Abstract
Background
Vascular mild cognitive impairment (VMCI) is the most common type of vascular cognitive impairment induced by cerebrovascular disease. No effective medicines are currently available for VMCI.
Objective
To assess the effectiveness and safety of acupuncture for VMCI.
Methods
Seven electronic databases were searched for randomised controlled trials which investigated the effects of acupuncture compared with no treatment, placebo or conventional therapies on cognitive function or other clinical outcomes in patients with VMCI. The quality of the trials selected was evaluated according to the ‘risk of bias’ assessment provided by the Cochrane Handbook for Systematic Reviews of Interventions. RevMan V.5.1 software was employed for data analysis.
Results
Twelve trials with 691 participants were included. The methodological quality of all included trials was unclear and/or they had a high risk of bias. Meta-analysis showed acupuncture in conjunction with other therapies could significantly improve Mini-Mental State Examination scores (mean difference 1.99, 95% CI 1.09 to 2.88, random model, p<0.0001, 6 trials). No included trials mentioned any adverse events of the treatment.
Conclusions
The current clinical evidence is not of sufficient quality for wider application of acupuncture to be recommended for the treatment of VMCI, and further large, rigorously designed trials are warranted.
Keywords: Acupuncture, Systematic Reviews
Introduction
The symptoms of vascular cognitive impairment (VCI) range from mild cognitive impairment to dementia. Risk factors for VCI include hypertension, diabetes mellitus, hyperlipidemia, localised cerebrovascular disease (including cerebral infarction and cerebral haemorrhage) and diffuse cerebrovascular disease (such as leukoaraiosis and chronic cerebral ischaemia). Vascular mild cognitive impairment (VMCI) is the most common type of VCI induced by cerebrovascular disease and does not meet the diagnostic criteria for dementia. The symptoms of VMCI range from cognitive function decline including partial memory loss, decreased concentration, reduced planning ability, impaired decision-making, and slowed action and data management, to psychological symptoms such as depression and anxiety.1
Currently, no effective medicines are available for the management of VMCI. Basic actions to prevent VMCI include actively identifying and controlling the various risk factors in order to reduce cognitive function impairment: early diagnosis, early intervention and early treatment; mental and psychological treatment; treatment of complications and rehabilitation.
Mild cognitive impairment and vascular dementia are categorised as ‘dementia’ (chi dai) or ‘stroke’ (zhong feng) in traditional Chinese medicine (TCM). It is suggested they are closely related to dysfunction of the heart, brain and kidney. The principal TCM treatments for VMCI include tonifying the kidney and promoting blood circulation.2
A number of studies3 4 demonstrated that acupuncture techniques that tonify the kidney and nourish the marrow (in PC6, GV20, GB20, etc) may be effective for improving intelligence, stimulating consciousness and enhancing memory. These effects may result from activation and/or stimulation by acupuncture of the regions responsible for cognition and memory. Scalp acupuncture, which involves stimulation of acupuncture points on the surface of the head using acupuncture needles, electroacupuncture or acupuncture with electrical stimulation, is the most commonly used acupuncture technique for vascular mental disease. Some published studies5 6 also demonstrated that acupuncture may be able to promote the proliferation and differentiation of neural stem cells in the brain, accelerate angiogenesis and inhibit apoptosis.
Although acupuncture has been commonly used in clinical practice in China for VMCI for years, no systematic review has been performed to evaluate the effectiveness of acupuncture for the condition. Thus, the aim of the current systematic review is to assess the effectiveness and safety of acupuncture for VMCI.
Methods
Inclusion criteria
Randomised controlled trials (RCTs) that compared acupuncture for the treatment of VMCI (without vascular dementia) to no treatment, placebo or conventional therapy (such as cognitive function training (CFT)) were included. RCTs that evaluated the use of acupuncture as an adjunct to existing conventional therapies for VCI were also included. Outcome measures for cognitive assessment had to include at least one of the internationally recognised scales such as the Mini-Mental State Examination (MMSE), Montreal Cognitive Assessment (MoCA), Modified Barthel Index (MBI), Wechsler Memory Scale (WMS) or similar. There were no limitations on language of publication or publication type.
Identification and selection of studies
We searched the China National Knowledge Infrastructure (1979–2012), Chinese Scientific Journal Database (1989–2012), Wan Fang (Dissertation and Conference Articles) Database (1985–2012), PubMed (1966–2012) and the Cochrane Library (Issue 12, 2012). All searches were completed in December 2012. The search terms included ‘VCI’, ‘VMCI’, ‘vascular dementia’, ‘acupuncture’, ‘meridian’, ‘three edged needle’, ‘triangle-edged needle’, ‘electroacupuncture’, ‘randomised’ and ‘randomisation’. Eligible studies were selected and checked independently by two authors (LZ and HC).
Data extraction and quality assessment
Two authors (HC and YW) independently extracted the data from the selected reports. The extracted data included the author names and title of the study, year of publication, diagnostic criteria, study size, age and sex of the participants, methodological information, type of acupuncture, treatment process, control interventions, outcomes and adverse effects.
The trials included were reviewed and assessed independently by two authors (YW and HC). Quality assessment was conducted according to the ‘risk of bias’ assessment table provided by the Cochrane Handbook for Systematic Reviews of Interventions.7 The following types of bias were assessed: selection bias (random sequence generation and allocation concealment), performance bias (blinding of participants and personnel), detection bias (blinding of outcome assessment), attrition bias (incomplete outcome data), reporting bias (selective reporting) and other bias.
Data analysis
RevMan V.5.1 software was employed for data analysis. Data were summarised using relative risk with 95% CI for binary outcomes or mean difference (MD) with 95% CI for continuous outcomes. Meta-analysis was used if the trials had good homogeneity for study design, participants, interventions, controls and outcome measures. Publication bias was explored by funnel plot analysis.
Results
Description of studies
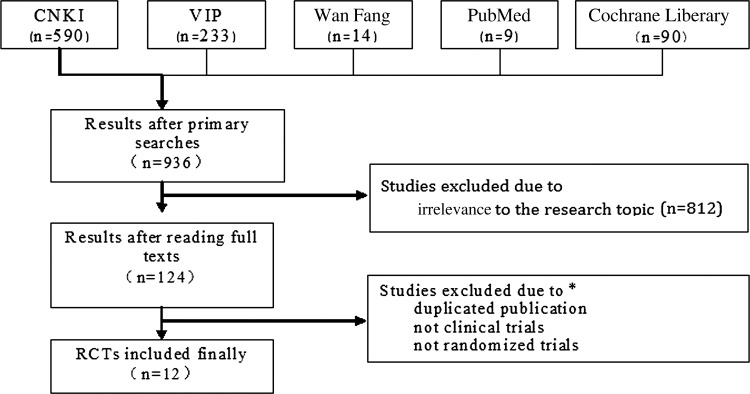
A total of 1223 articles were identified by the initial search and 124 studies with accessible full text were retrieved. However, the majority of these studies did not meet the inclusion criteria and were therefore excluded. Consequently, 12 trials including five publications8–12 and seven unpublished dissertations13–19 were included in this review (figure 1 gives details of the included and excluded studies). The characteristics of the included trials are listed in table 1.
Figure 1.
Details of the included and excluded studies of acupuncture in the treatment of vascular mild cognitive impairment (VMCI). CNKI, China National Knowledge Infrastructure; VIP, Chinese Scientific Journal Database; RCT, randomised controlled trial. *The numbers in each category are not recorded.
Table 1.
Characteristics of RCTs of acupuncture in the treatment of vascular mild cognitive impairment
| Included studies | Participants, male/female | Mean age, years | Diagnostic criteria | Intervention | Duration of treatment, weeks | Outcome measure | |||
|---|---|---|---|---|---|---|---|---|---|
| T | C | T | C | T | C | ||||
| Huang et al (2008)8 | 21/19 | 20/20 | 59.2 | 61 | GC | Body acupuncture, 30 min, daily, 6 times/week, plus CFT | CFT | 4 | MMSE, CDT, BDT |
| Sun and Wu (2011)9 | 24/12 | 25/11 | 63.6 | 64.1 | GC | Scalp acupuncture, 30 min, daily, 6 times/week, plus donepezil 0.25 mg, daily | Donepezil 0.25 mg, daily | 4 | Effective rate, MMSE, MBI |
| Xie et al (2007)10 | 24/17 | 22/17 | 53.0 | 56.5 | GC | Scalp acupuncture, 30 min, daily, 10/course, plus rehabilitation, daily | Rehabilitation, daily | 12 | ERP (P300), WAIS |
| Yu and Han (2007)11 | 16/15 | 17/16 | 67.2 | 67.0 | IC | Body acupuncture, 30 min, daily, 5 times/week | Nimodipine 30 mg, 3 times daily | 12 | MMSE, BBS |
| Yu et al (2007)12 | 14/11 | 15/11 | 63.3 | 57.7 | GC | Body acupuncture, 20–30 min, daily, 5 times/week, nimodipine 30 mg, 3 times daily | Nimodipine 30 mg, 3 times daily | 24 | MMSE, MBI, WMS |
| Jiang (2011)13 | 12/8 | 10/10 | 62.9 | 61.8 | GC | Body acupuncture, 30 min, daily, 7 times/week, plus CFT | CFT, daily, 7 times/week | 8 | ERP (P300), MMSE |
| Kang (2011)14 | 17/17 | 15/9 | 60.7 | 62.7 | GC | Body acupuncture, 30 min, daily, 7 times/week, plus CFT | CFT, daily, 7 times/week | 8 | ERP (P300), MMSE |
| Li (2011)15 | 14/16 | 15/15 | Unavailable | IC | Body acupuncture, 30 min, daily, 6/week, plus donepezil 5 mg, daily | Donepezil 5 mg, daily | 12 | MMSE, MoCA | |
| Yan (2009)16 | 14/16 | 9/21 | 61.8 | 62.9 | IC | Body acupuncture, 30 min, daily, 6 times/week, plus CFT, 5 times/week | Nimodipine 30 mg, 3 times daily, plus CFT, 5 times/week | 12 | MoCA, MMSE, WMS |
| Yang (2011)17 | 11/9 | 10/10 | 59.0 | 59.3 | GC | Scalp acupuncture, 30 min, daily, CFT daily, 7 times/week | CFT daily, 7 times/week | 8 | MMSE, ERP (P300) |
| Yang (2006)18 | 10/8 | 11/7 | 62.3 | 63.8 | GC | Body acupuncture, 30 min, daily, 6 times/week, plus CFT daily | CFT daily | 4 | NCSE, MBI, Fugl-Meyer |
| Zhao (2011)19 | 13/17 | 14/16 | 65.8 | 67.2 | IC | Body acupuncture, 30 min, daily | Enteric-coated aspirin tablets, 100 mg, daily | 12 | MMSE, MoCA |
BBS, Blessed-Roth Behavior Scale; BDT, block design test; C, control; CDT, clock drawing task; CFT, cognitive function training; ERP, event-related potentials; Fugl-Meyer, Fugl-Meyer Assessment of Sensorimotor Recovery after Stroke; GC, government criteria in China; IC, international criteria; MBI, Modified Barthel Index; MMSE, Mini-Mental State Examination; MoCA, Montreal Cognitive Assessment; NCSE, non-convulsive status epilepticus; RCT, randomised controlled trial; T, treatment; WAIS, Wechsler Adult Intelligence Scale; WMS, Wechsler Memory Scale.
A total of 691 participants (average age 61 years old) with VMCI were enrolled in the studies. Time from diagnosis ranged from 22 to 180 days and all trials used Chinese or international diagnostic criteria. The interventions included scalp acupuncture, body acupuncture and electroacupuncture, while the control groups received oral medicine and cognitive rehabilitation. Treatment duration lasted between 28 days and 6 months. All included trials used internationally recognised outcome measures to evaluate cognitive function, including the MMSE, MoCA, MBI and WMS. No trial reported whether adverse events had occurred during the intervention.
Methodological quality
In accordance with the quality evaluation criteria, all included trials clearly described participant characteristics, the study design, the intervention and the controls, and used appropriate methods for statistical analysis. There were 18–40 participants in each group, with an average of 29 patients per group. Sample size calculation was not reported. Eight trials8 11 13–18 described randomisation procedures, including central randomisation and the use of random number tables and computer software. Five trials11 13 14 17 18 used opaque envelopes for allocation concealment. Three trials13 14 17 reported the procedure for blinding the assessor, two17 18 stated that there was no blinding of participants or study personnel, and the other failed to report participant blinding. Four trials13 14 17 18 indicated there were no dropouts, two11 12 reported dropouts, and none used intention to treat analysis. Therefore, with the exception of four trials11 12 17 18 judged to have a high risk of bias, the remaining eight trials were judged to have an unclear risk of bias.
Effect estimates
Table 2 summarises the results from the included studies. Only one meta-analysis was conducted with a forest plot as shown in figure 2.
Table 2.
Summary of the individual studies included in the review
| Included studies | Comparison | No. of patients | Week of assessment | Outcome measure | Results, MD (95% CI) |
|---|---|---|---|---|---|
| Huang (2008)8 | Acupuncture plus CFT vs CFT | 80 | 4 | MMSE | 3.26 (1.69 to 4.83) |
| CDT | 0.61 (0.39 to 0.83) | ||||
| BDT | 3.57 (1.87 to 5.27) | ||||
| Sun and Wu (2011)9 | Acupuncture plus donepezil vs donepezil alone | 72 | 4 | MMSE | 2.01 (0.27 to 3.75) |
| MBI | −3.52 (−6.24 to −0.80) | ||||
| Xie et al (2007)10 | Acupuncture plus rehabilitation vs rehabilitation alone | 80 | 12 | WAIS | 4.90 (0.76 to 9.04) |
| Yu and Han (2007)11 | Acupuncture vs nimodipine | 64 | 12 | MMSE | 2.41 (1.38 to 3.44) |
| BBS | −1.08 (−2.15 to −0.01) | ||||
| Yu et al (2007)12 | Acupuncture plus nimodipine vs nimodipine alone | 51 | 24 | MBI | 10.57 (8.64 to 12.50) |
| WMS | |||||
| Jiang (2011)13 | Acupuncture plus CFT vs CFT alone | 40 | 8 | MMSE | 2.70 (0.71 to 4.69) |
| Kang (2011)14 | Acupuncture plus CFT vs CFT alone | 68 | 8 | MMSE | 0.54 (−0.71 to 1.79) |
| Li (2011)15 | Acupuncture plus donepezil vs donepezil alone | 60 | 12 | MMSE | 1.33 (−0.21 to 2.87) |
| MoCA | 1.37 (−0.21 to 2.95) | ||||
| Yan (2009)16 | Acupuncture plus CFT vs nimodipine plus CFT | 60 | 12 | MMSE | 1.76 (−0.30 to 3.82) |
| MoCA | 1.95 (−1.55 to 5.45) | ||||
| MBI | 7.99 (6.29 to 9.69) | ||||
| WMS | |||||
| Yang (2011)17 | Acupuncture plus CFT vs CFT alone | 40 | 8 | MMSE | 2.65 (0.99 to 4.31) |
| Yang (2006)18 | Acupuncture plus CFT vs CFT alone | 36 | 4 | NCSE | 5.89 (4.00 to 7.78) |
| MBI | 10.73 (6.25 to 15.21) | ||||
| Zhao (2011)19 | Acupuncture vs aspirin | 60 | 12 | MMSE | 1.80 (0.23 to 3.37) |
| MoCA | 2.00 (0.11 to 3.89) |
BBS, Blessed-Roth Behavior Scale; BDT, block design test; CDT, clock drawing task; CFT, cognitive function training; MBI, Modified Barthel Index; MD, mean difference; MMSE, Mini-Mental State Examination; MoCA, Montreal Cognitive Assessment; NCSE, non-convulsive status epilepticus; WAIS, Wechsler Adult Intelligence Scale; WMS, Wechsler Memory Scale.
Figure 2.
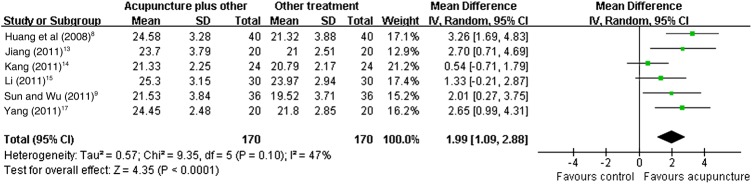
Forest plot of comparison: acupuncture plus other treatment versus other treatment alone. IV, inverse variance.
Acupuncture in conjunction with conventional therapy versus conventional therapy alone
Nine trials8–10 12–15 17 18 compared acupuncture as an adjunct to the existing therapy. Of these, four trials10 13 14 17 compared electroacupuncture in conjunction with CFT to CFT alone, two8 18 assessed body acupuncture in addition to CFT, two12 15 evaluated electroacupuncture in conjunction with pharmaceutical treatment, and one9 assessed body acupuncture in addition to pharmaceutical treatment.
Six trials8 9 13–15 17 reported MMSE scores after treatment. Meta-analysis suggested that acupuncture (MD 1.99, 95% CI 1.09 to 2.88, p<0.0001, 6 trials) in conjunction with CFT/donepezil (0.25 mg daily) improved MMSE scores compared to CFT/donepezil alone.
One trial15 reported cognitive assessment scores using MoCA; however, no significant difference was found between electroacupuncture in combination with donepezil and donepezil alone (MD 1.37, 95% CI −0.21 to 2.95, p=0.09, 1 trial).
Two trials12 18 reported MBI scores. One trial18 suggested that electroacupuncture in combination with CFT was superior to CFT alone (MD 10.73, 95% CI 6.25 to 15.21, p<0.00001, 1 trial), and the other trial12 showed that electroacupuncture in conjunction with nimodipine (90 mg daily) was also superior to nimodipine (90 mg daily) alone (MD 10.57, 95% CI 8.64 to 12.50, p<0.00001, 1 trial).
Acupuncture versus other interventions
Three trials11 12 16 compared acupuncture to oral medicine, including electroacupuncture versus nimodipine (90 mg daily), body acupuncture versus nimodipine (90 mg daily), and body acupuncture versus enteric-coated aspirin tablets (100 mg daily). A significant difference was found in MMSE scores in all three trials (table 2).
Two trials16 19 reported changes in MoCA scores after treatment, and a statistical difference was found between acupuncture (alone or in conjunction with CFT) and nimodipine (in conjunction with CFT, 90 mg daily)/aspirin (100 mg daily) (table 2).
One trial18 reported that electroacupuncture effectively increased MBI scores compared to nimodipine (90 mg daily) (MD 7.99, 95% CI 6.29 to 9.69, p<0.0001, 1 trial).
Adverse events
No trials mentioned whether adverse events had occurred in the treatment or control groups.
Funnel plot analysis
Funnel plot analysis could not be conducted due to the insufficient number of trials (less than 10) in the meta-analysis.
Discussion
Although the meta-analysis in the current review suggests that acupuncture could be effective as an adjunctive treatment with CFT or pharmaceutical therapies for VMCI, this result should be interpreted with caution as most of the trials had small sample sizes and poor methodological quality. Thus, no firm conclusion can be drawn on the efficacy of acupuncture for the treatment of VMCI.
A number of limitations were identified in this review. The overall quality of the studies included in this review was poor. The conclusions of most studies have potential bias due to missing information on randomisation concealment and the blinding procedure, and inappropriate methods for dealing with missing data. Funnel plot analysis could not be conducted due to the insufficient number of trials included in the meta-analysis; however, a high percentage of the trials conducted in China reported positive results, suggesting possible publication bias.
The participants involved in the trials were all diagnosed with MCI due to cerebral infarction, which limits the generalisability of the results. Another limitation was the variety of acupuncture treatments and controls used. Acupuncture techniques ranged from scalp acupuncture and body acupuncture to electroacupuncture, and so the acupuncture points selected differed greatly between studies. Various different controls were used in these studies, which could affect the results of the meta-analysis due to clinical heterogeneity. Although statistical heterogeneity was not demonstrated by the I2 test, variations in study quality, the characteristics of participants, types of interventions and outcome measures indicated some clinical heterogeneity among the included trials.
There are several ways the quality of future acupuncture trials in VMCI could be improved. Although it is difficult to blind practitioners and patients in acupuncture studies, implementation and measurement biases can be minimised if outcome assessors are blinded. Outcome measures used should be of international standard. Data analysis based on the intention-to-treat principle is critical, and clearly defined diagnostic criteria for VMCI should be used to improve comparability between trials. Finally, RCT reports should follow the Consolidated Standards of Reporting Trials (CONSORT) Statement,20 which requires transparent and explicit descriptions of the trial processes.
In conclusion, acupuncture appears to be beneficial for the management of cognitive and memory function in patients with VMCI; however, further rigorously designed clinical investigations with larger sample sizes are needed to confirm the efficacy of acupuncture.
Summary points.
We reviewed the literature on acupuncture for mild cognitive vascular impairment.
Twelve trials were identified, but their quality was too poor to allow conclusions; however, the results justify further studies.
Acknowledgments
The authors would like to thank Ms Yu-ting Sun for her assistance in preparing this manuscript.
Footnotes
Contributors: HC, LZ and YW screened papers for eligibility; HC obtained data on unpublished studies; HC and YW appraised the quality of papers, extracted data and sought additional information on papers, entered data into RevMan and wrote the final draft of the manuscript; HC analysed and interpreted data; HC, LZ, DC and JL worked on the methods section; HC, LZ and JL drafted the clinical sections and responded to the clinical comments of the reviewers; HC, DC and JL responded to the methodology and statistics comments of the reviewers.
Funding: JL and HC are supported by a research capacity establishment grant from Beijing University of Chinese Medicine (number 2011-CXTD-09 and 201207007).
Competing interests: None.
Ethics approval: All trials included in our review were approved by the appropriate ethics committees.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Jia JP. Pay attention to the early diagnosis and intervention of vascular cognitive impairment. Zhonghua Shen Jing Ge Za Zhi 2005;38:4–6 [Google Scholar]
- 2.Wang YY, Zhang BL. Chinese medicine of brain disease. Beijing: People's Medical Publishing House, 2007:26 [Google Scholar]
- 3.Han HY, Yin H, Zhou YL, et al. Investigation on the changes of dependent signal on the amplitude of low frequency fluctuations at blood oxygen level in brain after acupuncture Neiguan (PC 6). Zhongguo Zhen Jiu 2009;29:647–51 [PubMed] [Google Scholar]
- 4.Zhu XT, Feng TJ, Zheng L, et al. Influences of acupuncture with effects of awakening consciousness and improving intelligence in group acupoints on brain resting state function. J Beijing Univ Tradit Chin Med 2011;34:181–5 [Google Scholar]
- 5.Fang JL, Hong Y, Wang XL, et al. Electroacupuncture at Guanyuan(CV 4) and Zhongwan(CV 12) modulates functional connectivity of the brain network in healthy volunteers. Zhen Ci Yan Jiu 2011;36:366–72 [PubMed] [Google Scholar]
- 6.Yang ZX, Chen PD, Yu HB, et al. Research advances in treatment of cerebral ischemic injury by acupuncture of conception and governor vessels to promote nerve regeneration. Zhong Xi Yi Jie He Xue Bao 2012;10:19–24 [DOI] [PubMed] [Google Scholar]
- 7.Higgins JPT, Green S. eds 2011. Cochrane handbook for systematic reviews of interventions version 5.1.0. The Cochrane collaboration. http://www.cochrane-handbook.org (accessed 20 Jan 2013).
- 8.Huang F, Liu Y, Zhou FX. The influence of acupuncture in vascular cognitive impairment after cerebral infarction. Guangdong Med J 2008;29:1918–20 [Google Scholar]
- 9.Sun YZ, Wu WP. 36 cases for cluster needling of scalp point therapy in cognitive function impairment after ischemic stroke. Zhongguo Zhen Jiu 2011;27:11–13 [Google Scholar]
- 10.Xie DL, Zhu LF, Liu HY. Effect of scalp acupuncture for cognitive function in patients with stroke in convalescence stage. Chin J Rehabil Med 2007;22:834–5 [Google Scholar]
- 11.Yu T, Han JX. 31 cases for acupuncture in vascular cognitive impairment with no dementia. Shanxi J Tradit Chin Med 2007;28:726–8 [Google Scholar]
- 12.Yu XG, Sun SL, Chen YH. Clinical observation on acupuncture in points of governor vessel for mild cognitive impairment after ischemic stroke. Chin J Integr Med Cardio/Cerebrovasc Dis 2007;5:1171–3 [Google Scholar]
- 13.Jiang YJ. Electroacupuncture DU20 and DU24 treatment on cognitive impairment after stroke. [dissertation] Fujian: Fujian University of Traditional Chinese Medicine, 2011 [Google Scholar]
- 14.Kang JJ. Clinical study of effect of electroacupuncture on GV20 and EX-HN1 on stroke patients with cognitive impairment. [dissertation] Fujian: Fujian University of Traditional Chinese Medicine, 2011 [Google Scholar]
- 15.Li M. Electro-nape acupuncture and donepezil due to vascular cognitive impairment after cerebral infarction clinical research. [dissertation] Heilongjiang: Heilongjiang University of Traditional Chinese Medicine, 2011 [Google Scholar]
- 16.Yan HD. Observation on therapeutic effect of kidney supplementing & mind clearing acupuncture method combined with cognitive training on cerebral arterial thrombosis patients with mild cognitive impairment. [dissertation] Guangzhou: Guangzhou University of Traditional Chinese Medicine, 2009 [Google Scholar]
- 17.Yang J. The clinical study of cognitive impairment after stroke by using the treatment of electroacupuncture given at Du20 and GB20. [dissertation] Fujian: Fujian University of Traditional Chinese Medicine, 2011 [Google Scholar]
- 18.Yang SL. Effects of needling combined with cognitive function training on the cognitive function of stroke patients. [dissertation] Fujian: Fujian University of Traditional Chinese Medicine, 2006 [Google Scholar]
- 19.Zhao ZX. Acupuncture point limbs less yin meridians specific treatment after stroke study of mind cognitive dysfunction. [dissertation] Heilongjiang: Heilongjiang University of Traditional Chinese Medicine, 2011 [Google Scholar]
- 20.CONSORT Statement 2001-Checklist: items to include when reporting a randomized trial. http://www.consort-statement.org