Abstract
Recent trends in the recreational use of pharmaceuticals among young adults in the United States highlight a number of issues regarding the problematization of drugs. Two constructions of recreational pharmaceutical use are analyzed. On the one hand, categorical frameworks based upon epidemiological data are created by institutions and media and depict recreational pharmaceutical use as illicit in unqualified, absolute terms. This is done through discourses that equate nonmedical pharmaceutical use with culturally established forms of illicit drug use. On the other hand, users’ multi-dimensional constructions of recreational pharmaceutical use emphasise social context, personal experience, and individual risk perceptions. The problematization of recreational pharmaceutical use points to intergenerational conflicts, as well as to struggles over definitions of “drug abuse” and “hard drugs”, and highlights the impact of pharmaceuticalization on recreational drug use among young people.
Keywords: Young adults, epidemiological trends, recreational pharmaceutical use, pharmaceuticalization, qualitative research, United States
Recent epidemiological trends in the recreational use of pharmaceuticals among young adults in the United States (US) highlight a number of issues regarding how drugs and drug users are problematized. This article compares some of the findings from my research on recreational pharmaceutical use in college contexts with the discursive efforts by government authorities and news media to problematize these practices and those who engage in them. This includes an examination of the cultural factors shaping this form of drug use and an emphasis on how these developments not only require us to rethink fundamental meanings commonly associated with pharmaceutical drugs and those who use them, but also to reevaluate the place of these drugs in Western society.
Two constructions of recreational pharmaceutical use are analyzed. On the one hand, categorical frameworks based upon epidemiological data are created and circulated by governing institutions and popular media and depict recreational pharmaceutical use as illicit in unqualified, absolute terms. This is done through discourses that equate nonmedical pharmaceutical use with existing, culturally established forms of illicit drug use. These discourses have several distinguishing characteristics: They define all nonmedical use as “abuse”, they create cultural correspondences between illicit “hard” drugs and pharmaceuticals, and they emphasize the user’s intent to “get high” as the primary factor motivating use.
On the other hand, the constructions of recreational pharmaceutical use reported by users describe this practice in more multi-dimensional terms which are sensitive to social context, existing personal knowledge and experience, and individual perceptions of risk, drug effects, and social outcomes. These frames for understanding recreational pharmaceutical use reveal definitions of “abuse” and experientially-grounded perceptions that differ from those offered in categorical discourses.
Finally, this paper considers the implications of this state of affairs for the construction of recreational pharmaceutical use. The problematization of this practice points to intergenerational conflicts as well as struggles over definitions of “drug abuse” and “hard drugs.” Ultimately, this process underscores the impact of pharmaceuticalization processes on recreational drug use among young people in the US.
Background
During the 1990s, an important shift in drug use patterns occurred in the US. Epidemiological data showed that greater numbers of people, especially young, college-aged adults, reported using a variety of pharmaceuticals for nonmedical purposes (Colliver, Kroutil, Dai, & Gfoerer, 2006; National Institute on Drug Abuse [NIDA], 2001). Although the category of nonmedical use includes several distinct patterns, including self-medication for physical and emotional conditions and functional use directed at increasing individual academic performance, it is the recreational aspects of this practice that have generated particular alarm in the public health literature as well as popular media (Harmon, 2005; McCarthy, 2007; Wilford, Finch, Czechowicz, & Warren, 1994).
Theoretically, it is intriguing to view these increases in the recreational use of prescription drugs within the framework of “pharmaceuticalization” – a process involving “the translation or transformation of human conditions, capabilities and capacities into opportunities for pharmaceutical intervention” (Williams, Gabe, & Davis, 2011:711). As Williams and colleagues note: “These processes potentially extend far beyond the realms of the strictly medical … to encompass … non-medical uses for lifestyle, augmentation or enhancement purposes (amongst ‘healthy’ people)” (Williams et al., 2011:711).
While some analysts highlight how pharmaceuticals have come to influence basic aspects of subjectivity in modern times (Martin, 2006; Rose, 2003), as well as the central diagnostic, regulatory, and marketing dimensions of this process (Abraham, 2011; Williams et al., 2011), there has been relatively little attention to how pharmaceuticalization shapes an important, everyday social practice among young people – recreational drug use. Currently, certain pharmaceuticals are being actively developed and aggressively marketed that focus less on treating disease and more on managing aspects of lifestyle and enhancing ordinary states and conditions, including sexual performance, body weight, sleepiness, and cognitive ability (Hall, 2003; Talbot, 2009; Wolf-Meyer, 2009). Over 40 neuro-enhancing drugs are currently under development (Williams, Seale, Boden, Lowe, & Steinberg, 2008) and some lifestyle drugs, such as Viagra (sildenafil), have already entered into the recreational arena (Graham, Polles, & Gold, 2006). These trends toward increasing enhancement stand alongside the growth of so-called “cosmetic psychopharmacology” – the therapeutic use of psychoactive drugs not necessarily to treat clinically diagnosed mental disorders but to improve a person’s perception of their psychic well-being and to allow them to shift from one essentially normal state (e.g., sadness) to another (e.g., happiness) (Elliot, 2004; Kramer, 1993; Sperry & Prosen, 1998). At the same time, the practice of off-label prescribing (the prescription of a medication in a manner different from that approved by the Food and Drug Administration) and the expansion of diagnostic criteria for some mental disorders mean that pharmaceuticals are directed at conditions for which they have not been formally evaluated for medical efficacy or for states that are ambiguously in need of treatment (Conrad & Potter, 2000; Horwitz & Wakefield, 2007; Moynihan, 2006; Stafford, 2008; Timimi, 2004). These developments underscore the fact that young adult recreational users are not alone in utilizing pharmaceuticals for nonmedical purposes. The recreational use of prescription drugs is taking place within the context of these broader cultural developments which suggests that pharmaceuticals are increasingly being integrated into everyday life by a variety of social groups (Fox & Ward, 2009).
The medication of young Americans increased significantly in the 1990s. For example, between 1985 and 1999, doctors’ visits involving prescriptions increased 29% for those under 15 years of age and 19% for those aged 15 to 24 years (Burt, 2002). Increases in the prescription rates of pain relievers and central nervous system stimulants were even more significant, rising by 94% and 327%, respectively, for those under 15 years of age (Burt, 2002:211). These trends in prescribing are apparent in a number of different contexts (LeFever, Dawson & Morrow, 1999; Pincus et al., 1996; Robison, Scalar & Galin, 1999; Rushtom & Whitmire, 2001; Safer, Zito, & Fine, 1996; and Wilens et al., 2006). As a result, a wide range of pharmaceuticals are now widely accessible to young people and they possess considerable knowledge and experience regarding medications, including dosages, indications, effects, and side effects (Anderson-Fye & Floersch, 2011; Blanco et al., 2008; McKinney & Greenfield, 2010; Quintero, Peterson, & Young, 2006; Young, 2003). This experiential base provides a measure of confidence to individuals as they consider the use of these substances in a nonmedical context (Harmon, 2005; Quintero & Bundy, 2011).
Other emerging trends in medical prescribing practice may have important implications for recreational pharmaceutical use. These include a threefold increase during the 1990s in the use of antidepressants and neuroleptic mood stabilizer anticonvulsants (valproate sodium, carbamazepine, and gabapentin), which are commonly utilized for treating bipolar disorder and depression among young people (Zito et al., 2003). Overall, there is a sharp increase in treatment with second generation anti-psychotic pharmaceuticals (Olfson, Blanco, Lui, Moreno, & Laje, 2006) as well as the off-label use of these drugs to treat several common anxiety disorders (Comer, Mojtabai, & Mark, 2011). If previous experience with stimulant medications is any indication, many of these drugs will be diverted through peer social networks and utilized non-medically (McCabe, Teter, & Boyd, 2006; Novak, Kroutil, Williams, & Brunt, 2007). Qualitative evidence indicates that while not currently as widespread as the nonmedical use of pain relievers and stimulants, some individuals are already experimenting with the recreational potential of antidepressants, including Amitriptyline, Trazodone, and Zoloft (Quintero, 2009). If these trends continue, it is not unreasonable to assume that recreational drug use in the US will become increasingly pharmaceuticalized.
In sum, the analysis presented here contributes to understanding the emerging confluence of two cultural trends in drug use, pharmaceuticalization and recreational prescription drug use, and provides insights into how specific drugs, and users, are problematized. Understanding this confluence is particularly important at this point in time because while pharmaceuticals are entering into recreational arenas to a greater degree, there has been little recognition or analysis of how the proliferation of medicines may influence trends in recreational use. In addition, on a theoretical level these developments offer a unique opportunity to analyze how licit, medical substances are repurposed through culturally symbolic discourses and images to create the perception of a social problem.
Methods
Epidemiological and media sources for the textual analysis were selected by identifying and examining key sources exemplifying professional models of pharmaceutical “abuse.” As Agar (1985) notes, professional models are frames that enjoy privileged status in society and are typically “offered by those endowed with the authority to promulgate official interpretations of drug use” (Agar, 1985:175). These models are “official” in the sense that they are disseminated by mainstream political institutions. News media sources were selected because they utilized these professional models and altered them in ways that epitomized a particular type of framing process (described below).
Texts produced by the National Institute on Drug Abuse (NIDA) were selected because of this institutions status as the primary funder of scientific research on drug use in the US. NIDA sets the agenda in drug research through various program announcements and requests for proposals including those specific to nonmedical prescription drug use. NIDA extensively disseminates research findings through both traditional academic peer-reviewed journals and fact sheets, research reports, newsletters, and various outreach and education initiatives (NIDA, 2011). Likewise, materials from the Office of National Drug Control Policy (ONDCP) were selected because it is a component of the Executive Office of the President of the United States and, as such, is uniquely positioned to advance official definitions and perceptions of drug use (ONDCP, 2011).
The qualitative data presented in this article are drawn from an exploratory study funded by NIDA (DA 016329), which consisted of 91 interviews with college students at a public university in the southwestern US. The aim of this research was to investigate the sociocultural factors related to prescription drug use among college students, as well as the risks and harms related to this practice. Data collection involved in-depth interviews that included open-ended questions as well as structured and semi-structured elements (Bernard, 2011). These interviews examined a range of drug use practices and understandings, including types of pharmaceuticals used, social settings of use, recent drug experiences, perceptions of risk and social acceptability, and outcomes.
In order to participate in an interview an individual had to meet certain criteria. They had to be 18–25 years old, an enrolled college student, and a nonmedical user of prescription drugs (defined as use in the past year of at least one prescription drug without a medical prescription or use that was contrary to medical direction). All interviews took approximately 90 minutes to complete and individuals were compensated for their participation. Recruitment and research procedures were approved by a university Institutional Review Board, and all interviewees provided written informed consent.1
Interview participants had an average age of 22 years and were mainly white (73%). The majority lived off campus (91%), with roommates (75%), and were employed (53%). About a third (31%) self-identified as Hispanic, and just over half (55%) were upper-division students or graduate students. Nearly equal proportions of men (48%) and women (52%) participated. Although no clinical criteria were utilized to determine the level or severity of drug use, interviews did include questions on lifetime, last year and most recent use of specific pharmaceuticals – that is, interview participants listed the different prescription drugs they had utilized for recreational purposes during these time frames.
These data indicate that the sample possessed a wide range of direct experience with recreational pharmaceutical use. Over their lifetimes, the pain relievers hydrocodone/acetaminophen (e.g., Lortab, Vicodin) and oxycodone/acetaminophen (e.g., Percocet, Tylox) were the two pharmaceuticals most commonly used for recreational purposes (70% and 58%, respectively), followed by the anxiolytic diazepam (Valium) (42%) (Table 1). The sample reported recreational use of a total of 68 distinctive pharmaceuticals over the lifetime, including stimulants, central nervous system depressants, anti-depressants, and lifestyle drugs (e.g., sildenafil).
Table 1.
Pharmaceuticals Most Often Used Recreationally: Lifetime
| Pharmaceutical Name (Example Brand Name) | Percent |
|---|---|
| Hydrocodone/acetaminophen (Vicodin) | 70 |
| Oxycodone/acetaminophen (Percocet) | 58 |
| Diazepam (Valium) | 42 |
| Oxycodone (OxyContin) | 36 |
| Alprazolam (Xanax) | 33 |
| Dextroamphetamine/amphetamine (Adderall) | 23 |
| Methylphenidate (Ritalin) | 22 |
| Morphine (MS Contin) | 16 |
| Propoxyphene (Darvon) | 13 |
More recent experiences displayed similar patterns with pain relievers and anxiolytics being used most often. As Table 2 indicates, oxycodone/acetaminophen was involved in a higher percentage of recent episodes (30%) than any other pharmaceutical, followed by hydrocodone/acetaminophen and oxycodone (both 25%). Diazepam (21%) and alprazolam (14%) were also commonly cited as well as dextroamphetamine/amphetamine (11%).
Table 2.
Pharmaceuticals Used Recreationally: Most Recent Episode
| Pharmaceutical Name (Example Brand Name) | Percent |
|---|---|
| Oxycodone/acetaminophen (Percocet) | 30 |
| Hydrocodone/acetaminophen (Vicodin) | 25 |
| Oxycodone (OxyContin) | 25 |
| Diazepam (Valium) | 21 |
| Alprazolam (Xanax) | 14 |
| Dextroamphetamine/amphetamine (Adderall) | 11 |
| Acetaminophen/propoxyphene (Darvocet) | 5 |
| Meperidine (Demerol) | 5 |
| Cyclobenzaprine (Flexeril) | 5 |
Interviews were audio-recorded, transcribed, and coded using NVivo (Qualitative Solutions in Research [QSR], 2002). Coding focused on patterns and themes related to nonmedical prescription drug use. Initial analysis followed a descriptive coding approach based on questions and domains from the interview and then advanced to the development of pattern codes. Pattern codes are inferential and explanatory and allow the analyst to index data that illustrates emergent themes and categories (Miles & Huberman, 1994). In the context of the research presented here, pattern coding was employed to highlight examples of themes relevant to recreational pharmaceutical use.
One of the structured data collection procedures undertaken with a subset of 21 individuals during the interviews is particularly relevant for this article: constrained pile sorts. Pile sorts are a data collection procedure whereby individuals classify a set of stimuli from a particular cultural domain into categories according to whatever criteria make sense to them (Weller & Romney, 1988). This results in a situation where items that share membership in a specific pile are more similar to each other than they are to items in other piles. By examining aggregate patterns and relationships in classification schemes, researchers use pile sorts as a means to understand how cultural knowledge is structured and shared between individuals. This technique has been used to investigate a wide range of cultural phenomena, including social relationships, recreational activities, and drugs (Lee & Antin, 2011; Weller, 1998).
Researchers typically structure pile sorts in two ways. First, the pile sorting task can be unconstrained – individuals evaluate the stimulus items and create as many or as few categories as they deem appropriate. Second, participants can be asked to create a specific number of piles – a process commonly referred to as a “constrained pile sort” (Weller & Romney, 1988). I used a modified constrained pile sort procedure to examine how college students conceptualized the “hardness” of a set of drugs.
For this procedure a set of cards, each with the name of a drug printed on it, was randomized (shuffled) and given to interviewees.2 Next, participants were asked to examine the cards and to remove any items they were unfamiliar with or were not sure how to classify. They were then asked to sort the remaining cards into two piles: “hard drugs” and “soft drugs.” After this task was completed, individuals could make changes in their classifications if they wished to do so and then asked to explain the rationales for their categorizations (e.g., “You put these drugs in the ‘hard’ pile. Why is that?”).
Individual responses from sorting procedures were aggregated and subjected to exploratory descriptive analyses in SPSS (SPSS, 2000; Weller & Romney, 1988). This process provided frequencies, percentages, and averages for each drug item. Respondents’ rationales offered during the sorting procedures for categorizing specific items were documented in interview notes, and organized through descriptive coding in NVivo (QSR, 2002).
Making the Licit Illicit: Transforming Legal Medicines into Illegal Drugs through Categorical Discourse
Concern that licit medicines were being used illicitly became prominent in 2007, when leading authorities in the federal government announced that pharmaceuticals were the second “most abused illegal drug” among young people in the US, behind only cannabis (ONDCP, 2007). Roy Bostock, Chairman of the Partnership for a Drug Free America, echoed these concerns when commenting on a survey of prescription drug use among American youth:
For the first time, our national study finds that today’s teens are more likely to have abused a prescription painkiller to get high than they are to have experimented with a variety of illegal drugs. In other words, Generation Rx has arrived (Partnership for a Drug-Free America, 2005).
The advent of “Generation Rx” presents an opportunity to examine how an emerging trend in drug use is framed as a problem. The cultural work of transforming licit medicines into illicit drugs is carried out, in part, through categorical discourses and images created and circulated by a number of stakeholders, including public health authorities, government drug control agencies, and the news media. These discourses and images operate in the following ways: they categorize all forms of nonmedical pharmaceutical use as abuse; they equate nonmedical pharmaceutical use with the use of hard drugs, and they focus on one motivation for use: getting high.
Constructing All Forms of Nonmedical Pharmaceutical Use as “Abuse”
Recreational use of pharmaceuticals, along with other nonmedical forms of use, is labeled “abuse” through a categorical drug control discourse. Consider, for instance, the following characterization of illicit pharmaceutical use provided by the Office of National Drug Control Policy (ONDCP, 2007):
Nonmedical use, misuse and abuse of prescription drugs are…defined … as use of prescription medications without medical supervision for the intentional purpose of getting high, or for some reason other than what the medication was intended.
Note the conflation that takes place in this definition: all forms of nonmedical use, misuse and abuse become indistinguishable by being reduced to two essential features – they are all uses that are not explicitly medically sanctioned and which are consciously directed at achieving pleasure. This conflation is operationalized in a manner that is familiar to any student of critical analyses of drug representations in the media (see Orcutt & Turner, [1983] for instance).
Conflating of nonmedical use, misuse, and abuse also occurs in US survey research. For example, drug surveillance systems, such as Monitoring the Future (MTF) and the National Survey on Drug Use and Health (NSDUH), typically provide raw data on behaviors that are labeled “use and/or misuse.” Thus, recent results from the MTF survey note that “the use of sedatives (barbiturates) fell steadily among 12th graders from the mid-1970s through the early 1990s” (Johnston, O’Malley, Bachman & Schulenberg, 2011:32), while the NSDUH reports that “in 2007, there were 2.5 million persons aged 12 or older who used psychotherapeutics nonmedically for the first time within the past year” (Substance Abuse and Mental Health Services Administration [MHSA], 2008:55). Note that neither source uses the word “abuse.” Data such as these, however, are then incorporated into various reports and media accounts where the same behaviors that were labeled “use/misuse” in original analyses are transformed into episodes of “abuse”. In this way, individual self-reports of nonmedical pharmaceutical use from surveys are aggregated into annual prevalence rates that, on the face of it, indicate alarming increases in the proportion of a population (usually young people) who entered the ranks of drug “abuse” over the last year. But by defining all nonmedical use in this way, even the once-in-a-lifetime experimenter is labeled a drug “abuser”.
These aggregate representations are created and circulated in a variety of ways. To take one example, consider the results of a NIDA-funded research project published in a peer-reviewed journal and then evaluated, transformed, and disseminated through governmental reports and news media. In 2005, a group of researchers published findings on the prevalence rates and correlates associated with the nonmedical use of prescription stimulants (Ritalin, Dexedrine or Adderall) among US college students (McCabe, Knight, Teter, & Wechsler, 2005). Notably, the authors of this research did not uncritically equate nonmedical use with abuse. Instead, they describe this practice simply as “nonmedical use” and the people who participate in this activity as “nonmedical users” – there is no mention of “abuse” or “abusers.” This is apparent in the title of the piece, “Non-medical use of prescription stimulants among US college students,” as well as in the presentation of results:
The life-time prevalence of nonmedical prescription stimulant use was 6.9%, past year prevalence was 4.1% and past month prevalence was 2.1%. Past year rates of nonmedical use ranged from zero to 25% at individual colleges. (McCabe et al., 2005:96, my emphasis).
A noteworthy transformation takes place, however, when these same data are reframed through forms of institutional categorical discourse and disseminated in a manner that alters fundamental meanings. A NIDA research note publication entitled “Studies Identify Factors Surrounding Rise in Abuse of Prescription Drugs by College Students” reframes the nonmedical use presented in the original research article. Under the subheading “Stimulant Abuse Nationwide” this source reports:
Men were twice as likely as women (5.8 percent versus 2.9 percent) to have abused methylphenidate (Ritalin), dextroamphetamine (Dexedrine), and amphetamine/dextroamphetamine (Adderall) (NIDA, 2006, my emphasis).
These characterizations of abuse are then publicized through various news media. The study under consideration, for instance, became the subject of a report by the USA Today, a national daily American newspaper:
Recent nationwide surveys by the University of Michigan and other researchers have indicated that the abuse of prescription drugs among young adults and teens is increasing, while the abuse of drugs such as cocaine and heroin is decreasing among those groups (Leinwand, 2005, my emphasis).
In this way, what began as an investigation of nonmedical prescription stimulant use is transformed and amplified through governmental institutions and media outlets into aggregate portrayals of pharmaceutical abuse by young people.
It is particularly noteworthy that instead of relying on clinically utilized criteria (e.g., DSM, ICD) a number of other culturally salient features are used to create the perception of abuse. These include the production of various types of epidemiological and actuarial discourses that relate nonmedical pharmaceutical use with other types of drug use and risk behaviors (McCabe et al., 2005), accounts that emphasize worst-case scenarios by associating nonmedical pharmaceutical use with serious medical emergencies and death (Drug Abuse Warning Network [DAWN], 2006; Leinwand, 2005), and comparisons that frame the magnitude of prescription drug abuse in terms of the prevalence in use of quintessentially problematic drugs such as cannabis, cocaine, and heroin (PATS, 2005; Leinwand, 2005). Additionally, illicit pharmaceutical use is associated with a range of criminal activity – for example, “rogue pharmacies” (Krebs, 2007), physicians running “pill mills” to feed rising addiction and abuse, and pharmacy robberies (Inciardi & Goode, 2007; Kaushik, 2001).
Equating Nonmedical Pharmaceutical Use with the Use of “Hard Drugs”
At the same time, news and other media sources create discourses and images that equate nonmedical pharmaceutical use with established, popularized forms of illicit drug use. This is done in a number of ways, including the circulation of slang terminology that attempts to create direct correspondences between specific pharmaceuticals and certain street drugs, as when Ritalin is dubbed “kiddie coke” or when OxyContin is given the moniker “hillbilly heroin” and characterized as a “gateway drug” (Grau, Dasgupta, & Phinney-Harvey, 2007).2
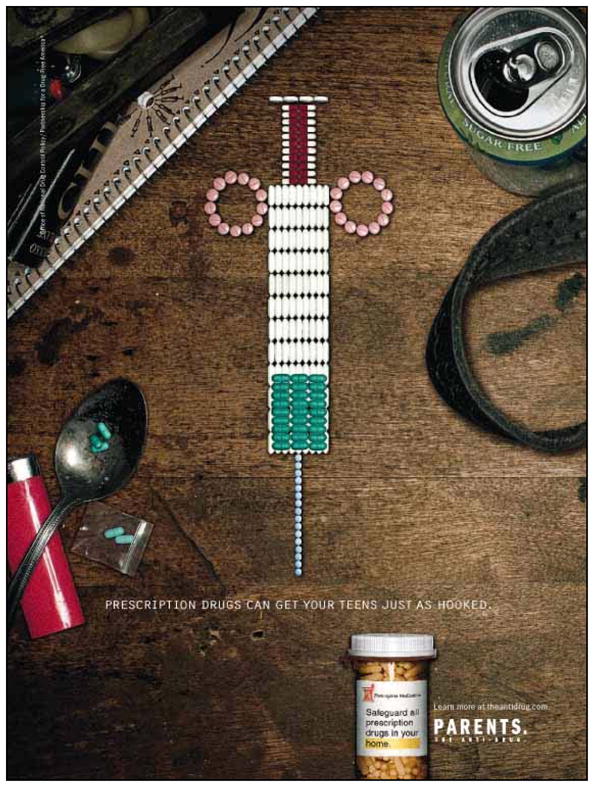
Anti-drug advertising campaigns also attempt to create this type of similarity. Take, for example, advertisements from the ONDCP directed at parents which highlight the dangers pharmaceutical drugs pose to young people. These carefully crafted images represent prescription drugs (many of which the parents themselves may have in their own medicine cabinets) as being as dangerous, damaging, and addictive as “street drugs.” These anti-drug campaigns utilize striking imagery to vividly draw associations between pharmaceutical use and the use of culturally meaningful “hard” drugs.
In one advertisement, an assortment of pharmaceutical drugs form a syringe loaded with drugs, poised to be administered through a needle made of apparently small blue Valium tablets (Figure 1). Here the syringe shape and associated equipment – a spoon, belt, plastic baggie – establish similarities between nonmedical pharmaceutical use and what is arguably the most culturally symbolic form of “hard” drug use in Western society, injecting drug use. The addictive potential of pharmaceuticals is also underscored: “Prescription drugs can get your teens just as hooked.”
Figure 1.
In another advertisement, bullet-shaped Vicodin tablets are aligned end-to-end and associated with specific drug-related equipment (e.g., a $20 bill, razor blade, tray, plastic baggie) to create equivalence between this prescription pain reliever and cocaine (Figure 2).
Figure 2.
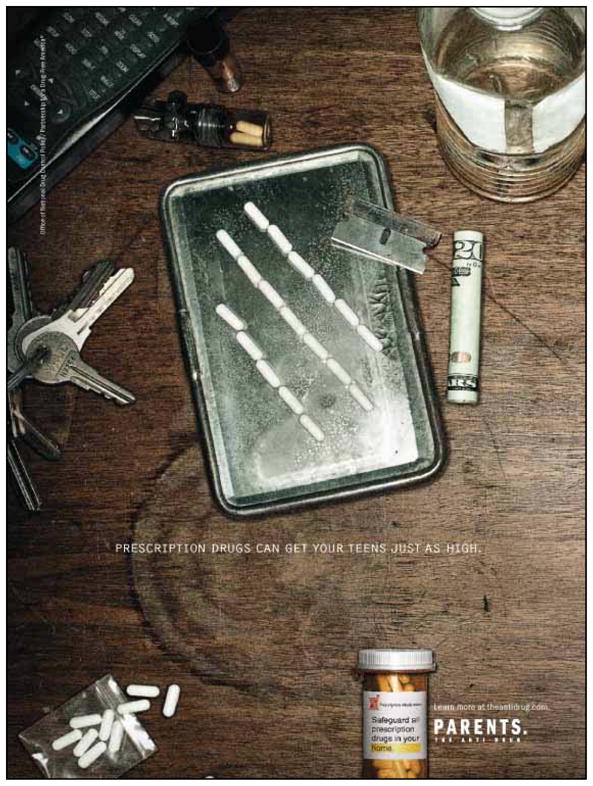
Note also the emphasis on altered states of consciousness: “Prescription drugs can get your teens just as high.” Licit medicine is made illicit through this emphasis on “getting high” and this particular intent of the user is a distinguishing feature of illicit drug use as represented in the categorical discourse. There is a special cultural prohibition directed at the intent “to get high” as an act of abuse in and of itself. Thus, prohibition is not based on the pharmacology of a drug or even its effects. Instead, the individual user’s intention becomes a principal defining criterion for the illicit nature of use. Here we move beyond simply policing states of consciousness to policing even the intent to achieve a state of consciousness. The idea that a medicine could be used because it might have a pleasurable effect is categorically deemed illicit.4
The Multi-Dimensional Discourse of Recreational Pharmaceutical Users
My qualitative research among young adults in the US, however, suggests that there is a marked discrepancy between these “official” constructions of pharmaceutical drug use and the discourses and practices of young people who engage in recreational pharmaceutical use. The following section examines the diverse ways in which they frame recreational pharmaceutical use.
Qualitative research among college students suggests that instead of drawing on categorical criteria to frame their recreational pharmaceutical use, they construct more nuanced, multi-dimensional understandings of drug use in relation to definitions of “hard” drugs, evaluations of the relative risks posed by different drugs, and definitions of “abuse.” In each of these domains, young adults challenge categorical constructions. Take, for instance, the categorical equation of any nonmedical pharmaceutical use with abuse. This definition does not tally with the activities and experiences of many young adults whose use is relatively limited and controlled, and which does not impair social function but, from their point of view, enhances it (McKinney & Greenfield, 2010; Quintero, 2009). The proliferation of pharmaceutical drugs in contemporary society ensures that many college students have direct experience with these drugs and see them used regularly by their peers to apparently no ill effect (Carter & Winseman, 2003; Fromm, 2007; Quintero et al., 2006). While there are exceptions, most notably for OxyContin, there is a general perception that irregular, episodic use of pharmaceutical drugs will not result in problems and that such drugs are no more dangerous than widely used licit drugs such as alcohol and nicotine (Quintero et al., 2006; cf. Green & Moore, 2009).
Likewise, the categorical equation of nonmedical pharmaceutical use with the use of “hard drugs” does not directly correspond to the criteria and experience base utilized by this group to formulate these types of distinctions. In assessing these depictions of recreational pharmaceutical use, it is important to bear in mind that young adults are exposed to a variety of drugs, each with their own specific risks and rewards. Individuals rarely base their understandings and evaluations of these drugs on conventional categorical constructions of medical utility and abuse, but rather draw on their personal experiences and understandings of what distinguishes “hard” drugs such as heroin from “soft” drugs like caffeine (Quintero & Bundy, 2011).
These experiences and understandings are evident in the pile sort data. Tables 3 and 4 display the descriptive results from the constrained pile sort procedure and indicate the percentage of participants who categorized a specific drug as being hard (Table 3) or soft (Table 4). These results point to considerable agreement on the extremes of each category. For example, as Table 3 illustrates, there was consensus among respondents that heroin and methamphetamine are “hard” drugs with 100% categorizing them in this way. Cocaine, LSD, and ecstasy were also commonly classified as “hard drugs.” Prescription drugs, however, occupied a more ambiguous position. One specific pharmaceutical drug, OxyContin, was considered to be a “hard drug” by almost three-quarters of the interviewees. As one participant explained, OxyContin “is the strongest of the painkillers… it’s like heroin.” Another respondent also felt that OxyContin is associated with heroin and therefore “you think of it when you say the word ‘junkie.’”
Table 3.
Percentage of Respondents Who Categorized Drug as Being “Hard”
| Heroin | 100 |
| Methamphetamine | 100 |
| Cocaine | 91 |
| Ecstasy | 86 |
| LSD | 82 |
| Oxycontin | 73 |
| Uppers | 59 |
| Mushrooms | 55 |
| Rohypnol | 50 |
| Steroids | 50 |
| Valium | 50 |
| Alcohol | 45 |
| Percocet | 45 |
| Vicodin | 41 |
| Xanax | 32 |
| Ritalin | 27 |
| Prozac | 23 |
| Adderall | 18 |
| Muscle Relaxers | 18 |
| Tobacco | 18 |
| Tylenol with Codeine | 18 |
| Marijuana | 14 |
| Zoloft | 14 |
| Dexatrim | 9 |
| Caffeine | 5 |
| Vivarin | 0 |
Table 4.
Percentage of Respondents Who Categorized Drug as Being “Soft”
| Caffeine | 95 |
| Marijuana | 86 |
| Tobacco | 82 |
| Tylenol with Codeine | 82 |
| Muscle Relaxers | 73 |
| Ritalin | 68 |
| Zoloft | 68 |
| Prozac | 64 |
| Dexatrim | 59 |
| Vicodin | 55 |
| Xanax | 55 |
| Alcohol | 50 |
| Percocet | 45 |
| Valium | 45 |
| Mushrooms | 41 |
| Steroids | 41 |
| Adderall | 36 |
| Oxycontin | 23 |
| Uppers | 23 |
| Vivarin | 18 |
| Ecstasy | 14 |
| LSD | 14 |
| Cocaine | 9 |
| Rohypnol | 5 |
| Heroin | 0 |
| Methamphetamine | 0 |
Other prescription drugs, however, were viewed differently. Of particular relevance is the position of several pharmaceuticals in relation to a very common, widely used licit drug – alcohol. In terms of “hardness,” several pharmaceuticals are seen as being more or less equivalent to alcohol, including Valium, Xanax, Ritalin, and Adderall. Converse patterns are apparent in Table 4, where a majority categorized Xanax and Vicodin as “soft drugs.” Although the difference is small, these two pharmaceuticals were considered even “softer” than alcohol. In addition, two-thirds of the interviewees classified Ritalin and Muscle Relaxers as soft drugs.
Individual rationales offered to explain these categorizations provide insight into the criteria utilized to distinguish hard from soft drugs. Interviewee comments suggest that “soft” drugs have the following characteristics: They are commonly used; they possess fewer, less intense physical, social, and mental side effects; they are legal; they are not as addictive; and they can provide positive outcomes. Exemplary quotations that capture these perceptions are provided in Table 5.
Table 5.
What Characterizes “Hard” Drugs: Interviewee Comments
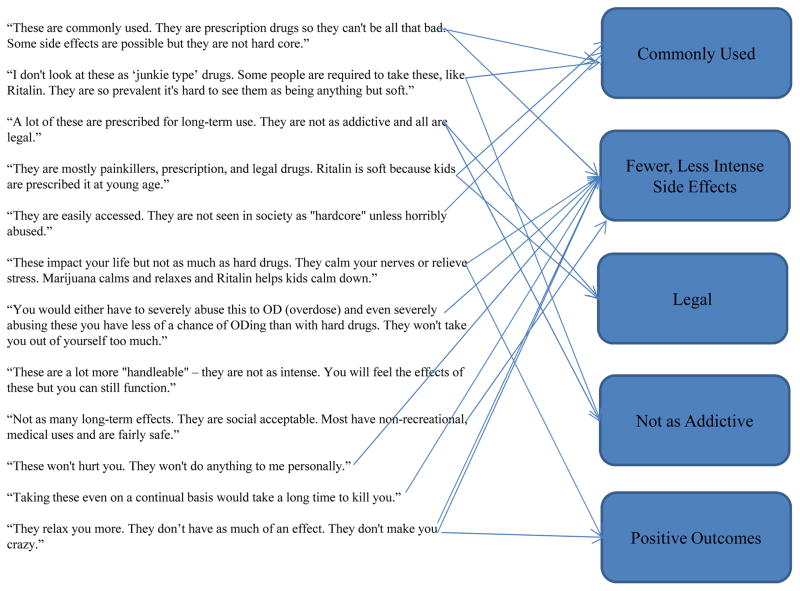
|
In contrast, “hard drugs” are those that bear some type of family resemblance to the prototype, culturally salient hard drugs heroin and methamphetamine. They are associated with more intense, negative effects, including the risk of death; they are more “addictive;” they are rarely used; and they have longer lasting impacts. Excerpts from interviews that illustrate these perceptions are detailed in Table 6.
Table 6.
What Characterizes “Soft” Drugs: Interviewee Comments
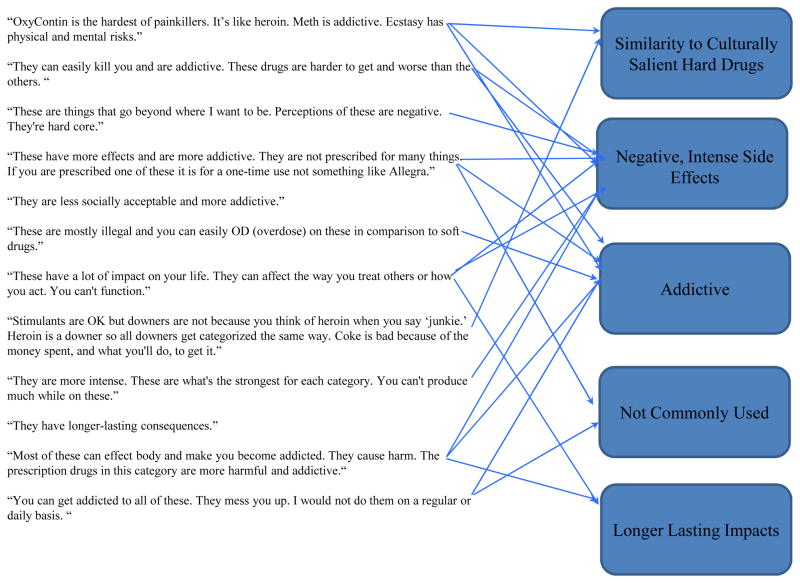
|
Thus, the categorical equation of pharmaceuticals with “hard drugs” takes little account of how users themselves make these types of evaluations. Some recreational pharmaceutical users categorize prescription drugs they were familiar with as “soft” drugs and see them as relatively safe to consume on physical and social levels (DeSantis & Curtis Hane, 2010; McKinney & Greenfield, 2010; Quintero et al., 2006; Quintero, 2009).5 There are a number of reasons for this but one of the most prominent is simply this: Young people are very familiar with a number of prescription drugs both directly and indirectly through their own medical use or their observations of family and peers (Blanco et al., 2008; Quintero, 2009; Quintero & Bundy, 2011). As a result, the comparison of pharmaceuticals with hard drugs does not map well onto the experiences and understandings of recreational pharmaceutical users themselves.
It is also important to note that some college students specifically use pharmaceuticals but explicitly avoid consuming what they consider to be “hard drugs.” In fact, prescription drugs are sometimes seen as attractive, socially acceptable alternatives to illicit drugs (cf. Bardhi, Sifaneck, Johnson, & Dunlap, 2007). Consider the flowing account offered by a 20 year-old woman. Here she recounts how she came to experiment with Codeine her first and only time at a social gathering:
We walk into the party and there were these lines of white powder on the table. And we were like, “Oh,” because none of my friends are heavy drug users like that, and we thought it was cocaine or something like that. So we were like, “Oh, God, we need to leave.” But it was really odd because it was one of our really good friends and we were like, “We didn’t know that he did this.” And we were like, “What is that?” And he was like, “Oh, it’s Codeine.” They had mashed it up and put it in lines, and they were snorting it. But I was like, I don’t want to snort it, so I put it in a drink and I drank it.
Note how pharmaceuticals are integrated into this young woman’s experimental drug-taking repertoire. There is the initial confusion that the substance on offer is a “hard” drug, followed by recognition of its acceptability for use.6
The categorical emphasis on the specific intention of “getting high” also warrants deeper analysis because it does not neatly coincide with perception and practice.7 In contrast to some reports that emphasize the user’s intention to “get high” other data indicate that achieving such a state of consciousness is important to only one set of users (Quintero, 2009). Epidemiological surveys and reports emphasize the intention to “get high” even though pharmaceutical use addresses a much wider range of social needs and cultural motivations. While hedonistic purposes can reasonably be attributed to many individuals, there are also other important dimensions to recreational pharmaceutical use.8
While young people do report the intentional utilization of pharmaceuticals in order “to get high,” they also express a number of other motives and purposes, including the use of pharmaceuticals simply to have fun in social settings or to otherwise socialize with friends and peers. Previous research uncovered several patterns of pharmaceutical misuse that are not adequately described as simply “getting high” (Quintero, 2009). Some young people do not describe their use in terms of intention to achieve a state of intoxication or pleasure, but instead emphasize the goal of facilitating social interchange and activities and personal experimentation through the consumption of pharmaceuticals. In contrast to the categorical discourse on “getting high”, these accounts center on utilizing pharmaceutical drugs to “party,” that is, to consume intoxicants while socializing with friends and peers in leisure settings (Quintero, 2009).
These uses are often described in casual terms: An individual is offered a pill at a party by a friend and takes it without any specific intent to get high, but simply because, as one 25-year-old woman described her use of Lortab, “It was there.” Young adults emphasize that this type of use was not an activity they would typically engage in – they do so only because a pharmaceutical was available in a specific social context. Thus this type of use is opportunistic and circumstantial. A 22-year-old male noted: “If there are people taking some Vicodin then I might take some, but I don’t go around looking for it. I’m not trying to find it off the street or anything.”
One question to consider is whether this self-described experimenter should be classified in the same way as someone who habitually takes pharmaceuticals with the sole intention to get high? In categorical constructions, no such distinction is made: the opportunistic one-time user, like the heavy and regular user, is labeled an “abuser.” The idea of the experimenter, however, highlights the social distinction that many young people find important – the critical difference between opportunistic, episodic use of a pharmaceutical drug for social purposes and the premeditated, habitual use for the sole purpose of “getting high” (cf. Boeri, 2004; Radcliffe & Stevens, 2008; Rødner, 2005).
For some users, the functions of recreational pharmaceutical use are not easily glossed as “getting high.” Young people, for instance, engage in this form of use in order to facilitate important social functions and activities as well as states of affect and these objectives are more important that getting high. Consider this statement (made by a 21-year-old woman) describing her use of Valium:
Valium makes me feel happier. Like if you have a little bit to drink and you’re out with your friends and you’re having a good time and you’re not drunk, you’re not buzzed, you’re just happy. That’s how it makes me feel. I feel more outgoing because I relax more. I’m more open. I’m not so tight with a situation.
In this case, achieving a high is a secondary consideration. What appears more important is the pharmaceutical drug’s capacity to enhance social interactions and activities.
Thus, young people are motivated by a range of intentions. They engage in recreational pharmaceutical use to have a good time, to be more open and outgoing in social situations, to relax, to be happy; to relieve stress, to have fun, and even to participate in “drug use” in a relatively safe manner when compared to the use of hard street drugs (Quintero et al., 2006:914–918). But an equally important aspect of pharmaceutical use is what users attempt to avoid: intoxication, undesired side effects of illicit drugs (e.g., paranoia from smoking cannabis), and the physical risks associated with hard drugs (Quintero et al., 2006:918–919). Thus, achieving a high is often not the sole or even most important priority. What appears more important is a pharmaceutical drug’s capacity to enhance social interactions and activities and states of relaxation as well as its attractiveness as an alternative to illicit drugs. Young people are not simply seeking the pleasures of intoxication, but also seeking other important states, and to enhance certain interactions and activities. They are using drugs to achieve not just states of mind, but social states and lifestyles as well.
In sum, pharmaceuticals are well integrated into the social lives and consumption practices of young adults. Far from being classified as hard street drugs, in most cases pharmaceuticals are seen as safer alternatives to those illicit substances. Recreational pharmaceutical use is targeted and strategic, being used not only to address particular emotional or physical conditions, or to achieve intoxication, but to enhance states and experiences, and engage in certain lifestyles.
Discussion
The recreational use of pharmaceutical drugs by young college students highlights several important issues. One concerns central elements of the “official” categorical discourse – cultural models of “hard drugs” and drug “abuse.” From a prevention standpoint, it is important to understand how young people evaluate and react to advertising campaigns that equate all nonmedical use with abuse and which liken almost all recreational pharmaceutical use to the consumption of hard drugs. A review of the “boomerang effects” of drug prevention programs suggests that such tactics may actually increase alcohol and other drug use (Ringold, 2002). In addition, qualitative investigations note that individual drug users attempt to avoid undesirable self-presentation as “abusers” and reject stigmatized self-identities (Radcliffe & Stevens, 2008; Rødner, 2005). Accepting categorical constructions of recreational pharmaceutical use may be problematic to the extent that these representations require individuals to see themselves in a discreditable, stigmatizing light.9
Another important issue concerns the ramifications of the categorical framing of abuse. One shortcoming of these representations is that the equation of pharmaceutical misuse with abuse may influence people to overestimate the pervasiveness of severe drug problems in a population. This may have unintended and unwelcome side-effects. For example, some analysts argue that dramatic press coverage directed at OxyContin abuse actually played an important role in fostering experimentation with this drug among youth (Inciardi & Goode, 2007). Aggregating relatively low-level prevalence data may lead young people to the conclusion that “abuse” is more common than it actually is and some research suggests that those who overestimate the extent of drug use are more likely to actually participate in these practices themselves. There are indications that this is the case, for example, with the interpretation of smoking prevalence rates by youth in the US (Nichter, 2000). This may also be the situation with alcohol use, drug use, and sexual activity (Martens et al., 2006; Reis & Riley, 2000; Wechsler et al., 2003). On a more conceptual level, the proliferation of the term abuse parallels the rise in addiction discourse noted by several analysts, and brings with it many of the same potential practical difficulties and negative effects (Ackers, 1991; Peele, 1985; Shaffer, 1991). The lack of conceptual clarity regarding what constitutes abuse can confuse efforts to define drug use problems and complicate attempts to address these issues in a systematic, efficacious manner (Shaffer, 1997).
Another set of questions concerns how the cultural model of soft and hard drugs is utilized to evaluate different sorts of substances. There appear to be discernible differences between professional and lay standards. The conventional discourse obviously attempts to play on certain aspects of this model, but without understanding and acknowledging how it is developed and deployed in real life situations. While drawing parallels between heroin and OxyContin may align closely with popular perceptions, the wholesale application of these sorts of equivalences, which make all pharmaceuticals “just like” hard drugs, not only obscures any contextual comprehension of drug use, but may also further discredit the authority of governmental institutions and the news media in the eyes of young people (Rosenbaum, 1998). One of the major limitations of this essentializing frame is that it does not examine how the hard/soft model is deployed in real life situations where young people determine the position of a specific drug on this spectrum in relation to other drugs. These types of understandings are important to examine as they relate to how individuals engage in risk assessments and harm reduction efforts. Utilizing existing cultural models to inform message and intervention development is a promising advance, but to be effective it may require learning how young adults understand the risks and benefits presented by pharmaceuticals in relation to a wide variety of drugs, licit and illicit, hard and soft.
The problematization of recreational pharmaceutical use among young adults also highlights a number of issues concerning the social construction of drug use(rs) and offers a productive site for examining a set of unique variables and social dynamics contributing to this process. The integration of prescription drugs into recreational repertoires is an object of anxiety for a number of stakeholders and, as a result, is actively contested. Classic social theory and historical case studies regarding the problematization of specific drugs and particular social segments of users illustrates a variety of means through which such practices and groups are framed, marked, and otherwise made into social problems. Individuals who occupy important social institutions utilize a number of legal, medical, and actuarial instruments and discursive practices to establish boundaries of proper behavior and society (Acker, 2002; Conrad & Schneider, 1992; Courtwright, 1988; Goode & Ben-Yehuda, 1994). These processes are often directed at groups already marked by their class, racial/ethnic status, or social position, and typically emphasize the pharmacological power of a drug to overwhelm basic aspects of individual agency, self-control, and subjectivity, as well as associations with other types of deviance, especially criminal activity (Acker, 2002). These efforts allow some segments of society to engage in social boundary maintenance and direct censure towards other groups, even as they highlight important cultural values, metaphors, and symbols (Stein, 1990; Szasz, 2003). Other discourses problematize drug use within behavioral frameworks. These practices, often with a public health inclination, use the concept of risk to characterize drug taking and certain other practices as uninformed, irrational, and pathological carried out by irresponsible, ignorant subjects (Bukoski, 1991; Lupton, 1999), while at the same time ignoring competing discourses and understandings (Hunt et al., 2007; Kelly, 2005; Mayock, 2005; Shewan, Dalgarno, & Reith, 2000).
The problematization of recreational pharmaceutical use, however, may represent a significant departure from these previous practices because it is taking place within a new context – the pharmaceuticalization of society. Debates regarding the acceptability and ethics of using some pharmaceuticals for enhancement, as well as persistent efforts to recategorize some forms of illicit drug use as medicinal, all suggest indeterminacy in cultural conceptions of legitimate medical and nonmedical uses (Greely et al., 2007; Grinspoon, 2000; Harris, 2007; Williams et al., 2008). These developments invite us to consider how the use of some licit drugs is actively framed as being illicit. In addition, these trends in pharmaceutical use, and attempts to frame them as problems, arise within a wider context where debates are taking place over how to conceptualize and assess the risk and harm wrought by the use and abuse of specific drugs (Nutt, King, & Phillips, 2010), as well as increasing efforts to categorize certain types of pharmaceutical use as “aberrant behavior” (Butler, Budman, Fernandez, & Jamison, 2004; Webster & Webster, 2005).
The problematization of recreational pharmaceutical use by young people points to the intersection of at least two underlying cultural conflicts. On one level these efforts may represent the latest rendition of the historical tension between generations (Springhall, 1999) being played out in the relatively new arena of pharmaceuticalization. Seen in this light, the problematization of recreational pharmaceutical use is part of a larger process that includes the institutionalized mistrust of young people and efforts by the state and other social institutions to subject this group to increased measures of surveillance and control (Kelly, 2003). At the same time, these competing discourses may reflect a struggle centered on maintaining collapsing cultural boundaries between pleasure and medicine in society. This involves a process where one set of uses (and users) are culturally sanctified as legitimate, while other people, practices and motivations are considered blemished – in other words, a contest between “illicit hedonism” and “therapeutic benefit” (Keane, 2008). Likewise, these competing discourses may represent more encompassing dynamics and point to ambivalence regarding fundamental cultural transformations that have taken place in the last 50 years in the US; a shift from “pharmacological Calvinism” characterized by a general wariness of drugs other than alcohol and buttressed by moral values of abstinence, to a state of “psychotherapeutic hedonism” (Klerman, 1972), the creation of “neurochemical selves” (Rose, 2003) and “cosmetic pharmacology” (Elliot, 2003) which emphasizes drug-mediated enhancement of personal interrelations, experiences, and aspects of self (Williams et al., 2008).
Finally, the recreational use of pharmaceuticals highlights a fundamental question: Are the patterns of drug use being considered here merely an example of young people taking up the basic proposition of pharmaceuticalization – that we have the right to use substances to meet lifestyle choices and enhance our lives beyond simple, institutionally defined medical need? This situation exposes a fundamental contradiction: Nonmedical pharmaceutical use is problematized in some quarters, but actively promoted in others. After all, there are presently two large-scale social efforts directed at influencing drug use in the US – a continuing war on illicit drug use and a coinciding campaign by the pharmaceutical industry to expand markets and sales through direct-to-consumer advertising, expansion of off-label prescribing, and diagnostic bracket creep (the application of biomedical disease labels and associated pharmaceutical treatments to symptoms previously considered to be nonmedical in nature [Kirmayer & Raikhel, 2009]). Thus, categorical constructions that frame nonmedical use as an illicit activity exist in a context where many types of nonmedical pharmaceutical use are openly sanctioned.
Conclusion
There are currently two countervailing cultural forces at work in relation to pharmaceutical drugs. On the one hand, institutional authorities problematize recreational pharmaceutical use by categorically defining this practice as the “abuse” of “hard drugs” in order to achieve intoxication. On the other hand, the multi-dimensional constructions of recreational pharmaceutical users are sensitive to social context, personal knowledge and experience, and individual perceptions of risk and social outcomes. These discourses exist within a wider context where the use of pharmaceutical drugs is increasingly a lifestyle choice as much as a decision related to health. Both sets of discursive constructions assume divisions between basic cultural classifications – medicine and drug, licit and illicit – that are being actively remade by pharmaceutical manufacturers and users. Because of these contradictions, discursive efforts to depict recreational pharmaceutical use as abuse will continue to underscore key symbolic and social processes involved in the problematization of drugs and users, even as they shed light on the potential limits of both the categorical discourse and the process of pharmaceuticalization.
Acknowledgments
The author gratefully acknowledges support from the National Institute on Drug Abuse (DA16329).
Footnotes
More complete descriptions of these methodological procedures, including recruiting and sampling, are provided elsewhere (Quintero et al., 2006; Quintero, 2009; Quintero, 2010).
This list of drugs was compiled from an initial set of 33 formative interviews which included a free listing activity (Bernard, 2011; Weller & Romney, 1988) where individuals were asked to list all the drugs that college students used. These responses were examined, semantically identical responses were subsumed under one label (e.g., weed and pot became marijuana), and results aggregated. Two general criteria were used to select drugs from this list to include as items for the pile sort exercise: 1) Drugs that were mentioned the most frequently and 2) drugs that were important to explore in relation to project research aims (pharmaceuticals). In addition, items were selected to reflect the range of general categories represented in the data (e.g., licit and illicit, OTC and prescription drugs, etc.).
Another example of this process occurs when news accounts of pharmaceutical exchanges portray them as being street drug deals rather than unmarked, informal transactions. Thus a number of sources tout the dangers of so-called “pharmers markets” (events involving the illicit exchange of prescription drugs between friends, peers or acquaintances; see Banta, 2005; Harmon, 2005; Whaley & Merritt 2005) and underscore the threat posed by unsavory Internet pharmacy “drug pushers” who “prey” upon children (Center for Addiction and Substance Abuse [CASA], 2004). Even parents are publicly labelled “passive pushers” for not maintaining adequate surveillance over their own medicines (CASA, 2005).
The erasure of pleasure from drug discourse has been noted by several researchers (Bourgois, 2000; Duff, 2004; Hunt, Evans, & Kares, 2007; Moore, 2008).
Similar perceptions are reported by young people in other Western social settings. Green and Moore (2009), for instance, note that young adults in Western Australia view dexamphetamine use as being relatively insignificant and “safer” in comparison to the use of other drugs, apparently because of its pharmaceutical status.
Stromberg, Nichter, and Nichter (2007) note the importance of such “play” in college student drug use, identity formation, and self-experimentation.
By focusing on the aim “to get high,” categorical constructions of illicit pharmaceutical use emphasize a limited range of ill-defined motivations to describe nonmedical use. There are a number of shortcomings to this approach. First, it is not clear just what “getting high” means. Is this meant to describe any sensation of pleasure or does it refer to more obviously impaired states of intoxication? Current categorical constructions collapse all such gradations for no obvious practical or theoretical purpose. Second, this emphasis on “getting high” as a primary motivation for consuming pharmaceuticals obscures a great deal of variability in what “getting high” actually means and how it is operationalized by young people. My qualitative research indicates variability in what constitutes “getting high” (Quintero, 2009). This includes not only simply achieving an altered state of consciousness, but also consuming specific drugs (or drug combinations) to manage the duration or intensity of a high, to experiment with and experience a new high sensation, or to substitute the sensation offered by one drug with another when the first was not readily available.
A similar point is made by Boys and colleagues (Boys, Marden, & Strang, 2001). These researchers found that relaxation, staying awake at night in order to socialize, enhancing social activities, and alleviating depressed mood were considered as important, or more important, than intoxication among young polydrug users (see also Bardhi et al. 2007; Boyd, McCabe, Cranford, & Young, 2006; McCabe, Cranford, Boyd, & Teter, 2007; Quintero et al., 2006). They also note that understanding these differences is important for the development of more relevant and appropriate prevention and treatment.
In this context it is worthwhile to note that even segments of the heroin-using population actively reject the “abuser” identity and emphasize the competent execution of social roles and controlled drug use when presenting themselves as moral subjects (Boeri, 2004).
References
- Abraham J. Sociology of pharmaceuticals development and regulation: A realist empirical research programme. In: Williams SJ, Gabe J, Davis P, editors. Pharmaceuticals and Society: Critical Discourses and Debates. West Sussex, UK: Wiley-Blackwell; 2011. pp. 54–70. [Google Scholar]
- Acker CJ. Creating the American junkie: addiction research in the classic era of narcotic control. Baltimore, MD: Johns Hopkins University Press; 2002. [Google Scholar]
- Ackers RL. Addiction: The troublesome concept. Journal of drug issues. 1991;27:777–793. [Google Scholar]
- Agar M. Folks and professionals: Different models for the interpretation of drug use. The International Journal of the Addictions. 1985;20(1):173–182. doi: 10.3109/10826088509074832. [DOI] [PubMed] [Google Scholar]
- Anderson-Fye EP, Floersch J. “I’m not your typical ‘homework stresses me out’ kind of girl”: Psychological anthropology in research on college student usage of psychiatric medications and mental health services. Ethos. 2011;39(4):501–521. doi: 10.1111/j.1548-1352.2011.01209.x. [DOI] [Google Scholar]
- Banta C. Trading for a high: An inside look at a “pharming party,” the newest venue for teenage prescription-drug abuse. Time. 2005 Jul 24; Retrieved April 16, 2012, from: http://www.time.com/time/magazine/article/0,9171,1086173,00.html.
- Bardhi F, Sifaneck SJ, Johnson BD, Dunlap E. Pills, thrills and bellyaches: Case studies of prescription pill use and misuse among marijuana/blunt smoking middle class young women. Contemporary Drug Problems. 2007;34 (1):53–101. doi: 10.1177/009145090703400104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernard HR. Research Methods in Anthropology. Lanham, MD: Rowman Altamira; 2011. [Google Scholar]
- Blanco C, Okuda M, Wright D, Hasin DS, Grant BF, Liu S, Olfson M. Mental health of college students and their non-college attending peers: Results from the National Epidemiologic Study on Alcohol Related Conditions. Archives of General Psychiatry. 2008;65 (12):1429–1437. doi: 10.1001/archpsyc.65.12.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boeri M. “Hell, I’m an addict, but I ain’t no junkie”: An ethnographic analysis of aging heroin users. Human Organization. 2004;63(2):236–245. [Google Scholar]
- Boys A, Marsden J, Strang J. Understanding reasons for drug use amongst young people: a functional perspective. Health Education Research. 2001;16(4):457–469. doi: 10.1093/her/16.4.457. [DOI] [PubMed] [Google Scholar]
- Boyd CJ, McCabe SE, Cranford JA, Young A. Adolescents’ motivations to abuse prescription medications. Pediatrics. 2006;118(6):2472–2480. doi: 10.1542/peds.2006-1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourgois P. Disciplining addictions: The bio-politics of methadone and heroin in the United States. Culture, Medicine and Psychiatry. 2000;24(2):165–195. doi: 10.1023/A:1005574918294. [DOI] [PubMed] [Google Scholar]
- Bukoski WJ. A framework for drug abuse prevention research. In: Leukefeld CG, Bukowski WJ, editors. Drug Abuse Prevention Intervention Research: Methodological Issues. National Institute on Drug Abuse; Rockville, MD: 1991. pp. 7–28.pp. 107 NIDA Research Monograph. [Google Scholar]
- Burt CW. National trends in use of medications in office-based practice, 1985–1999. Health Affairs. 2002;21 (4):206–214. doi: 10.1377/hlthaff.21.4.206. [DOI] [PubMed] [Google Scholar]
- Butler SF, Budman SH, Fernandez K, Jamison RN. Validation of a screener and opioid assessment measure for patients with chronic pain. Pain. 2004;112(1–2):65–75. doi: 10.1016/j.pain.2004.07.026. [DOI] [PubMed] [Google Scholar]
- Carter GC, Winseman JS. Increasing numbers of students arrive on college campuses on psychiatric medications. Journal of College Student Psychotherapy. 2003;18 (1):3–10. [Google Scholar]
- Center on Addiction and Substance Abuse. “You’ve got drugs!”: Prescription drug users on the internet. The National Center on Addiction and Substance Abuse at Columbia University; 2004. [Google Scholar]
- Center on Addiction and Substance Abuse. Under the counter: The diversion and abuse of controlled prescription drugs in the U.S. The National Center on Addiction and Substance Abuse at Columbia University; 2005. [Google Scholar]
- Colliver JD, Kroutil LA, Dai L, Gfoerer JC. DHHS Publication No. SMA 06-4192. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2006. Misuse of prescription drugs: Data from the 2002, 2003, and 2004 national surveys on drug use and health. [Google Scholar]
- Comer JS, Mojtabai R, Mark R. National trends in the antipsychotic treatment of psychiatric outpatients with anxiety disorders. The American Journal of Psychiatry. 2011;168 (10):1057–65. doi: 10.1176/appi.ajp.2011.11010087. [DOI] [PubMed] [Google Scholar]
- Conrad P, Potter D. From hyperactive children to ADHD adults: Observations on the expansion on medical categories. Social Problems. 2000;47:559. [Google Scholar]
- Conrad P, Schneider JW. Deviance and medicalization: from badness to sickness. Temple University Press; 1992. [Google Scholar]
- Courtwright D. Dark paradise : opiate addiction in America before 1940. Cambridge, MA: Harvard University Press; 1982. [Google Scholar]
- DeSantis AD, Curtis Hane A. “Adderall is definitely not a drug”: Justifications for the illegal use of ADHD stimulants. Substance Use & Misuse. 2010;45:31–46. doi: 10.3109/10826080902858334. [DOI] [PubMed] [Google Scholar]
- Duff C. Drug use as a ‘practice of the self’: is there any place for an ‘ethics of moderation’ in contemporary drug policy? International Journal of Drug Policy. 2004;15:385–393. [Google Scholar]
- Drug Abuse Warning Network. The New DAWN Report. Office of Applied Studies (OAS), Substance Abuse and Mental Health Services Administration (SAMHSA); 2006. Emergency department visits involving nonmedical use of selected pharmaceuticals. [Google Scholar]
- Elliott C. Introduction: Prozac as a way of life. In: Elliot C, Chambers T, editors. Prozac as a Way of Life. Chapel Hill, NC: The University of North Carolina Press; 2004. pp. 1–18. [Google Scholar]
- Fox NJ, Ward K. Pharma in the bedroom . . . and the kitchen. . . . The pharmaceuticalisation of daily life. Sociology of Health & Illness. 2009;30 (6):856–868. doi: 10.1111/j.1467-9566.2008.01114.x. [DOI] [PubMed] [Google Scholar]
- Fromm MG. The escalating use of medications by college students: What are they telling us, what are we telling them. Journal of College Student Psychotherapy. 2007;21 (3–4):27–44. [Google Scholar]
- Goode E, Ben-Yehuda N. Moral panics: culture, politics, and social construction. Annual Review of Sociology. 1994;20:149–171. [Google Scholar]
- Graham NA, Polles A, Gold MS. Performance enhancing, non-prescription use of erectile dysfunction medications. Journal of Addictive Diseases. 2006;25:S1, 61–68. [Google Scholar]
- Grau LE, Dasgupta N, Phinney-Harvey A. Illicit use of opioids: Is OxyContin® a “gateway drug”? The American Journal on Addictions. 2007;16 (3):166–173. doi: 10.1080/10550490701375293. [DOI] [PubMed] [Google Scholar]
- Green R, Moore D. ‘Kiddie drugs’ and controlled pleasure: Recreational use of dexamphetamine in a social network of young Australians. International Journal of Drug Policy. 2009;20:402–408. doi: 10.1016/j.drugpo.2008.12.002. [DOI] [PubMed] [Google Scholar]
- Greely H, Sahakian B, Harris J, Kessler RC, Gazzaniga M, Campbell P, Farah MJ. Towards responsible use of cognitive-enhancing drugs by the healthy. Nature. 2008;456:702–705. doi: 10.1038/456702a. [DOI] [PubMed] [Google Scholar]
- Grinspoon L. Whither medical marijuana? Journal of Contemporary Drug Problems. 2000;27:3–15. [Google Scholar]
- Hall SS. The quest for a smart pill. Scientific American. 2003;289:54–57. 60–65. doi: 10.1038/scientificamerican0903-54. [DOI] [PubMed] [Google Scholar]
- Harmon A. Young, assured and playing pharmacist to friends. The New York Times. 2005 Nov 16; Retrieved on April 16, 2012, from http://www.nytimes.com/2005/11/16/health/16patient.html?fta=y.
- Harris J. Enhancing evolution: The ethical case for making better people. Princeton, N.J: Princeton University Press; 2007. [Google Scholar]
- Horwitz AV, Wakefield JC. The loss of sadness: How psychiatry transformed normal sorrow into depressive disorder. New York, NY: Oxford University Press; 2007. [DOI] [PubMed] [Google Scholar]
- Hunt GP, Evans K, Kares F. Drug use and meanings of risk and pleasure. Journal of Youth Studies. 2007;10(1):73–96. doi: 10.1080/13676260600983668. [DOI] [Google Scholar]
- Inciardi JA, Goode JL. OxyContin: Miracle medicine or problem drug? In: Inciardi JA, McElrath K, editors. The American Drug Scene: An Anthology. 4. Los Angeles, CA: Roxbury; 2007. pp. 163–173. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future national results on adolescent drug use: Overview of key findings, 2010. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2011. [Google Scholar]
- Kaushik S. OxyCon game: Anatomy of a media-made drug scare. AlterNet. 2001 Jun 4; Retrieved April 16, 2012, from: http://www.alternet.org/story/10955/?page=entire.
- Helen K. Pleasure and discipline in the uses of Ritalin. International Journal of Drug Policy. 2008;19(5):401–409. doi: 10.1016/j.drugpo.2007.08.002. [DOI] [PubMed] [Google Scholar]
- Kelly P. Growing up as risky business? Risks, surveillance and the institutionalized mistrust of youth. Journal of Youth Studies. 2003;6 (2):165–180. [Google Scholar]
- Kelly BC. Conceptions of risk in the lives of club drug-using youth. Substance Use & Misuse. 2005;40:1443–1459. doi: 10.1081/JA-200066812. [DOI] [PubMed] [Google Scholar]
- Kirmayer L, Raikhel E. From Amrita to Substance D: pharmacology, political economy and technologies of the self. Transcultural Psychiatry. 2009;46:5–15. doi: 10.1177/1363461509102284. [DOI] [PubMed] [Google Scholar]
- Klerman GL. Psychotropic hedonism vs. pharmacological Calvinism. Hastings Center Report. 1972:1–3. [PubMed] [Google Scholar]
- Kramer P. Listening to Prozac. New York, NY: Penguin Books; 1993. [Google Scholar]
- Krebs B. “Rogue” internet pharmacies fueling Rx abuse, panel told. The Washington Post. 2007 May 16; Retrieved April 16, 2012, from: http://www.washingtonpost.com/wp-dyn/content/article/2007/05/16/AR2007051602015.html.
- LeFever GB, Dawson KV, Morrow AL. The extent of drug therapy for attention deficit-hyperactivity disorder among children in public schools. American Journal of Public Health. 1999;89 (9):1359–1364. doi: 10.2105/ajph.89.9.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J, Antin TMJ. How do researchers categorize drugs, and how do drug users categorize them? Contemporary Drug Problems. 2011;38(3) doi: 10.1177/009145091103800304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leinwand D. Prescription abusers not just after a high. USATODAY.com. 2005 May 5; Retrieved April 13, 2012, from: http://www.usatoday.com/news/health/2005-05-25-drugs_x.htm.
- Lupton D. Risk. New York, NY: Routledge; 1999. [Google Scholar]
- Martens MP, Page JC, Mowry ES. Differences between actual and perceived student norms: An examination of alcohol use, drug use, and sexual behavior. Journal of American College Health. 2006;54 (5):295–300. doi: 10.3200/JACH.54.5.295-300. [DOI] [PubMed] [Google Scholar]
- Martin E. The pharmaceutical person. Biosciences. 2006;1:237–287. [Google Scholar]
- Mayock P. ‘Scripting’ risk: Young people and the construction of drug journeys. Drugs: education, prevention and policy. 2005;12:349–368. [Google Scholar]
- McCabe SE, Knight JR, Teter CJ, Wechsler J. Non-medical use of prescription stimulants among US college students: prevalence and correlates from a national survey. Addiction. 2005;100 (1):96–106. doi: 10.1111/j.1360-0443.2005.00944.x. [DOI] [PubMed] [Google Scholar]
- McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use, and diversion of abusable prescription drugs. Journal of American College Health. 2006;54:269–278. doi: 10.3200/JACH.54.5.269-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Cranford JA, Boyd CJ, Teter CJ. Motives, diversion and routes of administration associated with nonmedical use of prescription opioids. Addictive Behaviors. 2007;32(3):562–575. doi: 10.1016/j.addbeh.2006.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy M. Prescription drug abuse up sharply in the USA. The Lancet. 2007;369 (9572):1505–1506. doi: 10.1016/S0140-6736(07)60690-4. [DOI] [PubMed] [Google Scholar]
- McKinney KA, Greenfield BG. Self-compliance at ‘Prozac campus’. Anthropology & Medicine. 2010;17 (2):173–185. doi: 10.1080/13648470.2010.493604. [DOI] [PubMed] [Google Scholar]
- Miles MB, Huberman AM. Qualitative data analysis: An expanded sourcebook. 2. Thousand Oaks, CA: Sage Publications; 1994. [Google Scholar]
- Moore D. Erasing pleasure from public discourse on illicit drugs: On the creation and reproduction of an absence. International Journal of Drug Policy. 2008;19:353–358. doi: 10.1016/j.drugpo.2007.07.004. [DOI] [PubMed] [Google Scholar]
- Moynihan R. Selling sickness: How the world’s biggest pharmaceutical companies are turning us all into patients. 1. New York, NY: Nation Books; 2006. [Google Scholar]
- Nichter M. Fat talk: What girls and their parents say about dieting. Cambridge, MA: Harvard University Press; 2000. [Google Scholar]
- National Institute on Drug Abuse. Research Report Series. Bethesda: National Institutes of Health; 2001. Prescription drugs: Abuse and addiction. (Publication No, 01-4881.) [Google Scholar]
- National Institute on Drug Abuse. Studies identify factors surrounding rise in abuse of prescription drugs by college students. NIDA Notes. 2006;20(4) Retrieved April 16, 2012, from: http://archives.drugabuse.gov/NIDA_Notes/NNVol20N4/Studies.html. [Google Scholar]
- Novak SP, Kroutil LA, Williams RL, Brunt DL. The nonmedical use of prescription ADHD medications: Results from a national internet panel. Substance Abuse Treatment, Prevention and Policy. 2007;2(32) doi: 10.1186/1747-597X-2-32. Retrieved April 13, 2012, from http://www.substanceabusepolicy.com/content/2/1/32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutt DJ, King LA, Phillips LD. Drug harms in the UK: a multicriteria decision analysis. The Lancet. 2010;376:1558–1565. doi: 10.1016/S0140-6736(10)61462-6. [DOI] [PubMed] [Google Scholar]
- Office of National Drug Control Policy. Teens and prescription drugs: An analysis of recent trends on the emerging drug threat. 2007 Retrieved April 13, 2012, from http://www.theantidrug.com/pdfs/TEENS_AND_PRESCRIPTION_DRUGS.pdf.
- Office of National Drug Control Policy. About ONDCP. 2011 Retrieved from: http://www.whitehouse.gov/ondcp/about.
- Olfson M, Blanco C, Liu L, Moreno C, Laje G. National trends in the outpatient treatment of children and adolescents with antipsychotic drugs. Archives of General Psychiatry. 2006;63(6):679–685. doi: 10.1001/archpsyc.63.6.679. [DOI] [PubMed] [Google Scholar]
- Orcutt JD, Turner JB. Shocking numbers and graphic accounts: Quantified images of drug problems in the print media. Social Problems. 1983;40:190–206. [Google Scholar]
- Partnership for a Drug-Free America. Generation Rx: National study reveals new category of substance abuse emerging: Teens abusing Rx and OTC medications intentionally to get high. 2005 Retrieved August 11, 2011 from http://www.drugfree.org/Portal/DrugIssue/Research/Generation_Rx_National_Study_Reveals_New_Category/Teens_Abusing_Rx_and_OTC_Medications.
- Peele S. The meaning of addiction : compulsive experience and its interpretation. Lexington, MA: Lexington Books; 1985. [Google Scholar]
- Pincus HA, Tanielian TL, Marcus SC, Olfson M, Zarin DA, Thompson J, Zito JM. Prescribing trends in psychotropic medications: Primary care, psychiatry, and other medical specialties. Journal of the American Medical Association. 1996;279 (7):526–531. doi: 10.1001/jama.279.7.526. [DOI] [PubMed] [Google Scholar]
- Quintero G, Peterson J, Young B. An exploratory study of socio-cultural factors contributing to prescription drug misuse among college students. Journal of Drug Issues. 2006;36:903–932. [Google Scholar]
- Quintero G. Rx for a party: Recreational pharmaceutical use in a collegiate setting. Journal of American College Health. 2009;58 (1):64–70. doi: 10.3200/JACH.58.1.64-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quintero G, Bundy H. “Most of the time you already know”: Pharmaceutical information assembly by young adults on the internet. Substance Use and Misuse. 2011;46:1–12. doi: 10.3109/10826084.2011.570630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qualitative Solutions in Research. NVivo (Version 9) [Computer software] Bundoora, Victoria, Australia: 2002. Available from http://www.qsrinternational.com. [Google Scholar]
- Radcliffe P, Stevens A. Are drug treatment services only for ‘thieving junkie scumbags’? Drug users and the management of stigmatised identities. Social Science & Medicine. 2008;67:1065–1073. doi: 10.1016/j.socscimed.2008.06.004. [DOI] [PubMed] [Google Scholar]
- Reis J, Riley W. Predictors of college students’ alcohol consumption: Implications for student education. The Journal of Genetic Psychology. 2000;161(3):282–291. doi: 10.1080/00221320009596711. [DOI] [PubMed] [Google Scholar]
- Ringold DJ. Boomerang effects in response to public health interventions: Some unintended consequences in the alcoholic beverage market. Journal of Consumer Policy. 2002;25:27–63. [Google Scholar]
- Robison LM, Scalar DA, Galin RS. National trends in the prevalence of attention-deficit/hyperactivity disorder and the prescribing of methylphenidate among school-age children: 1990–1995. Clinical Pediatrics. 1999;38:209–217. doi: 10.1177/000992289903800402. [DOI] [PubMed] [Google Scholar]
- Rødner S. “I am not a drug abuser, I am a drug user”: A discourse analysis of 44 drug users’ construction of identity. Addiction Research and Theory. 2005;13 (4):333–346. [Google Scholar]
- Rose N. Neurochemical selves. Society. 2003;41:46–59. [Google Scholar]
- Rosenbaum M. “Just say know” to teenagers and marijuana. Journal of Psychoactive Drugs. 1998;30:197–203. doi: 10.1080/02791072.1998.10399690. [DOI] [PubMed] [Google Scholar]
- Rushton JL, Whitmere JT. Pediatric stimulant and selective serotonin reuptake inhibitor prescription trends: 1992 to 1998. Archives of Pediatric and Adolescent Medicine. 2001;155 (5):560–565. doi: 10.1001/archpedi.155.5.560. [DOI] [PubMed] [Google Scholar]
- Safer DJ, Zito JM, Fine EM. Increased methylphenidate usage for attention deficit disorder in the 1990s. Pediatrics. 1996;98 (6):1084–1088. [PubMed] [Google Scholar]
- Shaffer HJ. Toward an epistemology of “addictive disease. Behavioral Sciences & the Law. 1991;9:269–286. [Google Scholar]
- Shaffer HJ. The most important unresolved issue in the addictions: conceptual chaos. Substance Use & Misuse. 1997;32:1573–1580. doi: 10.3109/10826089709055879. [DOI] [PubMed] [Google Scholar]
- Shewan D, Dalgarno P, Reith G. Perceived risk and risk reduction among ecstasy users: the role of drug, set, and setting. International Journal of Drug Policy. 2000;10:431–453. [Google Scholar]
- Sperry L, Prosen H. Contemporary ethical dilemmas in psychotherapy: Cosmetic psychopharmacology and managed care. American Journal of Psychotherapy. 1998;52 (1):54–63. doi: 10.1176/appi.psychotherapy.1998.52.1.54. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. NSDUH Series H-34, DHHS Publication No. SMA 08-4343. Office of Applied Studies; Rockville, MD: 2008. Results from the 2007 National Survey on Drug Use and Health: National Findings. [Google Scholar]
- Statistical Package for the Social Sciences. SPSS Base 11.5. Chicago, IL: SPSS, Inc; 2000. [Google Scholar]
- Springhall J. Youth, popular culture and moral panics: Penny gaffs to gangsta rap, 1830–1996. New York, NY: Palgrave Macmillan; 1999. [Google Scholar]
- Stafford RS. Regulating off-label drug use — rethinking the role of the FDA. New England Journal of Medicine. 2008;358:1427–1429. doi: 10.1056/NEJMp0802107. [DOI] [PubMed] [Google Scholar]
- Stein HF. In what systems do alcohol/chemical addictions make sense? Clinical ideologies and practices as cultural metaphors. Social Science & Medicine. 1990;30(9):987–1000. doi: 10.1016/0277-9536(90)90145-i. [DOI] [PubMed] [Google Scholar]
- Stromberg P, Nichter M, Nichter M. Taking play seriously: Low-level smoking among college students. Culture, Medicine and Psychiatry. 2007;31 (1):1–24. doi: 10.1007/s11013-006-9042-y. [DOI] [PubMed] [Google Scholar]
- Szasz TS. Ceremonial chemistry: the ritual persecution of drugs, addicts, and pushers. Syracuse, NY: Syracuse University Press; 2003. (Rev. ed.) [Google Scholar]
- Talbot M. The New Yorker. 2009. Apr 27, Brain gain: The underground world of ’neuroenhancment’ drugs; pp. 32–43. [PubMed] [Google Scholar]
- Timimi S. A critique of the international consensus statement on ADHD. Clinical Child and Family Psychology Review. 2004;7:59–63. doi: 10.1023/b:ccfp.0000020192.49298.7a. [DOI] [PubMed] [Google Scholar]
- Webster LR, Webster RM. Predicting aberrant behaviors in opioid-treated patients: Preliminary validation of the opioid risk tool. Pain Medicine. 2005;6 (6):432–442. doi: 10.1111/j.1526-4637.2005.00072.x. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Nelson TF, Lee JE, Seibring M, Keeling C. Perception and reality: A national evaluation of social norms marketing interventions to reduce college students’ heavy alcohol use. Journal of Studies on Alcohol. 2003;64 (4):484–494. doi: 10.15288/jsa.2003.64.484. [DOI] [PubMed] [Google Scholar]
- Weller SC. Structured interviewing and questionnaire construction. In: Bernard HR, editor. Handbook of methods in cultural anthropology. Walnut Creek, CA: Alta Mira; 1998. pp. 365–410. [Google Scholar]
- Weller SC, Romney AK. Systematic Data Collection. Newbury Park, CA: Sage Publications; 1988. [Google Scholar]
- Whaley M, Meritt G. “Pharmers” market thriving on state’s campuses; Abuse of prescription drugs becoming a huge but undocumented problem. Denver Post 2005 Feb 27; [Google Scholar]
- Wilens TE, Adler LA, Adams J, Sgambati S, Rotrosen J, Sawtelle R, Fusillo S. Misuse and diversion of stimulants prescribed for ADHD: A systematic review of the literature. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:21–31. doi: 10.1097/chi.0b013e31815a56f1. [DOI] [PubMed] [Google Scholar]
- Williams SJ, Seale C, Boden S, Lowe P, Steinberg DL. Waking up to sleepiness: Modafinil, the media and the pharmaceuticalisation of everyday/night life. Sociology of Health and Illness. 2008;30 (6):839–855. doi: 10.1111/j.1467-9566.2008.01084.x. [DOI] [PubMed] [Google Scholar]
- Williams SJ, Gabe J, Davis P. The sociology of pharmaceuticals: Progress and prospects. In: Williams SJ, Gabe J, Davis P, editors. Pharmaceuticals and Society: Critical Discourses and Debates. West Sussex, UK: Wiley-Blackwell; 2011. pp. 1–11. [Google Scholar]
- Wilford BB, Finch J, Czechowicz DJ, Warren D. An overview of prescription drug misuse and abuse: Defining the problem and seeking solutions. The Journal of Law, Medicine and Ethics. 1994;22:197–203. doi: 10.1111/j.1748-720x.1994.tb01295.x. [DOI] [PubMed] [Google Scholar]
- Wolf-Meyer M. Precipitating pharmakologies and capital entrapments: Narcolepsy and the strange cases of Provigil and Xyrem. Medical Anthropology. 2009;28 (1):11–30. doi: 10.1080/01459740802640529. [DOI] [PubMed] [Google Scholar]
- Young JR. Prozac campus: More students seek counseling and take psychiatric medications. The Chronicle of Higher Education, February. 2003;14:37–38. [Google Scholar]
- Zito JM, Safer DJ, DosReis S, Gardner JF, Magder L, Soeken K, Riddle M. Psychotropic practice patterns for youth: a 10-year perspective. Archives of Pediatrics and Adolescent Medicine. 2003;157 (1):17–25. doi: 10.1001/archpedi.157.1.17. [DOI] [PubMed] [Google Scholar]


