Abstract
Hymenolepis diminuta also known as rat tapeworm rarely causes hymenolepiasis in humans. We report a case of H. diminuta infection in an 18-year-old male farmer who presented with intermittent pruritic maculopaular rashes and dull aching left iliac fossa pain for 6 months. Patient was cured with 2 doses of praziquantel 20 mg/kg on day 0 and 7.
KEY WORDS: Hymenolepis diminuta, niclosamide, praziquantel
INTRODUCTION
Hymenolepis diminuta, the rat tapeworm is a common parasite of mice and rats. It causes occasional infection in humans. Mice, rats and occasionally humans are the definitive hosts harboring adult worms in their small intestine. Eggs are passed in their faces. Coprophilic arthropods are the intermediate hosts. The cysticercoid (larval stage) is found in these hosts. Rodents become infected by ingestion of these arthropod hosts. Foods such as grains and cereals contaminated with infected insects are the chief sources of infection.[1] Man acquires infection by ingestion of these infected arthropods harboring the cysticercoid larvae accidentally, which on release in the intestine develop into adult worms.[2] Worms are found in the small intestine and the eggs are passed in the stool. Presence of eggs in the stool specimen indicates infection.[3] H. diminuta infection in human beings is rather uncommon typically occurring as isolated cases. Different surveys have reported parasitization rates ranging between 0.001% and 5.5%.[3] The infection is most common in children. The condition is usually asymptomatic. Mild diarrhea, abdominal pain, vague gastrointestinal manifestations, arthromyalgias, transient thoracic rashes, irritability and generalized pruritus are the noted symptoms.[4] Almost all cases documented until date are in children.[5,6] We present this case because of its rarity in adults, for development of uniform treatment protocol in future and for the purpose of documentation, which will enable us to understand this disease better.
CASE REPORT
An 18-year-old male, farmer by profession presented to the out-patient department (OPD), for intermittent generalized maculopapular pruritic rash with vague left iliac fossa pain for 4-6 months. Patient had been evaluated by many physicians and dermatologists during this period, but without a final diagnosis. Many attributed this as food allergy (to sea foods). He had received albendazole, ivermectol, cetirizine and even short course oral corticosteroid (prednisolone 1 mg/kg for 10 days). At the time of admission temperature was 98°F, pulse 90/min, blood pressure 130/90 mm Hg and respiratory rate was 18/min. Examination of chest and heart did not reveal any specific abnormality. Abdominal examination did not reveal any significant objective finding. Patient was conscious without any focal neurological deficit. A provisional diagnosis of urticaria was made and thoroughly investigated. The initial laboratory investigation revealed hemoglobin was 10.6 g/dl, otal leukocyte count - 8.8 × 103/cmm, differential count - P68%, L26%, E4% and absolute eosinophil count - 380/cmm, total platelet count 220 × 103/cmm. Erythrocyte sedimentation rate - 46 1st h. Random plasma glucose was 118 mg/dl, blood urea nitrogen - 18 mg/dl, serum creatinine - 0.8 mg/dl, serum Na+- 146 mmol/l, serum K+ - 4.6 mmol/l. Urine examinations did not reveal any abnormality. Stool examination revealed numerous bile stained spherical eggs, 70-80 μm in diameter, which lacked polar filaments and presented a thick shelled outer membrane and a thin inner membrane containing six hooklets suggesting H. diminuta [Figures 1, 2 and Video 1]. Urine and blood culture were sent for aerobic culture. Allergen challenge test result was awaited. Ultrasonography of the abdomen and pelvis did not reveal any abnormality. At the end of this initial evaluation, we were at a dilemma whether to accept the diagnosis of hymenolepiasis and if at all we accept the diagnosis then how to treat it. We again ordered for the stool test for parasite and the second sample also showed eggs of H. diminuta. Three days later both the urine and blood culture did not grow any organisms and computed tomography scan of abdomen did not provide us any further information. Finally we started treatment in the line of hymenolepiasis and the patient was given praziquantel 1000 g (20 mg/kg) with breakfast on day 0. Post-treatment period was uneventful for 24 h. We discharged the patient with advice to repeat the dose after 7 days and visit the OPD after 1 month. Patient turned up after around 5 weeks and there was no relapse of the symptoms. We again searched for H. diminuta eggs in stool for two consecutive days but both the samples were found negative for any parasite. We followed-up the patient for 6 months at varying intervals and there was no sign of relapse both symptomatically and parasitologically in stool.
Figure 1.
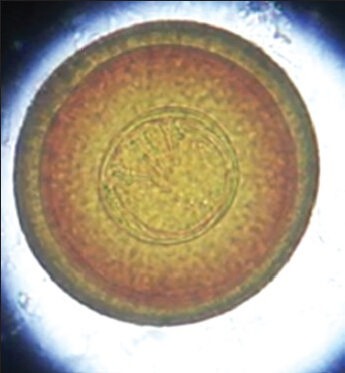
Egg of Hymenolepis diminuta in stool sample of patient
Figure 2.

Thin inner membrane of Hymenolepis diminuta egg with six hooklets
DISCUSSION
H. diminuta is prevalent world-wide, but only a few 100 human cases have been reported.[7,8,9] In developed countries, H. diminuta infection is very rare. On Medline search 48 cases of H. diminuta cases have been reported since 1965 in the United States.[10] In Spain 7 cases have been reported.[8] Isolated cases have been reported from other parts of the world like Australia, Italy, India, Malaysia, Thailand, Jamaica and Indonesia.[3] Most of the cases are documented in children and predominantly in lower socioeconomic status probably emphasizing that their food is contaminated with arthropods and there is proximity to rodents. In India a survey of 10,000 stool samples was carried out by Chandler and 23 cases of H. diminuta were found in this series.[3] Contrary to the other cases we report a case of hymenolepiasis in an 18-year-old male farmer who presented with features of intermittent pruritic maculopapular rash and dull aching pain abdomen in left iliac region. Even on extensive investigation we could not get any clue other than documenting H. diminuta in the concentrated stool sample on two occasions. Many physicians have used as many different doses. In the literatures praziquantel has been used 10 mg/kg single dose to as high as 25 mg/kg for 5 consecutive days.[4,10] Niclosamide was used in the doses of 1-2 g ranging from 5 to 15 days.[4,10] Many have repeated the dose after a variable time period. Since niclosamide was not available in our setup we preferred to use praziquantel in the dose of 20 mg/kg single dose. We repeated the dose after 7 days. There was no significant side-effect in this case except mild colicky pain abdomen on the following day. Even after following the case up to 6 months the stool sample was negative for any parasite and the patient was free of symptoms.
CONCLUSION
Humans are infected accidentally by the food contaminated by the arthropods. Though this infection is more commonly documented in children but adults are not immune. Though both praziquantel and niclosamide have been used in variable dose we used praziquantel in the dose of 20 mg/kg with breakfast and repeated the same dose on day 7. Patient was asymptomatic until 6 months and the stool samples did not reveal H. diminuta eggs after 1, 3 and 6 months of completion of treatment. There were no significant side-effects of praziquantel at this dose except mild colicky abdominal pain on the following day.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Parija SC. Textbook of Medical Parasitology. 4th ed. Ch. 11. New delhi: All India Publishers and Distributors; 2013. Cestodes: Cyclophyllidean tapeworms; p. 212. [Google Scholar]
- 2.Elminti DC. Parassitologia generale e umana. 13th ed. Milano, Italy: Casa Editrice Ambrosiana; 2004. Classe Cestoda. Ordine Cyclophillidea. Famiglia Hymenolepididae; pp. 307–9. [Google Scholar]
- 3.Watwe S, Dardi CK. Hymenolepis diminuta in a child from rural area. Indian J Pathol Microbiol. 2008;51:149–50. doi: 10.4103/0377-4929.40431. [DOI] [PubMed] [Google Scholar]
- 4.Patamia I, Cappello E, Castellano-Chiodo D, Greco F, Nigro L, Cacopardo B. A human case of Hymenolepis diminuta in a child from eastern Sicily. Korean J Parasitol. 2010;48:167–9. doi: 10.3347/kjp.2010.48.2.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Verghese SL, Sudha P, Padmaja P, Jaiswal PK, Kuruvilla T. Hymenolepis diminuta infestation in a child. J Commun Dis. 1998;30:201–3. [PubMed] [Google Scholar]
- 6.Sane SY, Irani S, Jain N, Shah KN. Hymenolepis diminuta a rare zoonotic infection report of a case. Indian J Pediatr. 1984;51:743–5. doi: 10.1007/BF02776395. [DOI] [PubMed] [Google Scholar]
- 7.Lo CT, Ayele T, Birrie H. Helminth and snail survey in Harerge region of Ethiopia with special reference to schistosomiasis. Ethiop Med J. 1989;27:73–83. [PubMed] [Google Scholar]
- 8.McMillan B, Kelly A, Walker JC. Prevalence of Hymenolepis diminuta infection in man in the New Guinea highlands. Trop Geogr Med. 1971;23:390–2. [PubMed] [Google Scholar]
- 9.Mercado R, Arias B. Taenia sp and other intestinal cestode infections in individuals from public outpatient clinics and hospitals from the northern section of Santiago, Chile (1985-1994) Bol Chil Parasitol. 1995;50:80–3. [PubMed] [Google Scholar]
- 10.Tena D, Pérez Simón M, Gimeno C, Pérez Pomata MT, Illescas S, Amondarain I, et al. Human infection with Hymenolepis diminuta: Case report from Spain. J Clin Microbiol. 1998;36:2375–6. doi: 10.1128/jcm.36.8.2375-2376.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


