Abstract
Background
Anthropometric measures such as waist-hip-ratio (WHR), waist-height-ratio (WHtR), waist circumference, Mid-upper arm circumference (MUAC), and upper thigh circumference, have been linked to the risk of cardiovascular disease (CVD). However, their relationships with subclinical atherosclerosis are unclear. Studies in normal-weight populations, especially in Asian countries where leanness is prevalent, are lacking.
Methods
We conducted a cross-sectional study to assess the associations of WHR, WHtR, waist circumference, hip circumference, body mass index (BMI), MUAC and upper thigh circumference with carotid intima-media thickness (cIMT) among 562 middle-aged participants free of CVD in rural Bangladesh.
Results
After adjusting for age and sex, WHR and waist circumference but not BMI showed a positive significant association with cIMT. In multivariate analysis, each standard deviation (SD) increase of WHR (0.08) or WHtR (0.07) was associated with an 8.96 μm (95% CI, 1.12–16.81) or 11.45 μm (95%CI, 0.86–22.04) difference in cIMT, respectively, after controlling for age, sex, BMI, smoking status, education level, and systolic blood pressure (SBP). The associations of WHR and WHtR with cIMT were independent of the influence of other anthropometric measures. The associations of other anthropometric measures and cIMT were not apparent.
Conclusions
In our relatively lean, healthy Asian population, WHR and WHtR appear to be better predictors of early atherosclerosis than other common surrogates of adiposity.
INTRODUCTION
Obesity is an established risk factor for clinical cardiovascular diseases (CVD), but the underlying mechanism remains unclear. Emerging clinical and epidemiological evidence indicates that the distribution of adiposity plays an important role in CVD risk, independent of the extent of general adiposity1. Several studies suggest that anthropometric measures of abdominal adiposity, such as waist-hip-ratio (WHR) and waist circumference, are better predictors of CVD risk than body mass index (BMI)2, the primary marker of general adiposity.
Atherosclerosis, a leading cause of ischemic CVD, is a process that begins in childhood and remains asymptomatic for decades before manifestation to clinical events at a later age3. Epidemiological evidence has suggested that abdominal obesity accelerates atherosclerotic progression, however, current evidence on the topic is limited and inconsistent2, 4.
Carotid intima-media thickness (cIMT), as measured noninvasively by ultrasonography5, is a established marker for subclinical atherosclerosis as well as an independent predictor for cardiovascular risk6. The reproducibility of cIMT and its validity as a surrogate for clinical CVD endpoints have been documented in large population-based study7. A few studies have examined the association between various anthropometric indices of obesity and cIMT8–12, suggesting that atherosclerosis contributes to the pathologic pathway linking obesity and CVD. However, most of the previous studies were conducted among mostly overweight or obese adults or adolescents2, 13–16, limiting the interpretation of the findings. In addition, previous evidence was derived from European and Western Caucasian populations, with limited evidence from Asians and populations with a lower BMI12, 17. Studies on anthropometric indices and cIMT may help the detection and prediction of subclinical atherosclerosis and early CVDs associated with obesity in the developing world.
In the present study, we examined the association of several anthropometric indices of obesity, including BMI, WHR, waist-height-ratio (WHtR), waist circumference, mid-upper arm circumference (MUAC), and upper thigh circumference, with the levels of cIMT in a relatively lean population in rural Bangladesh. The subjects included 562 individuals randomly selected from a prospective cohort in Bangladesh. To our knowledge, this is the first analysis of multiple anthropometric indices and cIMT within a lean population and South Asians.
MATERIALS AND METHODS
Study population
The parent study, Health Effects of Arsenic Longitudinal Study (HEALS), is an ongoing population-based prospective cohort study in Araihazar, Bangladesh18. Briefly, between October 2000 and May 2002, 11,746 men and women (“original cohort”) were recruited from a well-defined 25 km2 geographical area, under the criteria that all were married (to reduce loss to follow-up), between 18–75 years old, and had resided in the study area for at least 5 years. From 2006 to 2008, HEALS was expanded to include an additional 8,287 participants (“expansion cohort”) following the same methodologies. The overall response rate was 97%. Study participants underwent baseline clinical assessment and structured interviews. Informed consent was obtained from study participants; study procedures were approved by the Ethical Committee of the Bangladesh Medical Research Council and the Institutional Review Boards of Columbia University and the University of Chicago.
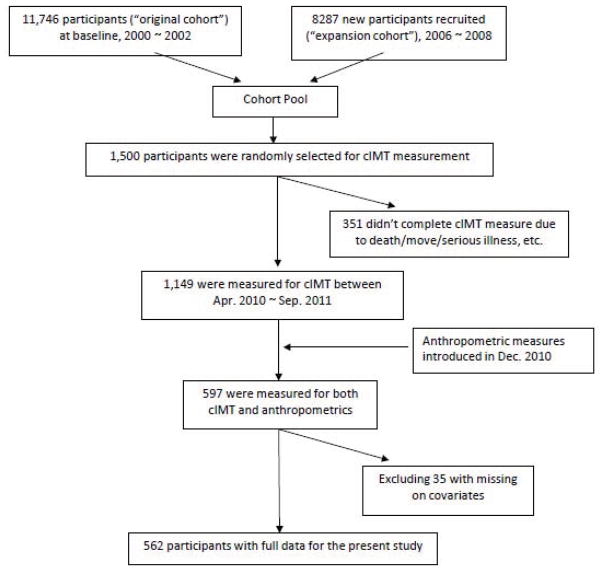
Carotid IMT was measured between April 2010 and September 2011, as previously described, as part of a previous study on urinary arsenic and IMT19. Briefly, a total of 1,500 participants were randomly selected from the overall cohorts. In total, IMT was measured for 1,149 individuals, and 351 participants did not complete IMT measurements due to deaths, move, serious illness, or time constraints. The distributions of demographic and lifestyle in those with IMT measurements and in the overall cohort were very similar19. Anthropometric measures including waist circumference, hip circumference, MUAC, and upper thigh circumference were introduced in December 2010, 8 months after the beginning of IMT measurement. A total of 597 participants had data on IMT measurements and anthropometric measures. After excluding 35 participants with missing values on other covariates of interest, a total of 562 participants were included in the present study. A flowchart of subjects selection is shown in Figure 1. Comparison of baseline characteristics (age, sex, education level, systolic blood pressure, smoking status and BMI) between the total participants with IMT measurement and the 562 participants included in this study did not show significant difference in sex, age, education level, smoking status, and age-adjusted systolic blood pressure (SBP) (data not shown).
Figure 1.
Flowchart of participant selection.
Measurement of carotid IMT
cIMT were measured with B-mode ultrasound using a SonoSite MicroMaxx ultrasound machine (SonoSite, Inc., Bothell, WA) equipped with an L38e/10-5 MHz transducer by one designated physician with extensive training in sonography throughout the study who was blinded to participants’ arsenic exposure levels, as previously described20. Briefly, all carotid imaging and IMT measurements were performed by a single physician who was trained and certified to perform carotid ultrasound measurements according to the specific ultrasound imaging and reading protocols developed, implemented and validated in the Oral Infections and Vascular Disease Epidemiology Study (INVEST)21. Bilateral carotid arteries were scanned in the common carotid artery (CCA), internal carotid artery and bifurcation, as described22. The optimal angle of insonation was used to measure the CCA-IMT in the near and far wall extending from 10mm distal to the flow divider and stopping at 20mm below the flow divider. IMT measurements were analyzed offline with Matlab (Mathworks, Natick, MA), which automatically calculated the distances between boundaries and expressed the results as the mean and maximal value. Common carotid artery (CCA) IMT has been demonstrated to be as effective as composite measurements, with measurement at a single site also yielding greater ease of access and reliability of measurements. The literature has documented that including near wall measures can reduce precision23. However, the inclusion of near wall measures should not impact validity. In our data, the variation of the summary measurement of IMT was actually reduced when near wall measures were considered. The STD of cIMT was 0.09 mm with the inclusion of near wall measures, compared with a STD of 0.11 mm without the the inclusion of near wall measures. Therefore, we used the mean of the near and far walls of the maximum CCA IMT from the both sides of the neck (mean of 4 measurements) as the main outcome variable, similar to previous studies24–26 and consistent with our prior study19. Additional sensitivity analyses for the main results were conducted using summary measure of cIMT excluding near wall measures.
Anthropometric measurement
Waist and hip circumference were measured at the end of a normal expiration with arms relaxed at the sides, directly over the skin or light clothing in standing position27. Waist circumference was measured at the midpoint between the lower margin of the last palpable rib and the top of the iliac crest (hip bone). Hip circumference was measured with the metric tape wrapped around the maximum circumference of the buttocks, with the participants standing with their feet together with weight evenly distributed over both feet. Upper thigh circumference was measured at the largest portion of the thigh with thigh muscles fully relaxed directly over the skin or light clothes. To measure the MUAC, the subject’s right arm was bent at the elbow at a 90° angle, with the upper arm held parallel to the side of the body. The midpoint of the distance between the acromion and the olecranon process of the elbow was marked. Then MUAC was measured with the metric tape around subject’s right arm at the previously marked midpoint. All the measures were read to the nearest 1cm. WHR and WHtR were calculated by dividing waist circumference by hip circumference and height respectively.
Statistical analysis
Description of baseline characteristics and anthropometric measurement were given within quartiles of cIMT; associations between these variables and cIMT were estimated by t-test or Pearson correlation with cIMT as a continuous variable.
Because waist circumference, hip circumference, MUAC, and upper thigh circumference were all highly correlated with BMI (r2 > 0.7), we investigated the association between each anthropometric measure and cIMT using BMI-adjusted anthropometric measures in two-step regression models. In the first step, each anthropometric measure (waist circumference for instance) was regressed on BMI in a separate linear model, and the residuals were computed for each observation. Residuals are, by definition, the portion of each anthropometric measure (waist circumference for instance) that is uncorrelated with the independent variable, BMI. In the second step, for each subject, we used the sum of the expected anthropometric measure (waist circumference for instance) for the mean BMI in the population and the residual for the subject as BMI-adjusted anthropometric measure (waist circumference for instance) in the linear regression model for cIMT. The residual method was adapted from energy adjustment techniques used within nutritional epidemiology28. For comparison reason, main analyses were also done using original anthropometric indices with BMI adjusted in the models instead.
Relationships between anthropometric indices and cIMT were examined by linear regression. We estimated differences in IMT as well as their 95% CIs comparing subjects in each higher quartile of a given anthropometric measure with those in the bottom quartile. We first adjusted for age and sex, and in a separate model, we further included other potential confounders such as education level, SBP, and BMI.
To assess whether the relationship between anthropometric measures and cIMT differed by other risk factors of CVD, stratified analyses by age, sex and smoking status were performed. In order to assess potential confounding of other anthropometric indices, we also estimated regression coefficients for WHR and WHtR with simultaneous adjustment for BMI-adjusted MUAC, BMI-adjusted upper thigh circumference, and BMI one at a time. All the above analysis was done in Stata 12.0. Two-tailed (α = 0.05) tests of significance were used.
RESULTS
Baseline characteristics, cIMT and anthropometric measurement are shown in Table 1. The sample consisted of 562 participants, 205 men (36.5%) and 357 women (63.5%). The mean age was 40.9 ± 9.1 with a minimum of 17 and maximum of 65 years. The education level was low among this population, with a mean education length of 2.7 ± 3.6 years. By adult BMI standards, this was a lean rural Asian population with a mean BMI of 21 kg/m2 despite a relatively high WHR with a mean of 0.91, suggesting excessive abdominal fat deposit. Currently WHO recommends cut-off points of 0.9 and 0.85 of WHR for men and women29, according to which 62.4% of men and 71.4% of women in this study could be classified as abdominal obese. Across the four quartiles of cIMT, no obvious association was observed between BMI or WHtR and cIMT. Age, SBP, waist circumference, WHR, and BMI-adjusted waist circumference were positively associated with cIMT at a statistically significant level.
Table 1.
Distribution of demographic and anthropometric characteristics by IMT.
| Overall* | Means or % of characteristics by quartiles of common carotid artery IMT
|
|
||||
|---|---|---|---|---|---|---|
| Q1 (597.5–722.4)) | Q2 (722.5–769.9) | Q3 (770.0–834.9) | Q4 (835.0–1155.0) | P Value† | ||
| No. participants | 562 | 135 | 144 | 141 | 142 | |
| Mean IMT (μm) | 786.3 (91.4) | 687.0 | 744.1 | 800.0 | 910.3 | |
| Baseline characteristics | ||||||
| Men, % | 36.5 | 24.4 | 34.0 | 38.3 | 48.6 | < 0.001 |
| Age, years | 40.9 (9.1) | 34.7 | 38.9 | 42.6 | 47.1 | < 0.001 |
| Education, years | 2.7 (3.6) | 3.1 | 2.4 | 2.9 | 2.3 | 0.902 |
| Ever smoker, % | 35.2 | 29.8 | 29.2 | 40.4 | 47.9 | < 0.001 |
| Systolic blood pressure, mmHg | 119.4 (16.0) | 114.4 | 117.3 | 120.4 | 125.2 | < 0.001 |
| Characteristics at the time of IMT measurement | ||||||
| Age | 46.5 (8.6) | 40.6 | 44.5 | 48.1 | 52.4 | < 0.001 |
| Body mass index, kg/m2 | 21.0 (4.6) | 21.3 | 20.9 | 21.4 | 20.5 | 0.252 |
| Systolic blood pressure, mmHg | 122.9 (16.0) | 117.8 | 120.1 | 123.8 | 129.5 | < 0.001 |
| Waist circumference, cm | 75.5 (10.1) | 73.3 | 75.8 | 75.4 | 77.3 | 0.029 |
| Hip circumference, cm | 82.6 (7.1) | 82.4 | 83.3 | 82.1 | 82.4 | 0.166 |
| Waist-Hip Ratio | 0.91 (0.08) | 0.89 | 0.91 | 0.92 | 0.93 | < 0.001 |
| Waist-Height Ratio | 0.49 (0.07) | 0.48 | 0.49 | 0.49 | 0.50 | 0.208 |
| Mid-arm circumference, cm | 25.6 (3.0) | 25.4 | 25.8 | 25.4 | 25.7 | 0.346 |
| Upper-thigh circumference, cm | 46.0 (5.7) | 46.0 | 46.5 | 45.6 | 45.9 | 0.145 |
| BMI-adjusted waist circumference | 75.5 (6.7) | 73.3 | 75.8 | 75.4 | 77.3 | < 0.001 |
| BMI-adjusted hip circumference | 82.6 (4.6) | 82.4 | 83.3 | 82.1 | 82.4 | 0.426 |
| BMI-adjusted MUAC | 25.6 (2.0) | 25.4 | 25.8 | 25.4 | 25.7 | 0.893 |
| BMI-adjusted upper thigh circumference | 46.0 (4.0) | 46.0 | 46.5 | 45.6 | 45.9 | 0.360 |
Values shown are mean and standard deviations in parentheses;
Values were computed with the univariate linear regression or t-test.
Table 2 shows the coefficients of linear regression between anthropometric indices and cIMT. In model 1 with age and sex adjusted, both BMI-adjusted waist circumference, WHR and WHtR were positively related to cIMT. For each SD (6.68 cm) increase in BMI-adjusted waist circumference, an average of 9.26μm difference in cIMT was observed (p < 0.05). Noticeably, the association of BMI-adjusted waist circumference as well as other anthropometric indices was not significantly associated with cIMT in fully adjusted models. An insignificant association between BMI and cIMT was observed in age-and-sex-adjusted model, and this relationship was attenuated in the multivariable model. Results based on original anthropometric indices without adjusting BMI using residual method) were shown in Appendix Table 1. The results were similar and did not change the interpretation of the data; however, caution should be taken as these results may be influenced by model instability caused by collinearity. Sensitivity analyses were also conducted using the summary measure of cIMT excluding near wall measures. However, the results were similar and therefore were not shown.
Table 2.
Differences in IMT (μm) in relation to quartiles or 1 SD increase in BMI-adjusted anthropometric measurements
| Differences in IMT (μm) (95%CI) by quartiles of each anthropometric variable
|
Coeff. per SD increase‡ | p for trend‡ | ||||
|---|---|---|---|---|---|---|
| < Q1 | Q2 | Q3 | Q4 | |||
| BMI adjusted waist circumference (cm) | < 71.98 | 71.98–75.28 | 75.29–79.46 | ≥ 79.47 | ||
| N | 141 | 140 | 140 | 141 | ||
| Model 1* | Ref. | 4.73 (−13.46, 22.92) | 0.01 (−18.21, 18.23) | 26.90 (8.18, 45.63) | 9.26 (2.75, 15.77) | 0.005 |
| Model 2† | Ref. | 4.50 (−13.39, 22.39) | −4.81 (−22.92, 13.30) | 18.40 (−1.16, 37.96) | 5.54 (−1.04, 12.12) | 0.099 |
| BMI adjusted hip circumference (cm) | < 80.24 | 80.24–82.47 | 82.48–85.01 | ≥ 85.02 | ||
| N | 141 | 140 | 140 | 141 | ||
| Model 1* | Ref. | 6.32 (−11.78, 24.43) | −6.60 (−24.77, 11.57) | −1.37 (−19.62, 16.88) | 0.62 (−5.84, 7.08) | 0.850 |
| Model 2† | Ref. | 4.55 (−13.18, 22.27) | −7.04 (−24.90, 10.83) | −8.46 (−26.97, 10.04) | −1.59 (−8.00, 4.82) | 0.625 |
| Waist-Hip ratio | < 0.86 | 0.86–0.91 | 0.91–0.96 | ≥ 0.96 | ||
| N | 141 | 146 | 134 | 141 | ||
| Model 1* | Ref. | 8.39 (−9.57, 26.37) | 8.44 (−9.98, 28.86) | 28.52 (10.21, 46.83) | 12.12 (5.30, 18.95) | 0.001 |
| Model 2† | Ref. | 4.02 (−14.19, 22.23) | 4.99 (−14.73, 24.70) | 17.65 (−3.48, 38.77) | 8.96 (1.12, 16.81) | 0.025 |
| Waist-Height ratio | < 0.44 | 0.44–0.48 | 0.49–0.53 | ≥ 0.54 | ||
| N | 166 | 119 | 124 | 153 | ||
| Model 1* | Ref. | 8.79 (−9.20, 26.78) | 15.77 (−2.10, 33.63) | 32.46 (15.28, 49.64) | 11.55 (4.82, 18.29) | 0.001 |
| Model 2† | Ref. | 10.78 (−7.45, 29.02) | 17.38 (−2.40, 37.17) | 33.31 (8.94, 57.67) | 11.45 (0.86, 22.04) | 0.034 |
| BMI adjusted upper thigh circumference (cm) | < 43.66 | 43.67–45.70 | 45.71–48.11 | ≥48.11 | ||
| N | 140 | 141 | 141 | 140 | ||
| Model 1* | Ref. | −5.09 (−23.35, 13.17) | −2.07 (−20.28, 16.14) | 0.69 (−17.67, 19.05) | 4.88 (−1.59, 11.36) | 0.139 |
| Model 2† | Ref. | −8.68 (−26.47, 9.11) | −3.80 (−21.71, 14.10) | −2.20 (−20.32, 15.93) | 3.55 (−2.82, 9.93) | 0.274 |
| BMI-adjusted MUAC (cm) | < 24.48 | 24.48–25.57 | 25.57–26.72 | ≥26.72 | ||
| N | 140 | 140 | 140 | 142 | ||
| Model 1* | Ref. | 4.16 (−14.09, 22.40) | 2.99 (−15.30, 21.28) | 12.23 (−6.21, 30.68) | 2.54 (−3.92, 9.00) | 0.441 |
| Model 2† | Ref. | 2.44 (−15.34, 20.21) | 0.34 (−17.56, 18.23) | 5.35 (−12.98, 23.68) | 0.15 (−6.23, 6.53) | 0.963 |
| BMI (kg/m2) | < 17.84 | 17.84–20.12 | 20.12–23.48 | ≥ 23.49 | ||
| N | 141 | 139 | 142 | 140 | ||
| Model 1* | Ref. | −10.80 (−28.88, 7.28) | 0.96 (−17.01, 18.93) | 18.20 (−0.20, 36.60) | 5.83 (−0.70, 12.36) | 0.080 |
| Model 2† | Ref. | −13.92 (−31.87, 4.03) | −6.58 (−24.95, 11.79) | 3.14 (−16.66, 22.94) | 0.42 (−6.64, 7.48) | 0.906 |
Model 1 adjusted for age and sex;
Model 2 adjusted for age, sex, education length, BMI (except when BMI was the main variable), smoking status, and systolic blood pressure;
Coefficients and p values were calculated with anthropometric variable included a continuous variable; SDs (standard deviation) are 6.68 cm, 4.65 cm, 4.04 cm, 2.01 cm, 0.08, 0.07, 4.56 kg/m2 for BMI-adjusted- waist, hip, upper thigh, mid-arm circumferences, WHR, WHtR and BMI, respectively.
To further examine the influence of other anthropometric measures on the relationship of WHR and WHtR with cIMT, we controlled for BMI-adjusted MUAC, BMI-adjusted thigh circumference alternatively, or BMI each at a time in the same model (Table 3). In the initial model, each SD increase of WHR (0.08) and WHtR (0.07) were associated with an 8.96 μm and 11.45 μm difference in cIMT, respectively. The estimates of the coefficients for WHR amd WHtR remained similar with the control of any one of the other anthropometric variables.
Table 3.
Differences in IMT (μm) in relation to 1 SD increase in WHR and WHtR after adjusting for MUAC/Thigh/BMI and covariates*
| Main variable | Differences in IMT per SD increase in WHR
|
Differences in IMT per SD increase in WHtR
|
||
|---|---|---|---|---|
| Coeff. (95%CI) | p-value | Coeff. (95%CI) | p-value | |
| BMI-adjusted MUAC | 9.30 (1.28, 17.31) | 0.023 | 13.86 (2.16, 25.56) | 0.020 |
| BMI adjusted thigh circumference | 8.73 (0.86, 16.59) | 0.030 | 10.71 (−0.65, 22.07) | 0.065 |
| BMI | 8.96 (1.12, 16.81) | 0.025 | 11.45 (0.86, 22.04) | 0.034 |
Model adjusted for the main variable as well as other covariates, including age, sex, education length, smoking status, SBP, and BMI (except for the model when BMI was the main variable); coefficients and p values were calculated with anthropometric variable included as continuous; SDs (standard deviation) are 0.08, 0.07, 4.56 kg/m2 for WHR, WHtR and BMI respectively.
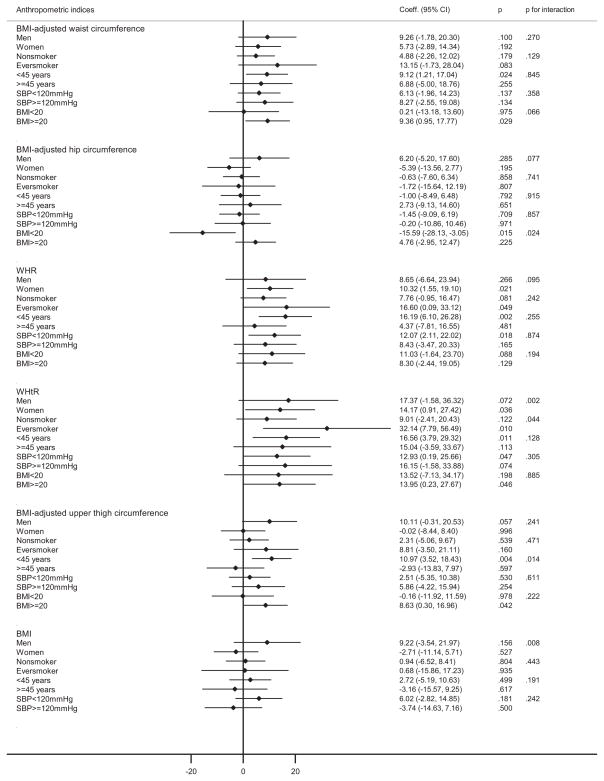
Results of stratified analysis for all the anthropometric indices in relation to cIMT according to sex, smoking status, age, SBP level and BMI are shown in Figure 2. Generally, the association patterns among the subgroups were similar to the overall pattern described in Table 2. It is worthy of noting that higher levels of BMI-adjusted waist circumference, WHR, WHtR and BMI-adjusted thigh circumference were associated with significantly increased cIMT in the younger individuals, with stronger associations than those in the older individuals, and the p-values for interaction with age were statistically significant for WHtR and upper thigh circumference. BMI-adjusted waist circumference was positively associated with cIMT in high BMI group only; in contrast, BMI-adjusted hip circumference was inversely associated with cIMT only in low BMI group. In addition, WHR appeared to be a better predictor of cIMT among women and never smokers, with a 10.32 μm (95% CI, 1.55–19.1) and 16.60 μm (95% CI, 0.09–33.12) differences in cIMT for every SD increase in WHR, respectively. Similarly, WHtR was positively related to cIMT in women and ever smokers, with a 14.17 μm (95% CI, 0.91–27.42) and 32.14 μm (95% CI, 7.79–56.49) differences in cIMT for each SD increase in WHtR, respectively. Interaction between WHtR and smoking status in cIMT was statistically significant (p = 0.044).
Figure 2.
Stratified analysis of the associations between BMI-adjusted anthropometric indices and cIMT by sex, smoking status, age, SBP and BMI*
*Model adjusted for age, education level, BMI (except when BMI was the main variable), smoking status, and SBP level (stratifying variable were not included except for age); coefficients and p values were calculated with anthropometric variable included as continuous variable; p for interaction was calculated by adding an interaction term produced by multiplying the corresponding anthropometric variable and stratifying variable (dichotomous); SDs (standard deviation) are 6.68 cm, 4.65 cm, 4.04 cm, 2.01 cm, 0.08, 0.07, 4.56 kg/m2 for BMI-adjusted waist, hip, upper thigh, mid-arm circumferences, WHR, WHtR and BMI, respectively.
DISCUSSION
Our study is one of the few studies evaluating the associations between anthropometry and cIMT, a valid clinical surrogate for atherosclerosis. We observed linear associations of both WHR and WHtR with cIMT, in this middle-aged, healthy and generally lean Asian population. The positive associations of WHR and WHtR with cIMT were stronger than associations for other anthropometric measures, and were independent of their influence.
Our data indicates that WHR and WHtR may be particularly important risk factors than other anthropometric measures for atherosclerosis in a relatively lean and healthy Asian population. The findings are consistent with the notion that caution is recommended while using BMI as a screening tool for detecting CVD risk, as abdominal adiposity may initiate atherosclerotic progress preceding enough weight gain to make a difference in BMI. A large European cohort study (EPIC) reported that the association between waist circumference and WHR and the risk of death was stronger among participants with a lower BMI than among those with a higher BMI30. WHtR has been more strongly associated with CVD risk factors, especially among Asian populations31. There’s also evidence suggesting that Asian Indians carry more fat, both total and in the abdominal region, for a given BMI than Europeans32. It has been shown that Asian Indians have a higher risk of diabetes at a lower BMI than white populations33. In our studies, other measurements such as MUAC and upper thigh circumference were not significantly related to cIMT. Other studies that investigate the relationship of MUAC and upper thigh circumference and cIMT were lacking. These anthropometric measures have been related to the risk of heart disease34 and death35. It is possible that mechanisms other than atherosclerosis underline the association of MUAC and upper thigh circumference with CVD, although more studies are needed. Taken together, the literature and our findings indicate a critical role of abdominal adiposity and atherosclerosis-related outcomes in population with a normal or low BMI especially in South Asians.
Consistent with several studies conducted in different populations2, 9, 11, 16–17, our findings suggested that fat distribution is predictive of atherosclerotic burden independent of the total amount of body mass. In multivariable adjusted model, a 0.08 (SD) increase in WHR was associated with an 8.96 μm increase in cIMT. Yan et al reported a 12 μm difference in cIMT for a 0.06 (SD) increase in WHR in 1,578 middle-aged fire fighters free of clinical CVD in Canada2, and Folsom et al found a 20 μm difference of cIMT in women and a 0.029 mm difference in men for each SD unit increase of WHR (0.07) in a cross-sectional study of blacks and whites aged 45–65 from US communities16. Evidence on association between WHtR and cIMT is limited. A study of 71 women and 29 men in Ireland reported that WHtR significantly correlated with cIMT in multivariate analysis36. Another study among 305 Spanish healthy, diabetics and hypertensive revealed that for every 0.1 point increase in WHtR, cIMT increased 0.001 mm37. However, these populations were generally overweight or obese, which made these findings less applicable to lean population.
We observed, though not statistically significant, a U-shaped association between BMI and cIMT. This is also consistent with prior epidemiological findings which suggested a survival benefit of overweight and moderate obesity in patients with existing chronic CVDs38. This has been referred to as the “obesity paradox”, which postulates that body fat might provide cardioprotective metabolic effects39 and benefits of higher metabolic reserves40. However, we observed a linear trend rather than a U-shaped relationship of WHR and WHtR with cIMT in the present study, with one possible explanation being that our population was relatively young whereas previous evidence indicated that older people benefited more from moderate adiposity39, 41. Another explanation is that while these studies focused on survival outcome in CVD patients, which could be confounded by diverse risk factors; we targeted on cIMT, a preclinical intermediate endpoint. Our study highlights the need of incorporating easily accessed anthropometric measures such as WHR or WHtR while evaluating the effects of obesity on CVD outcomes in future epidemiological studies in addition to BMI, as BMI alone may be a poor index with respect to distinguishing between lean body mass and body fat, or between central and peripheral adiposity.
WHR has been linked to coronary heart disease (CHD) independently of BMI and other conventional risk factors even in normal-weight or lean population42. The use of abdominal obesity as an index superior to BMI for predicting risk of CHD has been validated in most large prospective epidemiological studies1. Prospective studies found stronger associations between WHR and WHtR with CVD risks compared to BMI or waist circumference in both western and Asian populations43–44. Regional fat deposit shares the pathological pathway of general obesity. Increased abdominal adiposity determined by a simple WHR is a strong independent predictor of vascular endothelial dysfunction45. Reduced vascular smooth muscle responsiveness to nitric oxide46, which is an impaired function observed in patients with CHD and atherosclerosis47, has also been linked to abdominal fat accumulation. Abdominal and visceral fat depot could also lead to proinflammatory profile, increased plasma levels of C-reactive protein, dyslipidemia, insulin resistance and many other metabolic syndrome factors that have been examined to promote atherosclerosis as well as other cardiovascular events48.
Noticeably, we observed significant associations between waist circumference, WHR, WHtR, and thigh circumference with cIMT in younger participants rather than older ones as well as significant association between WHR, WHtR and cIMT in women only. Sex-specific difference in the association has been reported in a previous study in Korea12, and oppositely, they observed significant association within men only. This inconsistence may be due to the use of different anthropometric measures (WHR vs. WC) in different studies as well as potential racial and ethnic variability in susceptibility to abdominal fat accumulation and requires confirmation in future studies. Several studies have shown that the association between WHR and CVD risk is modifiable by age. The EPIC Norfolk cohort observed a stronger association between WHR and CHD risk in men less than 65 years than in men of at least 65 years but no age modification was noted in women1. In INTERHEART study, a standardized case-control study with 27,098 participants in 52 countries, there was also a stronger association between WHR and MI in younger individuals (men < 55 years, women < 65 years)49. The Nurses’ Health Study also reported higher association between abdominal obesity and CHD risk42 among women younger than 60 years. Taken together, the data suggest that WHR and WHtR are predictors of CVD risks or early atherosclerosis across different populations in the middle age, a critical time that modifications of lifetyles may have greater impact.
Several strengths of this study should be mentioned. First of all, to the best of our knowledge, this is the first investigation of the association between regional obesity and preclinical atherosclerostic progression among normal-weight South Asians using multiple anthropometric measures. A full consideration of these measures is critial, as abundent evidence from epidemioloigcal studies suggests that fat distribution as well as different body composition (fat vs. lean mass) may exert differing or even opposite efects on certain disease outcomes. Second, we addressed the colinearity between anthropometric indices and BMI with residual method, making our results more rubust with regard to the confouding effect of general adiposity. Our study is subjected to the usual limitations of cross-sectional studies, but the possibility of reverse causation was largely reduced as all the participants were free of CVD conditions. We did not include metabolic indicators such as plasma lipids and fasting insulin in the regression models as they were unavailable in this study. However, we consider metabolic abnormalities as part of the pathological linkage between abdominal obesity and arthrosclerosis, in other words, mediators that should not have controlled in the analyses. Attenuated and non-significant associations after including metabolic factors have been observed in previous study16, which further supports this notion. Also, as we used data based on one-time measurement of cIMT and anthropometric measures, measurement errors, likely non-differential, may have resulted in an underestimation of the true association. Our study focused on cIMT only, however, evidence from the literature indicates consistent associations between anthropometric variables and IMT measures at common carotid artery and carotid bifurcation and internal carotid artery12, and it also seems cIMT is stronger correlated with conventional CV risk factors than aortic intima-media thickness (aIMT) from young adulthood8. Despite that both WHR and waist circumference provide information on intra-abdominal fat, they do not appear to well distinguish between intra-abdominal and subcutaneous fat3, which have been shown to contribute differentially to metabolic syndrome risk factors50. Lastly, although we controlled for risk factors for CVD, like any epidemiologic studies, we can’t exclude the possibility of residual confounding or unmeasured confounders. For instance, we did not measure physical activity, which is inversely related to MUAC and upper thigh circumference as well as cIMT, which may potentially lead to a negative confounding. However, evidence from other studies, such as the Physicans’ Health Study, indicated that physical activity didn’t confound the association between anthropometric indices such as WHtR and CVD risk. 44
In conclusion, our study provides evidence of a positive association of WHR and WHtR with cIMT in a lean population in rural Bangladesh. Given that thinness is more prevalent in Asian than in Western populations, and that CVD is a growing concern in Asian, WHR and WHtR may be used as supplemental indices for redefining obesity and an alternative tool for further refining discrimination of early atherosclerotic burden in normal-weight population..
Supplementary Material
Highlights.
Waist-hip-ratio (WHR) and Waist-height-ratio (WHtR) positively associated with cIMT.
BMI, arm circumference, or thigh circumference was not associated with cIMT.
Associations of WHR and WHtR with cIMT were independent of other anthropometrics.
WHR/WhtR may predict preclinical atherosclerosis in normal-weight Asians.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Canoy D, Boekholdt SM, Wareham N, et al. Body fat distribution and risk of coronary heart disease in men and women in the European Prospective Investigation Into Cancer and Nutrition in Norfolk cohort: a population-based prospective study. Circulation. 2007 Dec 18;116(25):2933–2943. doi: 10.1161/CIRCULATIONAHA.106.673756. [DOI] [PubMed] [Google Scholar]
- 2.Yan RT, Yan AT, Anderson TJ, et al. The differential association between various anthropometric indices of obesity and subclinical atherosclerosis. Atherosclerosis. 2009;207(1):232–238. doi: 10.1016/j.atherosclerosis.2009.03.053. [DOI] [PubMed] [Google Scholar]
- 3.Ross R. The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature. 1993;362(6423):801–809. doi: 10.1038/362801a0. [DOI] [PubMed] [Google Scholar]
- 4.Chagas P, Caramori P, Barcellos C, Galdino TP, Gomes I, Augustin Schwanke CH. Association of Different Anthropometric Measures and Indices with Coronary Atherosclerotic Burden. Arquivos Brasileiros De Cardiologia. 2011 Nov;97(5):397–401. doi: 10.1590/s0066-782x2011005000093. [DOI] [PubMed] [Google Scholar]
- 5.O’Leary DH, Polak JF. Intima-media thickness: a tool for atherosclerosis imaging and event prediction. The American journal of cardiology. 2002;90(10C):18L–21L. doi: 10.1016/s0002-9149(02)02957-0. [DOI] [PubMed] [Google Scholar]
- 6.van den Oord SCH, Sijbrands EJG, ten Kate GL, et al. Carotid intima-media thickness for cardiovascular risk assessment: Systematic review and meta-analysis. Atherosclerosis. doi: 10.1016/j.atherosclerosis.2013.01.025. (0) [DOI] [PubMed] [Google Scholar]
- 7.Bots ML, Mulder PGH, Hofman A, van Es G-A, Grobbee DE. Reproducibility of carotid vessel wall thickness measurements. the rotterdam study. Journal of Clinical Epidemiology. 1994;47(8):921–930. doi: 10.1016/0895-4356(94)90196-1. [DOI] [PubMed] [Google Scholar]
- 8.Dawson JD, Sonka M, Blecha MB, Lin W, Davis PH. Risk Factors Associated With Aortic and Carotid Intima-Media Thickness in Adolescents and Young AdultsThe Muscatine Offspring Study. Journal of the American College of Cardiology. 2009;53(24):2273–2279. doi: 10.1016/j.jacc.2009.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Michele M, Panico S, Iannuzzi A, et al. Association of Obesity and Central Fat Distribution With Carotid Artery Wall Thickening in Middle-Aged Women. Stroke. 2002 Dec 1;33(12):2923–2928. doi: 10.1161/01.str.0000038989.90931.be. 2002. [DOI] [PubMed] [Google Scholar]
- 10.Kollias A, Psilopatis I, Karagiaouri E, et al. Adiposity, blood pressure and carotid intima-media thickness in Greek adolescents. Obesity. 2012:n/a–n/a. doi: 10.1002/oby.20194. [DOI] [PubMed] [Google Scholar]
- 11.Mittelman SD, Gilsanz P, Mo AO, Wood J, Dorey F, Gilsanz V. Adiposity Predicts Carotid Intima- Media Thickness in Healthy Children and Adolescents. The Journal of Pediatrics. 2010;156(4):592–597. e592. doi: 10.1016/j.jpeds.2009.10.014. [DOI] [PubMed] [Google Scholar]
- 12.Song YM, Lee K, Sung J, Kim YS, Lee JY. Sex-specific relationships between adiposity and anthropometric measures and carotid intima-media thickness in Koreans: The Healthy Twin Study. Eur J Clin Nutr. 2012 Jan;66(1):39–46. doi: 10.1038/ejcn.2011.150. [DOI] [PubMed] [Google Scholar]
- 13.Dalton M, Cameron AJ, Zimmet PZ, et al. Waist circumference, waist–hip ratio and body mass index and their correlation with cardiovascular disease risk factors in Australian adults. Journal of Internal Medicine. 2003;254(6):555–563. doi: 10.1111/j.1365-2796.2003.01229.x. [DOI] [PubMed] [Google Scholar]
- 14.Kotsis VT, Stabouli SV, Papamichael CM, Zakopoulos NA. Impact of Obesity in Intima Media Thickness of Carotid Arteries. Obesity. 2006;14(10):1708–1715. doi: 10.1038/oby.2006.196. [DOI] [PubMed] [Google Scholar]
- 15.Visscher TL, Seidell JC, Molarius A, van der Kuip D, Hofman A, Witteman JC. A comparison of body mass index, waist-hip ratio and waist circumference as predictors of all-cause mortality among the elderly: the Rotterdam study. International journal of obesity and related metabolic disorders: journal of the International Association for the Study of Obesity. 2001;25(11):1730–1735. doi: 10.1038/sj.ijo.0801787. [DOI] [PubMed] [Google Scholar]
- 16.Folsom AR, Eckfeldt JH, Weitzman S, et al. Relation of carotid artery wall thickness to diabetes mellitus, fasting glucose and insulin, body size, and physical activity. Atherosclerosis Risk in Communities (ARIC) Study Investigators. Stroke. 1994;25(1):66–73. doi: 10.1161/01.str.25.1.66. [DOI] [PubMed] [Google Scholar]
- 17.Takami R, Takeda N, Hayashi M, et al. Body fatness and fat distribution as predictors of metabolic abnormalities and early carotid atherosclerosis. Diabetes Care. 2001;24(7):1248–1252. doi: 10.2337/diacare.24.7.1248. [DOI] [PubMed] [Google Scholar]
- 18.Ahsan H, Chen Y, Parvez F, et al. Health Effects of Arsenic Longitudinal Study (HEALS): description of a multidisciplinary epidemiologic investigation. J Expo Sci Environ Epidemiol. 2006 Mar;16(2):191–205. doi: 10.1038/sj.jea.7500449. [DOI] [PubMed] [Google Scholar]
- 19.Chen Y, Wu F, Graziano J, et al. Arsenic exposure from drinking water, arsenic methylation capacity, and carotid intima-media thickness in Bangladesh. American Journal of Epidemiology. doi: 10.1093/aje/kwt001. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen Y, Hakim ME, Parvez F, Islam T, Rahman AM, Ahsan H. Arsenic exposure from drinking-water and carotid artery intima-medial thickness in healthy young adults in Bangladesh. Journal of health, population, and nutrition. 2006 Jun;24(2):253–257. [PubMed] [Google Scholar]
- 21.Desvarieux M, Demmer RT, Rundek T, et al. Periodontal microbiota and carotid intima-media thickness: the Oral Infections and Vascular Disease Epidemiology Study (INVEST) Circulation. 2005 Feb 8;111(5):576–582. doi: 10.1161/01.CIR.0000154582.37101.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Desvarieux M, Demmer RT, Rundek T, et al. Periodontal microbiota and carotid intima-media thickness the oral infections and vascular disease epidemiology study (INVEST) Circulation. 2005;111(5):576–582. doi: 10.1161/01.CIR.0000154582.37101.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Touboul P-J, Hennerici M, Meairs S, et al. Mannheim carotid intima-media thickness consensus (2004–2006) Cerebrovascular Diseases. 2006;23(1):75–80. doi: 10.1159/000097034. [DOI] [PubMed] [Google Scholar]
- 24.O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK., Jr Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. The New England journal of medicine. 1999 Jan 7;340(1):14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- 25.Kitamura A, Iso H, Imano H, et al. Carotid intima-media thickness and plaque characteristics as a risk factor for stroke in Japanese elderly men. Stroke. 2004 Dec;35(12):2788–2794. doi: 10.1161/01.STR.0000147723.52033.9e. [DOI] [PubMed] [Google Scholar]
- 26.Touboul PJ, Hennerici MG, Meairs S, et al. Mannheim carotid intima-media thickness and plaque consensus (2004-2006-2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovascular Diseases. 2012;34(4):290–296. doi: 10.1159/000343145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.WHO. WHO STEPS Surveillance; Part 2: Training and Practical Guides; Section 3: Guide to Physical Measurements (step 2) 2008. [Google Scholar]
- 28.Willett W. Implications of Total Energy Intake for Epidemiologic Analyses. Chapter 11. New York: Oxford University Press; 1998. Nutritional Epidemiology; pp. 288–291. [Google Scholar]
- 29.WHO. Waist circumference and waist-hip ratio: report of a WHO expert consultation. Geneva: World Health Organization (WHO); 2008. [Google Scholar]
- 30.Pischon T, Boeing H, Hoffmann K, et al. General and Abdominal Adiposity and Risk of Death in Europe. New England Journal of Medicine. 2008;359(20):2105–2120. doi: 10.1056/NEJMoa0801891. [DOI] [PubMed] [Google Scholar]
- 31.Hsieh SD, Muto T. Metabolic syndrome in Japanese men and women with special reference to the anthropometric criteria for the assessment of obesity: Proposal to use the waist-to-height ratio. Preventive medicine. 2006;42(2):135–139. doi: 10.1016/j.ypmed.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 32.McKeigue PM, Shah B, Marmot MG. Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet. 1991 Feb 16;337(8738):382–386. doi: 10.1016/0140-6736(91)91164-p. [DOI] [PubMed] [Google Scholar]
- 33.Snehalatha C, Viswanathan V, Ramachandran A. Cutoff values for normal anthropometric variables in asian Indian adults. Diabetes Care. 2003 May;26(5):1380–1384. doi: 10.2337/diacare.26.5.1380. [DOI] [PubMed] [Google Scholar]
- 34.Heitmann BL, Frederiksen P. Thigh circumference and risk of heart disease and premature death: prospective cohort study. BMJ: British Medical Journal. 2009:339. doi: 10.1136/bmj.b3292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mason C, Craig CL, Katzmarzyk PT. Influence of Central and Extremity Circumferences on All-cause Mortality in Men and Women. Obesity. 2008;16(12):2690–2695. doi: 10.1038/oby.2008.438. [DOI] [PubMed] [Google Scholar]
- 36.Maher V, O’Dowd M, Carey M, et al. Association of central obesity with early Carotid intima-media thickening is independent of that from other risk factors. Int J Obesity. 2009 Jan;33(1):136–143. doi: 10.1038/ijo.2008.254. [DOI] [PubMed] [Google Scholar]
- 37.Recio-Rodriguez JI, Gomez-Marcos MA, Patino-Alonso MC, et al. Abdominal obesity vs general obesity for identifying arterial stiffness, subclinical atherosclerosis and wave reflection in healthy, diabetics and hypertensive. Bmc Cardiovascular Disorders. 2012 Feb 1;:12. doi: 10.1186/1471-2261-12-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hastie CE, Padmanabhan S, Slack R, et al. Obesity paradox in a cohort of 4880 consecutive patients undergoing percutaneous coronary intervention. European heart journal. 2010;31(2):222–226. doi: 10.1093/eurheartj/ehp317. [DOI] [PubMed] [Google Scholar]
- 39.Auyeung TW, Lee JS, Leung J, Kwok T, Leung PC, Woo J. Survival in older men may benefit from being slightly overweight and centrally obese—a 5-year follow-up study in 4,000 older adults using DXA. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2010;65(1):99–104. doi: 10.1093/gerona/glp099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Doehner W, Clark A, Anker SD. The obesity paradox: weighing the benefit. European heart journal. 2010;31(2):146–148. doi: 10.1093/eurheartj/ehp339. [DOI] [PubMed] [Google Scholar]
- 41.Jee SH, Sull JW, Park J, et al. Body-Mass Index and Mortality in Korean Men and Women. New England Journal of Medicine. 2006;355(8):779–787. doi: 10.1056/NEJMoa054017. [DOI] [PubMed] [Google Scholar]
- 42.Rexrode Km, CVJHCH, et al. ABdominal adiposity and coronary heart disease in women. JAMA. 1998;280(21):1843–1848. doi: 10.1001/jama.280.21.1843. [DOI] [PubMed] [Google Scholar]
- 43.Larsson B, Svärdsudd K, Welin L, Wilhelmsen L, Björntorp P, Tibblin G. Abdominal adipose tissue distribution, obesity, and risk of cardiovascular disease and death: 13 year follow up of participants in the study of men born in 1913. BMJ. 1984;288(6428):1401–1404. doi: 10.1136/bmj.288.6428.1401. 1984-05-12 00:00:00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gelber RP, Gaziano JM, Orav EJ, Manson JE, Buring JE, Kurth T. Measures of obesity and cardiovascular risk among men and women. Journal of the American College of Cardiology. 2008 Aug 19;52(8):605–615. doi: 10.1016/j.jacc.2008.03.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Järvisalo MJ, Raitakari M, Toikka JO, et al. Endothelial Dysfunction and Increased Arterial Intima-Media Thickness in Children With Type 1 Diabetes. Circulation. 2004 Apr 13;109(14):1750–1755. doi: 10.1161/01.CIR.0000124725.46165.2C. 2004. [DOI] [PubMed] [Google Scholar]
- 46.Christou DD, Pierce GL, Walker AE, et al. Vascular smooth muscle responsiveness to nitric oxide is reduced in healthy adults with increased adiposity. American Journal of Physiology - Heart and Circulatory Physiology. 2012 Sep 15;303(6):H743–H750. doi: 10.1152/ajpheart.00394.2012. 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Heitzer T, Schlinzig T, Krohn K, Meinertz T, Münzel T. Endothelial Dysfunction, Oxidative Stress, and Risk of Cardiovascular Events in Patients With Coronary Artery Disease. Circulation. 2001 Nov 27;104(22):2673–2678. doi: 10.1161/hc4601.099485. 2001. [DOI] [PubMed] [Google Scholar]
- 48.Despres JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006 Dec 14;444(7121):881–887. doi: 10.1038/nature05488. [DOI] [PubMed] [Google Scholar]
- 49.Yusuf S, Hawken S, Ôunpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. The Lancet. 364(9438):937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 50.Alexander RW. Theodore Cooper Memorial Lecture. Hypertension and the pathogenesis of atherosclerosis. Oxidative stress and the mediation of arterial inflammatory response: a new perspective. Hypertension. 1995 Feb;25(2):155–161. doi: 10.1161/01.hyp.25.2.155. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.