Abstract
There has been a growing interest in examining dietary energy density (ED, kcal/g) as it relates to various health outcomes. Consuming a diet low in ED has been recommended in the 2010 Dietary Guidelines, as well as by other agencies, as a dietary approach for disease prevention. Translating this recommendation into practice; however, is difficult. Currently there is no standardized method for calculating dietary ED; as dietary ED can be calculated with foods alone, or with a combination of foods and beverages. Certain items may be defined as either a food or a beverage (e.g., meal replacement shakes) and require special attention. National survey data are an excellent resource for evaluating factors that are important to dietary ED calculation. The National Health and Nutrition Examination Survey (NHANES) nutrient and food database does not include an ED variable, thus researchers must independently calculate ED. The objective of this study was to provide information that will inform the selection of a standardized ED calculation method by comparing and contrasting methods for ED calculation. The present study evaluates all consumed items and defines foods and beverages based on both USDA food codes and how the item was consumed. Results are presented as mean EDs for the different calculation methods stratified by population demographics (e.g. age, sex). Using United State Department of Agriculture (USDA) food codes in the 2005–2008 NHANES, a standardized method for calculating dietary ED can be derived. This method can then be adapted by other researchers for consistency across studies.
Keywords: energy density; National Health and Nutrition Examination Survey, NHANES; What We Eat in America, WWEIA; USDA
1. Introduction
Energy density (ED), or the amount of energy (in kilocalories) per amount of food (in grams), is a property of food. As such, ED can be calculated for mixed dishes, meals, and the total diet by dividing total kilocalories by total grams. ED is influenced by various food components, such as the macronutrient and water content. Water has the greatest influence on the ED of a food because it adds substantial weight without adding energy. Of the macronutrients, fat is most influential because of its high energy content (9 kcal/g) relative to either protein or carbohydrate (both 4 kcal/g). In recent years, there has been a growing interest in evaluating dietary ED as a risk factor for obesity, diabetes, and other diseases. Organizations including the joint American Institute for Cancer Research / World Cancer Research Fund, the USDA, and 2010 Dietary Guidelines for Americans have recommended consumption of a diet low in ED as a dietary approach to disease prevention, particularly for the prevention of obesity [1,2]. A diet lower in ED tends to be higher in water-rich foods such as fruits and vegetables, has more fiber and is lower in fat than other types of diets. Several experimental studies have demonstrated that lowering the ED of a food also leads to decreased energy intake during a meal [3,4]. Though consumption of low-ED foods has many benefits, individuals commonly consume foods as mixed dishes and in meals, and identifying low-ED foods alone does not capture the total diet. Therefore, it is important to assess the ED of the entire diet when evaluating the association between ED and disease.
The majority of studies evaluating the relationship between ED and disease are epidemiological in nature. Several population-based studies have examined the association between dietary ED and weight status. Most, but not all, studies have found a positive relationship between ED and body mass index (BMI) [5–8], including data from both men and women [5] and across several racial and ethnic groups [8]. One potential reason for the mixed results across studies may be related to differing methods for assessing dietary ED.
The What We Eat in America (WWEIA) component of the National Health and Nutrition Examination Survey (NHANES) is an excellent source of nationally representative dietary data, and serves as the basis for several studies about dietary ED [9]. The WWEIA component of NHANES has detailed information about each food and beverage consumed by individuals (including but not limited to energy, gram weight, macro- and micronutrient content for each item consumed) however, the WWEIA data does not include a variable for ED. As such, researchers who are interested in evaluating the relationship between ED and any disease outcome must calculate dietary ED on their own. Previous reports have identified several potential ways to calculate dietary ED in a nationally representative sample of US adults [10]. Dietary ED can be calculated using only foods, beverages, or a combination of foods and beverages. The majority of studies calculate ED using what is known as the “food-only” method – calculating dietary ED using only the grams of food consumed and excluding beverages. However, even this “food only” method is not standardized. The wide variety of items consumed by a population includes items that may be considered either a food or a beverage. For example: meal replacement shakes may be considered to be a food by one researcher, but as a beverage by another. The classification of items as “foods” or “beverages” is crucial. Due to their high water content, beverages can substantially influence dietary ED. Therefore, when assessing the relationship between dietary ED and various disease outcomes, it is important for researchers to use a consistent, standardized method to calculate ED. The goal of the present study is to provide information that will inform the selection of a standardized method for calculating dietary ED in future studies.
1.1. Methods & Materials
The National Health and Nutrition Examination Survey (NHANES) is a large, cross-sectional survey conducted by National Center for Health Statistics. NHANES is designed to monitor the health and nutritional status of non-institutionalized civilians in the US; data are collected on a continual basis and released in two-year increments. Complete details regarding the NHANES sampling methodology, data collection, and interview process are available on the NHANES website (http://www.cdc.gov/nchs/nhanes.htm). Data from the 2005–2008 survey cycles were combined for this manuscript.
Adults who participated in NHANES provided one day (24-hours) of dietary recall data during their visit to the mobile examination unit as part of the What We Eat In America (WWEIA) survey [9]. Dietary recall data were collected in-person by trained interviewers using the USDA’s Automated Multiple-Pass Method (AMPM), http://www.ars.usda.gov/Services/docs.htm?docid=7710. For each food or beverage reported during the interview, detailed information regarding when and where the item was consumed, how much was consumed, the name of the eating occasion, as well as whether the food or beverage was consumed in conjunction with any other items (i.e.: coffee with cream and sugar; or lettuce, tomatoes, carrots, olive oil and vinegar consumed together as a salad) was recorded. During processing of the dietary recall data each item reported was assigned an 8-digit USDA food code, then the total energy (in kcal), gram weight, and nutrient content was calculated for each item reported. Specific status codes were used to indicate the quality, reliability, and completeness of the dietary data, and variables to identify dieting status (e.g.: persons currently following a weight loss diet) were included in the 24-hour recall files. Two types of dietary recall files exist in the NHANES WWEIA: a dietary interview file, which has one line for each item reported by each individual (multiple rows of data per person); and a total nutrients file, which has the total energy, nutrient, and water intake for each individual (one row of data per person). The USDA Food and Nutrition Database for Dietary Studies (FNDDS), versions 3.0 and 4.1 were used to process NHANES WWEIA dietary data (http://www.ars.usda.gov/Services/docs.htm?docid=12089).
| Nomenclature | |
| NHANES | National Health and Nutrition Examination Survey |
| WWEIA | What We Eat In America |
| USDA | United Stated Department of Agriculture |
| FNDDS | Food and Nutrition Database for Dietary Studies |
| ED | Energy Density |
| BMI | Body Mass Index |
For this study ED (kcal/g) was calculated using two methods: (a) using foods and all beverages, including water, and (b) using only foods. ED is calculated by dividing the energy content (in kilocalories) by weight of foods (or foods + beverages in g) consumed. For the foods + all beverages method of calculating dietary ED, use the total nutrients file:
Dietary EDfood+beverage = Total energy (kcal) / total weight (g)
For the food only method of calculating dietary ED, the dietary interview file is required to identify, and subsequently eliminate, beverages. Within the dietary interview file there are three critical components needed to identify beverages: (1) the 8-digit USDA food codes, (2) variables to identify combination food type (herein referred to as “combination codes”) and (3) variables to identify the name of the meal (herein referred to as “meal codes”).
Using the USDA food codes, the following items can be identified as beverages:
Coffee, tea and herbal teas
Soda, soft drinks, sports drinks, and energy drinks
Fruit and / or vegetable juices
Alcoholic beverages and non-alcoholic beers
Bottled and flavored water
It is of note that the above list lacks two widely consumed types of beverages: tap water and milk (including non-dairy milk substitutes). In order to identify milk and water consumed as a beverage, additional information beyond the 8-digit food codes are needed. Milk and water are often consumed as ingredients or additional components for other items, as such, combination codes can be used identify these items (e.g., milk added to ready-to-eat cereal, or tap water added to cooked cereal). Combination food codes can also be used to identify additions to beverages. For example, if a person reported consuming 8 oz of coffee, 2 cubes of sugar, and 2 Tbsp of whole milk together, the item would be coded as “beverage with additions”. Without using the combination food codes, the coffee and milk would be identified as beverages and eliminated from any food-only calculations; however, the 2 cubes of sugar would not be eliminated, and would be counted towards the total caloric intake of foods-only. Use of the combination codes is critical for accurate identification of beverages. Also worth noting: in the present study, yogurt was always classified as a food.
Finally, in order to classify more ambiguous food items (e.g., meal replacement shakes), the meal codes are used. For the present study, meal replacement shakes are considered a food if they are consumed in place of a meal (e.g., a shake and a glass of water alone are identified as ‘lunch’ in the interview file, or a shake and an apple are identified as ‘dinner’); however, if the shake is consumed as a beverage or snack along with meal, the shake is identified as a beverage and eliminated from the food-only calculation. In addition to meal replacement shakes, different investigators often classify smoothies and popsicles differently. For the purposes of this study, any smoothie that consists entirely of blended whole fruits and vegetables (no added juice, yogurt, milk, or other liquids) is identified as food (an identification similar in theory to a puréed soup, where whole vegetables are pureed and consumed as a liquid food), where juice-based smoothies are identified as beverages. Frozen fruit- or juice-based desserts (such as popsicles and ices) were also considered foods for the purposes of this study. These items (smoothies, popsicles, and meal replacements) were reported by less than 0.7% of the population, and therefore are mostly inconsequential to ED calculation. Once all beverages have been identified and eliminated, dietary ED can be calculated using the food-only method as follows:
Dietary EDfood-only = food energy (kcal) / food weight (g)
This food-only calculation of ED can then be compared to the food+beverage calculation to evaluate the relationship between ED and various disease outcomes. Additionally, since beverages have been previously identified in order to calculate the food-only ED, EDbeverage-only can also be determined.
1.2. Results & Discussion
Depending on the method of calculating ED, the ED of the diet can vary greatly. Dietary ED can be calculated for individual foods, meals, and the total diet. Using a standardized method of identifying foods and beverages, two methods of calculating dietary ED can be used in nationally representative data. The classification of items consumed as foods and beverages can greatly influence the ED of foods (particularly mixed dishes), meals, and the overall diet. Table 1 provides an example of a sample breakfast in which meal ED may be calculated one of three ways.
Table 1.
Sample breakfast
| Food Code (description) | Combination Code | Meal Code | Energy (Kcal) | Grams |
|---|---|---|---|---|
| 51302010 (granola) | 2 | 1 | 178 | 75 |
| 11112110 (2% milk) | 2 | 1 | 122 | 61 |
| 61210220 (orange juice) | 1 | 1 | 130 | 240 |
For the above sample breakfast, there are three potential values for meal ED. If the food+beverage method is used, the meal ED is calculated by totaling kilocalories for all three items (430) and dividing by total grams (376) for an ED of 1.14kcal/g. If the food-only method is used, and beverages are identified using only the USDA food codes, both the milk and orange juice would be eliminated and the meal ED would be calculated using only kilocalories of granola (178) divided by grams of granola (75) for an ED of 2.37 kcal/g. Alternatively, if food-only ED is calculated using the USDA food codes in addition to the combination codes, the milk would be included with the granola as part of a complete dish, and only the orange juice would be eliminated, giving a meal total kilocalories of 300, and total grams of 136 for an ED of 2.21 kcal/g. The difference in meal ED can have meaningful implications. The current WCRF/AICR recommendations for cancer prevention include increasing intake of low-ED foods, such as fruits and vegetables, and limiting consumption of high-ED foods (defined as foods with an ED ≥2.25) as a method for preventing obesity [2]. This research is supported by several population-based studies that have examined the association between dietary ED and weight status. Most studies have found a positive relationship between ED and body mass index (BMI), [5–8] including data from both men and women [5] and across several racial and ethnic groups [8, 11]. In the sample breakfast shown in Table 1, misidentification of the cereal + additions would result in this food being classified as high-ED, and would influence overall dietary ED of the meal. The preferred method for ED calculation is, therefore, using the food-only calculation.
Beyond combination food codes, beverages themselves are influential in the calculation of dietary ED. Of the studies that have identified significant associations between dietary ED and weight status did so only when using the food-only method. Because water provides a great deal of weight without providing any energy, food and beverage items with a high water content can substantially lower the ED of foods, meals, and the entire diet. The influence of beverages on ED is especially noteworthy in meals that have a low moisture content. Table 2 provides an example of two sample lunch menus.
Table 2.
Comparison of two sample lunches
| Menu #1 Food Items |
Grams | Energy (kcal) | Menu #2 Food Items |
Grams | Energy (kcal) |
|---|---|---|---|---|---|
| Turkey wrap | 383 | 350 | Fast food burger | 206 | 460 |
| 2 clementine oranges | 148 | 70 | French fries | 154 | 500 |
| 1 bottle water | 422 | 0 | Large soda (diet) | 908 | 310 (0) |
| Total | 953 | 420 | Total (diet) | 1340 | 1270 (960) |
| Food-only ED | 0.79 kcal/g | Food-only ED | 2.67 kcal/g | ||
| Food+bev ED | 0.44 kcal/g | Food+bev ED (diet) | 1.00 kcal / (0.75 kcal/g) |
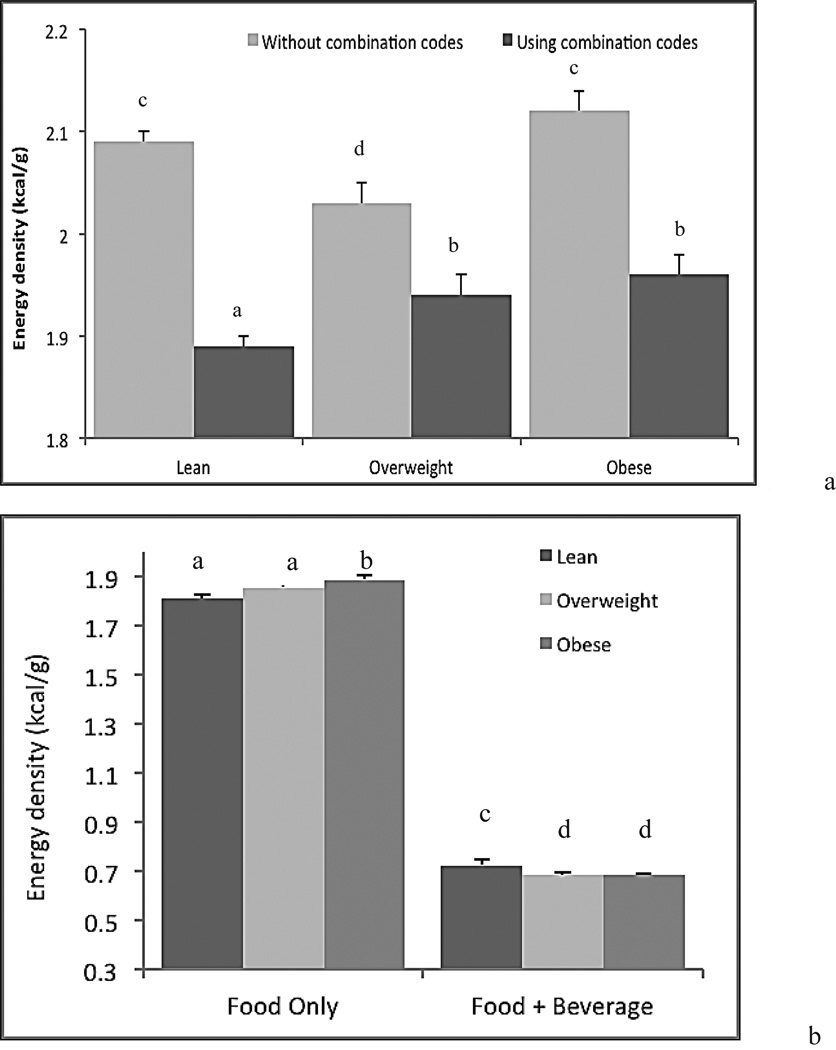
Table 2 demonstrates the substantial effect of beverages on dietary ED. The items in Menu #1 are relatively low in ED, and the foods have a high water content; thus, when a bottle of water is added to the meal, meal ED decreases but not by a substantial amount. The opposite trend occurs in Menu #2; when foods with a low moisture (or high fat) content are consumed, the effects of beverages on the meal ED are notable. Even when a highly caloric beverage (such as soda) is included as part of the meal, the water content of that beverage contributes a great amount of weight for the amount of energy provided, and meal ED is reduced from 2.67 to 1.00. When a non-caloric beverage (diet soda) is added to the meal, the meal ED decreases even further. At a population level, the impact of beverages can be significant. As mentioned previously, most, but not all, studies have found a relationship between dietary ED and weight status in US adults [5–8, 12, 13]. Lack of a standardized method for the calculation of ED may contribute to these mixed findings. Figure 1 represents the influence of both combination codes (1a) and beverages (1b) in the calculation of dietary ED.
Figure 1.
(a) Mean dietary ED by weight status of US adults calculated using the food-only method; (b) Mean dietary ED by weight status of US adults calculated using the food-only and food+beverage method. Adults were classified as lean (BMI ≤24.9 kg/m2), overweight (BMI of 25.0–29.9) or obese (BMI ≥30) using CDC cut points (http://www.cdc.gov/obesity/defining.html). Dietary ED expressed as least-squared means±SE adjusted for age, race, education, family poverty:income ratio, smoking status, and physical activity. Specific survey procedures were used in the analysis to account for sample weights, unequal selection probability, and clustered design. Bars with differing letter superscripts indicate a significant difference at p<0.05.
Figure 1 describes the relationship between dietary ED and weight status. In this figure, adults were classified as lean (BMI ≤24.9 kg/m2), overweight (BMI of 25.0–29.9) or obese (BMI ≥30) using CDC cut points (http://www.cdc.gov/obesity/defining.html). Figure 1a demonstrates the importance of using combination codes in the identification of beverages. Without use of combination codes, mean dietary ED is higher across weight classes. More importantly, when calculating food-only ED without using combination codes, there is no relationship between ED and body weight status. Alternatively, when using combination codes to identify beverages, there is a significant positive association between dietary ED and body weight status; obese individuals eat a diet that is significantly higher in ED than lean individuals. Figure 1a is likely an extension of the example meal given in Table 1 at the population level. Because of the high water content of milk, when milk is added to ready-to-eat cereal, the meal significantly increases in gram weight without a sharp increase in energy. Across an entire population, it is clear that use of the combination codes is essential to accurately calculating food-only ED and assessing the relationship between food-only ED and body weight status. Figure 1b demonstrates the importance of beverages (another high-water content item) at the population level, and also demonstrates the importance of using a food-only ED calculation to evaluate health outcome associations at the population level. Since all beverages have a high water content, the weight of the beverages is substantial compared to the energy that the beverages contain, giving them a lower ED than almost all foods. Even a caloric beverage, such as the soft drink in Table 2, has an ED of 0.34kcal/g, lower than that of most vegetables. The impact of beverages on the overall ED calculation makes it difficult to evaluate the influence of food-ED on health outcomes, particularly at the population level.
The identification of beverages and the selection of a standardized method for ED calculation are critical to consistent analysis of national survey data. The authors of this paper suggest use of USDA food codes, meal codes, and combination codes in order to thoroughly and accurately identify and eliminate beverages for the purposes of a food-only ED calculation. The differing methods for calculation of dietary ED may contribute to the mixed results observed in studies evaluating the relationship between dietary ED and weight status. The present study seeks to inform the selection of a standardized method for ED calculation to be used by investigators on future studies.
Acknowledgements
The authors acknowledge assistance provided by the Population Research Center at The Pennsylvania State University, which is supported by an infrastructure grant by the National Institutes of Health (2R24HD041025-11). The work was funded by the American Institute for Cancer Research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented at NNDC (March 25–28, 2012 – Houston, TX) as Paper #6, Session 2 “Food Composition Databases”
References
- 1.U.S. Department of Agriculture/U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 7th ed. Washington DC: U. S. Government Printing Office; 2010. [Accessed August 7, 2012]. at: http://health.gov/dietaryguidelines/dga2010/DietaryGuidelines2010.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR) In: Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. Research WCRFAICR, editor. Washington, DC: 2007. [Google Scholar]
- 3.Rolls BJ. The relationship between dietary energy density and energy intake. Physiol Behav. 2009;97:609–615. doi: 10.1016/j.physbeh.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rolls BJ, Roe LS, Kral TV, Meengs JS, Wall DE. Increasing the portion size of a packaged snack increases energy intake in men and women. Appetite. 2004;42:63–69. doi: 10.1016/S0195-6663(03)00117-X. [DOI] [PubMed] [Google Scholar]
- 5.Ledikwe JH, Blanck HM, Kettel Khan L, et al. Dietary energy density is associated with energy intake and weight status in US adults. Am J Clin Nutr. 2006;83:1362–1368. doi: 10.1093/ajcn/83.6.1362. [DOI] [PubMed] [Google Scholar]
- 6.Kant AK, Graubard BI. Energy density of diets reported by American adults: association with food group intake, nutrient intake, and body weight. Int J Obes (Lond) 2005;29:950–956. doi: 10.1038/sj.ijo.0802980. [DOI] [PubMed] [Google Scholar]
- 7.Stookey JD. Energy density, energy intake and weight status in a large free-living sample of Chinese adults: exploring the underlying roles of fat, protein, carbohydrate, fiber and water intakes. Eur J Clin Nutr. 2001;55:349–359. doi: 10.1038/sj.ejcn.1601163. [DOI] [PubMed] [Google Scholar]
- 8.Howarth NC, Murphy SP, Wilkens LR, Hankin JH, Kolonel LN. Dietary energy density is associated with overweight status among 5 ethnic groups in the multiethnic cohort study. J Nutr. 2006;136:2243–2248. doi: 10.1093/jn/136.8.2243. [DOI] [PubMed] [Google Scholar]
- 9.U.S. Department of Agriculture ARS, Beltsville Human Nutrition Research Center, Food Surveys Research Group (Beltsville, MD) and U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics (Hyattsville, MD) What We Eat in America, NHANES 2005–2008. Hyattsville, MD: U.S. Department of Agriculture; 2010. [accessed April 1 2011]. Also available from: http://www.ars.usda.gov/Services/docs.htm?docid=18354, [Google Scholar]
- 10.Ledikwe JH, Blanck HM, Khan LK, et al. Dietary energy density determined by eight calculation methods in a nationally representative United States population. J Nutr. 2005;135:273–278. doi: 10.1093/jn/135.2.273. [DOI] [PubMed] [Google Scholar]
- 11.Perez-Escamilla R, Obbagy JE, Altman JM, et al. Dietary energy density and body weight in adults and children: a systematic review. J Acad Nutr Diet. 2012;112:671–684. doi: 10.1016/j.jand.2012.01.020. [DOI] [PubMed] [Google Scholar]
- 12.Vernarelli JA, Mitchell DC, Hartman TJ, Rolls BJ. Dietary energy density is associated with body weight status and vegetable intake in U.S. Children. J Nutr. 2011;141:2204–2210. doi: 10.3945/jn.111.146092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.de Castro JM. Dietary energy density is associated with increased intake in free-living humans. J Nutr. 2004;134:335–341. doi: 10.1093/jn/134.2.335. [DOI] [PubMed] [Google Scholar]