair color | ||||
| Blonde–light brown | 68.5 | 70.8 | 66.3 | 0.13 |
| Red | 3.8 | 2.9 | 4.6 | |
| Medium–dark brown | 27.3 | 25.4 | 29.1 | |
| Black | 0.4 | 0.9 | 0.0 | |
| Eye color | ||||
| Black–brown | 27.8 | 28.8 | 26.8 | 0.65 |
| Blue | 48.7 | 46.9 | 50.4 | |
| Green/hazel | 23.5 | 24.3 | 22.8 | |
| Skin color | ||||
| Dark white | 11.0 | 11.6 | 10.4 | 0.20 |
| Medium white | 37.2 | 33.8 | 40.5 | |
| Fair white | 51.8 | 54.6 | 49.1 | |
| Skin sensitivity | ||||
| Painful burn followed by no tan (Type 1) | 12.1 | 14.2 | 10.0 | 0.38 |
| Painful burn followed by light tan (Type 2) | 33.2 | 33.2 | 33.2 | |
| Slight burn followed by little tan (Type 3) | 43.6 | 41.8 | 45.3 | |
| No burn followed by good tan (Type 4) | 11.1 | 10.7 | 11.5 | |
| Baseline sunscreen use | ||||
| Never–half the time | 18.9 | 15.3 | 22.3 | 0.03 |
| Most–all the time | 81.1 | 84.7 | 77.7 | |
p-value based on Chi-square test
Receipt and Use of Intervention Materials
Among parents in the intervention group, 78%–85% reported receiving project newsletters in each study year. Of those, 70%–82% reported reading all newsletters distributed in each year, 39%–60% reported learning some or a great deal of new information each year, 31%–38% rated the newsletters in each year as excellent, and 56%–61% reported that the annual newsletters motivated them to change the sun protection practices they use with their children. Use of sun protection resources was reported at levels from 73% (sun hat, swim shirt) to 94% (backpack). A small number of parents in the control group also reported being exposed to the project newsletters each year (3%–4%).
Sun Protection Behaviors
Table 2 presents descriptive statistics for all outcomes (except sun protection effectiveness and PAPM stage variables, which are not readily presented descriptively because of their ordinal nature) by study group and year, both unadjusted and adjusted for correlations within child over time, and Table 3 provides tests of significance. Relative to baseline, the intervention group reported higher frequency of using long clothing, hats, shade, sunscreen, midday sun avoidance, and all behaviors combined averaged across the 2005–2007 follow-up period, compared to the control group. In general, group differences were small in magnitude and not consistent across years.
Table 2. Unadjusted and adjusted descriptive statistics for study outcomes by intervention status and year among white non-Hispanic participants, aged 6–9 years, 2004–2007 (n=677), M (95% CI) unless otherwise noted.
| Unadjusted | Adjusteda | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Control Group | Intervention Group | Control Group | Intervention Group | |||||
|
|
||||||||
| Clothing | ||||||||
| 2004 | 2.29 | (2.17, 2.41) | 2.34 | (2.23, 2.45) | 2.30 | (2.23, 2.38) | 2.30 | (2.23, 2.38) |
| 2005 | 2.25 | (2.14, 2.36) | 2.46 | (2.34, 2.58) | 2.27 | (2.17, 2.38) | 2.43 | (2.32, 2.53) |
| 2006 | 2.21 | (2.10, 2.32) | 2.42 | (2.31, 2.53) | 2.24 | (2.14, 2.35) | 2.41 | (2.31, 2.52) |
| 2007 | 2.32 | (2.19, 2.45) | 2.48 | (2.36, 2.60) | 2.36 | (2.24, 2.49) | 2.47 | (2.35, 2.59) |
| Hats | ||||||||
| 2004 | 2.50 | (2.39, 2.61) | 2.53 | (2.41, 2.65) | 2.51 | (2.43, 2.59) | 2.51 | (2.43, 2.59) |
| 2005 | 2.53 | (2.42, 2.64) | 2.58 | (2.47, 2.69) | 2.56 | (2.46, 2.65) | 2.57 | (2.47, 2.67) |
| 2006 | 2.47 | (2.35, 2.59) | 2.79 | (2.68, 2.90) | 2.47 | (2.37, 2.57) | 2.78 | (2.68, 2.88) |
| 2007 | 2.53 | (2.41, 2.65) | 2.61 | (2.49, 2.73) | 2.56 | (2.45, 2.67) | 2.61 | (2.50, 2.72) |
| Shade | ||||||||
| 2004 | 2.81 | (2.73, 2.89) | 2.75 | (2.66, 2.84) | 2.76 | (2.71, 2.81) | 2.76 | (2.71, 2.81) |
| 2005 | 2.86 | (2.77, 2.95) | 2.84 | (2.75, 2.93) | 2.82 | (2.74, 2.90) | 2.81 | (2.74, 2.89) |
| 2006 | 2.76 | (2.68, 2.84) | 2.84 | (2.76, 2.92) | 2.75 | (2.67, 2.82) | 2.85 | (2.77, 2.92) |
| 2007 | 2.67 | (2.57, 2.77) | 2.89 | (2.80, 2.98) | 2.62 | (2.54, 2.71) | 2.90 | (2.81, 2.98) |
| Sunscreen | ||||||||
| 2004 | 4.31 | (4.21, 4.41) | 4.11 | (4.00, 4.22) | 4.18 | (4.11, 4.25) | 4.18 | (4.11, 4.25) |
| 2005 | 4.35 | (4.26, 4.44) | 4.38 | (4.29, 4.47) | 4.30 | (4.21, 4.38) | 4.42 | (4.34, 4.50) |
| 2006 | 4.25 | (4.15, 4.35) | 4.37 | (4.28, 4.46) | 4.20 | (4.12, 4.29) | 4.41 | (4.33, 4.50) |
| 2007 | 4.22 | (4.11, 4.33) | 4.29 | (4.20, 4.38) | 4.18 | (4.09, 4.27) | 4.33 | (4.23, 4.42) |
| Midday Sun Avoidance | ||||||||
| 2004 | 3.90 | (3.77, 4.03) | 3.89 | (3.76, 4.02) | 3.90 | (3.81, 3.99) | 3.90 | (3.81, 3.99) |
| 2005 | 4.03 | (3.91, 4.15) | 4.12 | (4.01, 4.23) | 4.02 | (3.91, 4.14) | 4.11 | (4.01, 4.22) |
| 2006 | 4.07 | (3.95, 4.19) | 4.14 | (4.02, 4.26) | 4.06 | (3.94, 4.17) | 4.14 | (4.02, 4.25) |
| 2007 | 3.85 | (3.72, 3.98) | 4.03 | (3.90, 4.16) | 3.83 | (3.71, 3.96) | 4.02 | (3.89, 4.14) |
| Sun Protection Composite | ||||||||
| 2004 | 15.74 | (15.47, 16.01) | 15.47 | (15.17, 15.77) | 15.63 | (15.43, 15.83) | 15.63 | (15.43, 15.83) |
| 2005 | 16.00 | (15.73, 16.27) | 16.34 | (16.05, 16.63) | 15.97 | (15.71, 16.22) | 16.38 | (16.12, 16.63) |
| 2006 | 15.72 | (15.47, 15.97) | 16.52 | (16.24, 16.80) | 15.71 | (15.46, 15.96) | 16.58 | (16.34, 16.83) |
| 2007 | 15.51 | (15.23, 15.79) | 16.28 | (15.99, 16.57) | 15.55 | (15.28, 15.81) | 16.32 | (16.06, 16.58) |
| Nevus Count <2mm | GMa | 95% CI | GMa | 95% CI | GMa | 95% CI | GMa | 95% CI |
| 2004 | 18.14 | (16.75, 19.65) | 18.19 | (16.88, 19.60) | 18.25 | (17.32, 19.22) | 18.25 | (17.32, 19.22) |
| 2005 | 23.08 | (21.19, 25.15) | 22.31 | (20.66, 24.10) | 23.01 | (21.48, 24.65) | 22.78 | (21.29, 24.38) |
| 2006 | 24.43 | (22.55, 26.47) | 25.91 | (24.23, 27.71) | 24.89 | (23.38, 26.50) | 26.44 | (24.86, 28.13) |
| 2007 | 35.17 | (32.56, 37.99) | 34.94 | (32.51, 37.57) | 35.23 | (33.10, 37.49) | 35.64 | (33.52, 37.90) |
|
| ||||||||
| Nevi ≥ 2mm | Odds | 95% CI | Odds | 95% CI | Odds | 95% CI | Odds | 95% CI |
| 2004 | 1.26 | (0.99, 1.60) | 1.33 | (1.05, 1.69) | 1.29 | (1.09, 1.52) | 1.29 | (1.09, 1.52) |
| 2005 | 2.37 | (1.83, 3.08) | 2.04 | (1.59, 2.62) | 2.34 | (1.83, 3.00) | 2.03 | (1.60, 2.57) |
| 2006 | 3.86 | (2.88, 5.17) | 2.45 | (1.90, 3.17) | 3.71 | (2.80, 4.91) | 2.49 | (1.90, 3.25) |
| 2007 | 3.89 | (2.87, 5.26) | 3.35 | (2.52, 4.46) | 3.95 | (2.95, 5.29) | 3.26 | (2.48, 4.27) |
| Nonsevere Sunburn | Odds | 95% CI | Odds | 95% CI | Odds | 95% CI | Odds | 95% CI |
| 2004 | 0.82 | (0.66, 1.03) | 0.79 | (0.63, 0.99) | 0.82 | (0.70, 0.96) | 0.82 | (0.70, 0.96) |
| 2005 | 1.72 | (1.37, 2.17) | 1.06 | (0.85, 1.31) | 1.72 | (1.37, 2.15) | 1.07 | (0.86, 1.32) |
| 2006 | 1.31 | (1.04, 1.64) | 1.09 | (0.88, 1.36) | 1.28 | (1.03, 1.60) | 1.09 | (0.88, 1.35) |
| 2007 | 1.45 | (1.15, 1.83) | 1.25 | (1.00, 1.57) | 1.43 | (1.14, 1.79) | 1.26 | (1.01, 1.57) |
| Severe Sunburn | Odds | 95% CI | Odds | 95% CI | Odds | 95% CI | Odds | 95% CI |
| 2004 | 0.01 | (0.003, 0.03) | 0.02 | (0.007, 0.04) | 0.01 | (0.01, 0.03) | 0.01 | (0.01, 0.03) |
| 2005 | 0.02 | (0.007, 0.04) | 0.02 | (0.008, 0.04) | 0.02 | (0.01, 0.04) | 0.02 | (0.01, 0.04) |
| 2006 | 0.02 | (0.01, 0.05) | 0.02 | (0.006, 0.04) | 0.02 | (0.01, 0.05) | 0.01 | (0.01, 0.04) |
| 2007 | 0.05 | (0.03, 0.09) | 0.02 | (0.007, 0.04) | 0.05 | (0.03, 0.09) | 0.02 | (0.01, 0.04) |
| Risk Factor Awareness | ||||||||
| 2004 | 9.15 | (8.99, 9.31) | 9.11 | (8.96, 9.26) | 9.13 | (9.02, 9.24) | 9.13 | (9.02, 9.24) |
| 2005 | 9.11 | (8.96, 9.26) | 9.30 | (9.15, 9.45) | 9.11 | (8.97, 9.25) | 9.31 | (9.17, 9.44) |
| 2006 | 8.93 | (8.77, 9.09) | 9.60 | (9.47, 9.73) | 8.93 | (8.79, 9.06) | 9.61 | (9.48, 9.74) |
| 2007 | 8.94 | (8.78, 9.10) | 9.36 | (9.21, 9.51) | 8.97 | (8.82, 9.11) | 9.36 | (9.21, 9.50) |
| Perceived Barriers | ||||||||
| 2004 | 2.59 | (2.54, 2.64) | 2.59 | (2.54, 2.64) | 2.59 | (2.56, 2.63) | 2.59 | (2.56, 2.63) |
| 2005 | 2.58 | (2.53, 2.64) | 2.51 | (2.46, 2.56) | 2.58 | (2.53, 2.63) | 2.51 | (2.47, 2.56) |
| 2006 | 2.58 | (2.53, 2.63) | 2.47 | (2.42, 2.52) | 2.58 | (2.54, 2.63) | 2.47 | (2.42, 2.51) |
| 2007 | 2.62 | (2.57, 2.68) | 2.52 | (2.47, 2.58) | 2.62 | (2.58, 2.67) | 2.53 | (2.49, 2.58) |
Geometric M
Table 3. Intervention effects, mixed-model analysis among white non-Hispanic participants, aged 6–9 years, 2004–2007 (n=677).
| Average intervention effect | Annual intervention effects | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||||||||||
| 2005–2007 | 2005 | 2006 | 2007 | |||||||||||||||||
|
|
||||||||||||||||||||
| b | 95% CI | p | b | 95% CI | p | b | 95% CI | p | b | 95% CI | p | |||||||||
| Sun Protection Outcomes | ||||||||||||||||||||
|
| ||||||||||||||||||||
| Clothinga | 0.14 | 0.03 | 0.26 | 0.01 | 0.15 | 0.01 | 0.29 | 0.03 | 0.17 | 0.03 | 0.31 | 0.02 | 0.11 | −0.06 | 0.27 | 0.20 | ||||
| Hatsa | 0.12 | 0.02 | 0.22 | 0.02 | 0.02 | −0.10 | 0.14 | 0.78 | 0.31 | 0.18 | 0.43 | 0.00 | 0.04 | −0.10 | 0.18 | 0.54 | ||||
| Shadea | 0.12 | 0.04 | 0.20 | 0.002 | −0.01 | −0.11 | 0.10 | 0.91 | 0.10 | 0.00 | 0.20 | 0.05 | 0.27 | 0.16 | 0.39 | <0.001 | ||||
| Sunscreena | 0.16 | 0.07 | 0.25 | <0.001 | 0.13 | 0.02 | 0.23 | 0.02 | 0.21 | 0.10 | 0.32 | <0.00 1 | 0.15 | 0.02 | 0.27 | 0.02 | ||||
| Midday suna | 0.12 | 0.00 | 0.23 | 0.04 | 0.09 | −0.06 | 0.24 | 0.23 | 0.08 | −0.08 | 0.23 | 0.33 | 0.18 | 0.01 | 0.35 | 0.04 | ||||
| Sun protection compositea | 0.69 | 0.43 | 0.94 | <0.001 | 0.41 | 0.09 | 0.74 | 0.01 | 0.87 | 0.55 | 1.19 | <0.00 1 | 0.77 | 0.43 | 1.12 | <0.001 | ||||
|
| ||||||||||||||||||||
| Sun Exposure Outcomes | ||||||||||||||||||||
|
| ||||||||||||||||||||
| Tanning levela | 0.13 | −0.17 | 0.44 | 0.39 | 0.10 | −0.26 | 0.45 | 0.59 | 0.14 | −0.22 | 0.51 | 0.44 | 0.17 | −0.23 | 0.56 | 0.41 | ||||
| Log nevus Count <2 mma | 0.02 | −0.04 | 0.08 | 0.52 | −0.01 | −0.09 | 0.07 | 0.81 | 0.06 | −0.01 | 0.14 | 0.11 | 0.01 | −0.06 | 0.09 | 0.76 | ||||
| Nevi ≥2 mm (0/1)b | −0.25 | −0.53 | 0.04 | 0.09 | −0.14 | −0.48 | 0.19 | 0.40 | −0.40 | −0.77 | −0.03 | 0.03 | −0.19 | −0.58 | 0.20 | 0.33 | ||||
| Nonsevere Sunburn (0/1)b | −0.25 | −0.47 | −0.04 | 0.02 | −0.47 | −0.78 | −0.17 | 0.003 | −0.16 | −0.46 | 0.14 | 0.30 | −0.13 | −0.44 | 0.19 | 0.43 | ||||
| Severe sunburn (0/1)b | −0.52 | −1.23 | 0.19 | 0.15 | 0.12 | −1.08 | 1.32 | 0.85 | −0.45 | −1.62 | 0.72 | 0.45 | −1.23 | −2.27 | −0.18 | 0.02 | ||||
|
| ||||||||||||||||||||
| Cognitive Mediators | ||||||||||||||||||||
|
| ||||||||||||||||||||
| Risk factor awarenessa | 0.42 | 0.28 | 0.57 | <0.001 | 0.20 | 0.02 | 0.38 | 0.03 | 0.68 | 0.51 | 0.86 | <0.001 | 0.39 | 0.19 | 0.58 | <0.001 | ||||
| Sun protection barriersa | −0.09 | −0.14 | −0.05 | <0.001 | −0.07 | −0.12 | −0.01 | 0.02 | −0.12 | −0.17 | −0.06 | <0.001 | −0.09 | −0.15 | −0.03 | 0.003 | ||||
| Melanoma riska | 0.03 | −0.06 | 0.12 | 0.54 | 0.03 | −0.10 | 0.15 | 0.67 | 0.01 | −0.11 | 0.13 | 0.82 | 0.05 | −0.08 | 0.17 | 0.45 | ||||
| Melanoma severitya | −0.04 | −0.10 | 0.02 | 0.18 | −0.04 | −0.12 | 0.03 | 0.27 | −0.06 | −0.14 | 0.02 | 0.14 | −0.02 | −0.10 | 0.06 | 0.59 | ||||
| Nonmelanoma riska | 0.04 | −0.06 | 0.15 | 0.45 | 0.01 | −0.12 | 0.14 | 0.86 | 0.08 | −0.05 | 0.22 | 0.23 | 0.03 | −0.11 | 0.17 | 0.69 | ||||
| Nonmelanoma severitya | 0.01 | −0.06 | 0.07 | 0.86 | 0.01 | −0.07 | 0.09 | 0.79 | 0.00 | −0.08 | 0.07 | 0.92 | 0.01 | −0.07 | 0.09 | 0.81 | ||||
| Sun protection effectivenessc | 0.42 | 0.13 | 0.71 | 0.005 | 0.04 | 0.34 | 0.43 | 0.83 | 0.49 | 0.10 | 0.87 | 0.01 | 0.74 | 0.34 | 1.13 | <0.001 | ||||
| Clothing stagec | 0.64 | 0.38 | 0.90 | <0.001 | 0.60 | 0.24 | 0.95 | <0.001 | 0.78 | 0.41 | 1.13 | <0.001 | 0.55 | 0.19 | 0.91 | 0.003 | ||||
| Midday sun stagec | 0.69 | 0.40 | 0.97 | <0.001 | 0.62 | 0.24 | 1.01 | 0.002 | 0 58 | 0.20 | 0.97 | 0.003 | 0.85 | 0.46 | 1.24 | <0.001 | ||||
SAS PROC MIXED. Regression coefficients represent the difference between the intervention and control group means on each measure for a given time period relative to baseline in 2004, as tested by the intervention group*year interactions. For the average intervention effect, the three separate group*year interactions were averaged.
SAS PROC GLMMIX. Regression coefficients represent the difference between the intervention and control group in the log odds of event occurrence for a given time period relative to baseline in 2004, as tested by the intervention group*year interactions. For the average effect, the three separate group*year interactions were averaged.
SAS PROC NLMIXED. Regression coefficients reflect the difference between the intervention and control group in the cumulative (ordinal) logit associated with classification in a higher stage or quartile compared to the lowest for a given time period relative to baseline in 2004, as tested by the group*year interactions. For the average effect, the three separate group*year interactions were averaged.
Significant group differences on most behavioral outcomes were limited to 1 or 2 of the 3 follow-up years (Table 3). Only sunscreen use and the composite measure showed significant group differences in all years of the study compared to baseline. Notably, group differences generally were evident for behaviors emphasized by the intervention for that year. For example, clothing was emphasized in 2005, and a difference in clothing behavior was reported for 2005 and 2006, but not 2007. Similarly, hats were emphasized in 2006 and a difference for hats was observed that year only, while shade was emphasized in 2007 and a difference in shade use was observed for 2006 and 2007, with the 2007 difference being much larger. Effect sizes, expressed as the percentage of variance explained by the intervention (R2), were 1% (hat, shade, clothing, midday sun avoidance), 2% (sunscreen use), and 4% (composite sun protection).
Sun Exposure Outcomes
Averaged across follow-up, fewer nonsevere sunburns were reported in the intervention group compared to the control group. Analysis of individual years shows this effect was only significant for 2005 (Table 3). For severe sunburns, there was an effect only for 2007, with the intervention group reporting fewer severe sunburns. There were no intervention effects on child tanning and counts of nevi <2 mm. For the presence of nevi ≥ 2 mm, there was a marginally significant average effect (p=0.09), with the intervention group having fewer large moles in 2006 only.
Cognitive Mediators
Compared to the control group, participants in the intervention group were more aware of skin cancer risk factors, perceived fewer barriers to engaging in sun protection, and regarded sun protection as more effective in reducing skin cancer risk (average effect across years and for each individual year; Table 3). Effect sizes (percentage of variance explained by the intervention, R2) were 5% for risk factor awareness and 2% for barriers. (R2 could not be calculated for log odds or cumulative logit outcomes.) There were no group differences in parents' perceptions of their child's risk for melanoma or nonmelanoma skin cancer or in the perceived severity of either form of skin cancer. There was a significantly greater shift towards higher PAPM stage for clothing and midday sun avoidance in the intervention group compared to the control (Table 3).
Discussion
This theory-based mailed intervention produced change in sun protection behaviors and the hypothesized cognitive mediators of these behaviors. Differences were found in all behaviors measured. Differences were small in magnitude, and within years, greater differences were found in behaviors emphasized by the intervention that year. The greater progression through the PAPM stages by the intervention group compared to the control group suggests the potential for future change. Studies of smoking cessation have shown that behavior change increases over a 2-year period following receipt of a stage-based intervention.43 However, two previous sun protection studies have demonstrated that continued intervention is necessary to maintain behavior change.15,44
Although this intervention emphasized clothing and avoidance of the midday sun as more-effective strategies than sunscreen, greater sustained change in sunscreen use was observed. This may reflect a dominant media emphasis on the use of sunscreen, as well as the ease of sunscreen compared to altering clothing styles and time-of-day for outdoor activities. A recent study showed that sunscreen is effective in reducing melanoma risk,45 but clothing and sun avoidance are less costly and may be more effective forms of sun protection.7
Changes in cognitive mediators of behaviors were relatively stronger than changes in behaviors, and more consistent across years. These findings support the utility of the PAPM for both intervention design and measuring cognitive change. The lack of difference in risk and severity perceptions may be due to relatively high baseline scores on these factors. The PAPM suggests that perceptions of risk and severity are more important for movement through earlier stages of change, and perceptions of effectiveness and barriers are more proximal to behavior change.27
The reduction in reported sunburns is promising, as sunburns have been shown to be an important risk factor for melanoma.3 The group difference in nonsevere sunburns was greatest in 2005, while the group difference in severe sunburns was isolated to 2007. It can only speculated as to why the experience of sunburns does not closely reflect reports of sun protection behaviors. There may be variation in the effective use of these strategies, which requires diligence by parents and cooperation by children. This may not have been captured in the measures. Buller and colleagues found a reduction in sunburns that was not coexistent with a change in reported sun protection behaviors,46 which suggests that measures for more objective outcomes (e.g., sunburns), though still subject to reporting bias and recall, may be more sensitive to intervention effects than reports of behaviors.
Only two previous behavioral studies have demonstrated an intervention effect on nevus counts.47,48 The results of the present study suggest an effect on the presence of nevi ≥2 mm, but not smaller nevi. The lack of clear differences between groups in nevi could be due to inadequate follow-up time; the lag between sun exposure and the appearance of nevi is estimated to be 2–3 years.44,47 Thus, it is possible that differences in nevus counts will emerge in the future. Lack of differences in tanning may be due to complex interactions between genetically determined ability to tan and degree of sun exposure.37 Sunscreen generally prevents sunburns but allows tanning, and sunscreen was the most commonly used form of sun protection. Degree of tanning was only measured on 1 day each summer, and thus only reflects sun exposure during the previous few weeks.
This study has limitations. Behavioral outcomes are based on self-report. Social desirability may have encouraged parents to selectively over-report sun protection strategies that were emphasized in a particular set of intervention mailings. The directly observed outcomes, tanning and nevi, have limitations as noted above. This study is also limited by the relatively high levels of education and income of the parents, and therefore the results may not be generalizable to lower socioeconomic populations. The study design does not allow any definitive conclusions to be made about the effectiveness of individual intervention components, the incorporation of tailoring, or the ideal number of newsletters for efficiency in achieving behavior change. Finally, a large number of statistical tests were performed and some findings may be due to chance.50
This study has important strengths, including large sample size and good study retention. Approximately 80% of the intervention participants recalled receiving the intervention, while fewer than 5% of the control group may have been exposed. The randomized longitudinal design allowed observance of shifting up and down of behaviors depending on the emphasis of the intervention in each year. While behavior changes were modest, the intervention was relatively inexpensive and, since it utilized postal mail, it could be readily delivered to a geographically broad population. It could also be converted to an electronic format, delivered either by e-mail or through a website.
Conclusion
This theory-based intervention is effective and is a candidate for inclusion in multicomponent community-wide interventions that use a range of approaches and message channels, including environmental change (such as increased shade and rescheduling of organized outdoor activities), to reduce skin cancer risk. The sometimes temporary behavioral changes observed suggest that the effectiveness of this intervention can be increased by greater reinforcement and redundancy in messages (perhaps through different channels), as well as sustained message delivery. As a stand-alone intervention, this intervention will produce small changes that may not measurably reduce skin cancer risk.
Supplementary Material
Acknowledgments
Thanks are extended to the data collection staff, the nurses and physicians who conducted skin exams (Alan Arbuckle, M.D., Joanna Burch, M.D., Brenda Mokrohisky, Cathi Sommer, and Laura Wilson), the Survey Research Shared Resource of the University of Colorado Cancer Center, and the parents and children who participate in the Colorado Kids Sun Care Program. This research was supported by National Cancer Institute grant # R01-CA74592.
The authors' work on this study was funded by National Cancer Institute grant # R01-CA74592.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Lori A. Crane, Department of Community and Behavioral Health, Denver, Colorado.
Nancy A. Asdigian, Department of Community and Behavioral Health, Denver, Colorado.
Anna E. Barón, Department of Biostatistics and Informatics, Denver, Colorado.
Jenny Aalborg, Department of Community and Behavioral Health, Denver, Colorado.
Alfred C. Marcus, Department of Community and Behavioral Health, Denver, Colorado.
Stefan T. Mokrohisky, Department of Pediatrics, Denver, Colorado.
Tim E. Byers, Department of Epidemiology, School of Medicine, University of Colorado Anschutz Medical Campus, University of Colorado Cancer Center, Denver, Colorado.
Robert P. Dellavalle, Department of Epidemiology, Colorado School of Public Health, Department of Dermatology, Aurora; Veteran's Administration Hospital, Denver, Colorado.
Joseph G. Morelli, Colorado School of Public Health, Department of Dermatology, Department of Pediatrics, Denver, Colorado.
References
- 1.Howlander N, Noone AM, Krapcho M, et al. National Cancer Institute; Bethesda, MD: SEER Cancer Statistics Review, 1975-2008. seer.cancer.gov/csr/1975_2008/ [Google Scholar]
- 2.Leiter U, Garbe C. Epidemiology of melanoma and nonmelanoma skin cancer – the role of sunlight. Adv Exp Med Biol. 2008;624:89–103. doi: 10.1007/978-0-387-77574-6_8. [DOI] [PubMed] [Google Scholar]
- 3.Gandini S, Sera F, Cattaruzza MS, et al. Meta-analysis of risk factors for cutaneous melanoma: II. Sun exposure. European J Cancer. 2005;41(1):45–60. doi: 10.1016/j.ejca.2004.10.016. [DOI] [PubMed] [Google Scholar]
- 4.Elwood JM, Whitehead SM, Davison J, Galt M. Malignant melanoma in England: risks associated with nevi, freckles, social class, hair color, and sunburn. Int J Epidemiol. 1990;9(4):801–10. doi: 10.1093/ije/19.4.801. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Photobiol B:Biol. 2001;63(1–3):8–18. doi: 10.1016/s1011-1344(01)00198-1. [DOI] [PubMed] [Google Scholar]
- 6.Buller DB, Cokkinides V, Hall HI, et al. Prevalence of sunburn, sun protection, and indoor tanning behaviors among Americans: review from national surveys and case studies of 3 states. J Am Acad Dermatol. 2011;65(5 suppl 1):S114–23. doi: 10.1016/j.jaad.2011.05.033. [DOI] [PubMed] [Google Scholar]
- 7.Lazovich D, Vogel RI, Berwick M, Weinstock MA, Warshaw EM, Anderson KE. Melanoma risk in relation to use of sunscreen or other sun protection methods. Cancer Epidemiol Biomarkers Prev. 2011;20(12):2583–93. doi: 10.1158/1055-9965.EPI-11-0705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aulbert W, Parpart C, Schulz-Hornbostel R, Hinrichs B, Krüger-Corcoran D, Stockfleth E. Certification of sun protection practices in a German child day-care centre improves children's sun protection--the ‘SunPass’ pilot study. Br J Dermatol. 2009;161(3):5–12. doi: 10.1111/j.1365-2133.2009.09443.x. [DOI] [PubMed] [Google Scholar]
- 9.Crane LA, Schneider LS, Yohn J, Morelli J, Plomer K. Block the Sun, Not the Fun: evaluation of a skin cancer prevention program for child care centers. Am J Prev Med. 1999;17(1):31–7. doi: 10.1016/s0749-3797(99)00031-8. [DOI] [PubMed] [Google Scholar]
- 10.Loescher LL, Emerson J, Taylor A, Christensen DH, McKinney M. Educating preschoolers about sun safety. Am J Public Health. 1995;85(7):939–43. doi: 10.2105/ajph.85.7.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gritz ER, Tripp MK, James AS, et al. An intervention for parents to promote preschool children's sun protection: effects of Sun Protection is Fun! Prev Med. 2005;41(2):357–66. doi: 10.1016/j.ypmed.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 12.Emmons KM, Geller AC, Viswanath V, et al. The SunWise Policy intervention for school-based sun protection: a pilot study. J Sch Nurs. 2008;24(4):215–21. doi: 10.1177/1059840508319627. [DOI] [PubMed] [Google Scholar]
- 13.Gilaberte Y, Alonso JP, Teruel MP, Granizo C, Gállego J. Evaluation of a health promotion intervention for skin cancer prevention in Spain: the SolSano program. Health Promot Int. 2008;23(3):209–19. doi: 10.1093/heapro/dan020. [DOI] [PubMed] [Google Scholar]
- 14.Milne E, English DR, Johnston R, et al. Reduced sun exposure and tanning in children after 2 years of a school-based intervention (Australia) Cancer Causes Control. 2001;12(5):387–93. doi: 10.1023/a:1011294023498. [DOI] [PubMed] [Google Scholar]
- 15.Buller DB, Taylor AM, Buller MK, Powers PJ, Maloy JA, Beach BH. Evaluation of the Sunny Days, Healthy Ways sun safety curriculum for children in kindergarten through fifth grade. Pediatr Dermatol. 2006;23(4):321–9. doi: 10.1111/j.1525-1470.2006.00270.x. [DOI] [PubMed] [Google Scholar]
- 16.Hunter S, Love-Jackson K, Abdulla R, et al. Sun protection at elementary schools: a cluster randomized trial. J Natl Cancer Inst. 2010;102(7):484–92. doi: 10.1093/jnci/djq010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glanz K, Geller AC, Shigaki D, Maddock JE, Isnec MR. A randomized trial of skin cancer prevention in aquatics settings: the Pool Cool program. Health Psychol. 2002;2(6):579–87. [PubMed] [Google Scholar]
- 18.Mayer JA, Slymen DJ, Eckhardt L, et al. Reducing ultraviolet radiation exposure in children. Prev Med. 1997;26(4):516–22. doi: 10.1006/pmed.1997.0166. [DOI] [PubMed] [Google Scholar]
- 19.Mayer JA, Lewis EC, Eckhardt L, et al. Promoting sun safety among zoo visitors. Prev Med. 2001;33(3):162–9. doi: 10.1006/pmed.2001.0875. [DOI] [PubMed] [Google Scholar]
- 20.Crane LA, Deas A, Mokrohisky ST, et al. A randomized intervention study of sun protection promotion in well-child care. Prev Med. 2006;42(3):162–70. doi: 10.1016/j.ypmed.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 21.Norman GJ, Adams MA, Calfas KJ, et al. A randomized trial of a multicomponent intervention for adolescent sun protection behaviors. Arch Pediatr Adolesc Med. 2007;161(2):146–52. doi: 10.1001/archpedi.161.2.146. [DOI] [PubMed] [Google Scholar]
- 22.Glasser A, Shaheen M, Glenn BA, Bastani R. The sun sense study: an intervention to improve sun protection in children. Am J Health Behav. 2010;34(4):500–10. doi: 10.5993/ajhb.34.4.11. [DOI] [PubMed] [Google Scholar]
- 23.Hornung RL, Lennon PA, Garrett JM, DeVellis RF, Weinberg PD, Strecher VJ. Interactive computer technology for skin cancer prevention targeting children. Am J Prev Med. 2000;18(1):69–76. doi: 10.1016/s0749-3797(99)00115-4. [DOI] [PubMed] [Google Scholar]
- 24.Buller MK, Kane IL, Martin RC, et al. Randomized trial evaluating computer-based sun safety education for children in elementary school. J Cancer Educ. 2008;23(2):74–9. doi: 10.1080/08858190701818267. [DOI] [PubMed] [Google Scholar]
- 25.Dietrich AJ, Olson AL, Sox CH, et al. A community-based randomized trial encouraging sun protection for children. Pediatrics. 1998;102(6):E64. doi: 10.1542/peds.102.6.e64. [DOI] [PubMed] [Google Scholar]
- 26.Olson AL, Gaffney C, Starr P, Gibson JJ, Cole BF, Dietrich AJ. SunSafe in the Middle School Years: a community-wide intervention to change early-adolescent sun protection. Pediatrics. 2007;119(1):e247–56. doi: 10.1542/peds.2006-1579. [DOI] [PubMed] [Google Scholar]
- 27.Weinstein ND, Lyon JE, Sandman PM, Cuite CL. Experimental evidence for stages of health behavior change: the precaution adoption process model applied to home radon testing. Health Psychol. 1998;17(5):445–53. doi: 10.1037//0278-6133.17.5.445. [DOI] [PubMed] [Google Scholar]
- 28.Dennis LK, Beane Freeman LE, VanBeek MJ. Sunscreen use and the risk for melanoma: a quantitative review. Ann Intern Med. 2003;139(12):966–78. doi: 10.7326/0003-4819-139-12-200312160-00006. [DOI] [PubMed] [Google Scholar]
- 29.Glanz K, Schoenfeld E, Weinstock MA, Layi G, Kidd J, Shigaki DM. Development and reliability of a brief skin cancer risk assessment tool. Cancer Detect Prev. 2003;27(4):311–5. doi: 10.1016/s0361-090x(03)00094-1. [DOI] [PubMed] [Google Scholar]
- 30.Perry CL, Stone EJ, Parcel GS, et al. School-based cardiovascular health promotion: the Child and Adolescent Trial for Cardiovascular Health (CATCH) J School Health. 1990;60:406–13. doi: 10.1111/j.1746-1561.1990.tb05960.x. [DOI] [PubMed] [Google Scholar]
- 31.Mayer JA, Sallis JF, Eckhardt L, et al. Assessing children's ultraviolet radiation exposure: the use of parental recall via telephone interviews. Am J Public Health. 1997;87(6):1046–9. doi: 10.2105/ajph.87.6.1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gallagher RP, McLean DI, Yang P, et al. Suntan, sunburn, and pigmentation factors and the frequency of acquired melanocytic nevi in children. Arch Dermatol. 1990;126(6):770–6. [PubMed] [Google Scholar]
- 33.Dodd AT, Morelli J, Mokrohisky ST, Asdigian N, Byers TE, Crane LA. Melanocytic nevi and sun exposure in a cohort of Colorado children: anatomic distribution and site-specific sunburn. Cancer Epidemiol Biomarkers Prev. 2007;16(10):2136–43. doi: 10.1158/1055-9965.EPI-07-0453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Glanz K, Yaroch AL, Dancel M, et al. Measures of sun exposure and sun protection practices for behavioral and epidemiologic research. Arch Dermatol. 2008;144(2):217–22. doi: 10.1001/archdermatol.2007.46. [DOI] [PubMed] [Google Scholar]
- 35.Crane LA, Mokrohisky ST, Dellavalle RP, et al. Melanocytic nevus development in Colorado children born in 1998: a longitudinal study. Arch Dermatol. 2009;145(2):148–56. doi: 10.1001/archdermatol.2008.571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pettijohn KJ, Asdigian NL, Aalborg J, et al. Vacations to waterside locations result in nevus development in Colorado children. Cancer Epidemiol Biomarkers Prev. 2009;18(2):454–63. doi: 10.1158/1055-9965.EPI-08-0634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aalborg J, Morelli JG, Mokrohisky ST, et al. Tanning and increased nevus development in very-light-skinned children without red hair. Arch Dermatol. 2009;145(9):989–96. doi: 10.1001/archdermatol.2009.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Aalborg J, Morelli JG, Byers TE, Mokrohisky ST, Crane LA. Effect of hair color and sun sensitivity on nevus counts in white children in Colorado. J Am Acad Dermatol. 2010;63(3):430–9. doi: 10.1016/j.jaad.2009.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Creech LL, Mayer JA. Ultraviolet radiation exposure in children: a review of measurement strategies. Ann Behav Med. 1997;19(4):399–407. doi: 10.1007/BF02895159. [DOI] [PubMed] [Google Scholar]
- 40.McCulloch CE, Searle SR, Neuhaus JM. Generalized, Linear, and Mixed Models. 2nd. Hoboken: Wiley; 2008. [Google Scholar]
- 41.Gandini S, Sera F, Cattaruzza MS, et al. Meta-analysis of risk factors for cutaneous melanoma: III. Family history, actinic damage and phenotypic factors. Eur J Cancer. 2005;41(14):2040–59. doi: 10.1016/j.ejca.2005.03.034. [DOI] [PubMed] [Google Scholar]
- 42.Fitzmaurice G, Laird N, Ware J. Applied Longitudinal Analysis. New York: Wiley; 2004. [Google Scholar]
- 43.Prochaska JO, Redding CA, Evers KE. The transtheoretical model and stages of change. In: Glanz K, Marcus Lewis F, Rimer BK, editors. Health Behavior and Health Education: Theory Research and Practice. 2nd. San Francisco: Jossey-Bass; 1997. pp. 60–84. [Google Scholar]
- 44.Milne E, Jacoby P, Giles-Corti B, Cross D, Johnston R, English DR. The impact of the kidskin sun protection intervention on summer suntan and reported sun exposure: was it sustained? Prev Med. 2006;42(1):14–20. doi: 10.1016/j.ypmed.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 45.Green AC, Williams GM, Logan V, Strutton GM. Reduced melanoma after regular sunscreen use: randomize trial follow-up. J Clin Oncol. 2011;29(3):257–63. doi: 10.1200/JCO.2010.28.7078. [DOI] [PubMed] [Google Scholar]
- 46.Buller DB, Andersen PA, Walkosz BJ, et al. Randomized trial testing a worksite sun protection program in an outdoor recreation industry. Health Educ Behav. 2005;32(4):514–35. doi: 10.1177/1090198105276211. [DOI] [PubMed] [Google Scholar]
- 47.Milne E, Johnston R, Cross D, Giles-Corti B, English DR. Effect of a school-based sun-protection intervention on the development of melanocytic nevi in children. Am J Epidemiol. 2002;155(8):739–45. doi: 10.1093/aje/155.8.739. [DOI] [PubMed] [Google Scholar]
- 48.Gallagher RP, Rivers JK, Lee TK, Bajdik CD, McLean DI, Coldman AJ. Broad-spectrum sunscreen use and the development of new nevi in white children: a randomized controlled trial. JAMA. 2000;283(22):2955–60. doi: 10.1001/jama.283.22.2955. [DOI] [PubMed] [Google Scholar]
- 49.Milne E, English DR, Cross D, Corti B, Costa C, Johnston R. Evaluation of an intervention to reduce sun exposure in children: design and baseline results. Am J Epidemiol. 1999;150(2):164–73. doi: 10.1093/oxfordjournals.aje.a009976. [DOI] [PubMed] [Google Scholar]
- 50.Cook R, Farewell V. Multiplicity considerations in the design and analysis of clinical trials. J R Stat Soc. 1996;159(1):93–110. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.