Abstract
Hydatid disease is an endemic and common zoonosis in India. Liver is the most common site of infection. However, extra hepatic primary pancreatic hydatid cyst is rare. We report a case of primary hydatid cyst in the tail of pancreas compressing the adjacent organs in a 43-year-old male who presented with abdominal mass and was diagnosed as pancreatic cyst/splenic cyst by ultrasonography. Computed tomography of abdomen revealed a large cystic lesion in the tail of pancreas suggestive of a pseudocyst of pancreas. The case was managed surgically by splenectomy and distal pancreatectomy with albendazole therapy. Microbiological Investigations of aspirated fluid revealed free hooklets and invaginated scolices of Echinococcus granulosus, which was correlated with histopathological findings.
KEY WORDS: Hydatid cyst, invaginated scolices, pseudocyst
Primary pancreatic hydatid cysts are most often confused with cystic lesions of the pancreas and pancreatic pseudocyst. Human hydatidosis, a zoonotic disease most commonly caused by larval stages of Echinococcus granulosus. Though, liver is the most common site followed by the lung, rarely the primary sites are spared and the infection may spread by venous circulation to other organs like spleen, pancreas, kidney, and soft-tissues.[1]
Primary hydatid cyst of pancreas is rare. During the last 30 years, less than 40 cases have been reported in journals on Medline.[2] The reported incidence of hydatid cyst of pancreas is 0.25%.[3] The incidence varies from 0.14% to 2.0% in endemic countries. The head of pancreas is most frequent location 57% followed by the corpus 24% than the tail 19%.[4]
Diagnosing hydatid cyst of pancreas pre-operatively is difficult due to its rarity. Computed tomography (CT) scan is helpful in identifying curvilinear calcifications and the presence of daughter cysts.[2] However, final diagnosis can be confirmed only by microscopic examination for hydatid sand supported by histopathology.
THE CASE
A 43-year-old male patient came to the out-patient consultation of the Department of Surgery with complaints of abdominal fullness and shortness of breath, only on exertion since 6 months. He noted a small mass in the left side of abdomen, which was found to be gradually increasing in size. He had occasional episodes of dull aching pain below the left ribcage. No history of trauma, radiating pain, bloating sensation, vomiting or constipation was reported. He is an alcoholic, non-smoker, non-hypertensive, and non-diabetic. On physical examination, the patient was moderately built and well-nourished, with normal vitals. Pulse rate was 96 beats/min, respiratory rate was 18/min, Blood Pressure was 130/80 mm of Hg.
Per abdominal examination revealed a swelling of 15 cm × 8 cm diameter, which was irregular, firm, non-tender, and bimanually palpable, in the epigastric and left hypochondriac region extending to the lumbar regions posteriorly up to the midline. The swelling was reducing in size on raising both lower limbs, but not falling in knee elbow position. All quadrants were moving equally with respiration. No local rise of temperature and no visible pulsations were seen.
Radiological examination, [Figure 1] on ultrasonography of the abdomen revealed moderate splenomegaly and a 20 cm × 14 cm cystic lesion in the region of the tail of pancreas compressing the splenic tissue and displacing the left kidney. The impression was suggestive of a large pseudocyst in the tail of pancreas/splenic cyst. CT scan of the abdomen showed a large 18 cm × 17 × 15 cm cystic lesion in the region of the tail of the pancreas. The tail of pancreas was stretched along the cyst and spleen was not visualized. The impression was suggestive of pseudopancreatic cyst with the possibility of splenic cyst also to be considered. Hematological investigations showed normal blood picture. Liver function tests were normal. Serum amylase was increased drastically to 4630 U/L when compared to the normal value, which is 100 U/L.
Figure 1.
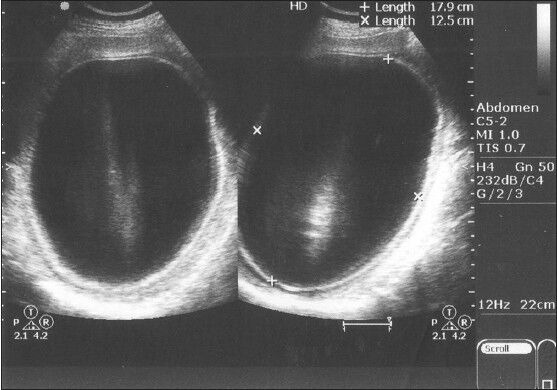
Ultrasound picture showing huge cystic lesion in the tail of pancreas
Pre-operatively, pseudocyst of pancreas was suspected and meningococcal and pneumococcal vaccines were administered. Perioperatively, splenectomy with distal pancreatectomy was carried out. Cyst fluid was sent for laboratory investigations to Departments of Microbiology and Pathology. In the Microbiology Department, on macroscopic observation, the fluid was pale yellow colored and turbid with deposits and membranous structures [Figure 2]. Microscopic examination of the cyst fluid showed invaginated scolices and free hooklets, suggestive of hydatid cyst of E. granulosus. The findings were correlated with histopathological examination showing lamellated membrane of hydatid cyst with brood capsules in both splenic and pancreatic tissue.
Figure 2.

Direct microscopic observation of cyst fluid showing the scolex with hooklets
CONCLUSIONS
E. granulosus is known to cause cystic infestations primarily in the liver or lung. The location of the cysts is mostly hepatic (75%) followed by pulmonary (15%) and only a 10% occurs in the rest of the body.[5] The incidence of primary extra hepatic hydatid disease is rare. Here, we would like to discuss a case of hydatidosis of pancreas. Hydatid cysts of pancreas are rare and very difficult to distinguish from cystic neoplasm of pancreas. The possible sources of infestation could include, hematogenous dissemination, local spread via pancreatobiliary ducts or by peripancreatic lymphatic invasion.[6]
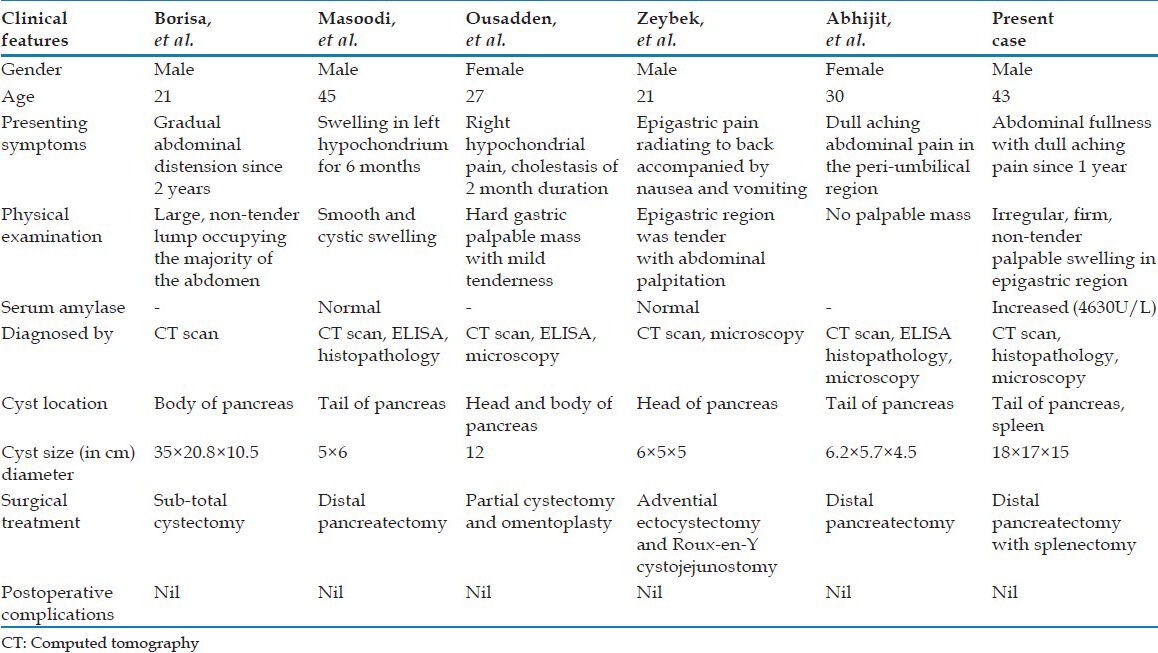
The clinical manifestations of hydatidosis in human are variable and insidious depending on the location and size of the cyst [Table 1]. Corpus and tail cysts of pancreas rarely show any symptoms. Most patients tolerate the infection for extended periods without any symptomatology or they may suddenly show dramatic and acute symptoms.[7] In the present case, the patient had abdominal fullness and episodes of dull aching pain since 1 year. The hydatid cysts of the pancreas often have severe adhesions to surrounding structures and do not communicate with pancreatic ducts.[6] In our case, cyst was seen along the tail of pancreas and spleen, adhering to diaphragm, splenic flexure, and stomach.
Table 1.
Salient features of a few reported cases of hydatid disease of pancreas
On abdominal ultrasonography, a cystic mass in pancreas was seen. Abdominal CT scan shows the presence of cyst in the pancreas and splenic region. Hematological investigations showed a normal complete blood picture and normal liver function tests. Serum Amylase was enormously increased, which was supportive for the involvement of pancreas. In our case pre-operatively, a provisional diagnosis of pseudocyst of pancreas was considered with splenic involvement. The differential diagnosis of cystic lesions of the pancreas is extensive and includes pseudocysts, Cystic neoplasms, and other rare tumors.[8] There are few reports in the literature, in which a cyst in the tail of pancreas was managed by distal pancreatectomy with splenectomy.[8]
As the cyst was huge in size and adherent to the adjacent structures, cyst decompression with distal pancreatectomy and splenectomy was planned and surgical removal of the cyst was carried out. Pneumococcal and meningococcal vaccines were also administered preoperatively. The cyst, after post-operative laboratory investigations was diagnosed as hydatid cyst. The diagnosis of a hydatid cyst of pancreas is easily confused with other more commonly encountered cystic lesions and is extremely difficult and can rarely be established pre-operatively.[4] A high index of suspicion, peripheral eosinophilia, typical findings of imaging studies, and a history of exposure in an endemic area are some hints to the diagnosis.[5]
Albendazole therapy with surgical resection is the treatment of choice for hepatic and pancreatic echinococcal cysts.[5] Peri-operative chemotherapy using albendazole has been shown to reduce the incidence of recurrent disease.[5] In our case, the patient was put on albendazole therapy for 6 months and periodic surveillance was done by abdominal ultrasonography and CT scan. Postoperative period was good and uneventful.
Hence to conclude, though primary hydatid disease in the tail of pancreas is extremely rare, the clinician should always consider it as differential diagnosis in diagnosing and treating patients presenting with cystic lesions of pancreas.
ACKNOWLEDGMENTS
We sincerely thank the management of our institution and also the staff members of our Department of Microbiology for their kind support, encouragement and cooperation.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Chatterjee KD. Echinococcus granulosis. In: Chatterjee KD, editor. Parasitology in Clinical Medicine. Clacutta: Academic; 1981. [Google Scholar]
- 2.Borisa AD, Bakhshi GD, Tayade MB, Pawar NH, Nikam NN, Pathrikar S. Hydatid cyst of pancreas. Bombay Hosp J. 2009;51:88–90. [Google Scholar]
- 3.Masoodi I, Nabi G, Kumar R, Lone MA, Khan BA, Naseer Al Sayari K. Hydatid cyst of the pancreas: A case report and brief review. Turk J Gastroenterol. 2011;22:430–2. doi: 10.4318/tjg.2011.0259. [DOI] [PubMed] [Google Scholar]
- 4.Ousadden A, Elbouhaddouti H, Ibnmajdoub KH, Mazaz K, Aittaleb K. Primary hydatid cyst of the pancreas with a hepatic pedicule compression. Cases J. 2009;2:201. doi: 10.1186/1757-1626-2-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zeybek N, Tas H, Kaymakcioglu N, Ozcan A, Cetiner S, Tufan T. Hydatid cyst in the head of the pancreas in an adult: Case report. Med J Kocatepe. 2006;7:9–12. [Google Scholar]
- 6.Wani RA, Wani I, Malik AA, Parray FQ, Wani AA, Dar AM. Hydatid disease at unusual sites. Int J Case Reposts Images. 2012;3:1–6. [Google Scholar]
- 7.Elshazly AM, Azab MS, Elbeshbishi SN, Elsheikha HM. Hepatic hydatid disease: Four case reports. Cases J. 2009;2:58. doi: 10.1186/1757-1626-2-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abhijit R, Prabhu R, Kantharia C, Supe A. Isolated pancreatic hydatid cyst: Preoperative prediction on contrast-enhanced computed tomography case report and review of literature. M J Dr. D. Y. Patil Univ. 2012;5:66–8. [Google Scholar]


