Abstract
Cancer prevention (chemoprevention) by using naturally occurring dietary agents has gained immense interest due to the broad safety window of these compounds. However, many of these compounds are hydrophobic and poorly soluble in water. They frequently display low bioavailability, poor systemic delivery, and low efficacy. To circumvent this problem, we explored a novel approach towards chemoprevention using nanotechnology to deliver luteolin, a natural compound present in green vegetables. We formulated water soluble polymer-encapsulated Nano-Luteolin from hydrophobic luteolin, and studied its anticancer activity against lung cancer and head and neck cancer. In vitro studies demonstrated that, like luteolin, Nano-Luteolin inhibited the growth of lung cancer cells (H292 cell line) and squamous cell carcinoma of head and neck (SCCHN) cells (Tu212 cell line). In Tu212 cells, the IC50 value of Nano-Luteolin was 4.13μM, and that of luteolin was 6.96μM. In H292 cells, the IC50 of luteolin was 15.56μM, and Nano-Luteolin was 14.96μM. In vivo studies using a tumor xenograft mouse model demonstrated that Nano-Luteolin has a significant inhibitory effect on the tumor growth of SCCHN in comparison to luteolin. Our results suggest that nanoparticle delivery of naturally occurring dietary agents like luteolin has many advantages and may have potential application in chemoprevention in clinical settings.
Keywords: Cancer, chemoprevention, luteolin, nanotechnology, nanomedicine
Introduction
Cancer remains one of the deadliest diseases causing a large number of deaths worldwide. In 2008, about 7.6 million people died of cancer-related causes globally, and it is estimated that by 2030, there will be 13.1 million cancer deaths (1).
Chemoprevention is a way of controlling cancer in which the occurrence of the disease can be completely prevented, slowed down, or reversed by administering one or more naturally occurring compounds or synthetic agents. Even after the treatment of cancer by surgical removal of tumor, or chemotherapeutic drug, radiation therapy or both, there is a high probability of cancer recurrence. Chemoprevention can prevent the risk of cancer recurrence among cancer patients, and it can also reduce the risk of cancer in the general population. Prevention offers the most cost-effective long term strategy for the control of cancer. Chemoprevention by using naturally occurring nontoxic molecules has emerged as a unique strategy for cancer management (2). Recently, naturally occurring dietary agents present in vegetables, fruits, spices, and herbs have generated immense interest for their potential application in chemoprevention and therapy, and in fact many of these compounds are currently under early phase clinical trials, and available over the counter in most pharmacies (3-8). The advantage of dietary agents in comparison to the currently used chemotherapeutic agents is their higher level of safety (3-8). An ideal chemopreventive compound is expected to be nontoxic, orally active, highly effective, less expensive, and easily available.
The flavonoid luteolin, 3’,4’,5,7-tetrahydroxyflavone, is a natural antioxidant that usually occurs in its glycosylated form in many green vegetables such as artichoke, broccoli, cabbage, celery, cauliflower, green pepper, and spinach (3, 9). Luteolin exhibits a wide range of pharmacological properties ranging from anti-inflammation to anticancer effects. Luteolin has shown anticancer effects against lung cancer, head and neck cancer, prostate, breast, colon, liver, cervical, and skin cancer (10-24). It triggers apoptotic cell death by activating apoptosis pathways and suppressing cell survival pathways. Luteolin has displayed anticancer effects by inducing cell cycle arrest, senescence, or apoptosis in lung carcinoma cells (10-12), oral squamous cancer cells (13-15), human esophageal adenocarcinoma cells (16), human colon cancer cells (17), and human hepatoma cells (18). Luteolin inhibited proliferation and induced apoptosis of prostate cancer (19-21) cells in vitro and in vivo. It increased the efficacy of cisplatin in gastric cancer cells (22). In an animal model, luteolin also inhibited tumor growth against breast cancer cell lines (MCF-7/6 and MDA-MB231-1833) (23). In another study, luteolin significantly reduced the incidence of colon cancer and the number of tumors per rat (24). The results of these studies warrant the evaluation of the chemopreventive potential of luteolin in human subjects.
Though chemoprevention using natural compounds has shown promising results in preclinical settings, its application to humans has met with various challenges, mainly due to inefficient systemic delivery and low bioavailability of these natural compounds (3, 9). In order to achieve the maximum possible efficacy of a chemopreventive compound, new strategies are required to enhance the bioavailability of potentially useful compounds, and reduce undesired toxicity.
Nanomedicine is an emerging research area and nanotechnology is being implemented and evaluated in several areas of cancer therapeutics and cancer management (25-38). Nanoparticles are known to have many advantages for the delivery of cancer therapeutics, for example, they have longer blood circulation time, higher bioavailability, enhanced permeability and retention (EPR) effect, higher tumor-specific delivery, and higher efficacy (25-38). Studies from our group and other researchers have demonstrated that nanoparticle-mediated delivery could be a promising approach to enhance the bioavailability of chemopreventive agents (such as EGCG, curcumin, luteolin), increase efficacy, and reduce undesired toxicities (38-40).
The flavonoid luteolin has immense potential for its application in cancer prevention and therapy (3, 8, 9). However, luteolin is poorly soluble in water, making its intravenous or intraperitoneal administration very difficult. In this study, we have formulated a polymer-encapsulated luteolin nanoparticle (Nano-Luteolin), which is water soluble, and studied its anticancer properties against squamous cell carcinoma of head and neck (SCCHN, Tu212) and non-small cell lung cancer (NSCLC, H292) cells. In vitro studies have shown that like luteolin, Nano-Luteolin can also inhibit the growth of H292 and Tu212 cells. In vivo studies using tumor xenograft mouse models have demonstrated that Nano-Luteolin has considerable inhibitory effect on tumor growth of SCCHN.
Materials and Methods
Nanoformulation
PLA-PEG-OMe (1 gm in 10 mL MeOH) and luteolin (100 mg in 60 ml MeOH) solutions were mixed together. This mixture of PLA-PEG-OMe and luteolin was added dropwise to 200 ml of 1% (w/v) polyvinyl alcohol solution with constant stirring. Stirring was continued for 20h. Unencapsulated luteolin precipitated in the solution. The solution was centrifuged at 6,000 rpm, the precipitate got accumulated at the bottom, and the supernatant was filtered using a Millipore Millex-HN syringe driven filter unit with cut-off 0.20 μm to remove the remaining unencapsulated luteolin. The filtrate was purified using an Amicon ultra-15 centrifugal filter with cut-off 30,000 to obtain pure polymer-encapsulated luteolin nanoparticle (Nano-Luteolin) solution. Freshly prepared Nano-luteolin solution was lyophilized to obtain yellowish powder, and reconstituted for biological studies. Luteolin content in the nanoparticle was calculated by measuring the absorbance of luteolin solution using a Shimadzu UV-2401 PC UV-Vis spectrophotometer at 355 nm (41-43). Nanoparticle was dissolved in solvent DMF, and then the nanoparticle lost its structural sanctity (42). The DMF was removed under reduced pressure, and the residue was dissolved in methanol. Then the UV absorbance of the solution was measured to determine the luteolin concentration (41-43). The luteolin content in nanoparticle is 1.4% (w/w) and the encapsulation efficiency is 9% (41-43). The hydrodynamic diameter was obtained using Malvern Zetasizer Nanoseries Nano-ZS90. A Zeiss LSM510 Meta confocal microscope was used for imaging.
Cell lines
SCCHN cell line Tu212 was obtained from Dr. Gary L. Clayman (University of Texas M.D. Anderson Cancer Center, Houston, TX) as described in our previous publication (44). This cell line was cultured in DMEM/F12 (1:1) with 10% heat inactivated fetal bovine serum (FBS) and maintained in a humidified incubator at 37°C, 5% CO2. The human origin of this cell line was confirmed by genotyping with 9 commonly used STR markers by Research Animal Diagnostic Laboratory (Columbia, MO) in 2009. The human NSCLC cell line H292 was provided by Dr. Shi-Yong Sun who obtained it from Dr. R. Lotan (MD Anderson Cancer Center, Houston, TX) in 2003. H292 cells can be maintained in RPMI1640 medium supplemented with 10% heat-inactivated FBS in a humidified incubator at 37°C, 5% CO2. This cell line has not been authenticated (45).
Reagents
Luteolin (Sigma-Aldrich, St. Louis, MO, USA) was dissolved in DMSO as a stock solution for in vitro studies. The reagent was further diluted in cell culture medium immediately before use. The final concentration of DMSO was less than 0.1%.
Cell viability assay
Cell viability was measured using a sulforhodamine B (SRB) assay (46). 3000 cells were seeded in a 96-well plate. After 16h, cells were treated with Nano-Luteolin or, PLA-PEG polymer solutions at various concentrations, and incubated for 72h. After 72 hrs of culture, cells were fixed with 10% trichloroacetic acid. Plates were stained with 0.4% SRB for 10 min and bound SRB was dissolved in 10mmol/L Tris base (pH 10.5). Cell growth was assessed by OD determination at 492 nm using a microplate reader. The percentage of survival was then calculated based on the absorbance values relative to the control samples. The no treatment group was considered as 100% cell growth and used as a control, and the treatment group was compared to this control.
Colony formation assay
The efficacy of luteolin against Tu212 and H292 cells was tested using a colony formation assay. 400 cells were seeded in 6-well plate tissue culture dishes and treated with luteolin, Nano-Luteolin, or polymer for 72h. The concentrations of luteolin in the nanoparticle (Nano-Luteolin) were 5μM and 10μM. Then the media was replaced by fresh media. The cells were maintained under standard cell culture conditions at 37°C and 5% CO2 in a humid environment. Colonies that formed in 2 weeks were fixed with 10% buffered formalin, stained with 2% gentian violet (w/v methanol solution), washed with water, and air-dried.
Immunofluorescence assay
5000 cells in 50μL were seeded in each chamber of a Lab Tek II chamber slide system and incubated at 37°C. After 24h, the media was removed, and new serum free media was added, and incubated for 24h. The media was removed, and the nanoparticle solution (in serum free media) encapsulating both luteolin and dye was added to the chamber, and incubated for various durations to determine cellular uptake at different time points. The reaction was stopped with cold PBS and any membrane-bound reagent was removed with cold 0.2M acetic acid in saline (pH 2.8) for 2 minutes on ice. Cells were washed three times with PBS, formalin in PBS (4%) was added, covered with aluminum foil, and kept for 20min. Formalin was removed, and cells were washed three times with PBS. The fluorescently labeled cells were treated with liquid mountant Prolong Gold antifade reagent containing DAPI.
Nude mouse xenograft model
Animal experiments were approved by the Institutional Animal Care and Use Committee (IACUC) of Emory University. Twenty eight nude mice (athymic nu/nu, Harlan Sprague Dawley, Company name), aged 4-6 weeks (~20 g weight), were randomly divided into four groups. Mice were intraperitoneally administered control (n=7), polymer (n=7), luteolin (3.3mg/Kg bodyweight) (n=7), or Nano-Luteolin (3.3mg/Kg bodyweight) (n=7) every alternate day for 7 days before inoculation of 2.5×106 Tu212 cells by subcutaneous injection into the right flank. Intraperitoneal administration every alternate day was continued for 30 days. The tumor size was measured on alternate days. The tumor volume was calculated using the formula: V = π/6 × larger diameter × (smaller diameter)2 as reported previously (47). Growth curves were plotted using average tumor size within each experimental group at the set time points.
Immunohistochemistry
Immunohistochemistry analysis for Ki-67 staining on formalin fixed, paraffin-embedded nude mouse xenograft tissue was performed using the R.T.U. Vectastain kit following the standard manufacturer’s protocol (Vector Laboratories, Burlingame, CA). Tissue sections were incubated with mouse anti-human Ki-67 (prediluted; Invitrogen, Frederick, MD) for one hour at room temperature. The slides were stained with 3, 30-diaminobenzidine (DAB) (Sigma Chemical) and counterstained with hematoxylin (Vector Laboratories). TUNEL assay was performed by immunofluorescence using the same specimens as above following the procedure provided by the manufacturer (Promega, Madison, WI). The slides were counterstained with DAPI (Invitrogen, Frederick, MD). Five areas were randomly selected from each slide for analysis. For Ki-67 staining, the intensity of positive cells was measured by counting the absolute number of pixels.
Statistical analysis
Statistical significance was assessed using Student’s T test for SRB-assay. P<0.05 was considered significant in all analyses. For the in vivo antitumor efficacy assay, a log-linear mixed model with random intercept was used to compare the significance of the mean tumor volumes among each group.
Results
Formulation of nanoparticle
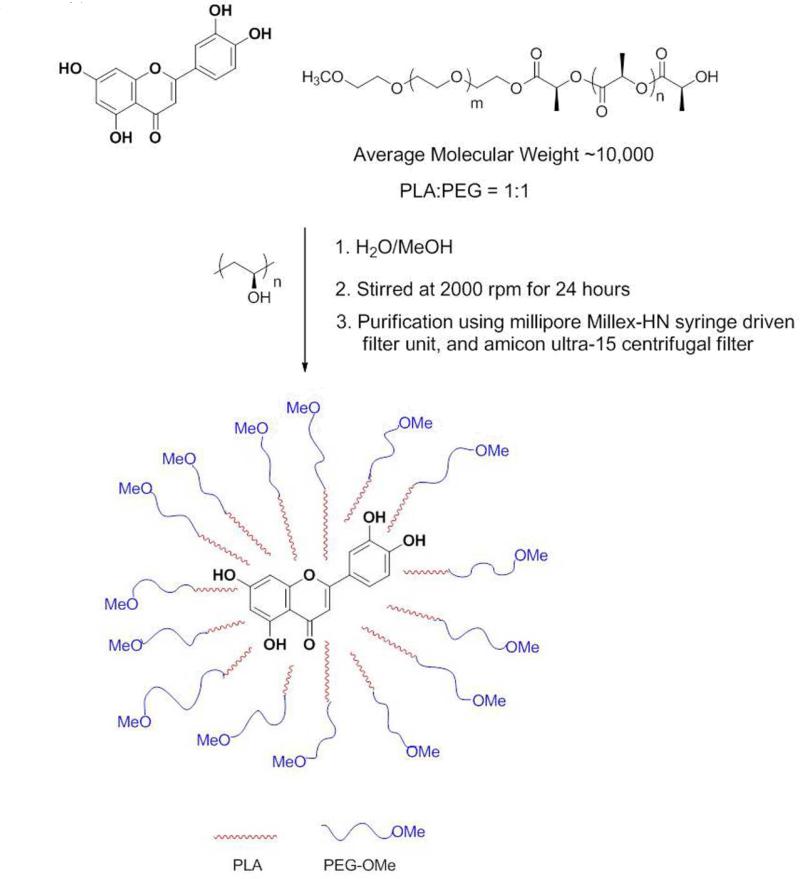
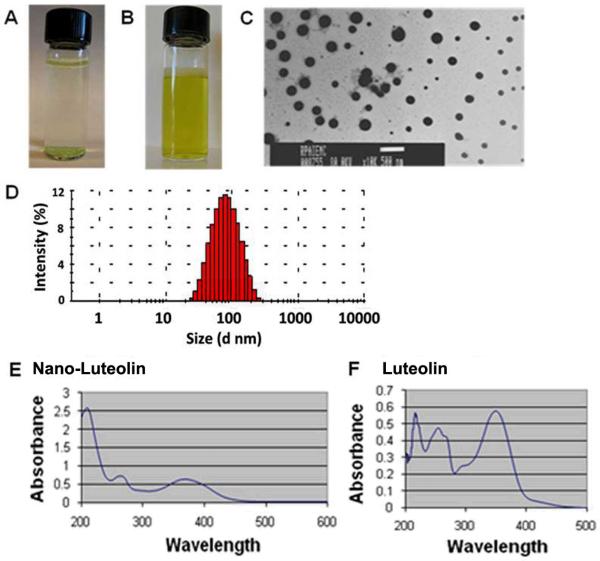
To facilitate the effective delivery of luteolin and obtain associated benefits, we used a diblock co-polymer consisting of polylactic acid (PLA) and polyethylene glycol ether (PEG) to formulate the Nano-Luteolin. An emulsion solvent evaporation method was used to formulate the water soluble Nano-Luteolin (Experimental Section) (Figure 1). The properties of polymer-encapsulated Nano-Luteolin were characterized by dynamic light scattering (DLS) and transmission electron microscopy (TEM) to give the size of each preparation (Figure 2A, 2B, 2C, 2D). UV-Vis spectroscopic analysis of both luteolin and Nano-Luteolin showed the absorbance maxima from the phenyl rings of luteolin at about 261 nm and 355 nm (Figure 2E, 2F). DLS and TEM studies revealed that the mean size of the nanoparticles was about 115 nm.
Figure 1.
Development of polymer-encapsulated Nano-Luteolin. Schematic representation of encapsulation of luteolin using the diblock copolymer, methoxy poly(ethylene glycol) polylactic acid, PLA-PEG.
Figure 2.
(A) Luteolin in water. (B) Water solution of Nano-Luteolin. (C) Representative transmission electron microscopy (TEM) image of polymer-encapsulated Nano-Luteolin. (D) DLS of Nano-Luteolin solution. (E) UV-Vis spectrum of Nano-Luteolin. (F) UV-Vis spectrum of luteolin.
In vitro anti-tumor efficacy study
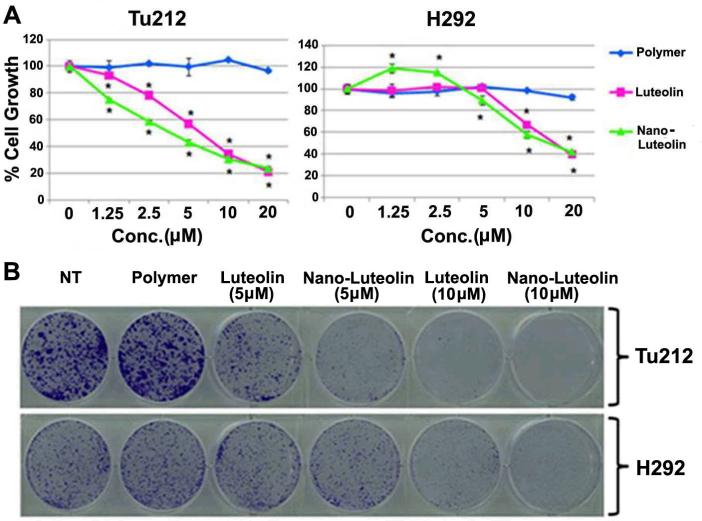
In order to evaluate the anti-cancer potential of Nano-Luteolin, we performed SRB assays (46) to determine live cell density based on the measurement of cellular protein content. We treated head and neck (Tu212) and lung (H292) cancer cells with luteolin, Nano-Luteolin, or the polymer, and performed SRB assays to compare their efficacy in cell growth inhibition. The SRB assay showed that in both cell lines, Nano-Luteolin exhibited cell growth inhibition similar to that of luteolin (Figure 3A). We used CalcuSyn software to determine the IC50 values. In Tu212 cells, the IC50 value of Nano-Luteolin was 4.13μM, and that of luteolin was 6.96μM. In H292 cells, the IC50 of Nano-Luteolin was 14.96μM and that of luteolin was 15.56μM.
Figure 3.
(A) SRB assay for study of cell growth inhibition in head and neck squamous cell carcinoma, HNSCC (Tu212), and lung cancer (H292) cell lines. *P< 0.05. (B) Colony formation assay. Tu212 and H292 cells were seeded at a concentration of 400 cells/well in 6-well plates and treated with the indicated concentrations of luteolin and Nano-Luteolin.
Next, we performed a colony formation assay to directly compare the anti-cancer efficacy of polymer-encapsulated Nano-Luteolin with that of luteolin in Tu212 and H292 cells (Figure 3B). This study showed that in Tu212 cells, at a concentration of 5μM, Nano-Luteolin inhibited colony formation more effectively than luteolin; and more colonies were observed following luteolin treatment than nanoparticle (Nano-luteolin) treatment. At a concentration of 10μM luteolin, both Nano-Luteolin and luteolin displayed a strong cell growth inhibitory effect, and the number of colonies was similar in both cases. In H292 cells, at a concentration of 5μM, both Nano-Luteolin and luteolin showed a similar effect in inhibition of colony formation, with a similar number of colonies observed. At a concentration of 10μM, Nano-Luteolin inhibited colony formation more effectively than luteolin; and the number of colonies was greater in luteolin-treated cells than in Nano-Luteolin-treated cells. At a concentration of 15 μM, both Nano-Luteolin and luteolin completely eradicated cancer cells and no colonies were observed in either case (data not shown).
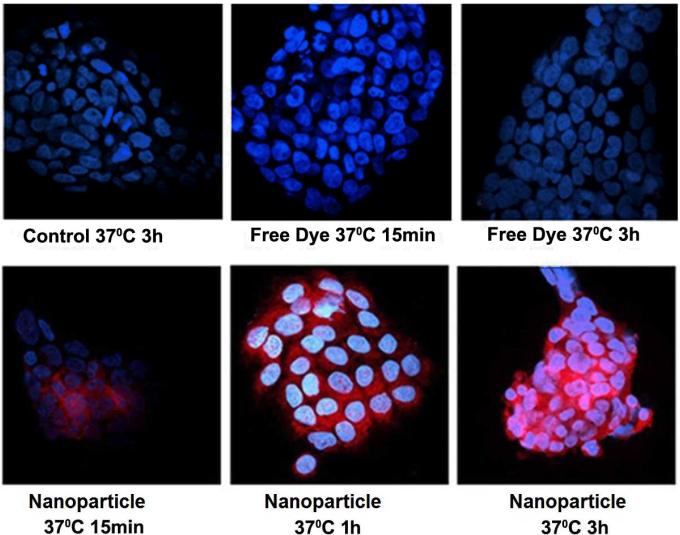
To investigate the cellular uptake of Nano-Luteolin, we formulated polymeric nanoparticles which encapsulated both luteolin and sulforhodamine B acid chloride. As a control, Tu212 cells were incubated with the nanoparticle at 4°C for 15 min and the nuclei were stained with DAPI; no internalization of nanoparticle was observed. We then increased the temperature to 37°C and incubated the Tu212 cells with the nanoparticle for 15min, 1h, and 3h. Confocal images showed that the nanoparticles were taken up by Tu212 cells; the cellular uptake of nanoparticle increased with incubation time (Figure 4). This shows the ability of the nanoparticle to be internalized into cells in a temperature and time dependent manner. Tu212 cells were also incubated with free sulforhodamine B acid chloride dye for 15min and 3h. A negligible amount of free dye was taken up by Tu212 cells even at 37°C.
Figure 4.
Cellular uptake of nanoparticles encapsulating both dye and luteolin in Tu212 cells. Tu212 cells were incubated with nanoparticles and free dye at 37°C for various time points. Confocal images show Tu212 cell uptake of nanoparticles 15min, 1h, and 2h after incubation.
In vivo antitumor study
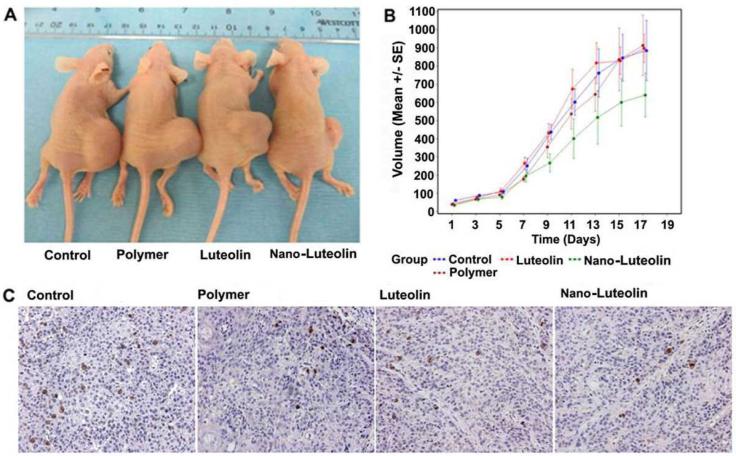
We next evaluated the efficacy of Nano-Luteolin in a xenograft mouse model of head and neck cancer developed by s.c. injection of Tu212 cells in the flank of athymic nude mice. We divided mice into four different groups (n=7 per group): i) control group treated with PBS, ii) polymer treated group, iii) luteolin treated group (3.3mg/Kg luteolin), iv) Nano-Luteolin treated group (3.3mg/Kg luteolin-equivalent). Each mouse was intraperitoneally administered their assigned compound every alternate day for 7 days before inoculation of 2.5×106 Tu212 cells by subcutaneous injection into the right flank. The compounds were intraperitoneally administered every alternate day for 30 days. When the tumors grew to a size of 1700mm3 and became ulcerous according to the IACUC guidelines, the mice were sacrificed. A log-linear mixed model with random intercept was used to compare the mean tumor volume between the treatment and control groups. The difference in tumor volume during the whole measurement period reached a significant level between the Nano-Luteolin group and luteolin group (p=0.0398). Compared to the control group, treatment with nanoparticles resulted in reasonable inhibition of tumor growth, but the difference was not significant (p=0.1193). Tumor volumes in the polymer (p=0.5978) and luteolin-treated (p=0.8719) groups were not significantly different from the control group. These results indicate that the efficacy of Nano-Luteolin is greater than that of luteolin. Indeed, our data showed that at 22 days post-inoculation, the tumor volume in control mice was 886mm3, compared with 641mm3 in the Nano-Luteolin treatment group (Figure 5A, 5B). The tumor volumes in the luteolin and polymer groups were 898mm3 and 914mm3, respectively. This study shows that the nanoparticle-treated group had a clear inhibitory effect on tumor growth over time when compared with control group (Figure 5A, 5B). Furthermore, no weight loss was observed for Nano-Luteolin-treated animals.
Figure 5.
Antitumor effect of Nano-Luteolin in an animal model. (A) Representative mouse from each group. (B) Tumor growth of Tu212 xenograft was inhibited in the Nano-Luteolin treated group compared to the control and luteolin. For Tu212 tumors, the difference in tumor volume during the whole measurement period reached a significant level between the nano-luteolin and luteolin group (p=0.0398). Other comparisons were insignificant (p>0.05). (C) Paraffin-embedded tissue sections from different treatment groups were immunostained with anti-Ki-67 for cell proliferation.
Ki-67 expression and apoptosis in xenograft tumors
Immunohistochemical analysis of Ki-67 staining revealed a greater inhibition of proliferating cells in the Nano-Luteolin-treated mice than the control group (Figure 5C). Though there was no statistically significant difference in mean Ki-67 expression between the treated and untreated groups (p = 0.3), we observed a clear trend within the groups. There was no significant difference in the numbers of apoptotic cells among groups (data not shown).
Discussion
Nanochemoprevention is a novel concept in which nanotechnology-based regimens are developed for the prevention of cancer. Using nanotechnology, we have prepared water soluble Nano-Luteolin from hydrophobic luteolin. Nanoparticles can enter into the cell by various mechanisms, including direct diffusion through the plasma membrane of the cell, and entry through receptor-mediated endocytosis (48-51). The receptor can be a nanoparticle-specific membrane protein, or it can simply be any lipid, protein, or carbohydrate to which the nanoparticle binds, and then undergoes endocytosis (48-51).
We used PLA-PEG polymer since it is safe, biocompatible and biodegradable, and is already approved by the United States Food and Drug Administration (FDA). PLA-PEG based polymeric nanoparticles have been well-studied for the delivery of various drugs and, they are found to be stable after storage (38, 52-63). In fact, a PLA-PEG based polymeric nanoparticle Genexol is approved for treatment of cancer in Korea, and it is undergoing clinical trials in USA for breast cancer, ovarian cancer, non-small cell lung cancer, pancreatic cancer, bladder cancer, ureter cancer, and locally advanced squamous cell head and neck carcinoma (64). PLA is a hydrophobic polymer and insoluble in water, whereas the PEG is hydrophilic and water soluble. Thus, PLA forms the hydrophobic inner core of the nanoparticle, whereas PEG constitutes the hydrophilic outer surface of the polymeric nanoparticle. Hydrophobic luteolin can position itself inside the inner core of the nanoparticle.
In order to study the in vitro efficacy of Nano-Luteolin, we initially compared the efficacy of luteolin, Nano-Luteolin, and the polymer in cell growth inhibition of head and neck cancer (Tu212) and lung cancer (H292) cells, as assessed by SRB assay. This study showed that in both cell lines, Nano-Luteolin exhibited cell growth inhibition similar to that of luteolin.
This prompted us to perform colony formation assays to compare the anti-cancer efficacy of polymer-encapsulated Nano-Luteolin with that of luteolin in Tu212 and H292 cells. In this study, we observed that the polymer encapsulation of luteolin and its release from polymeric nanoparticle had an effect on its anti-cancer activity. For example, in Tu212 cells, at a concentration of 5μM, Nano-Luteolin inhibited colony formation more effectively than luteolin. Similarly, in H292 cells at a concentration of 10μM, Nano-Luteolin inhibited colony formation more effectively than luteolin.
We also investigated the cellular uptake of polymeric nanoparticles that encapsulated both luteolin and sulforhodamine B acid chloride. This study confirmed the ability of the nanoparticle to be internalized into cells in a temperature and time dependent fashion.
Finally we evaluated the efficacy of Nano-Luteolin using a xenograft mouse model of head and neck cancer. Our study showed that in mice treated with the water soluble Nano-Luteolin with PEG surface coating, there was a marked inhibition of tumor growth over time when compared to that in the luteolin group. The PEG group on the nanoparticle surface is known to decrease the nonspecific biofouling of nanoparticles in vivo, minimize nanoparticle uptake by the RES, increase the circulation time of nanoparticle, and decrease the premature clearance of nanoparticles by the mononuclear phagocytic system (36-38, 52-63). Moreover, due to the EPR effect, nanoparticles can enter into the tumor through the leaky vasculature (36-38, 52-63). Most likely due to a combination of these advantages, Nano-Luteolin is more effective in tumor growth inhibition than free luteolin. In fact, the recent study (65) also suggested that nanoencapsulated combinations of ACS (aspirin, curcumin, and free sulforaphane) showed higher efficacy even in lower doses compared to the combinations of free drugs in a chemically induced pancreatic neoplasia model.
In this study, the luteolin content inside the polymeric nanoparticle is about 1.4% by weight, resulting in the administration of a low dose of luteolin (3.3mg/Kg body weight). We believe that if we increase the amount of luteolin encapsulation, or if we can administer a higher dose of luteolin through Nano-Luteolin, which in turn will further increase the in vivo efficacy of the nanoparticles. In order to increase luteolin encapsulation, we are investigating the use of various polymers such as PHB-B-PEG, PLGA-PEG, and PEO-PPO to formulate luteolin nanoparticles. Moreover, an appropriate targeting ligand can be conjugated to the nanoparticle surface to target a specific tumor-overexpressing receptor. We will investigate this approach through in vivo experiments using appropriate animal models, and explore the use of luteolin nanoparticles as a potential candidate for chemoprevention as well as cancer therapy in clinical settings.
Acknowledgements
We acknowledge the support from Robert P. Apkarian Integrated Electron Microscopy Core, Winship Cancer Institute Cell Imaging and Microscopy Shared Resource, and Division of Animal Resources of Emory University.
Grant Support
This work was supported by grants from the Specialized Program of Excellence (SPORE) in Head and Neck Cancer (P50CA128613) and National Cancer Institute (NCI) Centers of Cancer Nanotechnology Excellence (CCNE) Program (U54CA119338).
Footnotes
Current Address for D. Majumdar: Glycosyn LLC, Medford, MA 02155, USA.
Current Address for K-H. Jung: Samsung Advanced Institute for Health Sciences & Technology, Sungkyunkwan University School of Medicine, Seoul 135-710, Republic of Korea. Department of Nuclear Medicine, Samsung Medical Center, Seoul 135-710, Republic of Korea.
References
- 1. http://www.who.int/mediacentre/factsheets/fs297/en/
- 2.Hong WK, Sporn MB. Recent advances in chemoprevention of cancer. Science. 1997;278:1073–7. doi: 10.1126/science.278.5340.1073. [DOI] [PubMed] [Google Scholar]
- 3.Amin AR, Kucuk O, Khuri FR, Shin DM. Perspectives for cancer prevention with natural compounds. J Clin Oncol. 2009;27:2712–25. doi: 10.1200/JCO.2008.20.6235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheng AL, Hsu CH, Lin JK, Hsu MM, Ho YF, Shen TS, et al. Phase I clinical trial of curcumin, a chemopreventive agent, in patients with high-risk or pre-malignant lesions. Anticancer Res. 2001;21:2895–900. [PubMed] [Google Scholar]
- 5.Pisters KM, Newman RA, Coldman B, Shin DM, Khuri FR, Hong WK, et al. Phase I trial of oral green tea extract in adult patients with solid tumors. J Clin Oncol. 2001;19:1830–8. doi: 10.1200/JCO.2001.19.6.1830. [DOI] [PubMed] [Google Scholar]
- 6.Shanafelt TD, Call TG, Zent CS, LaPlant B, Bowen DA, Roos M, et al. Phase I trial of daily oral Polyphenon E in patients with asymptomatic Rai stage 0 to II chronic lymphocytic leukemia. J Clin Oncol. 2009;27:3808–14. doi: 10.1200/JCO.2008.21.1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsao AS, Liu D, Martin J, Tang XM, Lee JJ, El-Naggar AK, et al. Phase II randomized, placebo-controlled trial of green tea extract in patients with high-risk oral premalignant lesions. Cancer Prev Res (Phila) 2009;2:931–41. doi: 10.1158/1940-6207.CAPR-09-0121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kandaswami C, Lee LT, Lee PP, Hwang JJ, Ke FC, Huang YT, et al. The antitumor activities of flavonoids. In Vivo. 2005;19:895–909. [PubMed] [Google Scholar]
- 9.Lin Y, Shi R, Wang X, Shen HM. Luteolin, a flavonoid with potential for cancer prevention and therapy. Curr Cancer Drug Targets. 2008;8:634–46. doi: 10.2174/156800908786241050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ju W, Wang X, Shi H, Chen W, Belinsky SA, Lin Y. A critical role of luteolin-induced reactive oxygen species in blockage of tumor necrosis factor-activated nuclear factor-kappaB pathway and sensitization of apoptosis in lung cancer cells. Mol Pharmacol. 2007;71:1381–8. doi: 10.1124/mol.106.032185. [DOI] [PubMed] [Google Scholar]
- 11.Cai X, Ye T, Liu C, Lu W, Lu M, Zhang J, et al. Luteolin induced G2 phase cell cycle arrest and apoptosis on non-small cell lung cancer cells. Toxicol In Vitro. 2011;25:1385–91. doi: 10.1016/j.tiv.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 12.Lee HZ, Yang WH, Bao BY, Lo PL. Proteomic analysis reveals ATP-dependent steps and chaperones involvement in luteolin-induced lung cancer CH27 cell apoptosis. Eur J Pharmacol. 2010;642:19–27. doi: 10.1016/j.ejphar.2010.05.053. [DOI] [PubMed] [Google Scholar]
- 13.Yang SF, Yang WE, Chang HR, Chu SC, Hsieh YS. Luteolin induces apoptosis in oral squamous cancer cells. J Dent Res. 2008;87:401–6. doi: 10.1177/154405910808700413. [DOI] [PubMed] [Google Scholar]
- 14.Ong CS, Zhou J, Ong CN, Shen HM. Luteolin induces G1 arrest in human nasopharyngeal carcinoma cells via the Akt-GSK-3beta-Cyclin D1 pathway. Cancer Lett. 2010;298:167–75. doi: 10.1016/j.canlet.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 15.Amin AR, Wang D, Zhang H, Peng S, Shin HJ, Brandes JC, et al. Enhanced anti-tumor activity by the combination of the natural compounds (−)-epigallocatechin-3-gallate and luteolin: potential role of p53. J Biol Chem. 2010;285:34557–65. doi: 10.1074/jbc.M110.141135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang Q, Zhao XH, Wang ZJ. Flavones and flavonols exert cytotoxic effects on a human oesophageal adenocarcinoma cell line (OE33) by causing G2/M arrest and inducing apoptosis. Food Chem Toxicol. 2008;46:2042–53. doi: 10.1016/j.fct.2008.01.049. [DOI] [PubMed] [Google Scholar]
- 17.Lim do Y, Jeong Y, Tyner AL, Park JH. Induction of cell cycle arrest and apoptosis in HT-29 human colon cancer cells by the dietary compound luteolin. Am J Physiol Gastrointest Liver Physiol. 2007;292:G66–75. doi: 10.1152/ajpgi.00248.2006. [DOI] [PubMed] [Google Scholar]
- 18.Selvendiran K, Koga H, Ueno T, Yoshida T, Maeyama M, Torimura T, et al. Luteolin promotes degradation in signal transducer and activator of transcription 3 in human hepatoma cells: an implication for the antitumor potential of flavonoids. Cancer Res. 2006;66:4826–34. doi: 10.1158/0008-5472.CAN-05-4062. [DOI] [PubMed] [Google Scholar]
- 19.Chiu FL, Lin JK. Downregulation of androgen receptor expression by luteolin causes inhibition of cell proliferation and induction of apoptosis in human prostate cancer cells and xenografts. Prostate. 2008;68:61–71. doi: 10.1002/pros.20690. [DOI] [PubMed] [Google Scholar]
- 20.Zhou Q, Yan B, Hu X, Li XB, Zhang J, Fang J. Luteolin inhibits invasion of prostate cancer PC3 cells through E-cadherin. Mol Cancer Ther. 2009;8:1684–91. doi: 10.1158/1535-7163.MCT-09-0191. [DOI] [PubMed] [Google Scholar]
- 21.Fang J, Zhou Q, Shi XL, Jiang BH. Luteolin inhibits insulin-like growth factor 1 receptor signaling in prostate cancer cells. Carcinogenesis. 2007;28:713–23. doi: 10.1093/carcin/bgl189. [DOI] [PubMed] [Google Scholar]
- 22.Wu B, Zhang Q, Shen W, Zhu J. Anti-proliferative and chemosensitizing effects of luteolin on human gastric cancer AGS cell line. Mol Cell Biochem. 2008;313:125–32. doi: 10.1007/s11010-008-9749-x. [DOI] [PubMed] [Google Scholar]
- 23.Attoub S, Hassan AH, Vanhoecke B, Iratni R, Takahashi T, Gaben AM, et al. Inhibition of cell survival, invasion, tumor growth and histone deacetylase activity by the dietary flavonoid luteolin in human epithelioid cancer cells. Eur J Pharmacol. 2011;651:18–25. doi: 10.1016/j.ejphar.2010.10.063. [DOI] [PubMed] [Google Scholar]
- 24.Manju V, Nalini N. Protective role of luteolin in 1,2-dimethylhydrazine induced experimental colon carcinogenesis. Cell Biochem Funct. 2007;25:189–94. doi: 10.1002/cbf.1305. [DOI] [PubMed] [Google Scholar]
- 25.Nishiyama N. Nanomedicine: nanocarriers shape up for long life. Nat Nanotechnol. 2007;2:203–4. doi: 10.1038/nnano.2007.88. [DOI] [PubMed] [Google Scholar]
- 26.Peer D, Karp JM, Hong S, Farokhzad OC, Margalit R, Langer R. Nanocarriers as an emerging platform for cancer therapy. Nat Nanotechnol. 2007;2:751–60. doi: 10.1038/nnano.2007.387. [DOI] [PubMed] [Google Scholar]
- 27.LaVan DA, Lynn DM, Langer R. Moving smaller in drug discovery and delivery. Nat Rev Drug Discov. 2002;1:77–84. doi: 10.1038/nrd707. [DOI] [PubMed] [Google Scholar]
- 28.LaVan DA, McGuire T, Langer R. Small-scale systems for in vivo drug delivery. Nat Biotechnol. 2003;21:1184–91. doi: 10.1038/nbt876. [DOI] [PubMed] [Google Scholar]
- 29.Moses MA, Brem H, Langer R. Advancing the field of drug delivery: taking aim at cancer. Cancer Cell. 2003;4:337–41. doi: 10.1016/s1535-6108(03)00276-9. [DOI] [PubMed] [Google Scholar]
- 30.Kawasaki ES, Player A. Nanotechnology, nanomedicine, and the development of new, effective therapies for cancer. Nanomedicine. 2005;1:101–9. doi: 10.1016/j.nano.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 31.Pridgen EM, Langer R, Farokhzad OC. Biodegradable, polymeric nanoparticle delivery systems for cancer therapy. Nanomedicine (Lond) 2007;2:669–80. doi: 10.2217/17435889.2.5.669. [DOI] [PubMed] [Google Scholar]
- 32.2007;91:863–70. [Google Scholar]
- 33.Banerjee HN, Verma M. Application of nanotechnology in cancer. Technol Cancer Res Treat. 2008;7:149–54. doi: 10.1177/153303460800700208. [DOI] [PubMed] [Google Scholar]
- 34.Parveen S, Sahoo SK. Polymeric nanoparticles for cancer therapy. J Drug Target. 2008;16:108–23. doi: 10.1080/10611860701794353. [DOI] [PubMed] [Google Scholar]
- 35.Wang AZ, Langer R, Farokhzad OC. Nanoparticle delivery of cancer drugs. Annu Rev Med. 2012;63:185–98. doi: 10.1146/annurev-med-040210-162544. [DOI] [PubMed] [Google Scholar]
- 36.Gref R, Minamitake Y, Peracchia MT, Trubetskoy V, Torchilin V, Langer R. Biodegradable long-circulating polymeric nanospheres. Science. 1994;263:1600–3. doi: 10.1126/science.8128245. [DOI] [PubMed] [Google Scholar]
- 37.Gref R, Minamitake Y, Peracchia MT, Domb A, Trubetskoy V, Torchilin V, et al. Poly(ethylene glycol)-coated nanospheres: potential carriers for intravenous drug administration. Pharm Biotechnol. 1997;10:167–98. doi: 10.1007/0-306-46803-4_6. [DOI] [PubMed] [Google Scholar]
- 38.Siddiqui IA, Adhami VM, Bharali DJ, Hafeez BB, Asim M, Khwaja SI, et al. Introducing nanochemoprevention as a novel approach for cancer control: proof of principle with green tea polyphenol epigallocatechin-3-gallate. Cancer Res. 2009;69:1712–6. doi: 10.1158/0008-5472.CAN-08-3978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sahu A, Bora U, Kasoju N, Goswami P. Synthesis of novel biodegradable and self-assembling methoxy poly(ethylene glycol)-palmitate nanocarrier for curcumin delivery to cancer cells. Acta Biomater. 2008;4:1752–61. doi: 10.1016/j.actbio.2008.04.021. [DOI] [PubMed] [Google Scholar]
- 40.Thangapazham RL, Puri A, Tele S, Blumenthal R, Maheshwari RK. Evaluation of a nanotechnology-based carrier for delivery of curcumin in prostate cancer cells. Int J Oncol. 2008;32:1119–23. [PMC free article] [PubMed] [Google Scholar]
- 41.Govender T, Riley T, Ehtezazi T, Garnett MC, Stolnik S, Illum L, et al. Defining the drug incorporation properties of PLA-PEG nanoparticles. Int J Pharm. 2000;199:95–110. doi: 10.1016/s0378-5173(00)00375-6. [DOI] [PubMed] [Google Scholar]
- 42.Yang ZL, Li XR, Yang KW, Liu Y. Amphotericin B-loaded poly(ethylene glycol)-poly(lactide) micelles: preparation, freeze-drying, and in vitro release. J Biomed Mater Res A. 2008;85:539–46. doi: 10.1002/jbm.a.31504. [DOI] [PubMed] [Google Scholar]
- 43.Blanco E, Bey EA, Dong Y, Weinberg BD, Sutton DM, Boothman DA, et al. Beta-lapachone-containing PEG-PLA polymer micelles as novel nanotherapeutics against NQO1-overexpressing tumor cells. J Control Release. 2007;122:365–74. doi: 10.1016/j.jconrel.2007.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang X, Zhang H, Tighiouart M, Lee JE, Shin HJ, Khuri FR, et al. Synergistic inhibition of head and neck tumor growth by green tea (−)-epigallocatechin-3-gallate and EGFR tyrosine kinase inhibitor. Int J Cancer. 2008;123:1005–14. doi: 10.1002/ijc.23585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen S, Cao W, Yue P, Hao C, Khuri FR, Sun S-Y. Celecoxib promotes c-FLIP degradation through AKt-independent inhibition of GSK3. Cancer Res. 2011;7:6270–81. doi: 10.1158/0008-5472.CAN-11-0838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vichai V, Kirtikara K. Sulforhodamine B colorimetric assay for cytotoxicity screening. Nat Protoc. 2006;1:1112–6. doi: 10.1038/nprot.2006.179. [DOI] [PubMed] [Google Scholar]
- 47.Ciardiello F, Bianco R, Damiano V, De Lorenzo S, Pepe S, De Placido S, et al. Antitumor Activity of Sequential Treatment with Topotecan and Anti-Epidermal Growth Factor Receptor Monoclonal Antibody C225. Clin Cancer Res. 1999;5:909–16. [PubMed] [Google Scholar]
- 48.Verma A, Uzun O, Hu Y, Hu Y, Han HS, Watson N, et al. Surface-structure-regulated cell-membrane penetration by monolayer-protected nanoparticles. Nat Mater. 2008;7:588–95. doi: 10.1038/nmat2202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nel AE, Mädler L, Velegol D, Xia T, Hoek EM, Somasundaran P, et al. Understanding biophysicochemical interactions at the nano-bio interface. Nat Mater. 2009;8:543–57. doi: 10.1038/nmat2442. [DOI] [PubMed] [Google Scholar]
- 50.Wong-Ekkabut J, Baoukina S, Triampo W, Tang IM, Tieleman DP, Monticelli L. Computer simulation study of fullerene translocation through lipid membranes. Nat Nanotechnol. 2008;3:363–8. doi: 10.1038/nnano.2008.130. [DOI] [PubMed] [Google Scholar]
- 51.Rejman J, Oberle V, Zuhorn IS, Hoekstra D. Size-dependent internalization of particles via the pathways of clathrin-and caveolae-mediated endocytosis. Biochem J. 2004;377:159–69. doi: 10.1042/BJ20031253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Riley T, Govender T, Stolnik S, Xiong CD, Garnett MC, Illum L, et al. Colloidal stability and drug incorporation aspects of micellar-like PLA-PEG nanoparticles. Colloids and Surfaces B: Biointerfaces. 1999;16:147–59. [Google Scholar]
- 53.Bazile D, Prud'homme C, Bassoullet MT, Marlard M, Spenlehauer G, Veillard M, et al. PEG-PLA nanoparticles avoid uptake by the mononuclear phagocytes system. J Pharm Sci. 1995;84:493–8. doi: 10.1002/jps.2600840420. [DOI] [PubMed] [Google Scholar]
- 54.Tobío M, Sánchez A, Vila A, Soriano II, Evora C, Vila-Jato JL, et al. The role of PEG on the stability in digestive fluids and in vivo fate of PEG-PLA nanoparticles following oral administration. Colloids Surf B Biointerfaces. 2000;18:315–23. doi: 10.1016/s0927-7765(99)00157-5. [DOI] [PubMed] [Google Scholar]
- 55.Ueki K, Onishi H, Sasatsu M, Machida Y. Preparation of carboxy-PEG-PLA nanoparticles loaded with camptothecin and their body distribution in solid tumor– bearing mice. Drug Development Research. 2009;70:512–9. [Google Scholar]
- 56.Li Y, Qi XR, Maitani Y, Nagai T. PEG-PLA diblock copolymer micelle-like nanoparticles as all-trans-retinoic acid carrier: in vitro and in vivo characterizations. Nanotechnology. 2009;20(5):2–11. doi: 10.1088/0957-4484/20/5/055106. [DOI] [PubMed] [Google Scholar]
- 57.Bazile D, Prud'homme C, Bassoullet MT, Marlard M, Spenlehauer G, Veillard M. Stealth Me.PEG-PLA nanoparticles avoid uptake by the mononuclear phagocytes system. J Pharm Sci. 1995;84:493–8. doi: 10.1002/jps.2600840420. [DOI] [PubMed] [Google Scholar]
- 58.Gref R, Lück M, Quellec P, Marchand M, Dellacherie E, Harnisch S, et al. 'Stealth' corona-core nanoparticles surface modified by polyethylene glycol (PEG):influences of the corona (PEG chain length and surface density) and of the core composition on phagocytic uptake and plasma protein adsorption. Colloids Surf B Biointerfaces. 2000;18:301–13. doi: 10.1016/s0927-7765(99)00156-3. [DOI] [PubMed] [Google Scholar]
- 59.Miura H, Onishi H, Sasatsu M, Machida Y. Antitumor characteristics of methoxypolyethylene glycol-poly(DL-lactic acid) nanoparticles containing camptothecin. J Control Release. 2004;97:101–13. doi: 10.1016/j.jconrel.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 60.Nguyen CA, Allémann E, Schwach G, Doelker E, Gurny R. Cell interaction studies of PLA-MePEG nanoparticles. Int J Pharm. 2003;254:69–72. doi: 10.1016/s0378-5173(02)00685-3. [DOI] [PubMed] [Google Scholar]
- 61.Zhan C, Gu B, Xie C, Li J, Liu Y, Lu W. Cyclic RGD conjugated poly(ethylene glycol)-co-poly(lactic acid) micelle enhances paclitaxel anti-glioblastoma effect. J Control Release. 2010;143:136–42. doi: 10.1016/j.jconrel.2009.12.020. [DOI] [PubMed] [Google Scholar]
- 62.Lemoine D, Francois C, Kedzierewicz F, Preat V, Hoffman M, Maincent P. Stability study of nanoparticles of poly(epsilon-caprolactone), poly(D,L-lactide) and poly(D,L-lactide-co-glycolide) Biomaterials. 1996;17:2191–7. doi: 10.1016/0142-9612(96)00049-x. [DOI] [PubMed] [Google Scholar]
- 63.Stefani M, Coudane J, Vert M. In vitro ageing and degradation of PEG-PLA diblock copolymer-based nanoparticles. Polymer Degradation and Stability. 2006;91:2554–9. [Google Scholar]
- 64. www.clinicaltrials.gov.
- 65.Grandhi BK, Thakkar A, Wang J, Prabhu S. A novel combinatorial nanotechnology-based oral chemopreventive regimen demonstrates significant suppresion of pancreatic cancer neoplastic lesions. Cancer Prev Res. 2013;6:1015–25. doi: 10.1158/1940-6207.CAPR-13-0172. [DOI] [PMC free article] [PubMed] [Google Scholar]