Abstract
Changes in mental health symptoms throughout pregnancy and postpartum may impact a woman’s experience and adjustment during an important time. However, few studies have investigated these changes throughout the perinatal period, particularly changes in posttraumatic stress disorder (PTSD) symptoms. The purpose of this study was to examine longitudinal changes in PTSD, depression, and anxiety symptomatology during pregnancy and postpartum. Pregnant women of ethnically diverse backgrounds receiving services for prenatal care at an outpatient obstetric-gynecology clinic or private physicians’ office were assessed by interview on symptoms of PTSD, depression, anxiety, and general stress up to four times, including their first, second, and third trimester, and postpartum visits. Overall, during pregnancy there was a declining trend of PTSD symptoms. For anxiety, there was no overall significant change over time, however anxiety symptoms were individually variable in the rate of change. For both depression and general stress symptoms there was a declining trend, which was also variable in the individual rate of change among women during their pregnancy. Visual and post-hoc analyses also suggest a possible peak in PTSD symptoms in the weeks prior to delivery. While most mental health symptoms may generally decrease during pregnancy, given the individual variability among women in the rate of change in symptoms, screening and monitoring of symptom fluctuations throughout the course of pregnancy may be needed. Further studies are needed to examine potential spiking of symptoms in the perinatal period.
Keywords: Perinatal, PTSD, mental health, symptomatology, longitudinal
Introduction
Pregnancy and childbirth are significant events, whereby major physiological, psychological, and social changes can contribute as stressors in a woman’s life and act as significant risk factors in the development or exacerbation of mental health issues (Apter et al. 2011). Mental health problems during the perinatal period may impact adjustment during pregnancy and the postpartum period. Furthermore, mental health disorders during the perinatal period are associated with inadequate prenatal and pediatric care as well as numerous adverse outcomes for the offspring (Vesga-Lopez et al. 2008).
Perinatal PTSD and other mental health disorders
The most commonly recognized mental health disorders during the perinatal period are depression and anxiety, with systematic study reviews reporting estimated prevalence ranging from 6.5% to 12.8% for depression or depressive symptoms (Bennett et al. 2004; Gavin et al. 2005), and other studies reporting prevalence ranging from 13% to 16.3% for anxiety disorders or symptoms (Heron et al. 2004; Smith et al. 2004; Wenzel et al. 2005). More recently, posttraumatic stress disorder (PTSD) has also begun to emerge as a significant mental health concern during pregnancy and postpartum (Seng et al. 2010).
For women, the estimated occurrence of lifetime PTSD ranges from 9.7% to 20.2% (Kessler et al. 2005; Resnick et al. 1993; Seng et al. 2009) and from 4.6% to 5.2% for current PTSD (Kessler et al. 2005; Resnick et al. 1993). A majority of the traumatic events underlying PTSD symptoms in women often involve interpersonal violence such as physical assault, childhood sexual abuse, sexual assault, or intimate partner violence (Bruce et al. 2001).
There is a growing body of research in PTSD related to childbirth and perinatal complications (Alcorn et al. 2010; Ayers et al. 2009; Forray et al. 2009; Maggioni et al. 2006), recognizing that prior reproductive trauma may increase a woman’s risk for the re-emergence of PTSD symptoms and other mental health problems during the perinatal period (Born et al. 2006). However, it is also known that many women experience traumatic events well before their childbearing years and may enter pregnancy with mental health problems, including PTSD (Goebert et al. 2007; Mezey et al. 2005; Morland et al. 2007; Rodríguez et al. 2010; Yampolsky et al. 2010), which may be undiagnosed or untreated.
There is less known about the prevalence of PTSD during the perinatal period, although some studies have shown that 7.7% to 7.9% of women have PTSD during pregnancy (Loveland Cook et al. 2004; Seng et al. 2009) and 3.6% to 6.3% of women may have postpartum PTSD (Alcorn et al. 2010). PTSD has been seen to co-occur with depression and other anxiety disorders during the perinatal period (Cerulli et al. 2011; Loveland Cook et al. 2004; Smith et al. 2006).
Subclinical levels of PTSD, depression, and other anxiety symptoms have also been shown to be distressing for expectant mothers, diminishing the experience of pregnancy and potentially influencing maternal-child bonding and attachment (Ayers et al. 2006). In particular, symptoms of PTSD expressed at a subclinical level have been suggested to be related to the same problems as classic PTSD such as comorbid mental health problems, high risk behaviors such as depression and alcohol use (Yarvis and Schiess 2008) and clinically meaningful levels of functional impairment (Stein et al. 1997). Mental health concerns, such as traumatic stress and PTSD during pregnancy, may in turn have consequences on fetal development or birth outcomes (Alder et al. 2007; Dunkel Schetter and Tanner 2012; Federenko and Wadhwa 2004; Littleton et al. 2007; Morland et al. 2007; Rogal et al. 2007; Rosen et al. 2007; Seng 2002; Seng et al. 2001; Wadhwa et al. 2001) and infant and child development (Brand and Brennan 2009; Koubovec et al. 2005; Monk 2001; Van den Bergh et al. 2005)).
Changes in Symptomatology during Pregnancy and Postpartum
Although perinatal studies have examined discrete changes in symptomatology from pregnancy to postpartum, relatively fewer published studies have prospectively investigated the longitudinal fluctuations of mental health symptoms during the perinatal period (Brooks et al. 2009; Evans et al. 2001; Glynn et al. 2008; Heron et al. 2004; Ross and McLean 2006; van Bussel et al. 2009). Moreover, we were unable to find studies specifically measuring longitudinal PTSD symptoms changes throughout the perinatal period from early pregnancy through postpartum. This study seeks to fill this gap by prospective examination of longitudinal changes in PTSD, depression, and anxiety symptomatology during pregnancy and postpartum. Further, given that perinatal studies often lack inclusion of women from underrepresented ethnic populations, such as Asians and Pacific Islanders, this study also adds to our knowledge by examining these longitudinal changes in mental health symptomatology in a sample of ethnically diverse pregnant women.
Materials and Methods
Participants
Data are presented from a longitudinal study of perinatal behavioral health among women on Oahu, Hawai‘i (Goebert et al. 2007), that was approved by the local Institutional Review Board and conducted over a period of 4 years (2002–2006). One hundred and nineteen women were assessed on one or more of four occasions during the course of their pregnancies: (1) at their initial prenatal visit, which was usually during the first trimester; (2) during the second trimester; (3) during the third trimester; and (4) at postpartum. Women who met the following inclusion criteria were invited to participate in this study: (1) English speaking, (2) 18–35 years of age, and (3) presenting for their initial prenatal care visit at one of three outpatient obstetric-gynecology (ob/gyn) clinics or private physicians’ offices associated with a local community medical center specializing in the care of women and children on Oahu, Hawai‘i. Of 159 eligible women invited to join the study, the participation rate was 75%.
Procedures
All participants provided written informed consent prior to study enrollment. Participants were interviewed in a private area of the waiting room of the clinic or physician’s office during their prenatal and postpartum visits. The interview was conducted in English and lasted approximately 30 minutes. The interview at the initial screening included questions for the following: demographic information (age, ethnicity, marital status, education, and household income); substance use (alcohol, smoking, and other illicit drug use); general stress; history of trauma; symptomatology for PTSD, anxiety, and depression; and social support. During subsequent trimester and postpartum visits, the interview was repeated using a shorter questionnaire that lasted approximately 20 minutes. Participants were compensated with a $5 gift certificate to a local retailer for each trimester interview including the initial screening interview and a $10 gift certificate for the postpartum interview. The assessment measures that were collected during the interview and are the focus for the statistical analyses conducted in this study are described below.
Trauma and PTSD Symptoms
The Traumatic Life Events Questionnaire (TLEQ; Kubany et al. 2000) was used to assess the various types of trauma that women had experienced during their lifetime, including interim trauma during pregnancy and postpartum. Categories of trauma included interpersonal violence such as domestic abuse, sexual assault, and child abuse. The TLEQ also assessed the participants’ helplessness or horror in response to the endorsed trauma exposure and the event which caused the most distress.
Current PTSD symptoms related to the reported trauma exposure were measured using the PTSD Checklist - Civilian version (PCL-C; Weathers et al. 1994). Item responses, reflecting a range of symptom intensity, were used to calculate a total clinical symptomatology score. Cut off scores vary depending on the prevalence of PTSD in the target setting, with typical scores ranging from 40–50 in specialty mental health clinics to 30–35 in civilian primary care or active duty population screening (Blanchard et al. 1996; Bliese et al. 2008; Freedy et al. 2010). PCL-C items that measured re-experiencing, avoidance, and hyper-arousal symptoms based on the criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association 1994) were also used to determine PTSD status.
Depressive Symptoms
The Center for Epidemiologic Studies Depression Scale (CES-D; Radloff 1977), a 20-item self-report screening instrument, was used to measure symptoms of depression in the previous 7 days. The CES-D has been used as a screening instrument for depression (score of 16 or higher) in women during and after pregnancy (Marcus et al. 2003; Mosack and Shore 2006).
Anxiety
Levels of state anxiety at each assessment were measured using the 20-item State-Trait Anxiety Inventory (STAI; Spielberger et al. 1983). The STAI is the most widely used self-report measure of anxiety in adults. Cutoff scores of 40 or higher were considered to screen positive and be at risk for an anxiety disorder (Rondo et al. 2004).
General Stress
General stress was measured using a short 10-item version of the Perceived Stress Scale (PSS; Cohen et al. 1983). The self-report items ask respondents to appraise general and nonspecific distress.
Analyses
Data were organized into the number of weeks since the start of pregnancy, which follows the general convention of a trimester and postpartum calendar, and then further classified as follows: (1) early (0–6.9 weeks) and late (7–13.9 weeks) first trimester; (2) early (14–21.9 weeks) and late (22–27.9 weeks) second trimester, (3) early (28–32.9 weeks), middle (33–36.9 weeks), and late (37–40+ weeks) third trimester, (4) early postpartum (within 6 weeks after delivery), and (5) later postpartum (more than 6 weeks after delivery). Start of pregnancy was determined by subtracting the weeks of gestational age from the delivery date from available labor and delivery records, or by self-reported last menstrual period.
To examine potential differences among women from the different recruitment sites, dichotomous variables were created for depression and anxiety risk, based on cut-off criteria indicating risk for diagnosis. A dichotomous variable for current PTSD status was also created, using the corresponding PCL symptoms matching the DSM-IV diagnostic criteria for full PTSD or for symptoms in the subclinical PTSD range, which has been shown to have similar levels of impairment or relationship to associated mental health and behavioral risk factors (Breslau et al. 2004; Manne et al. 1998; Morland et al. 2007; Stein et al. 1997; Yarvis and Schiess 2008). Subclinical PTSD was defined as meeting the required number of symptoms for each of the categories of PTSD, but with a lesser intensity (Morland et al. 2007).
To determine appropriateness of the symptom measures for our sample of ethnically diverse women, Cronbach’s alpha internal consistency analyses were performed.
For the main analyses, total symptom scores for PTSD, depression, other anxiety, and stress were included for longitudinal analyses. Composite scores for subcategories of PTSD symptoms were calculated from PCL-C items (Weathers et al. 1994) into DSM-IV criteria for re-experiencing (Criterion B), avoidance (Criterion C), and arousal (Criterion D) symptoms.
Descriptive and inferential analyses using PASW Statistics 18.0 software were used to examine sociodemographic characteristics including age, education, ethnicity, marital status, socioeconomic level, and clinic site. To assess increases or decreases in scores within individual women, mixed-effects regression analyses were conducted using STATA (v11) to examine longitudinal changes in PTSD symptoms and other mental health problems, including depressive symptoms, additional symptoms of anxiety, and stress. In mixed effects regression, the fixed effects represent the mean impact of a predictor, weighted for each individual based on the number of observations and variance for the specific individual. Therefore, the fixed effect of time examined the mean change in our outcomes (PTSD, depression, and anxiety symptom scores) across all women. Mixed effects regression also has a random effects component. The random component of time was examined to determine whether the change in outcomes (PTSD, depression, and anxiety symptom scores) differs across the individual women.
Results
There were significant differences in age, education level, marital status, ethnic breakdown, and annual household income level across the three clinic recruitment sites. However, these differences were expected due to purposive sampling for ethnic and socioeconomic diversity. The overall mean age at first interview across the clinics was 27.2 years (SD=4.8), with a range of 18–35 years. Approximately 36% of women were high school educated, 34% had some college education, 14% had a college degree, and almost 16% had postgraduate education. Fifty-seven percent of women were married, while 43% were single, separated, or divorced. The sample was overrepresented for Asian (39.8%) and Native Hawaiian/Pacific Islander (38.1%), and underrepresented for Caucasian (20.4%) and Other (1.8%) ethnic groups. Annual household incomes were distributed as follows: $41,000 or higher (53.2%), $31,000-$40,000 (11.4%), $21,000-$30,000 (10.1%), and $20,000 or less (25.3%). Although the prevalence of PTSD (18.8%, 23.3%, 5.9%, respectively for three sites; n=109; χ2=4.321; df=2; p=0.115) and depression (30.3%, 52.3%, 31.4% respectively for three sites; n=112; χ2=5.134; df=2; p=0.077) at the initial assessment did appear to differ between the three sites, the differences were not statistically significant. For the remaining longitudinal analyses of mental health symptomatology, the data were analyzed as a single sample, representing a wide spread in mental health.
Internal consistency reliability Cronbach’s alpha statistics for the symptom measures verified that the instruments are performing adequately for our sample. The Cronbach’s coefficient alpha for raw and standardized scores as a function of assessment occasions (trimesters/postpartum) ranged as follows: 1) CESD raw (.84–.92), standardized (.87–.93); 2) PCL-C raw (.88–.95), standardized (.89–.95); 3) PSS raw (.88–.91), standardized (.88–.91); and 4) STAI raw (.88–.92), standardized (.88–.92).
Mental health symptom scores across pregnancy and postpartum yielded 260 observations for PTSD (PCL-C) from 97 women, 260 observations for depression (CESD) from 97 women, 264 observations for anxiety (STAI) from 98 women, and 264 observations for general stress (PSS) from 98 women. These represented between one to four scores per woman, as each woman could have as many as four observations – one for each pregnancy trimester, as well as a postpartum observation. Mean total scores on the measures of mental health symptomatology are presented in Table 1.
Table 1.
Mean total symptom scores for PTSD, anxiety, depression, and general stress across pregnancy and postpartum
| Weeks of pregnancy | N | PTSD (Mean PCL) | Anxiety (Mean STAI) | Depression (Mean CESD) | General Stress (Mean PSS) | |
|---|---|---|---|---|---|---|
| 1st Trimester | 0–6.9 | 2 | 17.00 | 31.00 | 6.50 | 14.00 |
| 7–13.9 | 47 | 27.74 | 31.98 | 13.98 | 15.08 | |
| 2nd Trimester | 14–21.9 | 58 | 27.95 | 32.54 | 13.71 | 15.39 |
| 22–27.9 | 35 | 26.11 | 33.31 | 12.14 | 13.64 | |
| 3rd Trimester | 28–32.9 | 30 | 27.40 | 34.00 | 13.07 | 14.77 |
| 33–36.9 | 32 | 25.19 | 33.39 | 11.45 | 13.00 | |
| 37–40.9 | 8 | 31.75 | 35.63 | 15.25 | 17.25 | |
| Postpartum | <6 wks | 21 | 24.10 | 30.85 | 10.67 | 12.14 |
| 6+ wks | 27 | 26.11 | 34.89 | 11.31 | 14.26 | |
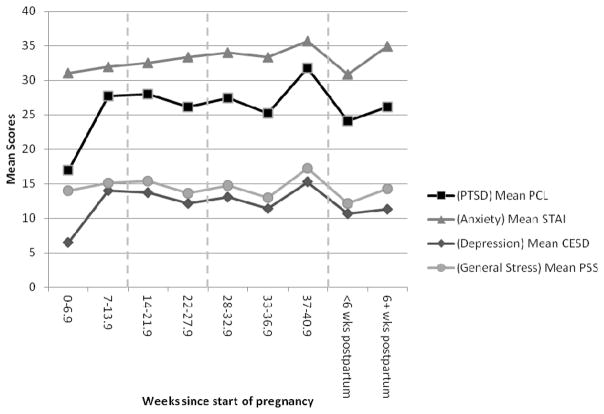
Figure 1 depicts the mean total scores on the measures of mental health symptomatology results plotted across weeks since the start of pregnancy. A visual peak in total scores for PTSD, anxiety, depression, and general stress symptoms was seen in the late third trimester followed by a decrease in symptoms in early postpartum.
Fig. 1.
Mean total scores for symptoms of PTSD, anxiety, depression, and general stress across pregnancy and postpartum
Results of Regression Models
A visual examination of the data made it apparent that scores between 7 weeks of pregnancy and <6 weeks postpartum may have linear trends that were not evident in the earliest pregnancy period or late postpartum period. We therefore restricted our regression analyses to observations measured between 7 weeks of pregnancy and <6 weeks postpartum, however, a comparative set of models were also fitted using all observations. Results of both sets of regression models for examining the trend of mental health symptoms across time among pregnant women are summarized below (Table 2). With one exception noted in the anxiety findings, both models produced similar pattern of results, therefore we have focused the findings for each of the mental health symptom measures to the models fitted using observations from 7 weeks pregnancy to <6 weeks postpartum.
Table 2.
Summary table of mixed linear regression models for symptom scores of PTSD, anxiety, depression, and general stress as a function of weeks since start of pregnancy. Two sets of models were fit using all observations versus using observations between 7 weeks pregnancy and <6 weeks postpartum.
| Models including all observations | Models including observations between 7 weeks pregnancy to <6 weeks postpartum | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| PTSD (PCL) | Anxiety (STAI) | Depression (CESD) | General Stress (PSS) | PTSD (PCL) | Anxiety (STAI) | Depression (CESD) | General Stress (PSS) | |
| Fixed Parameter | ||||||||
| Intercept [95% CI] | 30.01* [26.44, 33.58] P<.0001 |
33.14* [30.47, 35.80] P<.0001 |
16.27* [13.23, 19.31] P<.0001 |
17.10* [15.06, 19.15] P<.0001 |
30.46* [27.11, 33.81] P<.0001 |
32.27* [29.61, 34.94] P<.0001 |
16.24* [13.55, 18.94] P<.0001 |
17.01* [15.15, 18.87] P<.0001 |
| Time effect (week) [95% CI] | −.08* [−.16, −.01] p=.022 |
.01 [−.06, .09] p=.693 |
−.11* [−.19, − .03] p=.005 |
−.09* [−.15, −.03] p=.005 |
−.10* [−.20, −.01] p=.031 |
.06 [−.04, .15] p=.266 |
−.11* [−.20, − .03] p=.011 |
−.08* [−.15, −.02] p=.012 |
| Random Parameter | ||||||||
| S.D. of Intercept | 14.40* | 8.58* | 11.71* | 7.41* | 11.31* | 6.89* | 8.13* | 5.42* |
| S.D. of Time effect (week) | .15 | .13 | .22* | .17* | 1.28e-09 | .19* | .12* | .11* |
significant at .05 level
PTSD Symptoms
For PTSD outcomes using PCL scores, the average estimated score at the beginning of pregnancy (the intercept) was 30.46, and decreased by 0.10 per week (p=0.031). While there was statistically significant variability in the intercept (SD=11.31, p<0.001), the decrease in PCL score over time had little variability across women (SD=1.28e-09). This means that while women varied in their PCL level, with some women having generally high PCL scores and others low scores, individual changes in score throughout pregnancy were remarkably similar.
Anxiety
For anxiety levels, the average STAI score at the beginning of pregnancy (intercept) was estimated to be 32.27, but was found to vary significantly across pregnant women (SD=6.89, p<0.001). The mean individual change in STAI was not significantly different from 0 (0.06, p=0.266), but there was variability among the pregnant women in this change (SD=0.19, p<0.001). That is, some women experienced increases in STAI score through pregnancy and postpartum, while others experienced declines.
Depressive Symptoms
For depression outcomes, the average CESD score at the beginning of pregnancy (intercept) was estimated to be 16.24, but was found to be significantly variable among pregnant women (SD=8.13, p<0.001). On average, depressive symptom scores decreased 0.11 points per week of pregnancy and postpartum, but the variability of the declining trend was statistically significant (SD=0.12, p<0.05). This means that, while for most women CESD declined and this mean decline was statistically significant, for some women CESD actually rose and this difference in the changing CESD across women was also statistically significant.
General Stress
For general stress outcomes, using PSS scores, the average score at the beginning of pregnancy (intercept) was estimated to be 17.01. Like the other mental health scores, however, the PSS score was also found to be significantly variable among pregnant women (SD=5.42, p<0.001). On average, stress scores decreased by 0.083 per week (p=0.012), but the variability of this trend was also statistically significant (SD=0.11 p<0.001), meaning that for some women PSS rose.
Other Post-hoc Analyses
As seen in Figure 1, there appeared to be a peak period of symptom scores during the late third trimester (weeks 37–40 or prior to delivery). Therefore, although our subsequent analysis cannot be used to confirm that the peak we saw would likely be evident in a repeat study with a different population, we did conduct a hypothesis generating post-hoc analysis. We assessed the mean differences between the peak period and surrounding non-peak periods (weeks 33–36.9 and <6 weeks postpartum) for symptoms of PTSD, anxiety, depression, and general stress.
As shown in Table 3, when comparing the peak period at weeks 37–40.9 to the surrounding time periods (weeks 33–36.9 and <6 weeks postpartum), there were differences in mean PTSD as well as mean general stress symptom scores. In our population, symptoms of PTSD and general stress were significantly higher in the late third trimester just prior to delivery compared to before or after this time period. The mean scores of anxiety and depressive symptoms were also higher during the late third trimester, but the differences for these two mental health measures in our population were not statistically significant. Further, because PTSD showed a significant peak of symptom scores during the late third trimester, an additional post-hoc analysis for the subcategories of PTSD symptom clusters was performed to examine if re-experiencing, avoidance, or arousal symptoms showed similar peak symptoms during the period before delivery (data not shown in tables). Although the mean score on all three subcategories was higher during the late third trimester period, the difference in scores was only statistically significant for the PTSD subcategory of re-experiencing symptoms. The mean re-experiencing score was 2.41 higher during the late third trimester than during the surrounding periods, with mean scores of 8.75 and 6.34 respectively (t(59)=−2.40, p=0.020). Mean scores for avoidance were 12.75 during late third trimester and 10.24 during surrounding periods (t(60)=−1.38, p=0.172), while mean scores for arousal symptoms were 10.25 during late third trimester and 8.11 during surrounding periods (t(60)=−1.40, p=0.168).
Table 3.
Summary table of mean differences between peak period and surrounding (non-peak) periods for symptom scores of PTSD, anxiety, depression, and general stress
| PTSD (PCL) | Anxiety (STAI) | Depression (CESD) | General Stress (PSS) | |
|---|---|---|---|---|
| Non-peak period1 | 24.75 | 32.43 | 11.15 | 12.67 |
| Peak period2 | 31.75 | 35.63 | 15.25 | 17.25 |
| Difference | −7.00* | −3.20 | −4.10 | −4.58* |
| t-test | −1.79 | −.98 | −1.29 | −2.02 |
| p-value | .040 | .166 | .100 | .024 |
Weeks 33–36.9 of pregnancy and <6 weeks postpartum
Weeks 37–40.9 of pregnancy
For the postpartum period, comparison of mean differences from early (< 6 weeks) to later (6 weeks or more) postpartum revealed that for all mental health scores the mean was higher in later postpartum than in early postpartum. However, this difference was not statistically significant for any of the scores. The mean difference for PTSD was 2.02 (t(46)=−0.86, p=0.400), for anxiety it was 4.04 (t(45)=−1.45, p=0.154), for depression it was 0.64 (t(45)=−0.23, p=0.818), and for general stress it was 2.12 (t(46)=−0.92, p=0.361).
We also examined the effect of new trauma exposure during pregnancy (from the second trimester), the linear time effect, and a measure to assess whether the level of PTSD, anxiety, or depression changes course during pregnancy (e.g., rises and then falls, falls and then rises, or perhaps rises/falls and then flattens). This measure was assessed through our non-linear quadratic time effect on symptomatology of PTSD, anxiety, depression, and general stress using a mixed effects regression model. We found a statistically significant effect of new trauma exposure for PTSD and depression, but not for anxiety or general stress (see Table 4). Neither the linear nor quadratic effect of time was significant. However, for each additional exposure to a traumatic event, scores increased by 2.40 for PTSD symptoms and 2.07 for depression, controlling for time during pregnancy starting from the second trimester.
Table 4.
Summary table of multiple regression analyses for symptoms scores of PTSD, anxiety, depression, and general stress from linear effect of new trauma exposure, time of pregnancy, and the quadratic time effect
| PTSD (PCL) | Anxiety (STAI) | Depression (CESD) | General Stress (PSS) | |
|---|---|---|---|---|
| Intercept | 25.59* | 32.60* | 13.85* | 14.12* |
|
|
||||
| New Trauma Exposure Effect | 2.40* | 1.32 | 2.07* | 1.03 |
| Time Effect (weeks) | −0.09 | −0.12 | −0.21 | −0.10 |
| Time2 Quadratic Effect | .0012 | .0023 | .0027 | .0016 |
|
| ||||
| R2 | 0.05 | 0.05 | 0.05 | 0.04 |
| F | F(3,78) = 3.26 | F(3,79) = 5.37 | F(3,78) = 3.76 | F(3,79) = 2.17 |
| p | 0.026 | 0.002 | 0.014 | 0.099 |
significant at .05 level
Discussion
Overall, we found that during pregnancy there was a general declining trend in PTSD symptom scores, which was homogenous. However, for other mental health conditions (i.e., anxiety, depression, general stress), there was variability in the way in which symptoms changed among women throughout their pregnancy. Overall, anxiety symptoms appeared to be stable throughout pregnancy; however, there was individual variability in the rate of change. For both depression and general stress, there was a declining trend, which was also variable in the individual rate of change among women during their pregnancy. These findings may be similar to those found by Heron et al. (2004) in a large community sample of pregnant women in England, where self-reported depression and anxiety were found to be relatively stable, with a mean decrease in both depression and anxiety over time. Vesga-Lopez and colleagues found rates of the most common psychiatric disorders to be lower for pregnant women than for non-pregnant women, with the exception of postpartum depression (Vesga-Lopez et al. 2008).
In this study, in addition to exploring trends in PTSD, depression, and anxiety among all women, we also conducted post-hoc analyses after a visual inspection of the data. Results of these analyses properly describe our population and should be followed in future studies to assess whether our findings might describe other populations as well. Although found in post-hoc analyses and any interpretation must be made with caution, there was a significant “spike” in symptoms of PTSD and general stress in the late third trimester (weeks just prior to delivery) that subsided in the postpartum period; however, there were no significant differences in symptoms from early to later postpartum.
We also found that new trauma exposure during pregnancy was associated with PTSD and depression symptomatology in a dose-response relationship, where each additional traumatic event increases the PTSD symptom scores by 2.4 and depressive symptom scores by 2.07. Other researchers have also found this relationship between trauma exposure, PTSD, and depression, as well as symptom severity (Breslau et al. 2000; Dennis et al. 2009). There was no significant effect of new trauma exposure for anxiety or general stress. This post-hoc finding may be cautiously interpreted to suggest that new trauma exposure accounts for the temporal changes in PTSD and depression better than weeks of pregnancy. However, the effect of new trauma exposure, linear time and quadratic time effects only accounted for 5% of the variability in PTSD. It may also be possible that cumulative prior trauma is as equally important. As expected, a large proportion of women (92%) had a history of exposure to traumatic events entering into pregnancy. Over a quarter of the sample had either a single (11.2%) or comorbid probable diagnosis (14.9%) for a mental health disorder, with 2.8% having PTSD-only and 11.1% having some co-occurring combination of PTSD with depression, anxiety, or both. It is noted that all but one of the women with a probable mental health disorder had a history of at least one traumatic event in their life.
Although it is plausible that the interim trauma exposure may explain some variance in the finding of the pre-delivery “spike,” an increase in intrusive re-experiencing symptoms can also indicate the presence of triggers. Furthermore, biological changes associated with stress have been found to increase during the third trimester. For example, Hung et al (2010) found that all oxidative stress markers, such as urinary 8-hydroxydeoxyguanosine, and erythrocyte glutathione peroxidase, were increased in the third trimester, returning to pre-pregnancy levels during the postpartum period. Qualitative research examining women’s experiences during pregnancy may also be useful for understanding this peak. Many qualitative studies have explored the birth and/or postpartum period, with less exploration of the pre-birth period. More qualitative research is needed to explore a variety of aspects of pregnancy (e.g., fear of delivery, concerns about the health and well-being of her baby, worries about parenting) and maternity care (e.g., one’s own health and survival in pregnancy and delivery, level of control in medical decision-making, intrusive examinations, lack of alternatives to hospital birth). Such worries may provoke exacerbation of PTSD symptoms in the third trimester for affected women. Furthermore, as higher stress is associated with adverse obstetric outcomes, preventing spiking of symptoms in the pre-delivery period may be beneficial not only for the woman, but also for fetal health.
The increase in symptoms six weeks postpartum may be attributed to a perceived or real change in social support. Soderquist et al (2006) found that women with post-traumatic stress postpartum showed a decrease in perceived social support. In the early postpartum period, given the contact with health professionals such as physicians, nurses, lactation consultants as well as the excitement of welcoming a newborn into the family, perhaps mothers feel well-supported. With time, there may be fewer visitors and more expectations for the mother to manage on her own. Other contributing factors which have been suggested by past studies include a high level of obstetric intervention, postpartum depressive symptoms, limited breastfeeding, and anxiety during pregnancy (Beck et al. 2011; Zaers et al. 2008).
Conclusion
While it is natural to clinically conceptualize pregnancy and the postpartum period within a time-based framework, relatively few studies have explored this aspect of temporality in mental health symptoms throughout the perinatal period. In light of the literature that suggests mental health symptoms during pregnancy may be useful predictors of postpartum depression or other mental health problems (Homish et al. 2004; Onoye et al. 2009; Zelkowitz et al. 2008), screening and monitoring symptom fluctuations for stability or change throughout the course of pregnancy may be needed for some women, with particular attention to potential exacerbation of symptoms in the third trimester before delivery. Good clinical practice also often involves monitoring symptomatology for patient progress in determining response to treatment or if improvement is clinically meaningful.
Further, some of the research on perceived stress and physiological correlates, such as cortisol, have shed light on the temporal effects of prenatal stress on pregnancy and birth outcomes (Class et al. 2011) and fetal development (Rothenberger et al. 2011; Tollenaar et al. 2010). These research areas should be extended to link more closely with mental health symptom measures of depression (Yim et al. 2009), anxiety (Azar and Singer 2012; Hosseini et al. 2009), and PTSD (Seng et al. 2011b) across the entire course of pregnancy. Finally, given existing disparities in interpersonal trauma exposure, PTSD and other mental health issues of ethnic minority women (Seng et al. 2011a; Seng et al. 2011b), careful considerations for screening and intervention may be warranted in high risk clinical settings.
Strengths and Limitations
There are several strengths and limitations to the study. This is one of relatively few studies that includes an ethnically diverse sample of pregnant women. Further, this study contributes to the gap in the literature which aims to understand the pattern and changes in mental health symptomatology throughout pregnancy using a statistical approach, which allows for analysis of individual variation and change; moreover, to our knowledge, it is the first to specifically and prospectively examine PTSD symptomatology longitudinally throughout the entire course of pregnancy and postpartum. However, the generalizability of these findings is limited by the small sample size, including the relatively small number of observations for some time periods during pregnancy. There is also a potential for errors in interpretation due to the nature of multiple tests within the small sample size. Also, due to practical considerations for administering the instruments in a clinical setting, we did not use diagnostic measures. Although very few women reported receiving treatment for past or current mental health issues at the time of the initial assessment, another limitation is that we did not control for any treatment, either psychotherapy or pharmacologic, that may have occurred throughout the study. Finally, the longitudinal changes examined in the restricted model giving rise to the spike in PTSD symptoms prior to delivery were found using post-hoc testing and therefore a separate study with a priori hypotheses consistent with our findings is needed to determine if such fluctuation in symptomatology is statistically significantly different from the surrounding time periods. Further, our current analyses did not determine whether the spike in the peak period was specifically associated with the new trauma exposure. Other factors related to trauma, such as pre-existing trauma that is triggered during the course of pregnancy, the type of trauma related to interpersonal violence or non-interpersonal violence, and the distress caused by the trauma should be examined in the model to determine their relative influence on changes in symptoms.
Future Directions
In order to generalize our results, a larger expanded perinatal behavioral health study of women during pregnancy would allow for other types of future analyses. Future studies could account for the general trend of fluctuation of change in PTSD and other mental health symptomatology using more sophisticated latent difference structural equation models and better explain the effect of the different risk factors related to trauma and other life-changing events. In addition, with a larger sample size, we would be able to more clearly delineate how these mental health symptomatologies change during the course of pregnancy and through early and later postpartum. Future quantitative and qualitative longitudinal research should further examine the specific temporal sequencing and mutual influence of PTSD with depressive and other anxiety symptoms. In addition, research endeavors which seek to understand the biological correlates and mechanisms of PTSD and other mental health problems that occur across time during pregnancy may help to guide the development of treatment interventions for women experiencing difficulties with adjustment throughout the perinatal and postpartum periods.
Acknowledgments
Acknowledgments and Declarations
This research was supported, in part, by a Research Centers in Minority Institutions Award (P20 RR11091) from the National Center for Research Resources (NCRR), National Institutes of Health. Dissemination was supported in part by a National Institute on Alcohol Abuse and Alcoholism (NIAAA) and National Center on Minority Health and Disparities (NCMHD) Award (5U01AA014289-03) and The Queen’s Medical Center (QMC). Drs. Onoye and Goebert are faculty of the University of Hawai‘i (UH) John A. Burns School of Medicine as well as Senior Scientists at QMC. Dr. Matsu is also affiliated with QMC. The contents of this paper are solely the responsibility of the authors and do not represent the official views of NIAAA, NCMHD, NCCR, or QMC. The investigators thank the women and staff from the clinics that participated in and supported the study.
References
- Alcorn KL, O’Donovan A, Patrick JC, Creedy D, Devilly GJ. A prospective longitudinal study of the prevalence of post-traumatic stress disorder resulting from childbirth events. Psychol Med. 2010;40 (11):1849–1859. doi: 10.1017/s0033291709992224. [DOI] [PubMed] [Google Scholar]
- Alder J, Fink N, Bitzer J, Hosli I, Holzgreve W. Depression and anxiety during pregnancy: a risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. J Matern Fetal Neonatal Med. 2007;20 (3):189–209. doi: 10.1080/14767050701209560. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) 4. American Psychiatric Association; Washington, D.C: 1994. [Google Scholar]
- Apter G, Devouche E, Gratier M. Perinatal mental health. J Nerv Ment Dis. 2011;199 (8):575–577. doi: 10.1097/NMD.0b013e318225f2f4. [DOI] [PubMed] [Google Scholar]
- Ayers S, Eagle A, Waring H. The effects of childbirth-related post-traumatic stress disorder on women and their relationships: a qualitative study. Psychol Health Med. 2006;11 (4):389–398. doi: 10.1080/13548500600708409. [DOI] [PubMed] [Google Scholar]
- Ayers S, Harris R, Sawyer A, Parfitt Y, Ford E. Posttraumatic stress disorder after childbirth: Analysis of symptom presentation and sampling. J Affective Disord. 2009;119 (1–3):200–204. doi: 10.1016/j.jad.2009.02.029. [DOI] [PubMed] [Google Scholar]
- Azar R, Singer S. Maternal prenatal state anxiety symptoms and birth weight: A pilot study. Central European Journal of Medicine. 2012;7 (6):747–752. doi: 10.2478/s11536-012-0078-9. [DOI] [Google Scholar]
- Beck CT, Gable RK, Sakala C, Declercq ER. Posttraumatic stress disorder in new mothers: results from a two-stage U.S. national survey. Birth. 2011;38 (3):216–227. doi: 10.1111/j.1523-536X.2011.00475.x. [DOI] [PubMed] [Google Scholar]
- Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Prevalence of depression during pregnancy: systematic review. Gynecology. 2004;103 (4):698–709. doi: 10.1097/01.AOG.0000116689.75396.5f. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD checklist (PCL) Behav Res Ther. 1996;34 (8):669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, Hoge CW. Validating the primary care posttraumatic stress disorder screen and the posttraumatic stress disorder checklist with soldiers returning from combat. J Consult Clin Psychol. 2008;76 (2):272–281. doi: 10.1037/0022-006x.76.2.272. [DOI] [PubMed] [Google Scholar]
- Born L, Soares CN, Phillips SD, Jung M, Steiner M. Women and reproductive-related trauma. Ann N Y Acad Sci. 2006;1071:491–494. doi: 10.1196/annals.1364.049. [DOI] [PubMed] [Google Scholar]
- Brand SR, Brennan PA. Impact of Antenatal and Postpartum Maternal Mental Illness: How are the Children? Clin Obstet Gynecol. 2009;52 (3):441–455. doi: 10.1097/GRF.0b013e3181b52930. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Peterson EL, Schultz LR. A second look at comorbidity in victims of trauma: the posttraumatic stress disorder-major depression connection. Biol Psychiatry. 2000;48 (9):902–909. doi: 10.1016/S0006-3223(00)00933-1. [DOI] [PubMed] [Google Scholar]
- Breslau N, Lucia VC, Davis GC. Partial PTSD versus full PTSD: an empirical examination of associated impairment. Psychol Med. 2004;34 (7):1205–1214. doi: 10.1017/S0033291704002594. [DOI] [PubMed] [Google Scholar]
- Brooks J, Nathan E, Speelman C, Swalm D, Jacques A, Doherty D. Tailoring screening protocols for perinatal depression: prevalence of high risk across obstetric services in Western Australia. Arch Womens Ment Health. 2009;12 (2):105–112. doi: 10.1007/s00737-009-0048-7. [DOI] [PubMed] [Google Scholar]
- Bruce SE, Weisberg RB, Dolan RT, Machan JT, Kessler RC, Manchester G, Culpepper L, Keller MB. Trauma and posttraumatic stress disorder in primary care patients. Prim Care Companion J Clin Psychiatry. 2001;3 (5):211–217. doi: 10.4088/pcc.v03n0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerulli CC, Talbot NLNL, Tang WW, Chaudron LHLH. Co-occurring intimate partner violence and mental health diagnoses in perinatal women. CORD Conference Proceedings. 2011;20 (12):1797–1803. doi: 10.1089/jwh.2010.2201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Class QA, Lichtenstein P, Langstrom N, D’Onofrio BM. Timing of Prenatal Maternal Exposure to Severe Life Events and Adverse Pregnancy Outcomes: A Population Study of 2.6 Million Pregnancies. Psychosom Med. 2011;73 (3):234–241. doi: 10.1097/PSY.0b013e31820a62ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24 (4):385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- Dennis MF, Flood AM, Reynolds V, Araujo G, Clancy CP, Barefoot JC, Beckham JC. Evaluation of lifetime trauma exposure and physical health in women with posttraumatic stress disorder or major depressive disorder. Violence Against Women. 2009;15 (5):618–627. doi: 10.1177/1077801209331410. [DOI] [PubMed] [Google Scholar]
- Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatry. 2012;25 (2):141–148. doi: 10.1097/YCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans J, Heron J, Francomb H, Oke S, Golding J. Cohort study of depressed mood during pregnancy and after childbirth. BMJ. 2001;323 (7307):257–260. doi: 10.1136/bmj.323.7307.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federenko IS, Wadhwa PD. Women’s mental health during pregnancy influences fetal and infant developmental and health outcomes. CNS Spectr. 2004;9 (3):198–206. doi: 10.1017/s1092852900008993. [DOI] [PubMed] [Google Scholar]
- Forray A, Mayes LC, Magriples U, Epperson CN. Prevalence of post-traumatic stress disorder in pregnant women with prior pregnancy complications. Journal of Maternal-Fetal and Neonatal Medicine. 2009;22 (6):522–527. doi: 10.1080/14767050902801686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedy JR, Steenkamp MM, Magruder KM, Yeager DE, Zoller JS, Hueston WJ, Carek PJ. Post-traumatic stress disorder screening test performance in civilian primary care. Fam Pract. 2010;27 (6):615–624. doi: 10.1093/fampra/cmq049. [DOI] [PubMed] [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and Incidence. Obstet Gynecol. 2005;106 (5 Part 1):1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. 1010.1097/1001.AOG.0000183597.0000131630.db. [DOI] [PubMed] [Google Scholar]
- Glynn LM, Schetter CD, Hobel CJ, Sandman CA. Pattern of perceived stress and anxiety in pregnancy predicts preterm birth. Health Psychol. 2008;27 (1):43–51. doi: 10.1037/0278-6133.27.1.43. [DOI] [PubMed] [Google Scholar]
- Goebert D, Morland L, Frattarelli L, Onoye J, Matsu C. Mental Health During Pregnancy: A Study Comparing Asian, Caucasian and Native Hawaiian Women. Maternal and Child Health Journal. 2007;11 (3):249–255. doi: 10.1007/s10995-006-0165-0. [DOI] [PubMed] [Google Scholar]
- Heron J, O’Connor TG, Evans J, Golding J, Glover V. The course of anxiety and depression through pregnancy and the postpartum in a community sample. J Affect Disord. 2004;80 (1):65–73. doi: 10.1016/j.jad.2003.08.004. [DOI] [PubMed] [Google Scholar]
- Homish GG, Cornelius JR, Richardson GA, Day NL. Antenatal risk factors associated with postpartum comorbid alcohol use and depressive symptomatology. Alcohol Clin Exp Res. 2004;28 (8):1242–1248. doi: 10.1097/01.alc.0000134217.43967.97. 00000374-200408000-00014. [DOI] [PubMed] [Google Scholar]
- Hosseini SM, Biglan MW, Larkby C, Brooks MM, Gorin MB, Day NL. Trait anxiety in pregnant women predicts offspring birth outcomes. Paediatr Perinat Epidemiol. 2009;23 (6):557–566. doi: 10.1111/j.1365-3016.2009.01065.x. [DOI] [PubMed] [Google Scholar]
- Hung T-H, Lo L-M, Chiu T-H, Li M-J, Yeh Y-L, Chen S-F, Hsieh Ts-Ta. A longitudinal study of oxidative stress and antioxidant status in women with uncomplicated pregnancies throughout gestation. Reproductive Sciences. 2010;17 (4):401–409. doi: 10.1177/1933719109359704. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62 (6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Koubovec D, Geerts L, Odendaal HJ, Stein DJ, Vythilingum B. Effects of psychologic stress on fetal development and pregnancy outcome. Curr Psychiatry Rep. 2005;7 (4):274–280. doi: 10.1007/s11920-005-0081-9. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Haynes SN, Leisen MB, Owens JA, Kaplan AS, Watson SB, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: the Traumatic Life Events Questionnaire. Psychol Assess. 2000;12 (2):210–224. doi: 10.1037/1040-3590.8.4.428. [DOI] [PubMed] [Google Scholar]
- Littleton HL, Breitkopf CR, Berenson AB. Correlates of anxiety symptoms during pregnancy and association with perinatal outcomes: a meta-analysis. Am J Obstet Gynecol. 2007;196 (5):424–432. doi: 10.1016/j.ajog.2007.03.042. [DOI] [PubMed] [Google Scholar]
- Loveland Cook CA, Flick LH, Homan SM, Campbell C, McSweeney M, Gallagher ME. Posttraumatic stress disorder in pregnancy: prevalence, risk factors, and treatment. Obstet Gynecol. 2004;103 (4):710–717. doi: 10.1097/01.AOG.0000119222.40241.fb. [DOI] [PubMed] [Google Scholar]
- Maggioni C, Margola D, Filippi F. PTSD, risk factors, and expectations among women having a baby: a two-wave longitudinal study. J Psychosom Obstet Gynaecol. 2006;27 (2):81–90. doi: 10.1080/01674820600712875. [DOI] [PubMed] [Google Scholar]
- Manne SL, Du Hamel K, Gallelli K, Sorgen K, Redd WH. Posttraumatic stress disorder among mothers of pediatric cancer survivors: diagnosis, comorbidity, and utility of the PTSD checklist as a screening instrument. J Pediatr Psychol. 1998;23 (6):357–366. doi: 10.1093/jpepsy/23.6.357. [DOI] [PubMed] [Google Scholar]
- Marcus SM, Flynn HA, Blow FC, Barry KL. Depressive symptoms among pregnant women screened in obstetrics settings. J Womens Health (Larchmt) 2003;12 (4):373–380. doi: 10.1089/154099903765448880. [DOI] [PubMed] [Google Scholar]
- Mezey G, Bacchus L, Bewley S, White S. Domestic violence, lifetime trauma and psychological health of childbearing women. BJOG. 2005;112 (2):197–204. doi: 10.1111/j.1471-0528.2004.00307.x. [DOI] [PubMed] [Google Scholar]
- Monk C. Stress and mood disorders during pregnancy: implications for child development. Psychiatr Q. 2001;72 (4):347–357. doi: 10.1023/A:1010393316106. [DOI] [PubMed] [Google Scholar]
- Morland LA, Goebert DA, Onoye JM, Frattarelli L, Derauf C, Herbst M, Matsu C, Friedman M. Posttraumatic Stress Disorder and Pregnancy Health: Preliminary Update and Implications. Psychosomatics. 2007;48 (4):304–308. doi: 10.1176/appi.psy.48.4.304. [DOI] [PubMed] [Google Scholar]
- Mosack V, Shore ER. Screening for depression among pregnant and postpartum women. J Community Health Nurs. 2006;23 (1):37–47. doi: 10.1207/s15327655jchn2301_4. [DOI] [PubMed] [Google Scholar]
- Onoye JM, Goebert D, Morland L, Matsu C, Wright T. PTSD and postpartum mental health in a sample of Caucasian, Asian, and Pacific Islander women. Arch Womens Ment Health. 2009;12 (6):393–400. doi: 10.1007/s00737-009-0087-0. [DOI] [PubMed] [Google Scholar]
- Radloff L. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1 (3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. J Consult Clin Psychol. 1993;61 (6):984–991. doi: 10.1037/0022-006X.61.6.984. [DOI] [PubMed] [Google Scholar]
- Rodríguez MA, Valentine J, Ahmed SR, Eisenman DP, Sumner LA, Heilemann MV, Liu H. Intimate partner violence and maternal depression during the perinatal period: a longitudinal investigation of Latinas. Violence Against Women. 2010;16 (5):543–559. doi: 10.1177/1077801210366959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogal SS, Poschman K, Belanger K, Howell HB, Smith MV, Medina J, Yonkers KA. Effects of posttraumatic stress disorder on pregnancy outcomes. J Affect Disord. 2007;102 (1–3):137–143. doi: 10.1016/j.jad.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rondo PH, Vaz AJ, Moraes F, Tomkins A. The relationship between salivary cortisol concentrations and anxiety in adolescent and non-adolescent pregnant women. Braz J Med Biol Res. 2004;37 (9):1403–1409. doi: 10.1590/s0100-879x2004000900016. S0100-879X2004000900015. [DOI] [PubMed] [Google Scholar]
- Rosen D, Seng JS, Tolman RM, Mallinger G. Intimate partner violence, depression, and posttraumatic stress disorder as additional predictors of low birth weight infants among low-income mothers. J Interpers Violence. 2007;22 (10):1305–1314. doi: 10.1177/0886260507304551. [DOI] [PubMed] [Google Scholar]
- Ross LE, McLean LM. Anxiety disorders during pregnancy and the postpartum period: A systematic review. J Clin Psychiatry. 2006;67 (8):1285–1298. doi: 10.4088/jcp.v67n0818. [DOI] [PubMed] [Google Scholar]
- Rothenberger SE, Moehler E, Reck C, Resch F. Prenatal stress: course and interrelation of emotional and physiological stress measures. Psychopathology. 2011;44 (1):60–67. doi: 10.1159/000319309. [DOI] [PubMed] [Google Scholar]
- Seng JS. A conceptual framework for research on lifetime violence, posttraumatic stress, and childbearing. J Midwifery Womens Health. 2002;47 (5):337–346. doi: 10.1016/s1526-9523(02)00275-1. S1526952302002751. [DOI] [PubMed] [Google Scholar]
- Seng JS, Kohn-Wood LP, McPherson MD, Sperlich M. Disparity in posttraumatic stress disorder diagnosis among African American pregnant women. Arch Womens Ment Health. 2011a;14 (4):295–306. doi: 10.1007/s00737-011-0218-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng JS, Low LK, Sperlich M, Ronis DL, Liberzon I. Prevalence, trauma history, and risk for posttraumatic stress disorder among nulliparous women in maternity care. Obstet Gynecol. 2009;114 (4):839–847. doi: 10.1097/AOG.0b013e3181b8f8a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng JS, Low LK, Sperlich M, Ronis DL, Liberzon I. Post-traumatic stress disorder, child abuse history, birthweight and gestational age: a prospective cohort study. BJOG. 2011b;118 (11):1329–1339. doi: 10.1111/j.1471-0528.2011.03071.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng JS, Oakley DJ, Sampselle CM, Killion C, Graham-Bermann S, Liberzon I. Posttraumatic stress disorder and pregnancy complications. Obstet Gynecol. 2001;97 (1):17–22. doi: 10.1016/s0029-7844(00)01097-8. S0029-7844(00)01097-8. [DOI] [PubMed] [Google Scholar]
- Seng JS, Rauch SA, Resnick H, Reed CD, King A, Low LK, McPherson M, Muzik M, Abelson J, Liberzon I. Exploring posttraumatic stress disorder symptom profile among pregnant women. J Psychosom Obstet Gynaecol. 2010;31 (3):176–187. doi: 10.3109/0167482x.2010.486453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith MV, Poschman K, Cavaleri MA, Howell HB, Yonkers KA. Symptoms of posttraumatic stress disorder in a community sample of low-income pregnant women. Am J Psychiatry. 2006;163 (5):881–884. doi: 10.1176/appi.ajp.163.5.881. [DOI] [PubMed] [Google Scholar]
- Smith MV, Rosenheck RA, Cavaleri MA, Howell HB, Poschman K, Yonkers KA. Screening for and detection of depression, panic disorder, and PTSD in public-sector obstetric clinics. Psychiatr Serv. 2004;55 (4):407–414. doi: 10.1176/appi.ps.55.4.407. [DOI] [PubMed] [Google Scholar]
- Soderquist J, Wijma B, Wijma K. The longitudinal course of post-traumatic stress after childbirth. J Psychosom Obstet Gynaecol. 2006;27 (2):113–119. doi: 10.1080/01674820600712172. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Consulting Psychologists; Palo Alto: 1983. [Google Scholar]
- Stein MB, Walker JR, Hazen AL, Forde DR. Full and partial posttraumatic stress disorder: findings from a community survey. Am J Psychiatry. 1997;154 (8):1114–1119. doi: 10.1176/ajp.154.8.1114. [DOI] [PubMed] [Google Scholar]
- Tollenaar MS, Beijers R, Jansen J, Riksen-Walraven JM, de Weerth C. Maternal prenatal stress and cortisol reactivity to stressors in human infants. Stress. 2010;13 (6):491–497. doi: 10.3109/10253890.2010.499485. [DOI] [PubMed] [Google Scholar]
- van Bussel J, Spitz B, Demyttenaere K. Depressive symptomatology in pregnant and postpartum women. An exploratory study of the role of maternal antenatal orientations. Arch Womens Ment Health. 2009;12 (3):155–166. doi: 10.1007/s00737-009-0061-x. [DOI] [PubMed] [Google Scholar]
- Van den Bergh BR, Mulder EJ, Mennes M, Glover V. Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and child: links and possible mechanisms. A review. Neurosci Biobehav Rev. 2005;29 (2):237–258. doi: 10.1016/j.neubiorev.2004.10.007. [DOI] [PubMed] [Google Scholar]
- Vesga-Lopez O, Blanco C, Keyes K, Olfson M, Grant BF, Hasin DS. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65 (7):805–815. doi: 10.1001/archpsyc.65.7.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadhwa PD, Sandman CA, Garite TJ. The neurobiology of stress in human pregnancy: implications for prematurity and development of the fetal central nervous system. Prog Brain Res. 2001;133:131–142. doi: 10.1016/s0079-6123(01)33010-8. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Huska JA, Keane TM. PTSD Checklist-Civilian version. National Center for PTSD, Behavioral Science Division; Boston, Massachusetts: 1994. [Google Scholar]
- Wenzel A, Haugen EN, Jackson LC, Brendle JR. Anxiety symptoms and disorders at eight weeks postpartum. J Anxiety Disord. 2005;19 (3):295–311. doi: 10.1016/j.janxdis.2004.04.001. [DOI] [PubMed] [Google Scholar]
- Yampolsky L, Lev-Wiesel R, Ben-Zion IZ. Child sexual abuse: is it a risk factor for pregnancy? J Adv Nurs. 2010;66 (9):2025–2037. doi: 10.1111/j.1365-2648.2010.05387.x. [DOI] [PubMed] [Google Scholar]
- Yarvis JS, Schiess L. Subthreshold posttraumatic stress disorder (PTSD) as a predictor of depression, alcohol use, and health problems in veterans. Journal of Workplace Behavioral Health. 2008;23 (4):395–424. [Google Scholar]
- Yim IS, Glynn LM, Dunkel Schetter C, Hobel CJ, Chicz-DeMet A, Sandman CA. Risk of postpartum depressive symptoms with elevated corticotropin-releasing hormone in human pregnancy. Arch Gen Psychiatry. 2009;66 (2):162–169. doi: 10.1001/archgenpsychiatry.2008.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaers S, Waschke M, Ehlert U. Depressive symptoms and symptoms of post-traumatic stress disorder in women after childbirth. J Psychosom Obstet Gynaecol. 2008;29 (1):61–71. doi: 10.1080/01674820701804324. [DOI] [PubMed] [Google Scholar]
- Zelkowitz P, Saucier JF, Wang T, Katofsky L, Valenzuela M, Westreich R. Stability and change in depressive symptoms from pregnancy to two months postpartum in childbearing immigrant women. Arch Womens Ment Health. 2008;11 (1):1–11. doi: 10.1007/s00737-008-0219-y. [DOI] [PubMed] [Google Scholar]