Abstract
Introduction
A revised indoor air quality law has been implemented in Virginia to protect the public from the harmful effects of secondhand smoke exposure. This legislation contains exemptions that include allowances for smoking in a room that is structurally separated and separately ventilated. The objective of the current study was to examine the impact of this law on air quality in waterpipe cafés, as well as to compare the air quality in these cafés to restaurants that allow cigarette smoking and those where no smoking is permitted.
Methods
Indoor air quality in 28 venues (17 waterpipe cafés, five cigarette smoking-permitted restaurants and six smoke-free restaurants (five with valid data)) in Virginia was assessed during 4 March to 27 May 2011. Real-time measurements of particulate matter (PM) with 2.5 µm aerodynamic diameter or smaller (PM2.5) were obtained and occupant behaviour/venue characteristics were assessed.
Results
The highest mean PM2.5 concentration was observed for waterpipe café smoking rooms (374 µg/m3, n=17) followed by waterpipe café non-smoking rooms (123 µg/m3, n=11), cigarette smoking-permitted restaurant smoking rooms (119 µg/m3, n=5), cigarette smoking-permitted restaurant non-smoking rooms (26 µg/m3, n=5) and smoke-free restaurants (9 µg/m3, n=5). Smoking density was positively correlated with PM2.5 across smoking rooms and the smoke-free restaurants. In addition, PM2.5 was positively correlated between smoking and non-smoking rooms of venues.
Conclusions
The PM2.5 concentrations observed among the waterpipe cafés sampled here indicated air quality in the waterpipe café smoking rooms was worse than restaurant rooms in which cigarette smoking was permitted, and state-required non-smoking rooms in waterpipe cafés may expose patrons and employees to PM2.5 concentrations above national and international air quality standards. Reducing the health risks of secondhand smoke may require smoke-free establishments in which tobacco smoking sources such as water pipes are, like cigarettes, prohibited.
INTRODUCTION
Secondhand smoke (SHS) is a gas and particle mixture that includes mainstream smoke exhaled by cigarette smokers and sidestream smoke emitted directly from burning cigarettes.1 SHS exposure from cigarettes is associated with coronary heart disease, acute myocardial infarction, stroke, lung cancer and respiratory infection2 and accounts for ~65 000 non-smoker deaths in the USA each year.1 Interest in reducing SHS-associated risk has prompted the introduction of smoke-free laws in the USA and abroad. As of January 2012, 35 US states have passed laws that require 100% smoke-free non-hospitality workplaces and/or restaurants and/or bars.3 Many states have also introduced legislation that restricts cigarette smoking in public places, but often this type of legislation does not apply to or includes exemptions for other types of tobacco smoking (eg, cigar, waterpipe; see Noonan4). One means of assessing the effectiveness (ie, the ability to reduce SHS exposure) of such legislation is to measure changes in air quality in affected venues or geographic areas.
Continuous sampling of the concentration of a venue’s respirable suspended particles, defined as particulate matter (PM) of various sizes (<0.1 µm, ultrafine; <2.5 µm, PM2.5; <10 µm, PM10), can be used to evaluate air quality. In fact, the US Environmental Protection Agency (EPA) uses PM2.5 concentrations to quantify air quality and has set guidelines that limit daily (24 h average) PM2.5 exposure to 35 µg/m3 and annual (annual average concentration) exposure to 15 µg/m3.5 PM2.5 is an effective and commonly used marker of SHS.6 For example, a device used to measure indoor air quality unobtrusively and in real-time (SidePak Personal Aerosol Monitor) has allowed for examination of the impact of comprehensive smoke-free air legislation, whereby all indoor smoking is prohibited. In seven Kentucky communities where a comprehensive indoor smoking ban was instituted, pre-ban PM2.5 levels in bars and restaurants ranged from 67 to 304 µg/m3 and dropped significantly to a range of 9–32 µg/m3 after the ban.7 Similar reductions in PM2.5 levels have also been observed in various hospitality locations in Western New York (eg, 85% decline8). Additionally, this work has demonstrated differences in PM2.5 reductions between bans which are comprehensive (Lexington, Kentucky) versus those which include many exemptions (Louisville, Kentucky).9 The comprehensive Lexington-based ban resulted in an overall PM2.5 level an order of magnitude lower (18 µg/m3) than pre-ban levels. In contrast, the limited ban in Louisville had little effect on overall PM levels (PM2.5 of 338 µg/m3).9 Importantly, PM2.5 concentration was related directly to the number of cigarettes smoked in a venue during the sampling period, highlighting the fact that cigarette smoking is an important source of PM2.5. In sum, laws that reduce indoor cigarette smoking are effective at reducing SHS as indexed by indoor air concentrations of PM2.5. However, in the US and elsewhere, many people smoke tobacco using methods that may not be affected by smoke-free legislation, such as waterpipe tobacco smoking.
Waterpipe tobacco smoking involves passing smoke through water prior to inhalation and typically involves burning charcoal to heat the tobacco.10,11 This mode of tobacco use is surprisingly common among adolescents and young adults in the USA.12,13 For example, in one cross-sectional sample of 3770 college students in North Carolina, 17% reported current waterpipe use.12 Alarmingly, early evidence among waterpipe tobacco smokers indicates increased risk for tobacco-related disease including lung cancer, chronic obstructive lung disease and periodontal disease.14,15 In fact, many of the same carcinogens and smoke constituents associated with adverse health effects found in cigarette smoke are also detected in significant quantities in waterpipe smoke.16–18 Like cigarette smoking, waterpipe smoking also produces considerable PM2.5 when measured in a controlled laboratory (406 µg/m3)19 or in a café setting (464 µg/m3).20 However, in many US localities (eg, California, Illinois, New Mexico), waterpipe cafés escape smoke-free legislation by defining themselves as ‘tobacco retail shops’, being owner operated or avoiding alcohol sales.4 For example in 2007, out of 21 US states and the District of Columbia that have some of the strongest tobacco control laws, 16 had exceptions for retail tobacco establishments and seven had exceptions for tobacco/cigar lounges.21 In concert with these exceptions, there has been little to no publically available assessment of how waterpipe smoking venues adapt or comply with these laws. In Virginia, the Virginia Indoor Clean Air Act (VICAA; revised version implemented on 1 December 2009) banned smoking in most public places with only a few exceptions: restaurants located on the premises of a manufacturer of tobacco products, any portion of a restaurant that is used exclusively for private functions, any portion of a restaurant that is structurally separated (ie, constructed with a door, separately vented and contains a public entrance that enters a non-smoking area) or private clubs. In addition, if a restaurant/café limits their services to pre-packaged food and bottled/canned drinks, the ban does not apply.22 Virginia’s Governor specifically noted that waterpipe cafés are included in this legislation.23
Although previous laboratory-based work shows that waterpipe smoking increases PM concentration, there are no published reports of PM levels in US waterpipe cafés. Importantly, no study has compared directly the PM levels of waterpipe and cigarette smoking venues. There are also no studies examining the influence of smoking regulations on SHS in waterpipe cafés or how these venues are adapted structurally and/or procedurally to comply with the law. The implementation of such legislation in Virginia provides an opportunity to address these knowledge gaps. The purpose of the current study was to measure the PM levels in waterpipe cafés and restaurants/bars that allow smoking and those that do not. Results will provide novel information regarding waterpipe SHS effects on air quality as well as determine the effectiveness of regulatory efforts in guarding the public against SHS exposure.
METHODS
Venue selection
Between 4 March and 27 May 2011, indoor air quality (PM2.5) and occupant behaviour was measured inside 28 enclosed commercial venues in the state of Virginia. Selected study venues were distributed across the five health planning regions of Virginia (Northern, Southwest, West Central, East Central and Eastern Region; http://www.vdh.virginia.gov/). Within each region, at least two venues that allowed waterpipe smoking (eg, waterpipe cafés) were identified. Next, purposeful sampling was used to identify one restaurant that permitted cigarette smoking and one smoke-free restaurant within a 5-mile radius of at least one of the identified waterpipe cafés in each region. This technique was used to include venues that had similar public accessibility. For each region, at least four venues were sampled (two to four waterpipe cafés, one cigarette smoking-permitted restaurant, one smoke-free restaurant).
Materials
The TSI (Shoreview, Minnesota, USA) Sidepak AM510 Personal Aerosol Monitor was used to monitor PM2.5 levels. The Sidepak measures PM2.5 using light scattering and has been extensively validated for measuring tobacco smoke pollution.8,9,24–26 The TSI Sidepak is a continuous monitoring device that provides minute-by-minute concentrations of PM2.5. In addition, maximum occupancy, availability of alcohol/food and adherence to the VICAA (ie, structurally separate non-smoking room) were recorded and venue dimensions were determined using an infrared laser (1–100 ft; Craftsman Compact Laser Measuring Tool). Upon entry, every 15 min thereafter, and immediately before exiting each venue/room, the number of people present and the number of burning cigarettes/waterpipes were counted. The active smoker density was calculated by determining the average number of burning cigarettes/waterpipes per 100 m3.8,27
Sampling procedure
A team of at least two trained research assistants visited each venue and completed all assessments. Prior to each sampling session, the monitor was calibrated according to previously reported methods and manufacturer specifications. To maintain unobtrusive measurement, monitors were concealed in a closed handbag or backpack, except for a small portion of the Tygon tubing that protruded from one corner of the bag. TSI Sidepak measurement began 5 min prior to entry of the venue, continued for at least 30 min inside the venue and concluded with an additional 5 min of measurement after exiting each venue. For each room sampled in waterpipe cafés, cigarette smoking-permitted venues and smoke-free venues, air quality sampling and behaviour monitoring was performed for a minimum of 30 min. If a non-smoking room was present in a waterpipe café or cigarette smoking-permitted venue, research assistants transitioned between rooms and sampling and behaviour monitoring continued for another minimum of 30 min. The order of room measurement (smoking to non-smoking vs non-smoking to smoking) was counterbalanced across venues. Upon entering, research assistants sat or stood in a central location, and the sampler was kept at least at table level and was set to average 60 consecutive 1 s measurements (ie, a 1 min log interval). Based on our previous research,28 waterpipe cafés are most active during the late evening/early morning hours on Thursdays, Fridays and Saturdays, and thus, all study venues were sampled on either Friday or Saturday nights between 21:00 and 02:00. Each venue was visited once for air quality and behaviour monitoring, and four venues were revisited for dimension measurement due to equipment malfunction.
Data analysis
For each venue/room sampled, the first and last minute of logged PM2.5 data was discarded and the remaining data points were averaged to determine the mean PM2.5 concentration. There is no established waterpipe-specific calibration factor for the TSI Sidepak, although preliminary research indicates this calibration factor to be 0.37.29 A conservative calibration factor of 0.32, appropriate for cigarette SHS, was applied to all the PM2.5 data in this study, although this calibration factor may underestimate PM2.5 levels from waterpipe smoke.9,24,30 Each venue/room was grouped into categories based on the type of venue (waterpipe café, cigarette smoking-permitted restaurant or smoke-free restaurant) and room visited (smoking or non-smoking). Data were analysed using IBM SPSS (V.19), and due to the small sample sizes and lack of normality, non-parametric methods were used. Across categories, PM2.5 data were analysed using the Kruskal–Wallis test. Seven planned comparisons were used to examine differences of mean PM2.5 concentration between the waterpipe café smoking and non-smoking rooms and the cigarette smoking-permitted restaurant smoking and non-smoking rooms (Mann–Whitney U test between venues, Wilcoxon signed-rank test within venues, exact significance levels reported; see Nachar31). In addition, Spearman correlation analyses were used to explore the relationship between smoker density and PM2.5 as well as the PM2.5 concentrations between smoking and non-smoking rooms. A p value of <0.05 was considered statistically significant for all analyses.
RESULTS
Venue sample characteristics
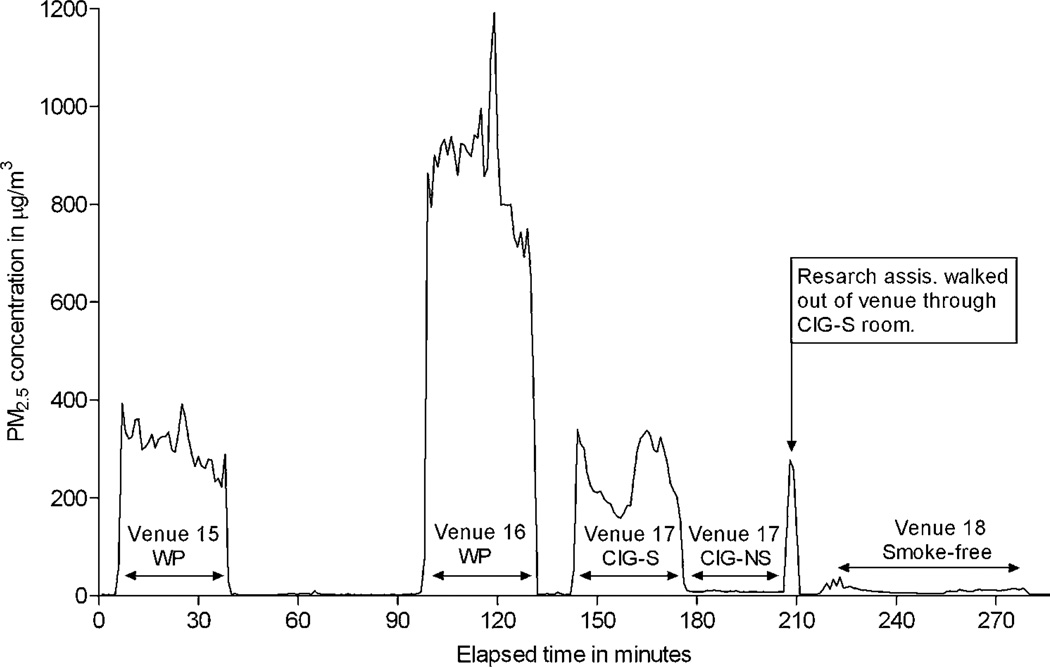
By region, six venues were visited in the Northern (four waterpipe cafés, one cigarette smoking-permitted restaurant and one smoke-free restaurant), four in the Southwest (two waterpipe cafés, one cigarette smoking-permitted restaurant and one smoke-free restaurant), six in the West Central (three waterpipe cafés, one cigarette smoking-permitted restaurant and two smoke-free restaurants (one with valid data)), six in the East Central (four waterpipe cafés, one cigarette smoking-permitted restaurant and one smoke-free restaurant) and six in the Eastern Region (four waterpipe cafés, one cigarette smoking-permitted restaurant and one smoke-free restaurant). Table 1 displays the characteristics of all 28 venues assessed including room volume (m3), smoker density and mean PM2.5. A wide range of room/venue sizes were sampled: waterpipe cafés =23–987 m3, cigarette smoking-permitted restaurants =144–826 m3 and smokefree restaurants =247–1163 m3. Cigarette smoking was observed in four of the five cigarette smoking-permitted restaurants, and waterpipe smoking was observed in all 17 waterpipe cafés. In addition to waterpipe smoking, cigarette smoking was present in three waterpipe cafés, but at a relatively low rate (mean number of burning cigarettes =0.42; mean number of lit waterpipes =12.72). Other tobacco smoking (cigars, bidis/cloves) was not observed in any venue sampled. In all five smoke-free restaurants, no smoking of any kind was observed. Of the 17 waterpipe cafés visited, the non-smoking room was clearly designated in 11 venues but was otherwise obscure (n=4) or not required (n=2; exempt from VICAA due to service of only pre-packaged food and bottled/canned drinks) in the remaining venues. All cigarette smoking-permitted restaurants had a clearly marked non-smoking room. In one waterpipe café, smoking was observed in the non-smoking room and data were retained from this venue to reflect compliance with the current policy accurately. Figure 1 displays real-time PM2.5 concentrations measured in select venues of each type (ie, venues 15 through 18).
Table 1.
Descriptive statistics and PM2.5 concentration for each venue by smoking status of room measured
| Smoking | Non-smoking | ||||||
|---|---|---|---|---|---|---|---|
| Venue ID | Venue type | Volume (m3) | Active smoker density* |
Mean PM2.5 (µg/m3) | Volume (m3) | Active smoker density* |
Mean PM2.5 (µg/m3) |
| 5 | Waterpipe café† | 412 | 6.15 | 1733 | 179 | 0.00 | 823 |
| 19 | Waterpipe café | 208 | 6.09 | 889 | 150 | 0.00 | 154 |
| 16 | Waterpipe café | 256 | 6.11 | 877 | NA | NA | NA |
| 10 | Waterpipe café | 49 | 7.15 | 518 | 99 | 0.00 | 34 |
| 28 | Waterpipe café† | 209 | 2.28 | 461 | NA | NA | NA |
| 13 | Waterpipe café | 304 | 3.87 | 381 | NA | NA | NA |
| 15 | Waterpipe café | 218 | 2.75 | 309 | NA | NA | NA |
| 7 | Waterpipe café | 182 | 0.73 | 263 | 169 | 0.00 | 44 |
| 8 | Waterpipe café | 275 | 5.22 | 223 | NA | NA | NA |
| 4 | Waterpipe café | 135 | 4.92 | 140 | 111 | 0.00 | 31 |
| 20 | Waterpipe café | 99 | 13.52 | 124 | 251 | 0.00 | 16 |
| 1 | Waterpipe café | 23 | 16.07 | 112 | 325 | 0.00 | 50 |
| 21 | Waterpipe café | 531 | 1.26 | 107 | 480 | 0.00 | 55 |
| 25 | Waterpipe café† | 316 | 2.95 | 95 | 57 | 2.33 | 98 |
| 6 | Waterpipe café | 987 | 1.66 | 67 | 819 | 0.00 | 20 |
| 11 | Waterpipe café | 464 | 1.08 | 53 | NA | NA | NA |
| 24 | Waterpipe café | 223 | 1.15 | 13 | 130 | 0.00 | 30 |
| 17 | Cigarette restaurant | 308 | 1.95 | 247 | 826 | 0.00 | 9 |
| 9 | Cigarette restaurant | 661 | 0.91 | 183 | 281 | 0.00 | 79 |
| 14 | Cigarette restaurant | 253 | 1.19 | 89 | 321 | 0.00 | 6 |
| 22 | Cigarette restaurant | 308 | 0.16 | 64 | 373 | 0.00 | 6 |
| 26 | Cigarette restaurant | 144 | 0.00 | 11 | 224 | 0.00 | 31 |
| 2 | Smoke-free restaurant | NA | NA | NA | NA | NA | NA |
| 3 | Smoke-free restaurant | NA | NA | NA | 247 | 0.00 | 11 |
| 18 | Smoke-free restaurant | NA | NA | NA | 392 | 0.00 | 11 |
| 12 | Smoke-free restaurant | NA | NA | NA | 1127 | 0.00 | 8 |
| 23 | Smoke-free restaurant | NA | NA | NA | 1163 | 0.00 | 8 |
| 27 | Smoke-free restaurant | NA | NA | NA | 401 | 0.00 | 7 |
Burning cigarettes-waterpipes per 100 m3.
Waterpipe cafés where cigarette smoking was observed.
Figure 1.
Real-time PM2.5 concentrations for two waterpipe cafés (WP), one cigarette smoking-permitted restaurant smoking (CIG-S) and nonsmoking room (CIG-NS), and one smoke-free restaurant on 15 April 2011.
Mean PM2.5 across venue type and room
Table 2 displays mean characteristics by venue and room measured that were used for analysis. Mean (±SD) PM2.5 concentrations across all waterpipe café smoking rooms (includes cafés that allowed smoking throughout; n=17) ranged from 13 to 1733 µg/m3, and the overall mean for these venues was 374 µg/m3 (±440). Mean PM2.5 concentrations across all waterpipe café non-smoking rooms (n=11) ranged from 16 to 823 µg/m3, and the overall mean was 123 µg/m3 (±236). For the cigarette smoking-permitted restaurants (n=5), the mean overall PM2.5 concentration for the smoking rooms was 119 µg/m3 (±95) with a range of 11–247 µg/m3, and the mean for the nonsmoking rooms was 26 µg/m3 (±31) with a range of 6–79 µg/m3. The mean PM2.5 concentration for the smoke-free restaurants (n=5) was 9 µg/m3 (±2) with a range of 7–11 µg/m3. Across all rooms/venues, which allowed smoking (cigarette and waterpipe) and smoke-free restaurants, there was a positive correlation between smoker density and PM2.5 (r=0.79, n=27, p=0.000). When PM2.5 concentration between room pairs (ie, only venues with a smoking room and non-smoking room) was compared across venues, there was a positive correlation (r=0.53, n=16, p=0.036).
Table 2.
Summary statistics (mean±SD) for each venue/room category
| N | Venue type | Room measured | Mean volume (m3) | Mean active smoker density* | Mean PM2.5 (µg/m3) | Median PM2.5 |
|---|---|---|---|---|---|---|
| 6 | Waterpipe café† | Smoking | 288±93 | 3.55±1.89 | 384±279 | 345 |
| 11 | Waterpipe café | Smoking | 288±278 | 4.32±3.87 | 369±520 | 124 |
| 11 | Waterpipe café | Non-smoking | 252±223 | 0.21±0.70 | 123±236 | 44 |
| 5 | Cigarette | Smoking | 335±194 | 0.84±0.79 | 119±95 | 89 |
| 5 | Cigarette | Non-smoking | 405±241 | 0.00±0.00 | 26±31 | 9 |
| 5 | Smoke-free | Non-smoking | 666±442 | 0.00±0.00 | 9±2 | 8 |
Burning cigarettes—waterpipes per 100 m3.
Venue locations did not have a visible non-smoking room (ie, smoking throughout).
The distribution of PM2.5 concentration across all six types of venues/rooms (n=43) differed significantly (H5=24.0, p=0.000). The PM2.5 concentrations of the waterpipe cafés with a nonsmoking (mean =123) and smoking (mean =369) room differed significantly (z=−2.7, n=11, p=0.008). For all other comparisons, waterpipe café smoking rooms from these locations (n=11) and those from waterpipe cafés that allowed smoking throughout (n=6) were collapsed into a single group (waterpipe café smoking rooms); there was not a significant difference in PM2.5 concentration between these two room types (U=25.0, p=0.462). PM2.5 concentrations for the cigarette smoking-permitted restaurant smoking rooms did not differ significantly from the cigarette smoking-permitted restaurant non-smoking rooms (z=−1.8, n=5, p=0.08). Importantly, no significant difference was observed between cigarette smoking-permitted restaurant smoking rooms and waterpipe café non-smoking rooms.
DISCUSSION
To the best of our knowledge, this is the first report of PM2.5 concentrations in waterpipe cafés in the USA. Results indicate that the air quality in waterpipe cafés, as indexed by PM2.5 concentrations, is poorer than the cigarette smoking-permitted restaurants that were assessed during this study. The PM2.5 concentrations in smoking rooms of waterpipe cafés (374 µg/m3) were 3.2 times greater on average than for the smoking rooms of cigarette smoking-permitted restaurants (119 µg/m3) and 41.6 times higher than those observed in smoke-free venues (9 µg/m3). Similarly, the mean PM2.5 value for the non-smoking room of waterpipe cafés (123 µg/m3) was 4.7 times higher on average than observed within the non-smoking room of cigarette smoking-permitted restaurants (26 µg/m3). Alarmingly, relative to smoke-free venues, the mean PM2.5 concentration in nonsmoking rooms of cigarette smoking-permitted restaurants was 2.8 times higher and in non-smoking rooms of waterpipe cafés was 13.7 times higher. Thus, employees and/or non-smoking patrons that occupy either a restaurant that allows cigarette smoking or waterpipe café will be exposed to PM2.5 concentrations above that found in a smoke-free environment.
In reference to the effectiveness of the VICAA, on average, the structurally separate non-smoking rooms provided a reduction in PM2.5 (as compared with the smoking rooms for waterpipe and cigarette smoking-permitted venues), but the mean concentration for the non-smoking rooms of waterpipe cafés was well above those observed in smoke-free venues (9 µg/m3) as well as daily (35 µg/m3) and annual (15 µg/m3) PM2.5 US EPA exposure limits5 and daily (25 µg/m3) and annual (10 µg/m3) WHO guidelines.32 In addition, there was one waterpipe café that allowed smoking in the non-smoking room, and four locations that did not appear to be in compliance with VICAA (no visible structurally separate non-smoking room).
Importantly, smoker density was correlated positively with measured PM2.5, suggesting that cigarette and/or waterpipe smoking was the major source of the measured PM2.5 in venues that were assessed during this study. The positive correlation between PM2.5 concentrations in the non-smoking and smoking rooms of cigarette smoking-permitted and waterpipe smoking venues indicates that the high levels of PM2.5 in one room were associated with high levels in the other. Worth noting is that, in only three of the five cigarette smoking-permitted restaurants and only three of the 11 waterpipe cafés, was the door between smoking and non-smoking areas consistently closed (ie, excluding brief entry or departure of patrons and employees). Patrons and employees may also be exposed and/or expose others to potential thirdhand smoke (THS; smoke pollutants trapped in clothing/fabrics, on surfaces or transferred by their hands).33 While the clinical implications of THS exposure are uncertain, potential THS-associated exposures include nicotine, PM and products of surface reactions involving tobacco smoke constituents.33
These results are comparable to those observed in venues where waterpipe smoking is prevalent. For example, in Syria across 40 restaurants/cafés where both cigarette and waterpipe smoking was observed, the mean PM2.5 concentration was 464 µg/m3.20 In Lebanon among a sample of 28 hospitality venues that allowed cigarette and waterpipe smoking, the mean PM2.5 concentration was 349 µg/m3.34 Also, the mean PM2.5 concentration for restaurants that permitted cigarette smoking was consistent with that observed in similar venues in western New York (156 µg/m3)8 and Paducah, Kentucky (177 µg /m3).35
While smoking density was a strong correlate of PM2.5 levels in venues sampled, other factors (open fires, cooking equipment) may have also contributed to these concentrations. Other types of ambient particulates within a building as well as outdoor PM can affect indoor readings.36 Specifically for waterpipe cafes, the charcoal used to heat the waterpipe tobacco may be an important source of PM.37 Other constituents besides tobacco (eg, honey, molasses, flavourings) present in the products used in the waterpipe may also contribute substantially to air quality. Future studies can examine the extent to which the results reported here are influenced by tobacco-containing and tobacco-free waterpipe products. Another characteristic deserving of future study is how multiple users who smoke the same waterpipe impact the smoke produced. While this study only assessed the number of waterpipes in use, a more precise determination of the number of waterpipe smokers using each waterpipe would aid the understanding of smoking density. Lastly, the lack of air quality data in these venues prior to VICAA implementation makes inferences concerning effectiveness more difficult.
Conclusions
The heightened levels of respirable suspended particles observed in waterpipe cafés and cigarette smoking-permitted venues represent a considerable potential health risk for employees and patrons. For instance, PM2.5 concentrations in the smoking room of one waterpipe café reached levels almost seven times higher than the US EPA-defined ‘hazardous’ level (>250 µg/m3 daily exposure) and the non-smoking room of the same café was three times higher than these ‘hazardous’ levels. These data suggest that regulations that allow for indoor smoking even if it is in a separate room are not effective at safeguarding non-smokers, especially for individuals who work or visit venues that allow waterpipe smoking. Stricter enforcement or implementation of a more comprehensive smoking ban in Virginia would be more effective for protecting public health.38
What this paper adds.
-
►
Few studies have assessed indoor air quality associated with waterpipe smoking and no study has examined how these venues are influenced by or adapt to indoor smoking regulations.
-
►
Venues that allowed waterpipe smoking had the highest mean concentrations of PM2.5 and the non-smoking areas of these venues did not differ significantly from the restaurants that permitted cigarette smoking.
-
►
These data corroborate others that indicate waterpipe smoking is an important source of PM2.5 and justify the inclusion of waterpipe smoking in legislation that restricts SHS.
Acknowledgments
Funding This work was supported by USA Public Health Service grants R01CA120142, R01DA025659, R01DA024876, T32DA007027-34 and F31DA028102 and Flight Attendant Medical Research Institute grant YCSA052333.
Footnotes
Contributors COC, ARV and MDB made significant contributions to the study design, data collection, analysis and writing of the manuscript. KJ assisted with data collection and the writing of the manuscript. MJT and TE provided study design and analysis guidance as well as critical revision of the manuscript. All authors gave final approval for the version to be published.
Competing interests None.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement The manuscript includes all data collected for this study except for minor venue characteristics observed. Data are available by email request to the corresponding author TE.
REFERENCES
- 1.US Department of Health and Human Services. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. [Google Scholar]
- 2.National Cancer Institute. Health Effects of Exposure to Environmental Tobacco Smoke. Smoking and Tobacco Control Monograph No. 10. [accessed 13 Nov 2011];1999 NIH Pub. No. 99-4645. http://cancercontrol.cancer.gov/tcrb/monographs/10/index.html.
- 3.American Nonsmokers’ Rights Foundation. Overview List - How Many Smoke Free Laws? [accessed 19 Jan 2012]; http://www.no-smoke.org/pdf/mediaordlist.pdf.
- 4.Noonan D. Exemptions for hookah bars in clean indoor air legislation: a public health concern. Public Health Nurs. 2010;27:49–53. doi: 10.1111/j.1525-1446.2009.00826.x. [DOI] [PubMed] [Google Scholar]
- 5.Environmental Protection Agency. National ambient air quality standards for particulate matter; final rule. [accessed 14 Nov 2011];Federal Register. 2006 71:61144–61233. http://www.gpo.gov/fdsys/pkg/FR-2006-10-17/html/06-8477.htm. [Google Scholar]
- 6.Avila-Tang E, Travers MJ, Navas-Acien A. Promoting smoke-free environments in Latin America: a comparison of methods to assess secondhand smoke exposure. Salud Publica Mex. 2010;52:138–148. doi: 10.1590/s0036-36342010000800009. [DOI] [PubMed] [Google Scholar]
- 7.Lee K, Hahn EJ, Robertson HE, et al. Strength of smoke-free air laws and indoor air quality. Nicotine Tob Res. 2009;11:381–386. doi: 10.1093/ntr/ntp026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Travers MJ, Cummings KM, Hyland A, et al. Indoor air quality in hospitality venues before and after the implementation of a clean indoor air law-Western New York, 2003. MMWR Morb Mortal Wkly Rep. 2004;53:1038–1041. [PubMed] [Google Scholar]
- 9.Lee K, Hahn EJ, Pieper N, et al. Differential impacts of smoke-free laws on indoor air quality. J Environ Health. 2008;70:24–30. 54. [PubMed] [Google Scholar]
- 10.Shihadeh A. Investigation of mainstream smoke aerosol of the argileh water pipe. Food Chem Toxicol. 2003;4:143–152. doi: 10.1016/s0278-6915(02)00220-x. [DOI] [PubMed] [Google Scholar]
- 11.Sepetdjian E, Saliba N, Shihadeh A. Carcinogenic PAH in waterpipe charcoal products. Food Chem Toxicol. 2010;48:3242–3245. doi: 10.1016/j.fct.2010.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sutfin EL, McCoy TP, Reboussin BA, et al. Prevalence and correlates of waterpipe tobacco smoking by college students in North Carolina. Drug Alcohol Depend. 2011;115:131–136. doi: 10.1016/j.drugalcdep.2011.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnston LD, O’Malley PM, Bachman JG, et al. Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings, 2010. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2011. [Google Scholar]
- 14.Akl EA, Gaddam S, Gunukula SK, et al. The effects of waterpipe tobacco smoking on health outcomes: a systematic review. Int J Epidemiol. 2010;39:834–857. doi: 10.1093/ije/dyq002. [DOI] [PubMed] [Google Scholar]
- 15.Raad D, Gaddam S, Schunemann HJ, et al. Effects of waterpipe tobacco smoking on lung function: a systematic review and meta-analysis. Chest. 2011;139:764–774. doi: 10.1378/chest.10-0991. [DOI] [PubMed] [Google Scholar]
- 16.Daher N, Saleh R, Jaroudi E, et al. Comparison of carcinogen, carbon monoxide, and ultrafine particle emissions from narghile waterpipe and cigarette smoking: sidestream smoke measurements and assessment of second-hand smoke emission factors. Atmos Environ. 2010;44:8–14. doi: 10.1016/j.atmosenv.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al Rashidi M, Shihadeh A, Saliba NA. Volatile aldehydes in the mainstream smoke of the narghile waterpipe. Food Chem Toxicol. 2008;46:3546–3549. doi: 10.1016/j.fct.2008.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shihadeh A, Saleh R. Polycyclic aromatic hydrocarbons, carbon monoxide, “tar”, and nicotine in the mainstream smoke aerosol of the narghile water pipe. Food Chem Toxicol. 2005;43:655–661. doi: 10.1016/j.fct.2004.12.013. [DOI] [PubMed] [Google Scholar]
- 19.Fromme H, Dietrich S, Heitmann D, et al. Indoor air contamination during a waterpipe (narghile) smoking session. Food Chem Toxicol. 2009;47:1636–1641. doi: 10.1016/j.fct.2009.04.017. [DOI] [PubMed] [Google Scholar]
- 20.Maziak W, Ali RA, Fouad MF, et al. Exposure to secondhand smoke at home and in public places in syria: a developing country’s perspective. Inhal Toxicol. 2008;20:17–24. doi: 10.1080/08958370701758783. [DOI] [PubMed] [Google Scholar]
- 21.American Lung Association. An Emerging Deadly Trend: Waterpipe Tobacco Use. Tobacco Policy Trend Alert; 2007. [accessed 24 Jan 2012]. http://www.lungusa2.org/embargo/slati/Trendalert_Waterpipes.pdf. [Google Scholar]
- 22.Virginia Department of Health. [accessed 14 Nov 2011];Restaurants and Smoking in Virginia FAQS. http://www.vdh.state.va.us/breatheeasy/faqs.htm. [Google Scholar]
- 23.Vaughan J. Smoking Ban Might Extinguish Hookah Bars. Richmond BizSense; 2009. [accessed 13 Nov 2011]. http://www.richmondbizsense.com/2009/03/03/smoking-ban-might-extinguish-hookah-bars/ [Google Scholar]
- 24.Klepeis NE, Ott WR, Switzer P. Real-time measurement of outdoor tobacco smoke particles. J Air Waste Manag Assoc. 2007;57:522–534. doi: 10.3155/1047-3289.57.5.522. [DOI] [PubMed] [Google Scholar]
- 25.Hyland A, Travers MJ, Dresler C, et al. A 32-country comparison of tobacco smoke derived particle levels in indoor public places. Tob Control. 2008;17:159–165. doi: 10.1136/tc.2007.020479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Waring MS, Siegel JA. An evaluation of the indoor air quality in bars before and after a smoking ban in Austin, Texas. J Expo Sci Environ Epidemiol. 2007;17:260–268. doi: 10.1038/sj.jes.7500513. [DOI] [PubMed] [Google Scholar]
- 27.Repace JL. Respirable particles and carcinogens in the air of delaware hospitality venues before and after a smoking ban. J Occup Environ Med. 2004;46:887–905. doi: 10.1097/01.jom.0000141644.69355.52. [DOI] [PubMed] [Google Scholar]
- 28.Smith-Simone S, Maziak W, Ward K, et al. Waterpipe tobacco smoking: knowledge, attitudes, beliefs, and behavior in two U.S. samples. Nicotine Tob Res. 2008;10:393–398. doi: 10.1080/14622200701825023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Travers MJ, Maher J, Vogl L. Measuring exposure to waterpipe tobacco smoke: a waterpipe-specific calibration factor for the sidepak aerosol monitor. Paper presented at the 15th World Conference on Tobacco or Health; 20–24 March 2012; Singapore. [Google Scholar]
- 30.Travers MJ, et al. Smoke-Free Air Policy: Changing What’s in the Air and in the Body, in Social and Preventive Medicine. [Dissertation] Buffalo, NY: State University of New York at Buffalo; 2008. [Google Scholar]
- 31.Nachar N. The Mann-Whitney U: A test for assessing whether two independent samples come from the same distribution. Tutorials Quant Meth Psych. 2008;4:13–20. [Google Scholar]
- 32.World Health Organization. Geneva, Switzerland: WHO; 2006. [accessed 13 Nov 2011]. WHO Air Quality Guidelines for Particulate Matter, Ozone, Nitrogen Dioxide and Sulfur Dioxide. http://whqlibdoc.who.int/hq/2006/WHO_SDE_PHE_OEH_06.02_eng.pdf. [Google Scholar]
- 33.Matt GE, Quintana PJ, Destaillats H, et al. Thirdhand tobacco smoke: emerging evidence and arguments for a multidisciplinary research agenda. Environ Health Perspect. 2011;119:1218–1226. doi: 10.1289/ehp.1103500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Saade G, Seidenberg AB, Rees VW, et al. Indoor secondhand tobacco smoke emission levels in six Lebanese cities. Tob Control. 2010;19:138–142. doi: 10.1136/tc.2009.030460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones SC, Travers MJ, Hahn EJ, et al. Secondhand smoke and indoor public spaces in Paducah, Kentucky. J Ky Med Assoc. 2006;104:281–288. [PubMed] [Google Scholar]
- 36.Brennan E, Cameron M, Warne C, et al. Secondhand smoke drift: examining the influence of indoor smoking bans on indoor and outdoor air quality at pubs and bars. Nicotine Tob Res. 2010;12:271–277. doi: 10.1093/ntr/ntp204. [DOI] [PubMed] [Google Scholar]
- 37.Monn C, Kindler P, Meile A, et al. Ultrafine particle emissions from waterpipes. Tob Control. 2007;16:390–393. doi: 10.1136/tc.2007.021097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hahn EJ. Smokefree legislation: a review of health and economic outcomes research. Am J Prev Med. 2010;39:66–76. doi: 10.1016/j.amepre.2010.08.013. [DOI] [PubMed] [Google Scholar]