Description
A 60-year-old patient was referred to our ear nose and throat (ENT) clinic for facial pain, bilateral midface swelling and purulent nasal discharge. The patient had undergone a bilateral maxillary sinus augmentation procedure 3 weeks before. A nasal endoscopy showed purulent material from both the middle meati, while oral examination revealed a left oroantral fistula.
The head CT scan (figure 1) showed both maxillary sinuses occupied by flogistic material with disperse calcifications and confirmed the left oroantral fistula. These calcifications hint towards a diagnosis of odontogenic sinusitis: multiple calcifications in a completely opacified maxillary sinus most likely represent infected grafts dislodged from the maxillary floor. In some cases, the fragments even tend to align to the mucociliary clearance flow.1
Figure 1.
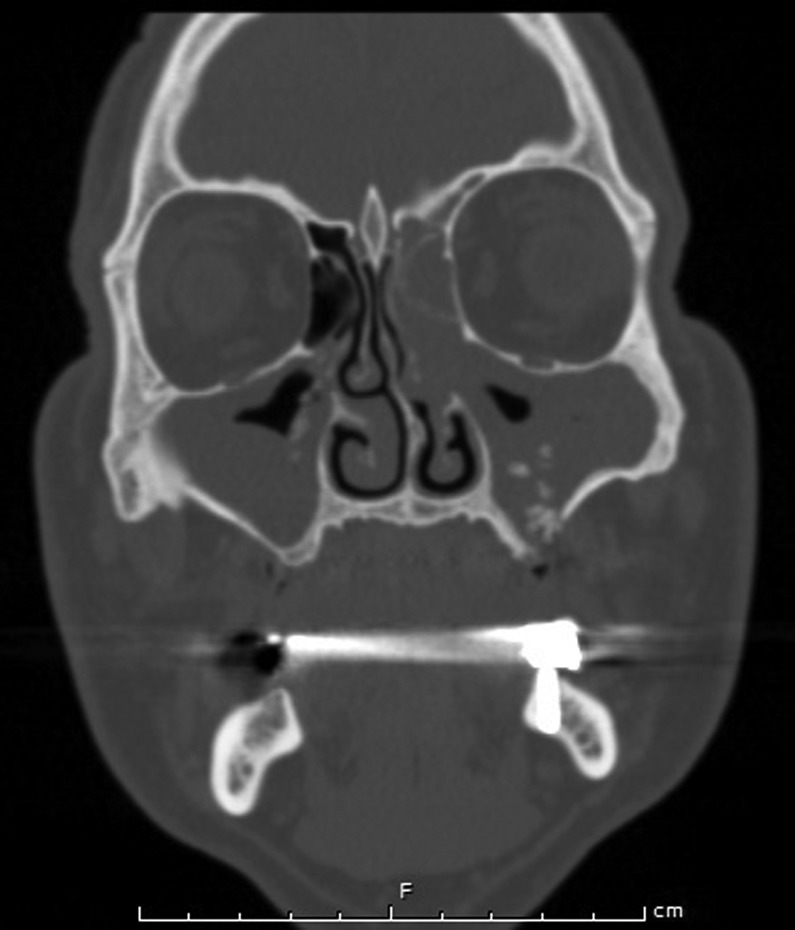
Coronal head CT scan. The image showing both the maxillary sinuses occupied by flogistic material with bilateral disperse calcifications. A left oroantral fistula can also be easily recognised.
Maxillary augmentation is considered a safe and predictable answer to vertical maxillary bone atrophies. Grafting the particulate bone and covering the lateral window access with a collagen membrane has been shown to increase implant survival.2 The use of piezoelectric tools has gained popularity to reduce damage to the Schneiderian membrane.
According to the classification of sinonasal complications following dental treatment, the patient showed a class 1a complication (condition following maxillary sinus augmentation).3 The patient was consequentially treated with an association of functional endoscopic sinus surgery and an intraoral approach as suggested by Chiapasco et al.4 A bilateral antrostomy restored the maxillary drainage and allowed the removal of bony fragments resulting from the prior sinus augmentation. The intraoral approach on the other hand was required to completely remove the grafting material and close the oroantral fistula with local rotation flaps. The patient was intravenously administered levofloxacin 750 mg for 2 days followed by oral levoxacin 500 mg for 7 days. Endoscopic follow-up at 1, 2, 4 and 12 weeks confirmed complete healing of the sinonasal complex.
Learning points.
Grafting the particulate bone and covering the lateral window access with a collagen membrane has been shown to increase implant survival. The use of piezoelectric tools has gained popularity to reduce damage to the Schneiderian membrane.
Before performing a maxillary sinus floor augmentation always evaluate the sinonasal status of the patient and patency of the ostiomeatal complex: this will allow you to maximise the success rate of the grafting.
Maxillary sinus floor augmentation complications cannot be treated by nasal endoscopy alone: a combined oral access is not only advisable but is also required along with adequate antibiotic therapy.
Footnotes
Contributors: DDP and AMS retrieved the data and were involved in writing the article. VB and GF performed the surgical procedure on the patient. GF acted as supervisor and senior ENT consultant.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Felisati G, Saibene AM, Lenzi R, et al. Late recovery from foreign body sinusitis after maxillary sinus floor augmentation. BMJ Case Rep. Published Online First: 23 Dec 2012.10.1136/bcr-2012-007434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wallace SS, Froum SJ. Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann Periodontol 2003;8:328–43 [DOI] [PubMed] [Google Scholar]
- 3.Felisati G, Chiapasco M, Lozza P, et al. Sinonasal complications resulting from dental treatment: outcome-oriented proposal of classification and surgical protocol. Am J Rhinol Allergy 2013;27:101–6 [DOI] [PubMed] [Google Scholar]
- 4.Chiapasco M, Felisati G, Zaniboni M, et al. The treatment of sinusitis following maxillary sinus grafting with the association of functional endoscopic sinus surgery (FESS) and an intra-oral approach. Clin Oral Impl Res 2013;24:623–9 [DOI] [PubMed] [Google Scholar]


