Abstract
Background
There is no uniform, standardized procedure for the treatment of persons with electrical injuries in Germany. Even if they have no risk factors, such persons are often hospitalized and observed on an intensive care unit because of concern that cardiac arrhythmia might arise some time after the initial accident. We analyzed secondary data to determine the frequency of cardiac arrhythmia in survivors of electrical accidents.
Methods
Using the hospital information system (HIS), we retrospectively identified all patients admitted to the Charité Berlin, Campus Virchow Klinikum, for the ICD diagnostic code T75.4 (effects of electric current) in the years 2001 to 2008. The data pertaining to each case were extracted from the patients’ medical records.
Results
Over the study period, 268 children and adults were admitted to our hospital with electrical injuries. All underwent cardiac rhythm monitoring, usually for more than 12 hours. On admission, 33 children (28.7%) and 33 adults (24.2%) had mild cardiac arrhythmias of various types (sinus tachycardia, sinus bradycardia, isolated extrasystoles). No patient developed a cardiac arrhythmia requiring intervention at any point in his or her hospital course.
Conclusion
Even though too few patients were included to permit any definitive conclusions from this retrospective study alone, the present findings accord with the findings of multiple earlier studies implying that asymptomatic, otherwise unharmed patients without any ECG changes may not need to be admitted to the hospital for observation. There should be an evidence-based, standardized procedure for the treatment of patients with electrical injuries, so that these patients can be cared for safely and cost-effectively.
Virtually no information is available on the prevalence of survived electrical injuries in Germany. The CHARITEM study, an analysis of Charité Berlin, evaluated the data of all 34 333 adult medical patients presenting to the Department of Emergency Medicine at the Campus Virchow-Klinikum or the Department of Emergency Medicine at the Campus Benjamin Franklin during a one-year period (2/2009 until 2/2010). Of these, 58 patients had the admission diagnosis “effects of electric current,” representing 0.17% of all emergency patients (1).
It is, according to our experience, common practice in many clinical centers in Germany to admit patients with electrical injuries to monitoring units—even if no associated signs and symptoms or diagnostic findings are present—to ensure that delayed arrhythmia can be excluded. The European Resuscitation Council Guidelines for Resuscitation 2010 recommend that “all those who survive electrical injury should be monitored in hospital if they (…) have had loss of consciousness; cardiac arrest; electrocardiographic abnormalities; soft-tissue damage and burns“ (2).
Only in a minority of hospitals these guidelines are followed closely. The fear of delayed cardiac arrhythmias is primarily fueled by case reports (3– 6); however, from these no causal relationship between electrical injury and arrhythmia can be derived.
Several clinical studies showed for pediatric and adult patients that electrical injuries were not associated with the occurrence of delayed arrhythmia; however, the case numbers in most of these studies were comparatively small (7– 10) (n = 145, 151, 212, and 31, respectively). Even studies with an exclusive focus on high-risk patients failed to show such association (11, 12) (n = 48 and n = 134).
In this study, the clinical data of all patients admitted with the ICD diagnosis T75.4 (effects of electric current) to a University hospital in Berlin during a period of eight years were retrospectively analyzed for the incidence of delayed cardiac arrhythmias.
Material and methods
The present study represents a secondary analysis of data from the hospital information system (HIS) and patient records. The clinical data of all patients admitted with the ICD diagnosis T75.4 (effects of electric current) to the Charité Berlin—Campus Virchow Medical Center between January 2001 and December 2008 were included in the analysis. No age limitations were applied. Patient identification was based on the ICD codes recorded in the HIS; an automatic search covering the above mentioned period was performed with the help of the IT department. Both primary and secondary diagnoses were included in this search.
This study’s primary endpoint, the incidence of delayed cardiac arrhythmias, was determined from the patient records. Delayed cardiac arrhythmias were defined as arrhythmias requiring treatment in patients who do not show arrhythmia after the electrical injury, i.e. who presented with no arrhythmia after the electrical accident. Since continuous cardiac rhythm monitoring was performed in many patients, but not or not continuously documented, it was accepted as evidence that the patient did not develop arrhythmia if no cardiac arrhythmia was mentioned in the patient records. The patients included in this study were not contacted or interviewed; they did not undergo any additional study-related interventions.
The study period was chosen in this way because the electronic documentation of diagnoses in the HIS started no earlier than January 2001.
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics Packages v. 19.0 and v. 20.0. The frequencies of categorical variables are reported as absolute numbers or percentages. Continuous variables are provided as medians and interquartile distances (25th and 75th percentile).
Results
Patient characteristics
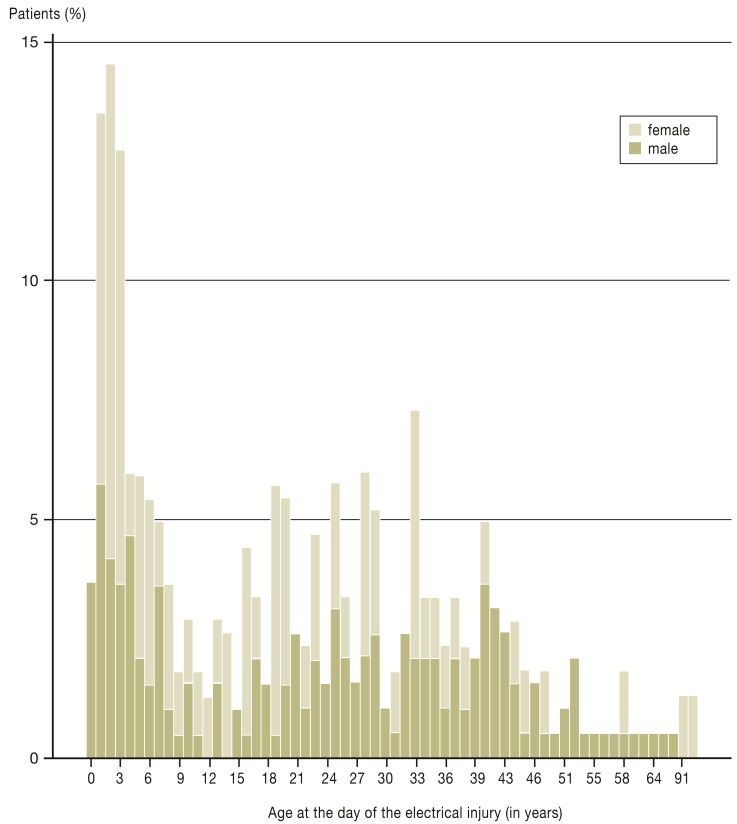
During the study period, 268 patients were admitted with the diagnosis ICD T75.4 (effects of electric current). Median patient age was 23 years (interquartile range: 6 to 35 years); the youngest patient was aged 10 months, the oldest 92 years. The majority of patients were male (Figure 1).
Figure 1.
Age and sex distribution for all electrical injury patients.
Only age categories with actual patients are depicted
The main patient characteristics, separate for the subgroups pediatric (aged 0–17 years) and adult patients (aged 18 years and over), are provided in the Table.
Table. Patient characteristics for all patients with electrical injury and separate for the age class subgroups 0–17 years (children) and ≥ 18 years (adults).
| Variable | All patients (n = 268) | Children (0–17 years) (n = 115) | Adults (≥ 18 years) (n = 153) |
|---|---|---|---|
|
Age (median [25/75 percentile]) |
23 (6/35) | 4 (2/8) | 33 (25/42) |
| Male sex | 71% (n = 191) | 64% (n = 73) | 77% (n = 118) |
Pre-existing conditions
|
83.2% (n = 223) 1.1% (n = 3) 7.6% (n = 18) 0.8% (n = 2) 1.1% (n = 3) |
89.6% (n = 73) 2.6% (n = 3) – 0.9% (n = 1) 1.7% (n = 2) |
78.4% (n = 118) – 13.3% (n = 20) 0.7% (n = 1) 0.7% (n = 1) |
| Workplace accidents | 36.9% (n = 99) | 4.3% (n = 5) | 61.4% (n = 94) |
| High-voltage accidents (>500 V) | 3.0% (n = 8) | 1.7% (n = 2) | 4.0% (n = 6) |
Power source
|
7.8% (n = 21) 28.4% (n = 76) 15.3% (n = 41) 26.5% (n = 71) 1.1% (n = 3) 18.3% (n = 49) 2.6% (n = 7) |
3.5% (n = 4) 51.3% (n = 59) 14.8% (n = 17) 19.1% (n = 22) 2.6% (n = 3) 7.0% (n = 8) 1.7% (n = 2) |
11.1% (n = 17) 11.1% (n = 17) 15.7% (n = 24) 32.0% (n = 49) – 26.8% (n = 41) 3.3% (n = 5) |
Transport to hospital
|
48.1% (n = 129) 6.3% (n = 17) 24.3% (n = 65) 17.9% (n = 48) 3.0% (n = 8) |
47.8% (n = 55) 3.5% (n = 4) 16.5% (n = 19) 26.1% (n = 30) 6.1% (n = 7) |
48.4% (n = 74) 8.5% (n = 13) 30.1% (n = 46) 11.8% (n = 18) 0.7% (n = 1) |
| Duration of hospital stay (hh:mm) | 19:50 (15:58/23:28) |
18:42 (15:33/23:15) |
20:33 (16:11/23:32) |
*missing data typically indicates self-referral;
CHD, coronary heart disease; EA+d, doctor-staffed emergency ambulance#; EA, emergency ambulance
Electrical injury
The majority of electrical injuries occur in a domestic environment (63.1%; n = 169). However, among adult patients the percentage of workplace accidents was significantly higher than that of accidents at home (61.4%; n = 94). In only 10.4% (children 13.0%, n = 15; adults 8.5%, n = 13) of cases, the accident was caused by a defective device or faulty material; in all other cases, improper use and human error were responsible for the electrical injuries. In 99.6% of patients, alternating current (AC) was the cause of the accidental injury.
Most patients arrived by foot or with their own transport at the emergency department: 47.8% (n = 55) of the pediatric and 48.4% (n = 74) of the adult patients. 20% (n = 23) of the children and 38.6% (n = 59) of the adults were brought in by emergency ambulance/ doctor-staffed emergency ambulance. In the majority of patients (94.0%; n = 252), the point of contact was the upper extremity, rarely the lower extremity (1.5%; n = 4), face (0.7%; n = 2), genitals (0.4%), or neck (0.4%).
In 32.5% (n = 87) of patients, electrical marks and in 9.8% (n = 26) electrical burns were visible at the point of entry. At the point of exit, 6.7% (n = 18) of patients showed electrical marks and 1.5% (n = 4) electrical burns. As a consequence of their exposure to electrical current, altogether 14.8% (n = 15) of the pediatric and 6.5% (n = 10) of the adult patients suffered burns (children 2.6% I°, 10.4% II°, and 1.7% III°; adults 1.3% I°, 4,6% II°, and 0,7% IV°).
Concomitant injuries were found in 2 of the pediatric and 9 of the adult patients. One of the children presented with a dislocated shoulder, the other child suffered a vertebral body fracture and a rip fracture with pneumothorax. The concomitant injuries of the adult patients included:
one shoulder dislocation
one vertebral fracture
one calcaneal fracture
one traumatic brain injury I
three contusions or sprains
one photoelectric keratitis
one traumatic brain injury I° with distorsion of the cervical spine.
Risk profile and clinical course
In 2.6% (n = 7) of patients, a family history positive for cardiovascular disease was documented (65.3% not stated). The patients’ pre-existing conditions are listed in the Table. At the time of accident, 5 patients were pregnant.
The median duration of hospital stay was 18.4 (15.3/23.5) hours in children (min.: 6 hours; max.: 430:18 hours [approx. 18 days]) and 20.3 (16.1/23.3) hours in adults (min.: 2:25 hours; max.: 406:55 hours [approx. 17 days]).
The majority of patients was monitored for more than 12 hours in the hospital; for 3 patients with no documented discharge time, this period could not be calculated. 17 patients stayed less than 12 hours in the hospital (min. 2:25h / max. 11:47h); of these, 7 were discharged against medical advice (5 patients with shorter hospital stays of 2:25h to 6:34h).
Cardiac variables and continuous cardiac monitoring
In 97.8% of patients, an admission ECG was available. On admission to hospital, 28.7% (n = 33) of the pediatric and 24.2% (n = 27) of the adult patients showed mild cardiac arrhythmias, most frequently sinus tachycardia (>100 bpm; 12.7%; n = 34), sinus bradycardia (<60 bpm; 7.8%; n = 21), isolated supraventricular (2.2%; n = 6) and ventricular (1.1%; n = 3) ectopic beats. Isolated ventricular ectopic beats were observed in one child and two adults, while in three adults the ECG showed a first-degree atrioventricular (AV) block; 11.2% of patients had an incomplete right bundle branch block.
In 61.2% (n = 164) of patients a follow-up ECG was recorded where the following abnormalities were found:
a new incomplete right bundle branch block
a new incomplete right bundle branch block with isolated supraventricular ectopic beats
in a child with complex heart defect, an incomplete right bundle branch block with isolated supraventricular ectopic beats and ventricular couplets; however, these had already been described earlier.
On admission, troponin, creatine kinase (CK), creatine kinase-myocardial band (CK-MB), and myoglobin were requested in 55.7% (n = 64) of pediatric and in 94% (n = 144) of adult patients. Troponin levels were within the normal range in all children; only in 2 adults they were found to be elevated. CK levels were elevated in 8.7% (n = 10) of pediatric and 26.1% (n = 40) of adult patients, with a CK-MB fraction >10% in 2.6% of children and 2% of adults. CK elevation was associated with concomitant injuries.
In altogether 16 patients, echocardiography was performed after admission; in 5 patients, abnormalities were detected, such as a small pericardial effusion, a thin fluid space in front of the right ventricle, a pre-existing heart valve defect, or a mild coarctation of the aorta.
All patients received continuous cardiac monitoring during their hospital stay.
In one child with numerous preexisting cardiac defects, monitoring revealed an episode of nocturnal sinus bradycardia with 51 bpm which did not require treatment. None of the patients developed higher grade arrhythmias or arrhythmias requiring treatment.
High-risk patients
In 3% of the patients (n = 8), electrical injury were caused by high-voltage (>500 V) currents.
According to the ERC criteria (ERC, European Resuscitation Council), which require cardiac monitoring, the following risk factors were found in our patient cohort:
Initial loss of consciousness in three cases, in one of these cases with cardiac arrest;
70 patients with mild ECG changes or arrhythmias
25 patients with soft-tissue damage and burns
In addition, two patients with elevated troponin levels on admission.
The complicating factors for all patients – and broken down for pediatric and adult patients – are provided in the eTable. The case illustration provides a typical example of a high-risk patient after electrical injury.
eTable. Complicating factors for all electrical injury patients and separate for adults (≥ 18 years) and children.
| Variable | All patients (n = 268) |
Adults (n = 153) |
Children (n = 153) |
|---|---|---|---|
|
Initial unconsciousness (%) |
0.7 (n = 2) |
0.7 (n = 1) |
0.9 (n = 1) |
|
Burns (%) I II III IV |
10.1 (n = 27) 1.9(n = 5) 7.1 (n = 19) 0.7 (n = 2) 0.4 (n = 1) |
6.5 (n = 10) 1.3 (n = 2) 4.6 (n = 7) – 0.7 (n = 1) |
14.8 (n = 17) 2.6 (n = 3) 10.4 (n = 12) 1.7 (n = 2) – |
| Concomitant injuries (%) | 4.2 (n = 11) | 6.2 (n = 9) | 1.8 (n = 2) |
| Admission ECG showing cardiac arrhythmias (%) | 26.1 (n = 70) | 24.2 (n = 37) | 28.7 (n = 33) |
Lab results on admission (% elevated)
|
0.7 (n = 2) 18.7 (n = 50) 2.2 (n = 6) |
1.3 (n = 2) 26.1 (n = 40) 2.0 (n = 3) |
– 8.7 (n = 10) 2.6 (n = 3) |
CK, creatine kinase; CK-MB, creatine kinase-myocardial band
Discussion
In this secondary data analysis, based on hospital data from all 268 patients admitted to hospital because of electrical injuries during the 8-year study period, none of the patients developed cardiac arrhythmia requiring treatment during their hospital stay, even though all ERC risk factors requiring cardiac monitoring were present in our cohort.
All patients received continuous ECG monitoring after admission in an ICU or observation unit.
A small number of case reports addressing delayed arrhythmias after electrical injury have been published. Bailey describes a female patient discharged home after an electrical injury event who was found dead 10 hours later; even though no ECG was available, cardiac arrhythmia was assumed as cause of death (13).
A case series by Jensen et al. described three patients who developed delayed severe ventricular arrhythmias after a time period of 8 to 12 hours between accident and arrhythmia onset. All three patients developed recurrent episodes of ventricular arrhythmia over months or years (3). In another case report, a high-voltage electrical injury sustained 8 years ago was considered to be the cause of newly diagnosed sick sinus syndrome that, however, had been causing symptoms ever since the accident (6).
Sharma et al. described a patient who, after a domestic electrical injury, was admitted to hospital with a first-degree AV block and low voltage showing in the ECG. During 24-hour monitoring, initially changing types of AV blocks developed 2 hours after admission, ultimately followed by ventricular fibrillation on the next day (4). This last case is the only case of the altogether 6 patients described here for whom an initial ECG was available; for all other patients, either no ECG or only ECGs obtained in connection with the occurrence of delayed arrhythmia were available (5).
The results of our study confirm the findings of numerous, generally small clinical studies which have so far been published on the topic:
In 1997, Arrowsmith et al. published a retrospective analysis based on the data of all 145 electrical injury patients admitted to hospital during the study period of 5 years; 75% of their patients received cardiopulmonary monitoring over at least 24 hours. In their cohort, four patients showed cardiac abnormalities; three of these patients had isolated supraventricular extrasystoles not requiring treatment. Already on hospital admission, one patient with a high-voltage electrical injury showed atrial fibrillation which was treated with digoxin. Of the four patients with ECG changes, two had experienced a high-voltage accident; all four patients suffered burns as a result of electrical injury. None of the patients included in the analysis developed higher-grade arrhythmias during the monitoring period (7). Bailey et al. conducted a prospective study in 2007 which included 134 high-risk patients after electric shock. In their study, a transthoracic pathway of the electric current, tetanic muscular contractions, unconsciousness, and high-voltage accidents (>1000 V) were regarded as risk factors. Even though 11% of the patients (n = 15) showed mild ECG changes on admission, none of them developed potentially life-threatening delayed arrhythmias during their further clinical course. None of the ECG changes required treatment (11). The same authors documented the results of cardiac monitoring in 141 children after domestic accidents—here, again, no delayed arrhythmias were observed (8).
A study by Claudet et al. arrived at the same result. The authors conducted a retrospective analysis of all pediatric patients (<15 years) with electrical injury covering a 7-year study period. In this study, 8 children showed ECG abnormalities (sinus tachycardia, incomplete right bundle branch block and negative T-waves) on admission; furthermore, 10 children were classified as high-risk patients (moist skin, chest pain on admission) (14).
A further case series by Gokdemir et al. analyzed the data from 36 children (<18 years) with electrical injury. Of these, 5 children died in hospital; among these, signs of shock, sinus tachycardia, unconsciousness, and elevated LDH levels were more frequently observed in comparison with the surviving children. Delayed arrhythmias were not described (15).
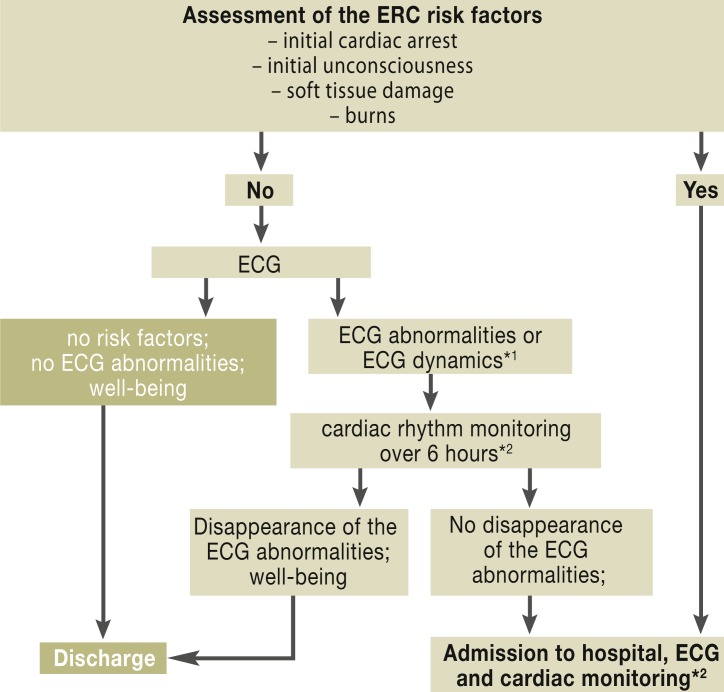
Also of interest is a study by Blackwell et al. where the authors conducted a prospective analysis of presentations to the emergency department after low-voltage electrical injury and developed a management protocol to ensure standardized care for these patients. In a 3-year observational study 212 patients presenting to the emergency department were included with a 4-year follow up after implementation of the new protocol, i.e., potential cardiac arrhythmias were documented and the new algorithm was evaluated. Asymptomatic patients without ECG changes were not admitted to hospital and received no cardiac monitoring. Using the new protocol, the authors achieved a substantial reduction in the number of hospital admissions without any negative impact on patient health (9). On the basis on this study, a standardized approach is conceivable, combining the ERC recommendations with the criteria evaluated by Blackwell et al. (Figure 2). Consequently, patients with at least one of the ERC risk factors (initial cardiac arrest, initial unconsciousness, soft-tissue damage, and burns) would be admitted to hospital immediately. An exemption would be the ERC criterion “ECG changes” which would trigger a separate algorithm in line with Blackwell et al: patients with ECG changes would initially receive monitoring over a period of six hours. If the ECG changes disappear and the patient continues to feel well, the patient could be discharged; if not, the patient would be admitted to hospital for further cardiac monitoring.
Figure 2.
Flowchart for a standard protocol for patients with electrical injury
(on the basis of the paper by Blackwell et al. 2002 [9])
*1if previous ECG is available;
*2With no prospective data available, a procedure in line with the acute coronary syndrome is recommended: Follow-up 12-channel ECG, CK and troponin after 6 hours and, if necessary, after 12 to 24 hours.
ERC, European Resuscitation Council
In contrast, asymptomatic patients with no ERC risk factors and no ECG changes would be directly discharged from hospital; they would not receive cardiac monitoring.
Conclusion
An evidence-based, standardized protocol for the management of electrical injuries should be established to ensure cost-efficient and safe patient care. So far, none of the systematic analyses based on higher case numbers of patients who sustained electrical injuries could confirm a case with delayed arrhythmia. Our study adds to the existing evidence on the topic indicating that asymptomatic, uninjured patients without ECG changes do not require hospital-based monitoring.
Limitations
The data used for this study are secondary standard care data which were not collected for research purposes. Even though the number of patients included in our analysis is relatively high compared to other studies on the topic, the case number is not sufficient to allow reliable statements on the occurrence of delayed arrhythmias after electrical injury, especially since it can be assumed that the incidence of such events is extremely low. Thus, this study should be regarded as an attempt to contribute to the collection of the evidence.
Case Illustration. A typical patient with electrical injury.
A 25-year-old electrician has sustained a work-related electrical injury and is admitted to the medical emergency department. When his left hand accidentally hit a non-insulated cable, he experienced a brief electrical shock. He was immediately separated from the power source (domestic mains). The patient experienced no initial loss of consciousness and showed no point of contact or point of exit electrical marks nor any burns or concomitant injuries. At presentation to the emergency department, the patient was symptom-free. The following vital parameters were recorded at the time of initial presentation: respiratory rate 20/min; weight 73 kg, height 192 cm, 02 saturation 98%, heart rate 76 bpm, blood pressure 108/73 mmHg.
All key laboratory values, including troponin and creatine kinase, fall within the normal range. ECG shows non-specific ST segment elevations and negative T waves. The patient is admitted to ICU for monitoring. There he receives continuous ECG monitoring and his vital parameters are checked every 2 hours. Cardiac arrhythmias are not observed at any point in time. The follow-up ECG shows a new incomplete right bundle branch block. The next day, the patient is seen by an accident insurance consultant and then discharged home symptom-free.
Key Messages.
Electrical injuries are sustained by patients of every age; among adults, the majority of electrical accidents are work-related accidents. Boys and men are more often affected than girls and women.
The European Resuscitation Council (ERC) considers survivors of electrical injury high-risk patients if they have experienced initial loss of consciousness or initial cardiac arrest, show electrocardiographic abnormalities, soft tissue damage, or burns.
So far, no standard cardiac monitoring protocol for patients with electrical injury has been established in Germany.
The concern about delayed cardiac arrhythmias stems from isolated case reports; the occurrence of delayed cardiac arrhythmias could not be confirmed in any of the systematic data analyses performed so far.
In this secondary data analysis of 268 cases, no cardiac arrhythmias requiring treatment were observed.
Acknowledgments
Translated from the original German by Ralf Thoene, MD.
Footnotes
Conflict of interest statement
Ms Maaß is an employee of Streit GmbH.
Dr. Searle, Ms Slagmann and Prof. Möckel declare that no conflict of interest exists.
References
- 1.Mockel M, Searle J, Muller R, et al. Chief complaints in medical emergencies: do they relate to underlying disease and outcome? The Charite Emergency Medicine Study (CHARITEM) Eur J Emerg Med. 2013;20:103–108. doi: 10.1097/MEJ.0b013e328351e609. [DOI] [PubMed] [Google Scholar]
- 2.Soar J, Perkins GD, Abbas G, et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 8. Cardiac arrest in special circumstances: Electrolyte abnormalities, poisoning, drowning, accidental hypothermia, hyperthermia, asthma, anaphylaxis, cardiac surgery, trauma, pregnancy, electrocution. Resuscitation. 2010;81:1400–1433. doi: 10.1016/j.resuscitation.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 3.Jensen PJ, Thomsen PE, Bagger JP, Norgaard A, Baandrup U. Electrical injury causing ventricular arrhythmias. Br Heart J. 1987;57:279–283. doi: 10.1136/hrt.57.3.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma BC, Patial RK, Pal LS, Saunkhla J, Thakur SS. Electrocardiographic manifestations following household electric current injury. J Assoc Physicians India. 1990;38:938–939. [PubMed] [Google Scholar]
- 5.Fatovich DM. Delayed lethal arrhythmia after an electrical injury. Emerg Med J. 2007;24 doi: 10.1136/emj.2007.050245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kose S, Iyisoy A, Kursaklioglu H, Demirtas E. Electrical injury as a possible cause of sick sinus syndrome. J Korean Med Sci. 2003;18:114–115. doi: 10.3346/jkms.2003.18.1.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arrowsmith J, Usgaocar RP, Dickson WA. Electrical injury and the frequency of cardiac complications. Burns. 1997;23:576–578. doi: 10.1016/s0305-4179(97)00050-8. [DOI] [PubMed] [Google Scholar]
- 8.Bailey B, Gaudreault P, Thivierge RL, Turgeon JP. Cardiac monitoring of children with household electrical injuries. Ann Emerg Med. 1995;25:612–617. doi: 10.1016/s0196-0644(95)70173-7. [DOI] [PubMed] [Google Scholar]
- 9.Blackwell N, Hayllar J. A three year prospective audit of 212 presentations to the emergency department after electrical injury with a management protocol. Postgrad Med J. 2002;78:283–285. doi: 10.1136/pmj.78.919.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wrobel N. Späte Herzrhythmusstörungen nach Stromunfällen. Late arrhythmias following accidental electric shock?] [Dtsch Med Wochenschr. 1988;113:1554–1556. doi: 10.1055/s-2008-1067849. [DOI] [PubMed] [Google Scholar]
- 11.Bailey B, Gaudreault P, Thivierge RL. Cardiac monitoring of high-risk patients after an electrical injury: a prospective multicentre study. Emerg Med J. 2007;24:348–352. doi: 10.1136/emj.2006.044677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Purdue GF, Hunt JL. Electrocardiographic monitoring after electrical injury: necessity or luxury. J Trauma. 1986;26:166–167. doi: 10.1097/00005373-198602000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Bailey B, Forget S, Gaudreault P. Prevalence of potential risk factors in victims of electrocution. Forensic Sci Int. 2001;123:58–62. doi: 10.1016/s0379-0738(01)00525-4. [DOI] [PubMed] [Google Scholar]
- 14.Claudet I, Marechal C, Debuisson C, Salanne S. Risque de trouble du rythme et électrisation par courant domestique. Risk of arrhythmia and domestic low-voltage electrical injury] [Arch Pediatr. 2010;17:343–349. doi: 10.1016/j.arcped.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 15.Gokdemir MT, Kaya H, Söğüt O, Cevik M. Factors affecting the clinical outcome of low-voltage electrical injuries in children. Pediatr Emerg Care. 2013;29:357–359. doi: 10.1097/PEC.0b013e3182854445. [DOI] [PubMed] [Google Scholar]