Abstract
Neurocysticercosis (NCC) is a neglected tropical disease caused by larval forms of the parasite Taenia solium lodging in central nervous system (CNS). There is a huge morbidity and debilitation due to CNS manifestations of NCC in developing and underdeveloped regions of the globe, mainly Asian, African and Latin American countries. It is the cause of epilepsy in about 1% of the population of endemic countries and is the underlying etiology in about 15-50% persons with epilepsy, depending upon the geographical region. There is no perfect diagnostic method and the diagnosis relies on a combination of clinical, radio-imaging, immunologic and epidemiologic data. Treatment includes anti-parasitic treatment by cysticidal drugs and management of associated symptoms and complications. The disease is eradicable and control depends on an integrated and coordinated involvement of international bodies like the World Health Organization along with scientific institutions and political and administrative strata of the endemic countries to provide the essential tools such as adequate sanitation, live-stock management, health education and improved socio-economic conditions.
KEY WORDS: Neglected tropical disease, neurocysticercosis, Taenia solium
INTRODUCTION
Cysticercosis, caused by metacestodes of Taenia solium, a two-host zoonotic cestode of the order cyclophyllidea, is a disease of antiquity. The ancient vedic texts describe infestations of head and eyes by parasites and Greek physicians Hippocrates and Theophratus were aware of human infection with a tape worm.[1,2] The name “cysticercosis” was given by Laennec derived from the Greek word “Kystic” meaning bladder and “Kercos” signifying tail. In 1809, Rudolphi gave the second name of “cellulose” due to its great affinity for connective tissue and in 1853, Beneden was the first to suspect its relationship to Taenia worm.[2] Humans acquire cysticercosis through feco-oral contamination with T. solium eggs from tapeworm carriers.[3] Though, cysticerci (larval cysts) can develop in any organ in the body, cystercerci in the brain or spinal cord, neurocysticercosis (NCC) is the most serious form of infection.
Cysticercosis is of much economic and public health importance causing morbidity and mortality in many developing countries of Asia, Africa and Latin America.[4] Until recently, NCC and echinococcosis were referred to as “neglected” diseases, but are now recognized by the World Health Organization (WHO) as “major neglected diseases”.[5,6] It is one of the most common parasitic diseases of the central nervous system (CNS) and is considered a “biological marker” of the social and economic development of a community. In many endemic communities, NCC is the cause of epilepsy in about 1% of the population.[5] It the past few decades, it has gained even more importance as it has spread to areas previously unknown to be endemic like the United States of America (USA) and Australia. This epidemiological diversity can be attributed to intensification of animal products, increase in world meat and live animal trade, large scale intra-and inter-country migration of agricultural and other workers such as domestic employers and international tourism.[7,8]
EPIDEMIOLOGY
The disease is world-wide in distribution, though major endemic regions are the world's poorer countries where families raise free-roaming pigs that are able to ingest human feces.[5,9] These regions include Latin America, most parts of Asia (including China and the Indian subcontinent), Eastern Europe and most of Africa. The world-wide prevalence of NCC still remains to be known, though, initiatives are underway to determine the burden in endemic countries as well as in developed nations like USA.[9,10,11,12] The data on the burden of NCC associated with epilepsy is relatively well-documented, hence is used to provide estimates of prevalence and incidence of NCC in endemic regions.[9,10] The estimated numbers of people suffering from epilepsy due to NCC are as high as 0.31-4.6 million in sub-Saharan Africa, 0.45-1.35 million in Latin America, 1 million in India and 0.3-0.7 million in China.[5] In a community-wide screening survey from rural Peru, the seroprevalence was 24% and was associated with seizures with an odd's ratio of 2.1,[13] with an additional 13% of those with negative serology demonstrating calcifications typical of NCC in computed tomography (CT) scans, thereby giving an overall estimate of 37% prevalence of cysticercosis.[5,13] Estimates of prevalence from other Latin American countries range from 15% to 38%.[5] In a systematic review conducted to estimate the frequency of NCC world-wide, the proportion of NCC among persons with epilepsy was consistently found to be about 29% (95% CI: 23.5-36.1%) from Latin America, sub-Saharan Africa and Southeast Asia.[10] The average incidence of T. solium infection in China has been estimated to be 0.11%, with 1.26 million suffering from teniasis and 3-6 million from cysticercosis.[6]
In the Indian subcontinent, the disease is documented to be endemic in India, Bhutan, parts of Indonesia (Bali and Papua), Nepal and Timor-Leste. In India, it is prevalent in all states, with WHO estimating NCC to be the cause of epilepsy in up to 50% of Indian patients who present with partial seizures; ocular cysticercosis also being common.[6] In a community survey in Vellore in southern India, among those suffering from active epilepsy, NCC was found in 28% by CT scan and 13% by the enzyme-linked immunoelectrotransfer blot (EITB). Overall, 34% of patients were diagnosed with NCC. Moreover, there was no significant difference in prevalence of NCC in urban and rural areas.[14] In Puducherry in south India, seroprevalence was observed to be 16% in patients with epileptic seizures[15] and 6% in blood donors when tested for both antibodies and antigens.[16] In Chandigarh in northern India, overall seroprevalence in the general population was found to be 17%, with 24% in slum areas, 20% in rural and 8% in organized urban sectors, with only 8% of the seropositive individuals having history suggestive of NCC.[17] Another study carried out in a rural pig farming community across 30 villages in north India showed a very high prevalence with 48% of those suffering from active epilepsy fulfilling the definitive or probable diagnostic criteria for NCC; epilepsy in the family and no separate place to keep pigs being the major risk factors.[18]
DISEASE
Human beings acquire cysticercosis through feco-oral contamination with T. solium eggs from tapeworm carriers.[3] Thus, vegetarians and other people who do not eat pork can acquire cysticercosis; exogenous autoinfection due to ano-oral contamination and endogenous autoinfection due to reverse peristalsis can also give rise to cysticercosis. After ingestion of eggs, the oncospheres are liberated in the duodenum, can penetrate the intestinal mucosa and enter the local lymphatics and mesenteric vessels and may migrate to locate anywhere in the body as larval cysts.[19] Within 2-3 months, the oncospheres lose the hooks and develop into fluid filled bladder worms or cysticerci. The most frequent site of cysticerci is subcutaneous and intramuscular tissues, followed by the brain and eye. These can also occur in heart, liver, lung, abdominal cavity and rarely spinal cord. Symptomatic disease results almost exclusively from invasion of the nervous system, i.e., NCC and the eye; there are case reports, though, of extraneural forms presenting as cystic masses involving skeletal muscles, subcutaneous tissues, buccal mucosa, tongue and lips[20,21] and rare cases of disseminated cysticercosis.[22]
NCC is polymorphic in clinical presentation and ranges from asymptomatic individuals to cases with severe neurological problems. The infected persons grossly vary in terms of the number of active episodes and recurrences, incidence of serious complications, as well as incidence of co-infections with Japanese Encephalitis and HIV.[23] Carabin et al. systematically reviewed estimates of frequencies of different manifestations, complications and disabilities associated with NCC and documented about 79% having seizures/epilepsy, 38% severe headaches, 16% focal deficits and 12% signs of increased intracranial pressure; all other manifestations such as cranial nerve palsy, gait abnormality/ataxia, focal deficits, visual changes, altered mental state/psychiatric symptoms and pyramidal signs occurring in lesser than 10% of symptomatic NCC patients.[24] The clinical presentation is clearly different in parenchymal and extraparenchymal NCC. The most common presentation of parenchymal NCC is with seizures, while extraparenchymal NCC may cause hydrocephalus by mechanical obstruction of the ventricles or the basal cisterns.[19,25,26]
NCC is common in adults as well as in children. Although it usually manifests after 5 years of age, symptomatic NCC is seen even in infants and preschool children. The prevalence of epilepsy in Mexico was seen to increase with age.[27] There are also age-related differences in the manifestation of NCC. Most of the cases of childhood NCC present with mild to moderate symptoms and single lesions and extraparenchymal NCC seen in adults are rarely seen in children.[28] There is also clinical heterogeneity across countries; most cases from the Indian subcontinent present with single degenerating lesions, whereas those from Latin America and China present with few viable lesions.[29] Extraparenchymal NCC is frequently seen in Latin American countries, whereas it is uncommon in the Indian subcontinent. These variations are perhaps due to complex interactions between the host, parasite and environmental factors.[30] Genetic differences in T. solium cysticerci have been reported from different countries and may contribute towards the clinical variations across countries.[31] A significantly increased frequency of HLA-A28 (39% vs. 15%) and decreased frequency of HLA-DQW2 (4% vs. 31%) has been reported from a Mexican cohort with parenchymal NCC when compared to healthy controls, with a relative risk of 3.5 for developing the disease in HLA-A28 positive individuals.[32] From India, in patients with single, small, contrast enhancing CT lesions, a positive association of HLA-DRB1* 13, HLA-B63 and HLA-B58 and a decrease in persons with HLA-A11 has been shown.[33,34] The environmental factors determining solitary cysts are young age and a patient being from the Indian subcontinent or travelers from non-endemic countries. Such patients are usually young teenagers or young adults (majority under 20 years of age) presenting with newly developed seizures.[35,36] Though not clearly known, the factors responsible could be that in India only a few individuals raise pigs and a vast subgroup is vegetarian or not eating pork.[35] The cooking habits in India where heating the food to high temperatures is commonly practiced, in contrast to South American countries and China where undercooked food is commonly used in recipes, may also be aiding milder egg challenges and thus low parasite loads and milder infections.
DIAGNOSIS
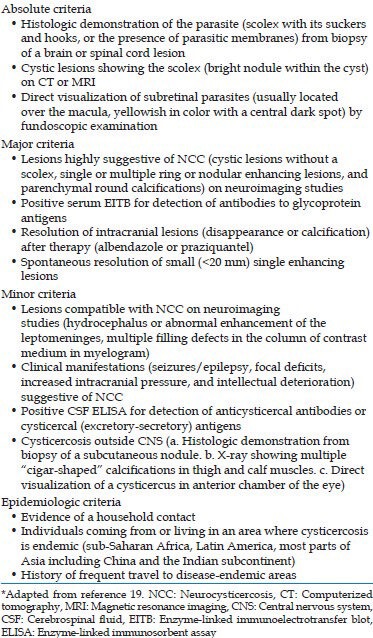
The lack of specificity of the neurological symptoms makes it impossible to diagnose the disease on clinical grounds alone. Thus clinical presumptive diagnosis is usually substantiated with radio-imaging techniques and serodiagnosis. An ideal test for diagnosis of NCC should be a non-expensive, simple-to-perform, point-of-care method with good sensitivity and specificity not only for multiple lesions but also for solitary cyst lesions. Such method is not yet available; hence the diagnosis depends on objective clinical, radio-imaging, immunologic and epidemiologic data, the only absolute diagnostic criteria being histologic demonstration of the parasite from biopsy of the brain or spinal cord, cystic lesions showing scolex on CT or magnetic resonance imaging (MRI), or direct visualization of subretinal parasites by funduscopy [Table 1].[19]
Table 1.
Diagnostic criteria for NCC*
Neuroimaging
In most cases, NCC diagnosis is based on neuroimaging studies (CT and MRI). CT and MRI also provide information about the parasite stage and location.[37,38] Three main stages have been described: Vesicular (viable), colloidal (degenerative) and calcified (inactive).[39] CT is the best radiological method for detection of intraparenchymal calcification, while MRI is more sensitive for the identification of cysts in the ventricles.[7] Radioimaging methods may serve the useful purpose, but due to the unavailability of the facilities at many cities and high cost, its use is limited in the developing countries. Moreover, imaging findings may mimic with other types of neurological diseases, thus posing problems in the diagnosis.[40,41] In some cases, particularly when parasites are located in the subarachnoid basal cisterns, neither CT nor MRI can detect the parasite. In these cases, NCC diagnosis is supported by clinical, epidemiological and serological data as well as by the response to cysticidal treatment.[42]
Immunodiagnosis
Immunodiagnosis of NCC by detecting an antigen and/or antibodies is an accessible, low-cost diagnostic tool in areas of endemicity.
Antibody detection
A variety of immunodiagnostic techniques and antigens (total metacestode soluble antigens, metacestode membrane or scolex soluble extracts, semi-purified proteins) have been assessed for the diagnosis of NCC with variable sensitivity and specificity.[43,44,45,46,47,48] It has been observed that immunodiagnostic tests based on crude antigen preparations have, at best, moderate sensitivity and specificity.[49] Using semi-purified/purified antigens could constitute a better alternative, but purification procedures are often complex and require considerable technical expertise.
Currently, the most reliable immunological test is an EITB assay with serum samples using lentil lectin glycoprotein antigens of T. solium cysts and is reported to have a 100% specificity for detection of antibodies in serum and cerebrospinal fluid (CSF).[7,50] Although, 90% sensitivity has been reported in patients with more than two lesions, it declines to 50-62% with a single lesion and for calcified lesions.[51] It is also estimated that most cured patients remain seropositive when followed-up for 1 year after anti-parasitic therapy, mainly due to persistence of antibodies after resolution of active infection.[52] Extraneural cysticercosis and cross-reactions with other cestodes and helminths can also contribute to false-positive results obtained by using serum antibodies.[52,53] Atluri et al. have shown a high sensitivity (100%) in all the thirteen NCC seropositive children (11 had solitary NCC lesion and 2 had multiple NCC lesions) and 60% sensitivity among suspected cases of NCC children who were seronegative for NCC (36% had solitary NCC lesion and 24% had multiple NCC lesions), with specificity of 92% by two-dimensional polyacrylamide gel electrophoresis EITB.[54] This could be a useful diagnostic modality in endemic countries for the serodiagnosis of NCC, however it requires expertise and facilities. EITB has been extensively used for diagnosis of human and porcine cysticercosis and is commercially available.[55] The drawback, however, is that it depends on infected pigs for supplying the source material. Preparation of the antigen and performance of western blot require considerable technical expertise. Furthermore, batch differences can exist between different antigen preparations and the antigen mixture is not suitable for use in an enzyme-linked immunosorbent assay (ELISA) format due to the presence of non-specific fractions. Further, a western blot assay is not suitable for field studies, nor is it a suitable or affordable assay for diagnosis in countries where cysticercosis is endemic.[56]
The development of numerous serodiagnostic tests using different parasitic antigens is indicative of the fact that none of them is 100% sensitive and specific, particularly in single-lesion parenchymal NCC. Michelet et al. compared the diagnostic efficacy of EITB and HP10 antigen detection by ELISA and found the sensitivities of antibody detection by both tests not to be significantly different, with ELISA identifying HP10 even when vesicular cysticerci were located in the subarachnoideal basal cisterns.[57] Other tests like dot-blots have also been used for the serodiagnosis of several parasitic infections and can give sensitivities as high as those observed with ELISA, at the same time being rapid, easy to carry out and read. Mandal et al. have shown that ELISA and dot-blot assays developed “in-house” can give good sensitivity in the detection of anti-cysticercal IgG, especially among the pediatric cases of NCC who have multiple brain lesions (100%) when compared to those with single-lesion (87%).[58]
Antigen detection
Antigen detection assays have also been described. The detection of secreted cysticercal Ag by ELISA is highly sensitive and specific for the diagnosis of living cysticerci (vesicular) localized in the subarachnoideal space at the base of the skull.[59,60] Antigen detection assays also permit monitoring and follow-up of anti-parasitic treatment.[39] Though the antigen detection reflects the presence of viable parasites, but a positive antigen detection test is no definitive indication of active NCC, because cysts can be located outside the CNS. Fleury et al. have shown the detection of secreted cysticercal antigen in CSF a useful tool for the diagnosis of inflammatory NCC.[60] Sensitivity was shown to be higher in cases with inflammation compared to non-inflammatory disease (94% vs. 33%) and in cases of multiple- compared with single-cyst cysticercosis (85% vs. 33%). Thus, antigen positivity is a strong indicator of active, inflammatory, multiple-cyst NCC.[60] Garcia et al. evaluated the utility of circulating parasite antigen in sera of patients with hydrocephalous secondary to NCC.[61] The assay gave positive results in 48% of patients with hydrocephalus, but was consistently negative in patients with calcifications. A study from Peruvian individuals demonstrated the sensitivity of 86% for detection of antigen in CSF by ELISA.[62] Negative results were restricted to patients with only a single live cyst or only enhancing lesions. Thus, though the sensitivity was high in multiple cystic lesions, but it had poor diagnostic value in patients having single cyst.
Most of the immunodiagnostic tests need elaborate standardization and cannot be performed with ease at rural areas and underdeveloped regions where the actual burden of disease is present. This creates a necessity of exploration of simpler tests with/without use of non-invasive samples, which can be utilized for point-of-care service. Such tests have not, though, seen the light of the day to be truly useful for patient care in large scale settings. Simple and rapid latex-based agglutination test for detection of T. solium metacestode antigen in the CSF and serum has been evaluated for diagnosis of NCC exhibiting sensitivity and specificity of 64% and 85% and 52% and 96% in CSF and serum samples, respectively.[63] Non-invasive samples such as urine and saliva have also been evaluated for antigen detection. Parija et al. reported a sensitivity of 62% and specificity of 91% for detection of cysticercus antigen in urine specimens using a polyclonal antibody-based ELISA assay.[64] Castillo et al. reported 92% sensitivity of urine antigen detection for viable parasites, which decreased to 62% in single cyst patients.[65]
Molecular techniques
More recently, methods based on detection of cysticercal deoxyribonucleic acid (DNA) have been increasingly explored. Nucleic acid amplification techniques may provide an answer to the challenge of diagnosis of NCC by virtue of their high sensitivity and specificity, ability to detect parasite load and faster turn-around-time. Both conventional and real-time polymerase chain reaction (PCR) assays have been developed for diagnosis of NCC in CSF samples. In a study, using highly repetitive elements of the parasite as probes, as little as 10 fg of T. solium DNA has been detected by PCR in CSF of 96% patients.[66] A semi-nested PCR based on HDP2 able to detect 0.174 fg of T. solium DNA has been reported.[28,67] PCR based on pTsol9 amplification detected 90-100% of NCC cases depending on stage and location of the parasite, exhibiting 95% sensitivity and variable specificity (80% or 100%) depending on the controls used.[57] A real-time TaqMan based PCR has been developed targeting pTsol9 gene yielding a sensitivity of 92% and specificity of 100% in CSF samples from patients with definitive NCC.[68] There is a lack of literature regarding the usefulness of molecular diagnosis of NCC in patients with single lesions, in serum samples and whether parasite DNA load in CSF can be used for follow-up of NCC patients. Solitary NCC lesions are often missed by serological methods and laboratory confirmation of such cases is a major challenge. Thus detection of parasite DNA by PCR can aid in diagnosing cases, which are missed by available radiological or immunological tests.
Treatment
The treatment of NCC is controversial and despite several advances, the various therapies remain either suboptimal or based on empiric observations and subsequent refinements through clinical trials.[69] The treatment depends on anatomic location, stage of evolution, number of cysts, degree of inflammation, severity of disease and life-threatening complications which require emergency treatment. Both praziquantel and albendazole are proven cysticidal agents, though their effectiveness is variable and a single course of anti-parasitic therapy may not eliminate all cysts. A meta-analysis assessing the effect of cysticidal drugs on neuroimaging and clinical outcomes of patients with NCC concluded that with therapy there is better resolution of colloidal and vesicular cysticerci, with lower recurrence of seizures in patients with colloidal cysticerci and a reduction in the rate of generalized seizures in patients with vesicular cysticerci.[70] More randomized controlled studies are required in future studies to evaluate and identify more efficacious and safe anthelmintic agents, better combinations of agents and better regimens. Surgery plays a role in the treatment of complicated disease, in removal of easily approachable symptomatic cysts through neuroendoscopy, removal of large approachable cysts that are likely to lead to long-term exposure to immunosuppressives or anthelmintics by open surgery, or shunt placement for hydrocephalus.[69]
Prevention
NCC is a preventable and eradicable disease. The transmission of parasite is related to social, cultural and economic factors such as poverty, inadequate sanitation and close association of humans with pigs with access of pigs to areas used for defecation. Hence the control measures, which are certain to be effective are health education, improved socio-economic conditions and life-style changes, mass treatment of carriers, restricted sale of measly pork and full cooking of pork.[23] Another important measure to break the host-parasite transmission cycle is the development of vaccines targeting cysticercosis in pigs which are safe, effective, inexpensive and administrable in edible form. Flisser et al. have evaluated recombinant oncosphere antigens TSOL18 and TSOL45-1A to induce 100% protection in three independent vaccine trials in pigs in Mexico and Cameroon.[71] Gauci et al. evaluated the recombinant antigens TSOL16, TSOL45-1A and TSOL45-1B and found TSOL16 to be capable of inducing high levels of immunity in pigs against a challenge infection.[72] Further studies are thus required for production of effective vaccines, which would aid in control and eradication of NCC.
CONCLUSION
NCC is an important cause of morbidity and mortality in humans. Being a disease of poor socio-economic strata, the approach toward control of this disease is multi-sectorial; the control requiring not just delivery of practical instruments of diagnosis, treatment and prevention by science, but also commitment at administrative and political level, which is required to improve basic health care infrastructure of endemic nations. A simple measure such as provision of adequate sanitary latrines to prevent indiscriminate defecation can effectively prevent millions of cases of epilepsy. Despite being the most common cause of adult-acquired epilepsy world-wide, the morbidity due to NCC is underappreciated and research is underfunded and hence the study of NCC lags behind most other major infectious diseases.[73] A balanced commitment of resources to develop more effective approaches that could lead to better treatment and control of the disease may be the key to improve the quality-of-life of millions of people.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Ramesh V. Cysticercosis. Int J Dermatol. 1984;23:348–50. doi: 10.1111/j.1365-4362.1984.tb04067.x. [DOI] [PubMed] [Google Scholar]
- 2.Nieto D. Historical notes on cysticerocsis. In: Flisser A, Wilms K, Laclette JP, Larralde C, Ridaura C, Beltran F, editors. Cysticercosis. Present State of Knowledge and Perspectives. New York: Academic Press Inc; 1982. pp. 1–7. [Google Scholar]
- 3.Garcia HH, Del Brutto OH. Taenia solium cysticercosis. Infect Dis Clin North Am. 2000;14:97–119. doi: 10.1016/s0891-5520(05)70220-8. ix. [DOI] [PubMed] [Google Scholar]
- 4.Giri S, Parija SC. A review on diagnostic and preventive aspects of cystic echinococcosis and human cysticercosis. Trop Parasitol. 2012;2:99–108. doi: 10.4103/2229-5070.105174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coyle CM, Mahanty S, Zunt JR, Wallin MT, Cantey PT, White AC, Jr, et al. Neurocysticercosis: Neglected but not forgotten. PLoS Negl Trop Dis. 2012;6:e1500. doi: 10.1371/journal.pntd.0001500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Savioli LS, Daumerie D. Geneva: World Health Organisation; 2010. First WHO Report on Neglected Tropical Diseases: Working to Overcome the Global Impact of Neglected Tropical Diseases. WHO/HTM/NTD/2010.1. [Google Scholar]
- 7.White AC., Jr Neurocysticercosis: A major cause of neurological disease worldwide. Clin Infect Dis. 1997;24:101–13. doi: 10.1093/clinids/24.2.101. [DOI] [PubMed] [Google Scholar]
- 8.Walker J, Chen S, Packham D, McIntyre P. Five cases of neurocysticercosis diagnosed in Sydney. Southeast Asian J Trop Med Public Health. 1991;22:242–4. [PubMed] [Google Scholar]
- 9.Lustigman S, Prichard RK, Gazzinelli A, Grant WN, Boatin BA, McCarthy JS, et al. A research agenda for helminth diseases of humans: The problem of helminthiases. PLoS Negl Trop Dis. 2012;6:e1582. doi: 10.1371/journal.pntd.0001582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ndimubanzi PC, Carabin H, Budke CM, Nguyen H, Qian YJ, Rainwater E, et al. A systematic review of the frequency of neurocyticercosis with a focus on people with epilepsy. PLoS Negl Trop Dis. 2010;4:e870. doi: 10.1371/journal.pntd.0000870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sanchez AL, Ljungström I, Medina MT. Diagnosis of human neurocysticerocosis in endemic countries: A clinical study in Honduras. Parasitol Int. 1999;48:81–9. doi: 10.1016/s1383-5769(99)00007-0. [DOI] [PubMed] [Google Scholar]
- 12.Praet N, Speybroeck N, Manzanedo R, Berkvens D, Nsame Nforninwe D, Zoli A, et al. The disease burden of Taenia solium cysticercosis in Cameroon. PLoS Negl Trop Dis. 2009;3:e406. doi: 10.1371/journal.pntd.0000406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Montano SM, Villaran MV, Ylquimiche L, Figueroa JJ, Rodriguez S, Bautista CT, et al. Neurocysticercosis: Association between seizures, serology, and brain CT in rural Peru. Neurology. 2005;65:229–33. doi: 10.1212/01.wnl.0000168828.83461.09. [DOI] [PubMed] [Google Scholar]
- 14.Rajshekhar V, Raghava MV, Prabhakaran V, Oommen A, Muliyil J. Active epilepsy as an index of burden of neurocysticercosis in Vellore district, India. Neurology. 2006;67:2135–9. doi: 10.1212/01.wnl.0000249113.11824.64. [DOI] [PubMed] [Google Scholar]
- 15.Parija SC, Raman GA. Anti-Taenia solium larval stage Ig G antibodies in patients with epileptic seizures. Trop Parasitol. 2011;1:20–5. doi: 10.4103/2229-5070.72113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parija SC, Balamurungan N, Sahu PS, Subbaiah SP. Cysticercus antibodies and antigens in serum from blood donors from Pondicherry, India. Rev Inst Med Trop Sao Paulo. 2005;47:227–30. doi: 10.1590/s0036-46652005000400010. [DOI] [PubMed] [Google Scholar]
- 17.Khurana S, Aggarwal A, Malla N. Prevalence of anti-cysticercus antibodies in slum, rural and urban populations in and around Union territory, Chandigarh. Indian J Pathol Microbiol. 2006;49:51–3. [PubMed] [Google Scholar]
- 18.Prasad KN, Prasad A, Gupta RK, Nath K, Pradhan S, Tripathi M, et al. Neurocysticercosis in patients with active epilepsy from the pig farming community of Lucknow district, north India. Trans R Soc Trop Med Hyg. 2009;103:144–50. doi: 10.1016/j.trstmh.2008.07.015. [DOI] [PubMed] [Google Scholar]
- 19.García HH, Evans CA, Nash TE, Takayanagui OM, White AC, Jr, Botero D, et al. Current consensus guidelines for treatment of neurocysticercosis. Clin Microbiol Rev. 2002;15:747–56. doi: 10.1128/CMR.15.4.747-756.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carlos R, Contreras E, Rivera H, Galvez M. Extracranial head and neck cysticercosis: Report of nine cases with emphasis in serologic analysis and natural history of the disease. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:196–8. [Google Scholar]
- 21.Jain S, Kumar S, Joshi D, Kaushal A. Racemose cysticercosis presenting as cystic neck swelling. Trop Parasitol. 2012;2:55–7. doi: 10.4103/2229-5070.97241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bothale KA, Mahore SD, Maimoon SA. A rare case of disseminated cysticercosis. Trop Parasitol. 2012;2:138–41. doi: 10.4103/2229-5070.105183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prasad KN, Prasad A, Verma A, Singh AK. Human cysticercosis and Indian scenario: A review. J Biosci. 2008;33:571–82. doi: 10.1007/s12038-008-0075-y. [DOI] [PubMed] [Google Scholar]
- 24.Carabin H, Ndimubanzi PC, Budke CM, Nguyen H, Qian Y, Cowan LD, et al. Clinical manifestations associated with neurocysticercosis: A systematic review. PLoS Negl Trop Dis. 2011;5:e1152. doi: 10.1371/journal.pntd.0001152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bickerstaff ER, Cloake PC, Hughes B, Smith WT. The racemose form of cerebral cysticercosis. Brain. 1952;75:1–18. doi: 10.1093/brain/75.1.1. [DOI] [PubMed] [Google Scholar]
- 26.Rabiela MT, Rivas A, Flisser A. Morphological types of Taenia solium cysticerci. Parasitol Today. 1989;5:357–9. doi: 10.1016/0169-4758(89)90111-7. [DOI] [PubMed] [Google Scholar]
- 27.Fleury A, Morales J, Bobes RJ, Dumas M, Yánez O, Piña J, et al. An epidemiological study of familial neurocysticercosis in an endemic Mexican community. Trans R Soc Trop Med Hyg. 2006;100:551–8. doi: 10.1016/j.trstmh.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 28.Hernández M, Gonzalez LM, Fleury A, Saenz B, Parkhouse RM, Harrison LJ, et al. Neurocysticercosis: Detection of Taenia solium DNA in human cerebrospinal fluid using a semi-nested PCR based on HDP2. Ann Trop Med Parasitol. 2008;102:317–23. doi: 10.1179/136485908X278856. [DOI] [PubMed] [Google Scholar]
- 29.Singh G. Neurocysticercosos in South-Central America and the Indian subcontinent. A comparative evaluation. Arq Neuropsiquiatr. 1997;55:349–56. doi: 10.1590/s0004-282x1997000300001. [DOI] [PubMed] [Google Scholar]
- 30.Fleury A, Escobar A, Fragoso G, Sciutto E, Larralde C. Clinical heterogeneity of human neurocysticercosis results from complex interactions among parasite, host and environmental factors. Trans R Soc Trop Med Hyg. 2010;104:243–50. doi: 10.1016/j.trstmh.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 31.Maravilla P, Gonzalez-Guzman R, Zuñiga G, Peniche A, Dominguez-Alpizar JL, Reyes-Montes R, et al. Genetic polymorphism in Taenia solium cysticerci recovered from experimental infections in pigs. Infect Genet Evol. 2008;8:213–6. doi: 10.1016/j.meegid.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 32.Del Brutto OH, Granados G, Talamas O, Sotelo J, Gorodezky C. Genetic pattern of the HLA system: HLA A, B, C, DR, and DQ antigens in Mexican patients with parenchymal brain cysticercosis. Hum Biol. 1991;63:85–93. [PubMed] [Google Scholar]
- 33.Jain S, Padma MV, Kanga U, Puri A, Mehra NK, Maheshwari MC. Human leukocyte antigen studies in Indian probands with seizures associated with single small enhancing computed tomography lesions and seizure types in their family members. J Epilepsy. 1997;10:55–61. [Google Scholar]
- 34.Jain S, Padma MV, Kanga U, Mehra NK, Puri A, Maheshwari MC. Family studies and human leukocyte antigen class II typing in Indian probands with seizures in association with single small enhancing computed tomography lesions. Epilepsia. 1999;40:232–8. doi: 10.1111/j.1528-1157.1999.tb02080.x. [DOI] [PubMed] [Google Scholar]
- 35.García HH, Gonzalez AE, Rodriguez S, Tsang VC, Pretell EJ, Gonzales I, et al. Neurocysticercosis: Unraveling the nature of the single cysticercal granuloma. Neurology. 2010;75:654–8. doi: 10.1212/WNL.0b013e3181ed9eae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rajshekhar V. Etiology and management of single small CT lesions in patients with seizures: Understanding a controversy. Acta Neurol Scand. 1991;84:465–70. doi: 10.1111/j.1600-0404.1991.tb04996.x. [DOI] [PubMed] [Google Scholar]
- 37.Garcia HH, Del Brutto OH, Nash TE, White AC, Jr, Tsang VC, Gilman RH. New concepts in the diagnosis and management of neurocysticercosis (Taenia solium) Am J Trop Med Hyg. 2005;72:3–9. [PubMed] [Google Scholar]
- 38.Osborn AG, Preece MT. Intracranial cysts: Radiologic-pathologic correlation and imaging approach. Radiology. 2006;239:650–64. doi: 10.1148/radiol.2393050823. [DOI] [PubMed] [Google Scholar]
- 39.Garcia HH, Del Brutto OH Cysticercosis Working Group in Peru. Neurocysticercosis: Updated concepts about an old disease. Lancet Neurol. 2005;4:653–61. doi: 10.1016/S1474-4422(05)70194-0. [DOI] [PubMed] [Google Scholar]
- 40.Garcia HH, Herrera G, Gilman RH, Tsang VC, Pilcher JB, Diaz JF, et al. Discrepancies between cerebral computed tomography and western blot in the diagnosis of neurocysticercosis. The Cysticercosis Working Group in Peru (Clinical Studies Coordination Board) Am J Trop Med Hyg. 1994;50:152–7. doi: 10.4269/ajtmh.1994.50.152. [DOI] [PubMed] [Google Scholar]
- 41.Sciutto E, Fragoso G, Fleury A, Laclette JP, Sotelo J, Aluja A, et al. Taenia solium disease in humans and pigs: An ancient parasitosis disease rooted in developing countries and emerging as a major health problem of global dimensions. Microbes Infect. 2000;2:1875–90. doi: 10.1016/s1286-4579(00)01336-8. [DOI] [PubMed] [Google Scholar]
- 42.Del Brutto OH, Rajshekhar V, White AC, Jr, Tsang VC, Nash TE, Takayanagui OM, et al. Proposed diagnostic criteria for neurocysticercosis. Neurology. 2001;57:177–83. doi: 10.1212/wnl.57.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Das S, Mahajan RC, Ganguly NK, Sawhney IM, Dhawan V, Malla N. Detection of antigen B of Cysticercus cellulosae in cerebrospinal fluid for the diagnosis of human neurocysticercosis. Trop Med Int Health. 2002;7:53–8. doi: 10.1046/j.1365-3156.2002.00810.x. [DOI] [PubMed] [Google Scholar]
- 44.Flisser A, Woodhouse E, Larralde C. Human cysticercosis: Antigens, antibodies and non-responders. Clin Exp Immunol. 1980;39:27–37. [PMC free article] [PubMed] [Google Scholar]
- 45.Kaur M, Ganguly NK, Mahajan RC, Malla N. Identification of antigenic fractions of Cysticercus cellulosae by Western blotting in the serodiagnosis of human neurocysticercosis: Before and after treatment. Immunol Infect Dis. 1995;5:67–72. [Google Scholar]
- 46.Kaur M, Goyal R, Ganguly NK, Mahajan RC, Malla N. Evaluation and characterization of purified antigenic fraction-II of Cysticercus cellulosae by enzyme-linked immunosorbent assay for the diagnosis of neurocysticercosis: Before and after treatment. Immunol Infect Dis. 1996;6:25–9. [Google Scholar]
- 47.Mahajan RC, Chopra JS, Chitkara NL. Comparative evaluation of indirect haemagglutination and complement fixation tests in serodiagnosis of cysticercosis. Indian J Med Res. 1975;63:121–5. [PubMed] [Google Scholar]
- 48.Malla N, Kaur M, Kaur U, Ganguly NK, Mahajan RC. Evaluation of enzyme linked immunosorbent – Assay for the detection of anticysticercus antibodies in cerebrospinal fluid from patients with neurocysticercosis. J Hyg Epidemiol Microbiol Immunol. 1992;36:181–90. [PubMed] [Google Scholar]
- 49.Dorny P, Brandt J, Zoli A, Geerts S. Immunodiagnostic tools for human and porcine cysticercosis. Acta Trop. 2003;87:79–86. doi: 10.1016/s0001-706x(03)00058-5. [DOI] [PubMed] [Google Scholar]
- 50.Tsang VC, Brand JA, Boyer AE. An enzyme-linked immunoelectrotransfer blot assay and glycoprotein antigens for diagnosing human cysticercosis (Taenia solium) J Infect Dis. 1989;159:50–9. doi: 10.1093/infdis/159.1.50. [DOI] [PubMed] [Google Scholar]
- 51.Prabhakaran V, Rajshekhar V, Murrell KD, Oommen A. Taenia solium metacestode glycoproteins as diagnostic antigens for solitary cysticercus granuloma in Indian patients. Trans R Soc Trop Med Hyg. 2004;98:478–84. doi: 10.1016/j.trstmh.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 52.Garcia HH, Gilman RH, Catacora M, Verastegui M, Gonzalez AE, Tsang VC. Serologic evolution of neurocysticercosis patients after antiparasitic therapy. Cysticercosis Working Group in Peru. J Infect Dis. 1997;175:486–9. doi: 10.1093/infdis/175.2.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Larralde C, Montoya RM, Sciutto E, Diaz ML, Govezensky T, Coltorti E. Deciphering western blots of tapeworm antigens (Taenia solium, Echinococcus granulosus, and Taenia crassiceps) reacting with sera from neurocysticercosis and hydatid disease patients. Am J Trop Med Hyg. 1989;40:282–90. doi: 10.4269/ajtmh.1989.40.282. [DOI] [PubMed] [Google Scholar]
- 54.Atluri VS, Singhi PD, Khandelwal N, Malla N. 2D-PAGE analysis of Taenia solium metacestode 10-30 kDa antigens for the serodiagnosis of neurocysticercosis in children. Acta Trop. 2011;118:165–9. doi: 10.1016/j.actatropica.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 55.Tsang VC, Pilcher JA, Zhou W, Boyer AE, Kamango-Sollo EI, Rhoads ML, et al. Efficacy of the immunoblot assay for cysticercosis in pigs and modulated expression of distinct IgM/IgG activities to Taenia solium antigens in experimental infections. Vet Immunol Immunopathol. 1991;29:69–78. doi: 10.1016/0165-2427(91)90053-f. [DOI] [PubMed] [Google Scholar]
- 56.Hancock K, Khan A, Williams FB, Yushak ML, Pattabhi S, Noh J, et al. Characterization of the 8-kilodalton antigens of Taenia solium metacestodes and evaluation of their use in an enzyme-linked immunosorbent assay for serodiagnosis. J Clin Microbiol. 2003;41:2577–86. doi: 10.1128/JCM.41.6.2577-2586.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Michelet L, Fleury A, Sciutto E, Kendjo E, Fragoso G, Paris L, et al. Human neurocysticercosis: Comparison of different diagnostic tests using cerebrospinal fluid. J Clin Microbiol. 2011;49:195–200. doi: 10.1128/JCM.01554-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mandal J, Singhi PD, Khandelwal N, Malla N. Evaluation of ELISA and dot blots for the serodiagnosis of neurocysticercosis, in children found to have single or multiple enhancing lesions in computerized tomographic scans of the brain. Ann Trop Med Parasitol. 2006;100:39–48. doi: 10.1179/136485906X78445. [DOI] [PubMed] [Google Scholar]
- 59.Fleury A, Hernández M, Avila M, Cárdenas G, Bobes RJ, Huerta M, et al. Detection of HP10 antigen in serum for diagnosis and follow-up of subarachnoidal and intraventricular human neurocysticercosis. J Neurol Neurosurg Psychiatry. 2007;78:970–4. doi: 10.1136/jnnp.2006.107243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fleury A, Hernández M, Fragoso G, Parkhouse RM, Harrison LJ, Sciutto E. Detection of secreted cysticercal antigen: A useful tool in the diagnosis of inflammatory neurocysticercosis. Trans R Soc Trop Med Hyg. 2003;97:542–6. doi: 10.1016/s0035-9203(03)80019-6. [DOI] [PubMed] [Google Scholar]
- 61.Garcia HH, Gonzalez AE, Gilman RH, Bernal T, Rodriguez S, Pretell EJ, et al. Circulating parasite antigen in patients with hydrocephalus secondary to neurocysticercosis. Am J Trop Med Hyg. 2002;66:427–30. doi: 10.4269/ajtmh.2002.66.427. [DOI] [PubMed] [Google Scholar]
- 62.Garcia HH, Harrison LJ, Parkhouse RM, Montenegro T, Martinez SM, Tsang VC, et al. A specific antigen-detection ELISA for the diagnosis of human neurocysticercosis. The Cysticercosis Working Group in Peru. Trans R Soc Trop Med Hyg. 1998;92:411–4. doi: 10.1016/s0035-9203(98)91069-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Biswas R, Parija SC. A rapid slide agglutination test for the diagnosis of neurocysticercosis in the rural health set up. Trop Parasitol. 2011;1:94–8. doi: 10.4103/2229-5070.86942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Parija M, Biswas R, Harish BN, Parija SC. Detection of specific cysticercus antigen in the urine for diagnosis of neurocysticercosis. Acta Trop. 2004;92:253–60. doi: 10.1016/j.actatropica.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 65.Castillo Y, Rodriguez S, García HH, Brandt J, Van Hul A, Silva M, et al. Urine antigen detection for the diagnosis of human neurocysticercosis. Am J Trop Med Hyg. 2009;80:379–83. [PubMed] [Google Scholar]
- 66.Almeida CR, Ojopi EP, Nunes CM, Machado LR, Takayanagui OM, Livramento JA, et al. Taenia solium DNA is present in the cerebrospinal fluid of neurocysticercosis patients and can be used for diagnosis. Eur Arch Psychiatry Clin Neurosci. 2006;256:307–10. doi: 10.1007/s00406-006-0612-3. [DOI] [PubMed] [Google Scholar]
- 67.Harrison LJ, Delgado J, Parkhouse RM. Differential diagnosis of Taenia saginata and Taenia solium with DNA probes. Parasitology. 1990;100(Pt 3):459–61. doi: 10.1017/s0031182000078768. [DOI] [PubMed] [Google Scholar]
- 68.Yera H, Dupont D, Houze S, Ben M’rad M, Pilleux F, Sulahian A, et al. Confirmation and follow-up of neurocysticercosis by real-time PCR in cerebrospinal fluid samples of patients living in France. J Clin Microbiol. 2011;49:4338–40. doi: 10.1128/JCM.05839-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nash TE, Singh G, White AC, Rajshekhar V, Loeb JA, Proaño JV, et al. Treatment of neurocysticercosis: Current status and future research needs. Neurology. 2006;67:1120–7. doi: 10.1212/01.wnl.0000238514.51747.3a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Del Brutto OH, Roos KL, Coffey CS, García HH. Meta-analysis: Cysticidal drugs for neurocysticercosis: Albendazole and praziquantel. Ann Intern Med. 2006;145:43–51. doi: 10.7326/0003-4819-145-1-200607040-00009. [DOI] [PubMed] [Google Scholar]
- 71.Flisser A, Gauci CG, Zoli A, Martinez-Ocaña J, Garza-Rodriguez A, Dominguez-Alpizar JL, et al. Induction of protection against porcine cysticercosis by vaccination with recombinant oncosphere antigens. Infect Immun. 2004;72:5292–7. doi: 10.1128/IAI.72.9.5292-5297.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gauci CG, Jayashi CM, Gonzalez AE, Lackenby J, Lightowlers MW. Protection of pigs against Taenia solium cysticercosis by immunization with novel recombinant antigens. Vaccine. 2012;30:3824–8. doi: 10.1016/j.vaccine.2012.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nash TE, Mahanty S, Garcia HH. Neurocysticercosis-more than a neglected disease. PLoS Negl Trop Dis. 2013;7:e1964. doi: 10.1371/journal.pntd.0001964. [DOI] [PMC free article] [PubMed] [Google Scholar]


