Abstract
Duodenal varices are an uncommon, life-threatening cause of acute gastrointestinal (GI) bleeding commonly caused by portal hypertension. Though generally regarded as a complication of advanced cirrhosis and portal hypertension, often overlooked is that in about 2.7% of cases, it can be the first presenting symptom of advanced hepatocellular carcinoma (HCC). We report a case of an isolated, duodenal variceal bleeding as the first clinical manifestation of HCC, complicated by portal venous thrombosis. Diagnosis of HCC was established by a markedly elevated α-fetoprotein, hepatitis B surface and core antibody positivity and consistent radiological findings. Although not the first choice, variceal bleeding was successfully arrested with endoclips. The patient thereafter declined further evaluation and unsurprisingly died within a few weeks from a massive GI bleed. An initial bleed from a duodenal varix often confers a poor prognosis. Patients with HCC who present with variceal bleeding reportedly have a median survival of 71 days.
Background
Duodenal varices (DV) are an uncommon, life-threatening cause of gastrointestinal (GI) bleeding often caused by portal hypertension. They can present as profuse melena, haematochezia or haematemesis with diagnosis often made on the upper endoscopy. Isolated DV are a rare manifestation of portal hypertension in the absence of oesophageal or gastric varices as was found in this case. Although better known as a presentation of advanced cirrhosis and portal hypertension, variceal bleeding is also an important manifestation of hepatocellular carcinoma (HCC).1
As is often overlooked, this case illustrates variceal bleeding as the only initial presenting symptom in advanced HCC.
Case presentation
A 77-year-old woman was evaluated for 4–6 daily episodes of maroon-coloured stools for 2 weeks associated with abdominal discomfort and weakness. She had a medical history of well-controlled type II diabetes mellitus and hypertension, and denied alcohol, herbal medication and non-steroidal drug use. Pertinent findings on physical examination included marked conjunctival and skin pallor without scleral icterus. She was haemodynamically unstable with tachycardia with orthostatic hypotension. Abdominal examination revealed a non-distended abdomen without prominent abdominal wall veins, and mild epigastric tenderness on palpation without a fluid thrill.
Investigations
Basic laboratory tests reported haemoglobin 5.3 gm/dL, haematocrit 17.8%, mean corpuscular volume 73 0fL, white cell count 19×10E3/UL, platelet count 462×10E3/UL, blood urea nitrogen 63 mg/dL, creatinine 1.8 mg/dL, albumin 2.1 g/dL, international normalised ratio 1.4 and marginal alkaline phosphatase 136 U/L; and normal amylase, lipase, amino transferases and total bilirubin. Emergency upper endoscopy revealed no oesophageal or gastric varices, but a small non-bleeding varix in the proximal duodenum (figure 1) which was treated with endoclips. Biopsy for Helicobacter pylori testing returned as negative. Repeat endoscopy to evaluate haematochezia confirmed a bleeding duodenal varix in the second part of the duodenum (figure 2) which was reclipped.
Figure 1.
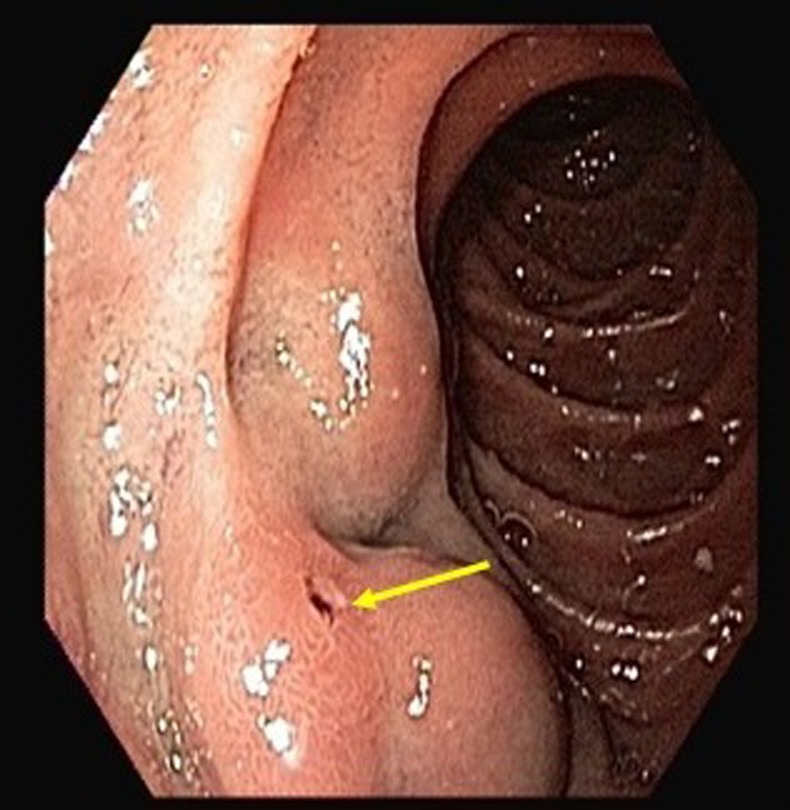
Non-bleeding varix in the second part of the duodenum seen initially on endoscopy.
Figure 2.

Isolated bleeding duodenal varix in the second part of the duodenum.
Abdominal CT revealed a heterogeneous-appearing, nodular liver with scattered hypodensities; splenomegaly; ascites; complete portal, superior mesenteric and splenic venous thrombosis with varices (figure 3). Follow-up endoscopy within 48 h confirmed haemostasis. On further evaluation, she was hepatitis B surface and core antibody positive with a markedly elevated serum α-fetoprotein (AFP) of 104 410 supportive of HCC.
Figure 3.
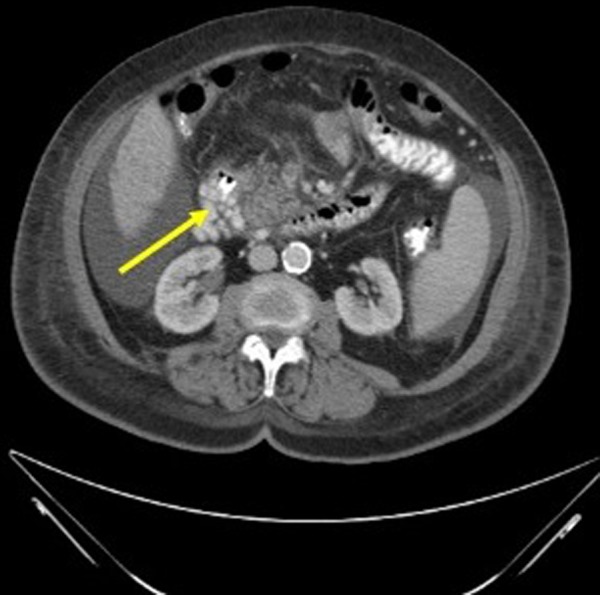
Contrast-enhanced CT of the abdomen and pelvis showing a heterogenous nodular liver and duodenal varices (arrow) with perihepatic and perisplenic free fluid.
Differential diagnosis
A non-alcoholic, elderly woman who presented with melana and haematochezia associated with mild epigastric discomfort may be bleeding from a gastritis or oesophagitis, a stomach or intestinal ulcer, a diverticular bleed or an angiodysplasia. She may also be bleeding from a varix (gastro-oesophageal or ectopic) in the presence of supporting evidence of chronic liver disease or cirrhosis.
Following diagnostic endoscopy, the source of bleeding was identified as variceal and CT evaluation revealed a cirrhotic-appearing liver with portal venous thrombosis. Further evaluation for chronic liver disease revealed hepatitis B surface and core antibody positivity, suggestive of postinfectious immunity and a markedly elevated AFP establishing diagnosis of HCC in this previously asymptomatic woman.
Treatment
The patient was initially volume resuscitated with isotonic fluids and then packed red cell transfusions until haemodynamically stable. Small non-bleeding varix visualised in the proximal duodenum on emergency endoscopy was treated with endoclips. Repeat endoscopy to evaluate haematochezia noted a bleeding duodenal varix in the second part of the duodenum which was reclipped. She subsequently received a β-blocker and a 48 h continuous infusion of octreotide with follow-up endoscopy within 48 h that confirmed haemostasis. She thereafter declined further evaluation and treatment.
Outcome and follow-up
Following a presumptive diagnosis of HCC, she declined further evaluation or treatment of the underlying cause of variceal bleed. She was discharged home with hospice services and died within a few weeks from a massive GI bleed.
Discussion
Variceal bleeding, generally a terminal event in advanced cirrhosis and portal hypertension, can also be, in about 2.7% of the cases, an initial presenting feature of a previously silent HCC.1 Isolated DV in the absence of gastric or oesophageal varices are an even rarer manifestation of portal hypertension. In the index case, hepatitis panel was supportive of postinfectious immunity. We therefore hypothesise that she developed liver cirrhosis secondary to undiagnosed chronic hepatitis B infection with transitioning to HCC which predisposed to portal venous thrombosis. Interestingly, she remained asymptomatic, only presenting with an acute variceal bleed without stigmata of chronic liver disease, evidence of encephalopathy or systemic infection. An initial bleed from a duodenal varix often confers a poor prognosis with mortality rates as high as 40%.2 Management of duodenal variceal bleeding is usually dictated by local expertise, resource availability and directed at the underlying cause.3 Treatment options are endoscopic or interventional radiological, with surgery often limited to the refractory patient. Although endoscopy is an effective therapy, additional medical management is recommended for long-term haemostasis and survival.4
While endoscopic interventions for DV are not standardised, typical options include band ligation; injection therapy with sclerosants such as thrombin, or tissue adhesives such as histoacryl glue; and clipping. Injection sclerotherapy is useful as a first-line therapeutic measure in acute duodenal variceal bleeding,5 though it carries with it the risk of tissue damage and perforation. Band ligation on the other hand is often used in the short term and mainly limited to small varices. Clipping of DV though used in our patient is generally not the method of choice. Generally, successes with endoscopic therapies have been mixed. Additional challenges with endoscopic therapy for DV have been attributed to a duodenal anatomy that hinders visualisation of the extent of the varix, and the relative thinness of the duodenal wall which increases the risk of perforation.
In patients who are not amenable to, or have failed endoscopic therapies, interventional radiological options are often used. Options include transjugular intrahepatic portosystemic shunt (TIPS) which reduces portosystemic pressure gradient, and embolisation using percutaneous transhepatic or balloon occluded retrograde transvenous obliteration.
Surgery is generally limited to patients who have failed all other therapies. Surgical options include variceal ligation, duodenal resection and surgical shunt placement. A surgical shunt though invasive has been reported to be the most effective procedure to stop acute and subsequent bleeding from DV.2
Patients with HCC who present with variceal bleeding are mostly characterised by the presence of more severe cirrhosis and a high incidence of portal venous thrombosis caused by tumour infiltration or advanced cirrhosis.1 These patients can be expected to have significantly worse outcomes than general patients with HCC with an overall median survival of about 71 days.6
Learning points.
Isolated duodenal varix secondary to portal hypertension is rare in the absence of oesophageal or gastric varices.
Although uncommon, variceal bleeding can be the first clinical manifestation of a previously silent hepatocellular carcinoma (HCC).
Treatment options for duodenal varices are endoscopic, interventional radiological and surgery. Although endoscopic therapy is not standardised, clipping is not the first-line treatment.
Patients with HCC who present with variceal bleeding have significantly worse clinical outcomes.
Footnotes
Contributors: All authors have made substantive contributions to the manuscript and have approved the final draft for submission.
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed
References
- 1.Lang BH, Poon RT, Fan ST, et al. Outcomes of patients with hepatocellular carcinoma presenting with variceal bleeding. Am J Gastroenterol 2004;99:2158–65 [DOI] [PubMed] [Google Scholar]
- 2.Khouqeer F, Morrow C, Jordan P. Duodenal varices as a cause of massive upper gastrointestinal bleeding. Surgery 1987;102:548–52 [PubMed] [Google Scholar]
- 3.Attila T, Kolbeck KJ, Bland ZM, et al. Duodenal variceal bleeding successfully treated with transjugular intrahepatic portosystemic shunt: a case report and review of the literature. Turk J Gastroenterol 2008;19:284–90 [PubMed] [Google Scholar]
- 4.Kakizaki S, Toyoda M, Ichikawa T, et al. Clinical characteristics and treatment for patients presenting with bleeding duodenal varices. Dig Endosc 2010;22:275–81 [DOI] [PubMed] [Google Scholar]
- 5.Norton ID, Andrews JC, Kamath PS. Management of ectopic varices. Hepatology 1998;28:1154–8 [DOI] [PubMed] [Google Scholar]
- 6.Chen CH, Sheu JC, Huang GT, et al. Characteristics of hepatocellular carcinoma presenting with variceal bleeding. J Gastroenterol Hepatol 1998;13:170–4 [DOI] [PubMed] [Google Scholar]


