Abstract
Objective
Little is known about whether levels of physical fitness, which is related to adiposity and physical activity (PA), have changed in children, particularly the progressive increase in childhood obesity levels. We aimed to examine the time trends in resting pulse rate (a marker of physical fitness) among UK children, in order to better understand the trends in levels of physical fitness in recent decades.
Design and setting
We used a cross-sectional study design and included data on over 22 000 children aged 9–11 years (mean 10.3 years) from five population-based studies conducted in the UK between 1980 and 2008.
Main outcome measures
Resting pulse rate (bpm).
Results
Observed mean resting pulse rate was higher for girls than boys (82.2 bpm vs 78.7 bpm). During the study period mean pulse rate increased by 0.07 bpm/year (95% CI 0.04 to 0.09) among boys and to a lesser extent among girls, by 0.04 bpm/year (0.01 to 0.06) (p<0.05 for gender interaction). For boys, there was an indication that the trend was steeper after the mid-1990s, compared to that prior to 1994 (annual increase 0.14 vs 0.04 bpm). The trends for Body Mass Index (BMI) accounted for only 13.8% (11.3% to 16.3%) of increase in pulse rate for boys and 17.2% (9.4% to 24.9%) for girls.
Conclusions
Increases in mean resting pulse rate have occurred during the period 1980–2008 in girls and especially in boys. The increase was not explained by increased BMI. The observed trends in children, though modest, could have important public health implications for future cardiovascular risk.
Keywords: Adolescent Health, Comm Child Health, Epidemiology, Obesity
What is already known.
Resting pulse rate is an important indicator of physical fitness and cardiovascular health. It is also positively associated with levels of adiposity in children.
Child adiposity levels have increased in recent decades in many populations including the UK. But the impact of secular trends in obesity on their physical fitness is not clear.
What this study adds.
Modest increases in mean resting pulse rate have occurred between 1980 and 2008 in girls and especially in boys and are not explained by increased BMI.
The observed trends in children could have important public health implications for future cardiovascular disease risk.
Introduction
Resting pulse rate is a measure of cardiovascular health, indicating relative stress placed on the cardiopulmonary system.1 In adults, increased resting pulse rate has been associated with hypertension, atherosclerosis and cardiovascular risk.2–4 In children, it is positively associated with blood pressure (BP) and adiposity.2 5 6 Resting pulse rate is a marker of physical fitness, and the two are inversely correlated, at individual and population levels.7–9
During the last 30 years, there has been growing concern about the effect on children's health of increasing adiposity10 and declining physical activity (PA) levels.11 12 It is possible that levels of physical fitness, which are related to adiposity and PA levels, have also declined in children. This would be an important public health concern, because low physical fitness is associated with increased cardiovascular disease (CVD) risk factors in children2 13 and risks of CVD mortality and morbidity in adults.2 14
Examining recent trends for physical fitness for children is challenging as there is little consistency in the measures used over time.15 However, resting pulse rate has been measured in several population-based studies in children during recent decades. Trends in resting pulse rate in children can provide important evidence of changes in physical fitness in the absence of more detailed information. However, no previous studies have investigated time trends in pulse rate in UK children, or elsewhere.
We therefore examined time trends in resting pulse rate among UK children to better understand changes in childhood physical fitness in recent decades. We specifically focused on the first decade of life in predominantly prepubertal children, an age group in which extensive survey data are available. We also examined whether trends of resting pulse rate can be explained by trends in body size.
Methods
We included five population-based studies in which resting pulse rate was recorded during BP measurement in British children aged 9–11 years.16–21 Among these studies, one (Health Survey for England (HSE)) included resting pulse rate measurements at three time points (1995–1998, 2002, 2006–2008).20 21 As resting pulse rate might differ by ethnicity,6 analyses were based on white European children.
Study samples
The 1970 British birth cohort included all births in 1 week in 1970 in Britain (n≈17 000). At 10 years, pulse rate was measured once by nurses over 1 min at the start and the end of the examination with the child seated after 2 min rest.16 Height (to 0.1 cm or ¼ inch) and weight (0.1 kg or ¼ ounce) were measured. We included 12 164 children aged 10 years in 1980.
The Brompton cohort included 1895 full-term births in Farnborough Hospital, Kent, between April 1975 and May 1977, followed to May 1985.17 We used data collected at 10 years or at 9 years when the follow-up ended. Pulse rate was measured twice by nurses with the child seated after 5 min rest. Height (cm) and weight (kg) were measured. We included 774 children aged 9–10 years in 1984–1985.
The Two-Towns Study included a sample of 9–11-year children in two English towns, Carlisle and Guildford.18 Three pulse rate measurements were taken by nurses with the Dinamap1846 BP recorder with the child seated after 5 min rest. Height (mm) and weight (0.1 kg) were measured. We included 1293 children aged 9–11 years in 1991.
The Ten-Towns Study included ten towns in England and Wales, five each with the highest and lowest rates of adult heart disease.19 22 In 1994, a survey was carried out in 9–11-year children. Two pulse rate measurements were made by nurses with the Dinamap1846 BP recorder with the child seated after 5 min rest. Height (mm) and weight (0.1 kg) were measured. We included 3363 children aged 9–11 years in 1994.
HSE is an annual health survey and has included a sample of children since 1995. We considered children aged 9–11 years in 1995–1998 and 2002 surveys (with boost child samples) and 2006–2008 surveys.21Three pulse rate measurements were taken by nurses with the Dinamap 8100 device between 1995 and 2002 with the child seated after 5 min rest,20 and with the Omron 907 BP recorder from 2003. Height (mm) and weight (0.1 kg) were measured. We included 5249 children aged 9–11 years between 1995 and 2008.
Statistical analysis
BMI (weight (kg)/height (m)2) was calculated for all children. Overweight and obesity were defined using age-specific and gender-specific International Obesity Taskforce (IOTF) standards.23
Measurements were not taken at the same age for all individuals (table 1). It is known that pulse rate decreases with age,6 whereas adiposity increases with age. We centred measures of pulse rate, height and BMI to 10.3 years (mean age of all participants) using predictions from regression models assuming a linear age trend in all studies.
Table 1.
Mean (SD) pulse rate (bpm), Body Mass Index (BMI) (kg/m2) and height (cm)*
| Age (y) | Boys | Overweight/ obese (%) | Girls | Overweight/ obese (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Study year | N† | Mean | Range | Pulse rate‡ | BMI | Height | Pulse rate‡ | BMI | Height | ||
| 1980 | 12 164 | 10.3 | 9.8–10.7 | 78.4 (10.5) | 16.9 (1.9) | 5.7 | 139.0 (6.3) | 81.9 (11.0) | 17.1 (2.2) | 9.7 | 138.6 (6.5) |
| 1984–1985 | 774 | 9.7 | 9.0–10.7 | 79.2 (10.1) | 17.2 ( 2.2) | 6.9 | 141.0 (5.7) | 82.1 (10.4) | 16.9 (1.9) | 8.3 | 140.5 (6.3) |
| 1991 | 1293 | 10.3 | 9.0–11.7 | 78.2 (12.6) | 17.5 (2.4) | 10.0 | 140.3 (6.0) | 82.4 (13.8) | 17.7 (2.7) | 18.1 | 140.0 (6.5) |
| 1994 | 3363 | 10.5 | 9.0–11.8 | 79.3 (12.2) | 17.5 (2.7) | 13.0 | 141.0 (5.7) | 82.8 (12.1) | 17.8 (2.6) | 16.5 | 140.2 (5.9) |
| 1995–1998 | 3083 | 10.5 | 9.0–11.9 | 78.6 (11.3) | 18.3 (3.3) | 16.0 | 140.2 (6.2) | 82.2 (12.0) | 18.3 (3.1) | 21.6 | 140.5 (6.4) |
| 2002 | 1181 | 10.5 | 9.0–11.9 | 80.9 (11.8) | 18.8 (3.3) | 21.9 | 140.1 (6.4) | 84.0 (11.6) | 19.2 (3.7) | 30.4 | 140.8 (6.7) |
| 2006–2008 | 985 | 10.5 | 9.0–11.9 | 80.6 (11.6) | 18.3 (3.3) | 21.1 | 141.0 (6.8) | 82.0 (12.4) | 18.8 (3.6) | 24.2 | 141.1 (7.3) |
| Total | 22 843 | 10.3 | 9.0–11.9 | 78.8 (11.1) | 17.3 (2.5) | 12.0 | 139.8 (6.4) | 82.2 (11.6) | 17.7 (2.9) | 16.7 | 139.6 (6.7) |
*All height, BMI and pulse rate measures were centred at mean age (10.3 years) using pooled estimate for all studies (estimated annual age trend for pulse rate was −2.34 bpm for boys and −1.48 bpm for girls).
†Study sample (9–11-year white European children with pulse rate measures).
‡First pulse rate reading for all studies; for 1970 cohort, the reading taken at end of exam was used.
All studies (except the 1970 cohort) had ≥2 readings at one occasion. Pulse rate tends to increase across readings which are made close together.24 We used the first reading as the resting pulse rate for these studies. For the 1970 cohort, we used the one reading at the end of the examination, which was lower than the reading at the start (mean 79.5 vs 79.9 bpm for boys; 82.0 vs 82.8 bpm for girls).
To assess whether resting pulse rate changed over time, we applied linear regression models with exact year of study as a covariate. The models were then adjusted for BMI and height to assess whether the pulse rate trends were explained by changes in BMI and height over time. The percentage of trends explained by changes in BMI and its 95% CI were estimated using bootstrap sampling. The interaction between study year and BMI was tested to establish whether the pulse rate trends differed across BMI levels.
Figure 1A indicates a nonlinear time trend for pulse rate in boys. We first applied fractional polynomial models to identify the shape of the trend. The best fitting model based on deviance (for models of the same degree), Bayesian Information Criterion and Akaike Information Criterion (models of a different degree) had only a cubic term (a+b×year3), suggesting two distinct trends. We applied a linear spline model with one knot in 1994 (determined using the likelihood profile25) to assess the trends in pulse rate during 1980–1994 and 1994–2008. As shown in figure 1B, there was no significant nonlinear trend for girls.
Figure 1.
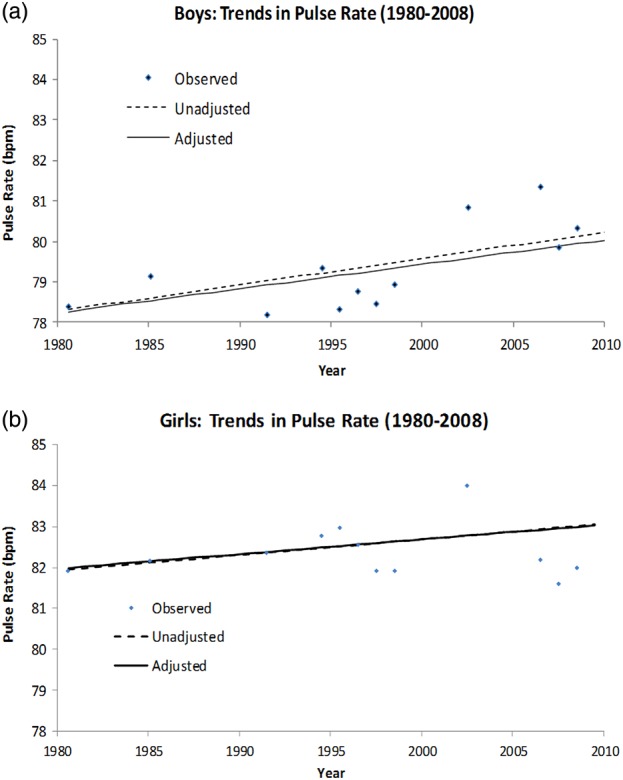
(A) Observed mean resting pulse rate and estimated time trends† for boys 1980–2008. †Models for estimating adjusted trends included individual BMI and height. (B) Observed mean resting pulse rate and estimated time trends† for girls 1980–2008. †Models for estimating adjusted trends included individual BMI and height.
We performed sensitivity analysis by restricting to (1) nationally representative studies (1970 cohort and HSE); (2) studies using automated devices (Two-Towns, Ten-Towns studies and HSE) and (3) girls aged 9–10 years to limit effects of earlier pubertal development in recent studies.
Results
Our analyses were based on 22 843 children of white European origin in the UK, from five studies at seven time points (94% of all aged 9–11 years). Overall, mean pulse rate was higher in girls (82.2 bpm) than in boys (78.7 bpm) (p<0.001 for gender difference) (table 1).
Trends in pulse rate
Table 1 shows a slight increase in mean pulse rates (1980–2008) in both sexes, which was confirmed by regression analyses (table 2). The estimated annual increases in mean resting pulse rates were 0.07 bpm (95% CI 0.04 to 0.09) among boys and 0.04 bpm (0.01 to 0.06) among girls (p<0.05 for gender interaction).
Table 2.
Regression coefficients (95% CI) for resting pulse rate (bpm)* on study year (1980–2008), Body Mass Index (BMI) (kg/m2) and height (cm)†
| Boys | Model 1‡ | Model 2‡ | Model 3‡ | Model 4‡ |
|---|---|---|---|---|
| Year | 0.07 (0.04 to 0.09) | 0.06 (0.03 to 0.08) | 0.07 (0.05 to 0.09) | 0.06 (0.04 to 0.08) |
| BMI | 0.18 (0.09 to 0.27) | 0.24 (0.14 to 0.33) | ||
| Height | −0.08 (−0.11 to −0.05) | −0.10 (−0.14 to −0.07) | ||
| Girls | ||||
| Year | 0.04 (0.01 to 0.06) | 0.03 (0.01 to 0.06) | 0.04 (0.02 to 0.07) | 0.04 (0.01 to 0.06) |
| BMI | 0.11 (0.03 to 0.20) | 0.16 (0.07 to 0.24) | ||
| Height | −0.07 (−0.11 to −0.04) | −0.09 (−0.12 to −0.05) | ||
*First pulse rate for all studies, for 1970 cohort the reading taken at end of exam was used.
†All pulse rate, BMI, and height measures were centred at mean age (10.3 years).
‡All models were fitted to all individual children: Model 1 includes study year; Model 2 includes study year and BMI; Model 3 includes study year and height; Model 4 includes study year, BMI and height.
Impact of changes in BMI and height
Mean BMI increased during the period, from 16.9 kg/m2 (boys) and 17.1 kg/m2 (girls) in 1980 to 18.8 kg/m2 and 19.2 kg/m2, respectively, in 2002, and remained high until 2008. The prevalence of overweight/obesity increased from 5.7% (boys) and 9.7% (girls) to 21.9% and 30.4%, respectively, in 2002, remaining high thereafter. While not all studies included were national samples (ie, were drawn from certain UK areas), the prevalences of overweight/obesity in the Brompton study in 1985 (7.6%) and Ten-towns study in 1994 (18%) were comparable to those in the National Study of Health and Growth (NSHG) in 1984 (8.8%) and 1994 (16.9%). Mean height increased between 1980 and 1985, but changed little thereafter (table 1). Resting pulse rate was positively associated with BMI and inversely associated with height among all children: mean pulse rate increased by 0.24 bpm (0.14 to 0.33) in boys and 0.16 bpm (0.07 to 0.24) in girls for every kg/m2 increase in BMI and decreased by 0.10 bpm (0.07 to 0.14) and 0.09 bpm (0.05 to 0.12), respectively, for every centimetre increase in height. Trends in pulse rate were only slightly reduced by adjustment for BMI and/or height, by 13.8% (11.3% to 16.3%) for boys and 17.2% (9.4% to 24.9%) for girls (table 2).
Adding polynomial terms of BMI to the model indicates a nonlinear association between BMI and resting pulse rate, such that the association strengthened with increasing BMI (data not presented). Specifically, there was no association for children with BMI<18 kg/m2, whereas for every kg/m2 increase in mean BMI mean pulse rate increased by 0.39 bpm (0.29 to 0.49) in boys and 0.21 bpm (0.11 to 0.30) in girls with BMI≥18 kg/m2 (24.8% children) (IOTF cut-offs for overweight/obesity at 10 years were 19.8 kg/m2 (boys) and 19.9 kg/m2 (girls)23). However, there was no significant interaction between study year and BMI, suggesting that pulse rate trends did not differ across BMI levels.
Findings from additional analysis
In boys, linear spline models suggest that mean pulse rate rose faster between 1994 and 2008 (annual increase of 0.14 bpm (0.09 to 0.19)) than between 1980 and 1994 (0.04 bpm (0.002 to 0.07)). The trend persisted after adjusting for BMI and height 0.13 bpm (0.07 to 0.19) (figure 2). For girls, the trend was consistent throughout the period with the annual increase of 0.04 bpm (0.02 to 0.07).
Figure 2.
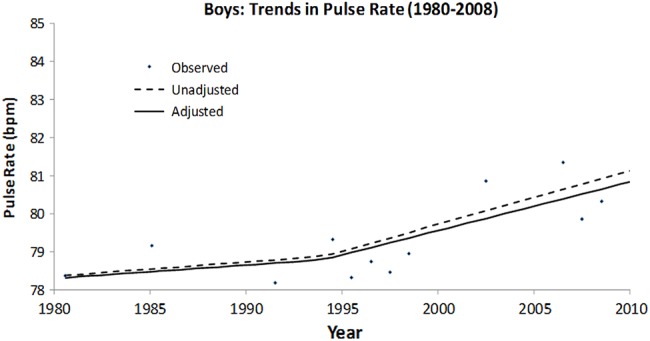
Observed mean resting pulse rate and estimated nonlinear time trends† for boys 1980–2008). †Models for estimating adjusted trends included individual BMI and height.
Sensitivity analysis restricting to national samples gave a similar annual trend for boys of 0.07 bpm (0.04 to 0.09) and a slightly weaker trend of 0.03 bpm (0.01 to 0.06) for girls. Analysis of studies using an automated device gave a similar trend for boys of 0.06 bpm (0.00 to 0.12) and a slightly stronger trend for girls of 0.08 bpm (0.05 to 0.10). Repeating analysis using 9–10-year girls made little difference to the findings with annual trends of 0.04 bpm (0.01 to 0.07), indicating that the trends were little affected by earlier maturation in recent studies (see online supplementary appendix, table A).
Discussion
In our study based on over 22 000 UK children, resting pulse rate increased by approximately 2 bpm among boys and 1 bpm among girls between 1980 and 2008. The trends for pulse rate were not explained by changes of BMI and height during the period and did not differ across levels of BMI. For boys, there was an indication that the trends were steeper after the mid-1990s, compared to the trends prior to 1994 (annual increase of 0.14 vs 0.04 bpm, respectively).
Methodological considerations
This is the first investigation in the UK or elsewhere to examine the trends in resting pulse rate in children. Resting pulse rate is a proxy measure of fitness.8 26 There are no comparable measurements for physical fitness over time. We used data from several cross-sectional studies because data from standardised pulse rate surveys over extended time periods were limited. As methodological aspects of these studies differed, we have focused on white European children aged 9–11 years and centred their pulse rate to mean age of all children. Although not all studies included were national samples, the prevalence of overweight/obesity in Brompton and Ten-town studies was consistent with that of the NSHG in comparable years. Moreover, the estimated trends in mean pulse rate were little affected by restriction to nationally representative studies HSE.
The trends persisted (slightly stronger in girls) when restricting analyses to studies which used automated devices. All studies except for 1970 cohort had two to three pulse readings after 5 min rest. For the 1970 cohort, we took the reading at the end of the examination after 2 min rest as resting pulse rate.16 Each study contributes one time point, apart from the HSE, which contributes three periods. Thus, the estimated pulse rate trends from 1995 would be largely influenced by the national samples (HSE). The sample size differed by study year and large studies would have contributed more to the trend estimation. However, weighted regression analysis (using inverse of sampling fraction) shows that the estimated pulse rate trends (0.07 bpm for boys and 0.02 bpm for girls) were consistent with those from the unweighted analysis reported here.
Comparison with other studies
Although resting pulse rate is routinely recorded when BP is measured, only two previous studies examined trends in resting pulse rate for young adults.27 28 One study of Glasgow university students focused on trends prior to 1968.27 The other study of Belfast university students shows an increase in the second half of the 20th century, but there is a gap between the early 1990s and 2000.28
We found an increase in mean resting pulse rate among boys and girls in recent decades, consistent with a previous study of adults.28 Evidence suggests that physical fitness has declined in some countries.29 However, there are no existing studies examining the trend in physical fitness in children. Previously using the same cross-sectional studies, we found increasing trends in childhood BP where BMI accounted for 15% of the observed trends.22 Although pulse rate is associated with BMI, the pulse rate trends were little altered by adjustment for BMI and height. This observation is consistent with the Belfast study, which reported trends in young adults were little influenced by changes in body size.28
While for girls, the trend is consistent throughout the period, a faster trend is found for boys from the mid-1990s which continued to late 2000s. This is also reflected in the Belfast study where there was little increase before 1993 but an increase in resting pulse rate from 1993 to 2004.28
Potential explanations
Although there is a positive association between BMI and resting pulse rate in our study, the rapid increase in BMI did not explain the pulse rate trend during the same period. However, BMI is an imperfect measure of adiposity30 and other more precise markers which differentiate between lean and fat mass might have accounted for more of the trend. Another potentially important explanation is a reduction in PA levels in children, which could be associated with a decline in physical fitness8 26 and increases in resting pulse rate.7 9 26
A school-based PA intervention shows significant improvement in cardiorespiratory fitness and cardiovascular risks in children without much change in BMI.31 32 While health benefits of PA are well accepted, children have become less active in many countries.11 Data from the HSE suggest that daily PAs in children may have declined, particularly in boys. For example, the prevalence of engaging in PA for >60 min/day in boys of same ages declined from 66.7% (63.3% to 70.0%) in 1997 to 59.2% (53.8% to 64.4%) in 2007, while there was an increase in girls from 46.4% (43.2% to 50.3%) to 55.2% (49.6% to 61.0%). The marked decline in PA in boys would be consistent with the greater increase in mean pulse rate observed. There is little research on trends in physical fitness in the UK.
Implications
Observed trends in children could have important public health implications for future CVD risk. The association between pulse rate and risk of CVD mortality is found to be stronger in boys than girls. This may also indicate gender differences in regulation and impact of pulse rate.33 If an increase of 2 bpm in mean resting pulse rate in boys persists to the adult population, this could result in a 4% increase in coronary heart disease mortality among healthy men34 and a 2% increase in risk of developing diabetes among over 65 years.35
In summary, mean resting pulse rate has increased by up to 2 bpm among 9–11-year UK children over nearly 30 years. Although modest, it is important to monitor these trends, especially in boys as they appear to have increased at a faster rate in recent years. Increases in PA in children would have a beneficial effect on their physical fitness and cardiovascular health while reducing resting pulse rate.
Supplementary Material
Acknowledgments
The authors would like to thank Professor Michael de Swiet for providing access to the Brompton data and Miss Claire Nightingale for preparing data from the Two-Towns and Ten-Towns Studies.
Footnotes
Contributors: LL, PHW and DGC conceptualised and designed the study. PHW and DGC provided data for the Two-Towns and Ten-Towns studies. CL provided data for the Brompton study. HP carried out the analyses and prepared the Methods and Results sections of the text. LL drafted the initial manuscript. All authors critically reviewed and revised the manuscript and approved the final version as submitted. LL will act as a guarantor for the paper
Funding: This work was supported by the UK Medical Research Council (MRC) Centre of Epidemiology for Child Health Small Project Grant (MRC Centre Grant G0400546) and was undertaken at UCL Institute of Child Health, which received a portion of its funding under the UK Department of Health's National Institute for Health Research (NIHR) Biomedical Research Centres funding scheme. The CPEB also benefits from funding support provided by the MRC in its capacity as the MRC Centre of Epidemiology for Child Health. The Ten-Towns Study was supported by project grants from the Wellcome Trust (Grant 038976/Z/93/Z). LL was supported by an MRC Career Development Award in Biostatistics (Grant G0601941).
Competing interests: None.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Armstrong N. Young people's physical activity patterns as assessed by heart rate monitoring. J Sports Sci 1998;16(Suppl):9–16 [DOI] [PubMed] [Google Scholar]
- 2.Van Mechelen W, Twisk JWR, Van Lenthe G, et al. Longitudinal relationships between resting heart rate and biological risk factors for CVD; the Amsterdam Growth and Health Study. J Sports Sciences 16:S17–23 [DOI] [PubMed] [Google Scholar]
- 3.Farinaro E, Stranges S, Guglielmucci G, et al. Heart rate as a risk factor in hypertensive individuals. The Italian TensioPulse Study. Nutr Metab Cardiovasc Dis 1999;9:196–202 [PubMed] [Google Scholar]
- 4.Kim JR, Kiefe CI, Liu K, et al. Heart rate and subsequent blood pressure in young adults: the CARDIA study. Hypertension 1999;33:640–6 [DOI] [PubMed] [Google Scholar]
- 5.Voors AW, Webber LS, Berenson GS. Resting heart rate and pressure-rate product of children in a total biracial community: the Bogalusa Heart Study. Am J Epidemiol 1982;116:276–86 [DOI] [PubMed] [Google Scholar]
- 6.Rabbia F, Grosso T, Cat GG, et al. Assessing resting heart rate in adolescents: determinants and correlates. J Hum Hypertens 2002;16:327–32 [DOI] [PubMed] [Google Scholar]
- 7.Shigetoh Y, Adachi H, Yamagishi S, et al. Higher heart rate may predispose to obesity and diabetes mellitus: 20-year prospective study in a general population. Am J Hypertens 2009;22:151–5 [DOI] [PubMed] [Google Scholar]
- 8.Kannel WB, Wilson P, Blair SN. Epidemiological assessment of the role of physical activity and fitness in development of cardiovascular disease. Am Heart J 1985;109:876–85 [DOI] [PubMed] [Google Scholar]
- 9.Folsom AR, Caspersen CJ, Taylor HL, et al. Leisure time physical activity and its relationship to coronary risk factors in a population-based sample. The Minnesota Heart Survey. Am J Epidemiol 1985;121:570–9 [DOI] [PubMed] [Google Scholar]
- 10.Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet 2011;377:557–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dollman J, Norton K, Norton L. Evidence for secular trends in children's physical activity behaviour. Br J Sports Med 2005;39:892–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tremblay MS, Willms JD. Is the Canadian childhood obesity epidemic related to physical inactivity? Int J Obes Relat Metab Disord 2003;27:1100–5 [DOI] [PubMed] [Google Scholar]
- 13.Rennie KL, Wells JC, McCaffrey TA, et al. The effect of physical activity on body fatness in children and adolescents. Proc Nutr Soc 2006;65:393–402 [DOI] [PubMed] [Google Scholar]
- 14.Myers J, Prakash M, Froelicher V, et al. Exercise capacity and mortality among men referred for exercise testing. N Engl J Med 2002;346:793–801 [DOI] [PubMed] [Google Scholar]
- 15.Park RJ. Measurement of physical fitness: a historical perspective.. Washington, DC: U.S. Department of Health and Human Services, Public Health Service; Office of Disease Prevention and Health Promotion Monograph Series, 1989:1–35 [Google Scholar]
- 16.Barker DJ, Osmond C, Golding J, et al. Growth in utero, blood pressure in childhood and adult life, and mortality from cardiovascular disease. BMJ 1989;298:564–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.deSwiet M, Fayers P, Shinebourne EA. Blood pressure in first 10 years of life: the Brompton study. BMJ 1992;304:23–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Whincup P, Cook D, Papacosta O, et al. Birth weight and blood pressure: cross sectional and longitudinal relations in childhood. BMJ 1995;311:773–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Whincup PH, Cook DG, Adshead F, et al. Cardiovascular risk factors in British children from towns with widely differing adult cardiovascular mortality. BMJ 1996;313:79–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The Health of Children and Young People 2002. http://www.archive2.official-documents.co.uk/document/deps/doh/survey02/hcyp/hcyp01.htm (accessed 11 Apr 2011)
- 21.The Health Survey for England 2008 Program Document. 2008. http://www.esds.ac.uk/doc/6397%5Cmrdoc%5Cpdf%5C6397interviewingdocs.pdf. (accessed 6 Jul 2011)
- 22.Peters H, Whincup PH, Cook DG, et al. Trends in blood pressure in 9 to 11-year-old children in the United Kingdom 1980–2008: the impact of obesity. J Hypertens 2012;30:1708–17 [DOI] [PubMed] [Google Scholar]
- 23.Cole TJ, Bellizzi MC, Flegal KM, et al. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 2000; 320:1240–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thomas PW, Haslum MN, MacGillivray I, et al. Does fetal heart rate predict subsequent heart rate in childhood? Early Hum Dev 1989;19:147–52 [DOI] [PubMed] [Google Scholar]
- 25.Hall CB, Ying J, Kuo L, et al. Bayesian and profile likelihood change point methods for modeling cognitive function over time. Comput Stat Data Anal 2003;42:91–109 [Google Scholar]
- 26.Tell GS, Vellar OD. Physical fitness, physical activity, and cardiovascular disease risk factors in adolescents: the Oslo Youth Study. Prev Med 1988;17:12–24 [DOI] [PubMed] [Google Scholar]
- 27.Smith GD, Galobardes B, Jeffreys M, et al. Trends in resting pulse rate among students attending Glasgow University between 1948 and 1968: analyses of cross sectional surveys. Int J Obes (Lond) 2006;30:380–1 [DOI] [PubMed] [Google Scholar]
- 28.Black A, Murray L, Cardwell C, et al. Secular trends in heart rate in young adults, 1949 to 2004: analyses of cross sectional studies. Heart 2006;92:468–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wedderkopp N, Froberg K, Hansen HS, et al. Secular trends in physical fitness and obesity in Danish 9-year-old girls and boys: Odense School Child Study and Danish substudy of the European Youth Heart Study. Scand J Med Sci Sports 2004;14:150–5 [DOI] [PubMed] [Google Scholar]
- 30.Wells JC, Fewtrell MS. Measuring body composition. Arch Dis Child 2006;91:612–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Resaland GK, Anderssen SA, Holme IM, et al. Effects of a 2-year school-based daily physical activity intervention on cardiovascular disease risk factors: the Sogndal school-intervention study. Scand J Med Sci Sports 2011;21:e122–31 [DOI] [PubMed] [Google Scholar]
- 32.Resaland GK, Andersen LB, Mamen A, et al. Effects of a 2-year school-based daily physical activity intervention on cardiorespiratory fitness: the Sogndal school-intervention study. Scand J Med Sci Sports 2011;21:302–9 [DOI] [PubMed] [Google Scholar]
- 33.Morcet JF, Safar M, Thomas F, et al. Associations between heart rate and other risk factors in a large French population. J Hypertens 1999;17(12 Pt 1):1671–6 [DOI] [PubMed] [Google Scholar]
- 34.Cooney MT, Vartiainen E, Laatikainen T, et al. Simplifying cardiovascular risk estimation using resting heart rate. Eur Heart J 2010;31:2141–7 [DOI] [PubMed] [Google Scholar]
- 35.Carnethon MR, Yan L, Greenland P, et al. Resting heart rate in middle age and diabetes development in older age. Diabetes Care 2008; 31:335–9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


