Abstract
The present investigation evaluated the main and interactive effects of distress tolerance and negative affect intensity in relation to posttraumatic stress disorder (PTSD) symptom severity and symptom cluster severity. Participants were 190 trauma-exposed adults (52.6 % women; Mage=25.3 years, SD=11.4) recruited from the community. Distress tolerance (i.e., perceived ability to withstand distressing emotional states) demonstrated significant incremental associations with global PTSD symptom severity as well as Re-Experiencing, Emotional Numbing, and Hyperarousal symptom cluster severity. Negative affect intensity (i.e., perceived intensity of negative emotional responses) demonstrated significant incremental associations with each of the PTSD symptom outcomes. Moreover, the incremental interactive effect of distress tolerance and negative affect intensity was significantly associated with PTSD symptom severity as well as PTSD—Emotional Numbing symptom cluster severity. These incremental effects were evident after accounting for the variance explained by anxiety sensitivity (i.e., fear of anxiety-related sensations). Post hoc probing analyses supported the moderating role of negative affect intensity in the association between distress tolerance and PTSD symptom severity, such that low levels of distress tolerance, in the context of elevated levels of negative affect intensity, were associated with the greatest levels of PTSD symptoms.
Keywords: Distress tolerance, Affect intensity, PTSD, Trauma
Distress tolerance is gaining theoretical and empirical attention as a cognitive-affective factor relevant to the etiology and maintenance of posttraumatic stress disorder (PTSD; Vujanovic, Bernstein and Litz 2011). Distress tolerance is generally conceptualized as the perceived or actual capacity to withstand aversive experiential states (Simons and Gaher 2005), such as negative emotion, uncertainty, and physical discomfort (Zvolensky et al. 2010). Indeed, several empirical studies to date have documented significant inverse relations between distress tolerance and PTSD symptoms (Marshall-Berenz et al. 2010; Vujanovic, Bonn-Miller et al. 2011), such that higher levels of tolerance for negative emotional states were related to lower levels of PTSD symptoms (and vice versa) among trauma-exposed populations, even after controlling for theoretically-relevant factors (e.g., number of potentially traumatic events, neuroticism). Significant difficulty managing distressing trauma-related emotional and physiological experiences is a hallmark feature of PTSD (Keane and Barlow 2002); therefore, one’s ability to tolerate negative emotional states may indeed predispose trauma-exposed individuals to either vulnerability (if distress tolerance is low) or resilience (if distress tolerance is high), thus underscoring the clinical significance of gaining a better understanding of distress tolerance-PTSD relations (Vujanovic, Bernstein and Litz 2011).
Less is known about the interplay of distress tolerance with other cognitive-affective or behavioral factors relevant to PTSD symptoms. To the best of our knowledge, only two studies to-date (Berenz et al. 2012; Marshall-Berenz et al. 2011) have investigated the main and interactive effects of distress tolerance with respect to other theoretically-relevant factors in relation to PTSD symptom severity. First, in a study of trauma-exposed adults, the interactive effect of distress tolerance and a past two-year history of nonclinical panic attacks was found to be significantly, incrementally associated with PTSD symptom severity, specifically PTSD—Hyperarousal symptom severity (Marshall-Berenz et al. 2011). Those with low levels of distress tolerance and a recent history of panic attacks evidenced the highest level of PTSD Hyperarousal symptoms (Marshall-Berenz et al. 2011). Second, also among trauma-exposed adults, the interactive effect of physical, behaviorally indexed distress tolerance (i.e., breath-holding duration; Hajek et al. 1987)—and anxiety sensitivity (i.e., fear of anxiety-related sensations; McNally 2002) was significantly incrementally associated with PTSD symptom severity, specifically PTSD Avoidance symptom severity (Berenz et al. 2012). Those with low physical distress tolerance and high anxiety sensitivity reported the highest levels of PTSD Avoidance symptoms. These findings underscore the importance of examining interactive associations between distress tolerance and other potential risk factors with regard to PTSD symptoms, as such understanding is important to the development of novel prevention/intervention programs for trauma-exposed individuals.
A particularly promising construct of clinical and theoretical relevance to better understanding distress tolerance-PTSD relations is affect intensity. Affect intensity has been conceptualized as a dimension of temperament that reflects individual differences in the activation and intensity of both negative and positive emotional responses (Larsen and Diener 1987). Affect intensity has been described as a vulnerability factor for psychological distress, generally (e.g., Lynch et al. 2001). Emerging work indicates that affect intensity may also be a vulnerability and maintenance factor with relevance to PTSD, specifically (e.g., Tull et al. 2007). For example, as PTSD is characterized by hyper-emotionality, data suggest that the intensity of anxiety and arousal symptoms influences the extent of emotional numbing among individuals with PTSD (Flack et al. 2000; Litz and Keane 1989). Furthermore, in a sample of adults who were victims of childhood interpersonal violence, significant positive associations were documented between negative affect intensity and PTSD symptom severity and severity of re-experiencing, avoidance, and hyperarousal symptom clusters (Tull et al. 2007). Indeed, research has demonstrated that the inhibition of emotion is more likely prominent among those with greater affect intensity levels, and it has been suggested that such individuals may begin to rely more on avoidance techniques to attempt to escape the arousal of particularly intense negative affect (Lynch et al. 2001).
Hence, it appears that both distress tolerance and negative affect intensity hold clinical significance with regard to PTSD symptoms and that their interplay may be particularly meaningful with regard to better understanding the etiology and maintenance processes relevant to PTSD. Theoretically, it can be postulated that the interaction of low levels of distress tolerance and high levels of negative affect intensity may be related to the highest levels of PTSD. That is, trauma-exposed individuals with lower perceived abilities to withstand negative emotional states who are predisposed to high degrees of negative affect intensity may be especially vulnerable to experiencing heightened levels of PTSD following trauma exposure. These individuals may be more apt to employ escape/avoidance strategies to inhibit or avoid intense negative emotional states in the aftermath of trauma (e.g., Lynch et al. 2001; Vujanovic, Bernstein and Litz 2011). Conversely, trauma-exposed individuals with low levels of distress tolerance and low negative affect intensity may not be as likely to use escape/avoidance behaviors following trauma exposure, perhaps due to the lower intensity of their affective experience. These individuals may be somewhat less likely to experience heightened PTSD symptoms following trauma exposure, even despite their low levels of distress tolerance, as affect intensity theoretically may buffer the distress tolerance—PTSD association. No studies to date have examined the interaction of distress tolerance and negative affect intensity with regard to PTSD symptoms, among trauma-exposed adults.
Thus, the current study extends previous work by examining the individual and interactive effects of distress tolerance and negative affect intensity in relation to PTSD symptoms. Past research has demonstrated that trauma-exposed adults with and without PTSD tend to report significant levels of functional impairment, thus underscoring the clinical relevance of further research on trauma-exposed populations with subclinical symptoms (e.g., Norman et al. 2007; Shea et al. 2010). This study focused upon a trauma-exposed sample, recruited from the community, with varying levels of PTSD symptoms. We operationalized distress tolerance using the Distress Tolerance Scale (Simons and Gaher 2005), as extant work has indicated that, among trauma-exposed samples, the self-reported, perceived ability to withstand negative emotional states is more robust than alternative means to measure distress tolerance (Marshall-Berenz et al. 2010). First, it was hypothesized that distress tolerance and negative affect intensity would each demonstrate significant incremental associations with overall PTSD symptom severity and symptom cluster severity; with negative and positive associations expected, respectively. Second, it was hypothesized that the interactive effect of distress tolerance and negative affect intensity would demonstrate significant associations with PTSD symptom severity, above and beyond the independent contributions of distress tolerance and affect intensity. The most robust effects were expected with regard to the following PTSD symptom clusters: Emotional Numbing, Effortful Avoidance, and Hyperarousal symptoms, as based on theoretical (e.g., Flack et al. 2000; Vujanovic, Bernstein and Litz 2011) and empirical (e.g., Berenz et al. 2012; Marshall-Berenz et al. 2011; Tull et al. 2007) work in this domain. Specifically, it was expected that negative affect intensity would moderate—or exacerbate—the association between distress tolerance and PTSD symptom severity such that low distress tolerance in concert with high negative affect intensity would be associated with the greatest severity of PTSD symptoms, both globally and with regard to each PTSD symptom cluster. Low distress tolerance in conjunction with low negative affect intensity was expected to be associated with lower—though still elevated—levels of PTSD global and symptom cluster severity. The lowest levels of PTSD symptoms were expected among individuals with high distress tolerance and low and high negative affect intensity, respectively. These effects were expected even after controlling for the variance contributed by anxiety sensitivity, which has demonstrated significant, positive associations with PTSD (e.g., Fedoroff et al. 2000), negative affect intensity (e.g., Vujanovic et al. 2006), and distress tolerance (e.g., Berenz et al. 2012).
Method
Participants
A total of 190 participants (52.6 % women; Mage=25.3 years, SD=11.4), ranging in age from 18 to 62 years, were recruited via flyer and newspaper advertisements for participation in studies on “emotion.” All participants included in this study endorsed exposure to a DSM-IV-TR Criterion A traumatic life event (American Psychiatric Association [APA], 2000). The ethnic/racial background of participants was generally consistent with that of the Vermont population (State of Vermont Department of Health, 2011): 93.0 % of participants identified as White/Caucasian; 1.6 % identified as Black/African-American; 1.6 % identified as Hispanic/Latino; 1.1 % identified as Asian; 1.1 % identified as biracial; and 1.6 % of participants endorsed the ‘other’ race/ethnicity category.
The current study was based on data yielded from a larger database focused on emotional vulnerability with consistent recruitment and baseline assessment procedures (please see Procedure section). Differences in recruitment hinged upon inclusion and exclusion of Axis I psychopathology as follows: Approximately 34.2 % (n=65) of participants who comprise the present sample were recruited for studies that excluded for current (past month) Axis I disorders; and approximately 65.8 % (n=125) of participants who comprise the present sample were recruited for studies that did not exclude for current (past month) Axis I disorders. This data integration provides a variable range of symptomatology as well as a sufficient sample size to evaluate the broad range of individual differences in PTSD symptom responding. Across studies, inclusionary criteria were comprised of: (a) being an adult over the age of 18; and (b) endorsing exposure to a DSM-IV-TR PTSD Criterion A traumatic life event (APA, 2000). Across studies, exclusionary criteria included: (a) limited mental competency and/or the inability to provide informed, written consent, (b) psychotic-spectrum psychopathology, (c) current suicidal ideation, (d) current or past serious medical illness (e.g., chronic cardiopulmonary illness, current respiratory illness. seizure disorder, cardiac dysfunction), and (e) pregnancy.
Measures
Structured Clinical Interview for DSM-IV—Non-Patient Version
(SCID-I/N-P; First et al. 1995). The SCID-I/N-P was used to index current (past month) Axis I diagnoses and assess exclusionary criteria (please see above). The DSM-IV version of the SCID-I has been shown to have good to excellent reliability (Zanarini et al. 2000) and validity (Basco et al. 2000). In the present study, all SCID-I/N-P administrations were conducted by trained clinical assessors. A random sampling of 20 % of the SCID-I/NP administrations was reviewed by the PIs to ensure inter-rater agreement, and no cases of diagnostic disagreement were noted.
Posttraumatic Diagnostic Scale (PDS; Foa 1995)
The PDS is a 49-item self-report instrument designed to assess the presence of DSM-IV-TR PTSD symptoms (APA, 1994; 2000). Respondents report if they have experienced any of 12 traumatic events, including an “other” category, and then indicate which event was most disturbing. The PDS assesses Criterion A trauma exposure as well as the frequency (0=“not at all” or “only one time” to 3=“five or more times a week/almost always”) of 17 past-month PTSD symptoms for the most disturbing event endorsed. The items are summed to assess PTSD symptom severity (range from 0 to 51) and symptom cluster severity. In the current study, the four-factor model of PTSD (King et al. 1998) was utilized to derive four symptom clusters: Re-Experiencing, Effortful Avoidance, Emotional Numbing, and Hyperarousal. The PDS has evidenced generally excellent psychometric properties (Foa et al. 1997; Foa et al. 1993). In the present sample, the PDS demonstrated high internal consistency (α=.94).
Distress Tolerance Scale (DTS; Simons and Gaher 2005)
The DTS is a 15-item self-report measure on which respondents indicate, on a 5-point Likert-type scale (1=“strongly agree” to 5=“strongly disagree”), the extent to which they believe they can experience and withstand distressing emotional states (Simons and Gaher 2005). The DTS encompasses four sub-scales, including: perceived ability to tolerate emotional distress (e.g., “I can’t handle feeling distressed or upset”), subjective appraisal of distress (e.g., “My feelings of distress or being upset are not acceptable”), attention absorption by negative emotions (e.g., “When I feel distressed or upset, I cannot help but concentrate on how bad the distress actually feels”), and regulation efforts to alleviate distress (e.g., “I’ll do anything to avoid feeling distressed or upset;” Simons and Gaher 2005). The DTS has excellent psychometric properties (Simons and Gaher 2005). As in past work, the DTS total score was employed as a global index of perceived distress tolerance (Leyro et al. 2010). High levels of perceived distress tolerance are indicated by higher total scores on the DTS (Simons and Gaher 2005). In the present sample, the DTS demonstrated high internal consistency (α=.89).
Affect Intensity Measure (AIM; Larsen and Diener 1987)
The AIM is a 40-item self- report questionnaire, based on a 6-point Likert-type scale (0=“never” to 6=“always”), which assesses the characteristic magnitude with which an individual experiences emotions (e.g., “When I do feel anxiety, it is normally very strong;” “When I am happy, I bubble over with energy”). Affect intensity is a stable dimension of personality that pertains to all emotions, regardless of hedonic tone (Larsen and Diener 1987). The AIM has excellent psychometric properties (Larsen and Diener 1987). In the present investigation, the AIM—Negative Item total score was used, as it was the most theoretically relevant to the study objectives. This approach in scoring the AIM has been employed in relevant past work (e.g., Flett et al. 1986; Tull et al. 2007). In the present sample, the AIM- Negative Item subscale demonstrated high internal consistency (α=.86).
Anxiety Sensitivity Index (ASI; Reiss et al. 1986)
The ASI is a 16-item questionnaire on which respondents indicate, on a 5-point Likert-type scale (0=“very little” to 4=“very much”), the degree to which they fear the negative consequences of anxiety symptoms (Reiss et al. 1986). Specifically, anxiety sensitivity reflects relatively stable individual differences in the fear of anxiety and anxiety-related sensations (McNally 2002). The ASI is the most widely used and tested measure of anxiety sensitivity and has demonstrated good psychometric properties, including internal consistency (Peterson and Reiss 1992). The current study utilized the total ASI score, which evidenced good internal consistency (α=.84).
Procedure
The integrated database was comprised of individuals who responded to advertisements about studies on emotion. Interested individuals were scheduled for a session in the laboratory to determine eligibility and collect study data. Upon arrival to the laboratory, all participants first provided verbal and written informed consent. The SCID-I/N-P was then administered to determine eligibility based on the criteria identified above. Across studies, eligible participants completed a battery of self-report measures and received $25 compensation for their time and involvement. Data collection was approved by the Institutional Review Board.
Data Analytic Plan
Analyses were conducted in PASW Statistics 18.0. First, descriptive characteristics of participants were evaluated with regard to trauma exposure and current Axis I psychopathology. Second, zero-order correlations among variables were examined. Third, a series of five hierarchical regression analyses was performed.1 Criterion variables included: (1) PTSD symptom severity (PDS—total score), (2) PTSD—Re-Experiencing symptom severity (PDS—Re-Experiencing symptom cluster score), (3) PTSD—Effortful Avoidance symptom severity (PDS—Effortful Avoidance symptom cluster score), (4) PTSD—Emotional Numbing symptom severity (PDS—Emotional Numbing symptom cluster score), and (5) PTSD—Hyperarousal symptom severity (PDS—Hyperarousal symptom cluster score). At step one of each of the models, anxiety sensitivity (ASI—total score) was entered as a covariate. At step two of each of the models, distress tolerance (DTS—total score; mean-centered) and negative affect intensity (AIM—Negative Item total score; mean-centered) were entered. At step three of each of the models, the distress tolerance by negative affect intensity interaction terms (DTS—total score × AIM—Negative Item total score) were entered. All tests were two-tailed with an alpha level set at 0.05.
The forms of any significant interactions were subsequently examined both graphically (Cohen and Cohen 1983) and statistically (Holmbeck 2002). First, we examined the forms of these interactions by inserting specific values for each predictor variable (0.5 SD above and below the mean) into the regression equation associated with the described analysis (Cohen and Cohen 1983; pp. 323, 419). Second, we conducted post hoc probing analyses to examine the significance of the simple slopes and interactions to test for moderation (Holmbeck 2002).
Results
Participant Characteristics
Participants for the current study were selected on the basis of lifetime exposure to a DSM-IV-TR PTSD Criterion A traumatic event (APA, 2000), as assessed by the PDS (Foa 1995). On average, participants reported experiencing 2.4 different types of traumatic life events. The types of traumatic events reported, as per responses on the PDS (Foa 1995), included: serious accident, fire, or explosion (47.4 %), sexual contact when younger than 18 years with someone five or more years older (27.4 %), non-sexual assault by a stranger (25.8 %), natural disaster (24.7 %), non-sexual assault by a family member or someone known (24.2 %), sexual assault by a family member or someone known (18.4 %), life-threatening illness (13.7 %), imprisonment (12.1 %), sexual assault by a stranger (10.0 %), torture (2.6 %), military combat or a war zone (2.1 %), and “other” trauma type (e.g., sudden unexpected death of a friend or family member; 33.2 %).
The SCID-I/N-P (First et al. 1995) was administered to index current Axis I psychopathology (i.e., past month for all disorders; substance use disorders not assessed) and assess exclusionary criteria (please see Procedure section). Of the total sample, approximately 12.6 % of participants (n=24) met diagnostic criteria for a current Axis I disorder. More specifically, 11 participants met criteria for major depressive disorder; 10 for generalized anxiety disorder; 6 for specific phobia; 4 for panic disorder; 4 for social phobia; 3 for PTSD; 2 for bipolar-spectrum disorders; and 1 for agoraphobia.
Zero-Order Correlations
Please see Table 1 for descriptive statistics and zero-order correlations. The ASI—total score was significantly positively correlated with each of the criterion variables (r’s =.20 – .39, p’s < .01). The DTS—total score was significantly negatively correlated with each of the criterion variables (r’s=–.26 to–.46, p’s<.01). The AIM—Negative Item total score was significantly positively correlated with each of the criterion variables (r’s=.31 to .48, p’s<.01). Finally, the DTS—total score and the AIM—Negative Item total score were significantly negatively correlated (r=–.53, p<.01); and the ASI—total score was significantly negatively related to both DTS—total score (r=–.49, p<.01) and AIM—Negative Item total score (r=–.43, p<.01).
Table 1.
Descriptive Data and Zero-Order Correlations among Theoretically-Relevant Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | M(SD) | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. | ASI—Total Score | 1 | –0.49** | 0.43** | 0.39** | 0.37** | 0.20** | 0.36** | 0.37** | 16.78 (8.50) |
| 2. | DTS—Total Score | – | 1 | –0.54** | –0.45** | –0.41** | –0.26** | –0.38** | –0.46** | 3.50 (0.78) |
| 3. | AIM—Negative Item total score | – | – | 1 | 0.48** | 0.48** | 0.32** | 0.36** | 0.49** | 39.51 (9.57) |
| 4. | PDS—Total Score | – | – | – | 1 | 0.88** | 0.77** | 0.90** | 0.91** | 8.30 (9.88) |
| 5. | PDS—Re-Experiencing | – | – | – | – | 1 | 0.69** | 0.69** | 0.71** | 2.24 (2.92) |
| 6. | PDS—Avoidance | – | – | – | – | – | 1 | 0.60** | 0.56** | 1.23 (1.74) |
| 7. | PDS—Numbing | – | – | – | – | – | – | 1 | 0.79** | 2.14 (3.07) |
| 8. | PDS—Hyperarousal | – | – | – | – | – | – | – | 1 | 2.70 (3.52) |
The PDS-Total Score is a sum score of all 17 PTSD symptoms measured by the PDS. Subscales of the PDS are represented as means of the items that comprise each subscale
p<.01
Regression Analyses
Please refer to Table 2 for a summary of regression analyses
PTSD Total Symptom Severity
The proposed model accounted for 31.6 % of variance, F(4, 185)=21.36, p<.001. Step one of the model (i.e., ASI—total score) accounted for 14.9 % of variance (p<.001), with higher ASI scores related to greater PTSD symptom severity. Step two of the model accounted for an additional 15.2 % of unique variance (p<.001), with lower DTS—total scores and greater AIM—Negative Item total scores each significantly related to greater PTSD symptom severity at that step. Step three of the model accounted for an additional 1.5 % of unique variance (p=.044), with evidence for a significant interactive effect for DTS—total score × AIM—Negative item total score.
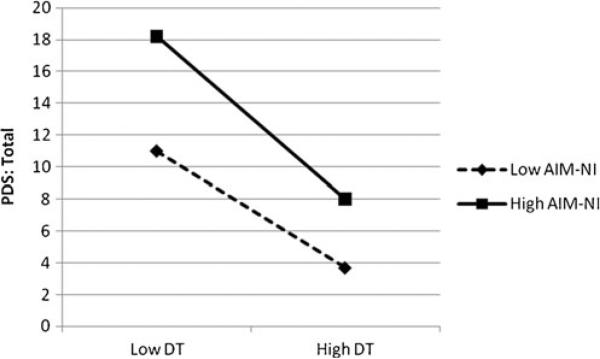
Please see Fig. 1 for a graphical representation of the distress tolerance by negative affect intensity interactive effect in relation to PTSD symptom severity. Post hoc probing analyses of the simple slopes and interactions supported the significant moderating role of negative affect intensity in the association between distress tolerance and PTSD symptom severity. Specifically, distress tolerance was significantly related to PTSD symptom severity among those high in negative affect intensity (t=–2.87, β=–.42, p=.005), with lower levels of distress tolerance being related to greater PTSD symptom severity. However, the relationship between distress tolerance and PTSD symptom severity was not statistically significant when negative affect intensity was low (t=–1.39, β=–.19, p=.165).
Fig. 1.
Interactive effects of distress tolerance (DT) and negative affect intensity (AIM-NI) in predicting PTSD symptom severity (PDS: Total)
PTSD—Re-Experiencing
The proposed model accounted for 28.8 % of variance, F(4, 185)=18.67, p<.001. Step one of the model (i.e., ASI—total score) accounted for 13.4 % of variance (p<.001), with higher ASI scores related to greater Re-Experiencing symptom severity. Step two of the model accounted for an additional 14.2 % of unique variance (p<.001), with the DTS—total score and the AIM—Negative Item total score demonstrating significant incremental relations with the PDS—Re-Experiencing symptom cluster in the expected directions. Step three of the model was not significant (p=.081).
PTSD—Effortful Avoidance
The proposed model accounted for 11.4 % of variance, F(4, 185)=5.97, p<.001. Step one of the model (i.e., ASI—total score) accounted for a significant 3.9 % of variance (p=.006), with greater ASI scores associated with greater Effortful Avoidance symptom severity. Step two of the model accounted for an additional 7.5 % of unique variance (p=.001), with only the AIM—Negative Item total score demonstrating significant incremental relations with the PDS—Effortful Avoidance symptom cluster. Step three of the model was not significant (p=.806).
PTSD—Emotional Numbing
The proposed model accounted for 22.8 % of variance, F(4, 185)=13.63, p<.001. Step one of the model (i.e., ASI—total score) accounted for 13.0 % of variance (p<.001), with greater ASI scores associated with greater Emotional Numbing symptom severity. Step two of the model accounted for an additional 7.5 % of unique variance (p<.001), with the DTS—total score and the AIM—Negative Item total score accounting for significant variance in the expected directions. The interaction of DTS—total score and AIM—Negative item total score at step three of the model accounted for an additional 2.3 % of unique variance (p=.021).
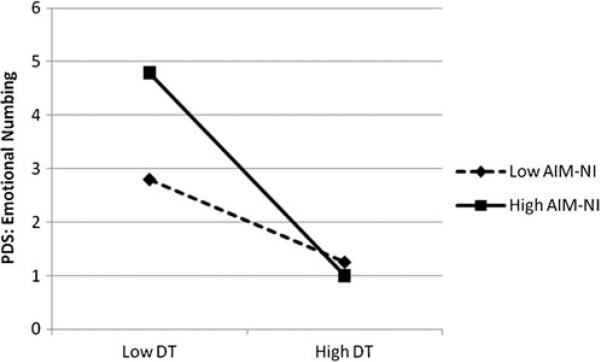
Please see Fig. 2 for a graphical representation of the distress tolerance by negative affect intensity interaction effect in relation to PTSD—Emotional Numbing symptom severity. Post hoc probing analyses of the simple slopes and interactions supported the significant moderating role of negative affect intensity in the association between distress tolerance and PTSD—Emotional Numbing Symptoms. Specifically, distress tolerance was significantly related to PTSD—Emotional Numbing symptoms among those high in negative affect intensity (t=–2.92, β=–.46, p=.004), such that symptom severity was greater among those lower in distress tolerance. However, the relation between distress tolerance and PTSD—Emotional Numbing symptoms was not statistically significant when negative affect intensity was low (t=–.20, β=–.03, p=.843).
Fig. 2.
Interactive effects of distress tolerance (DT) and negative affect intensity (AIM-NI) in predicting PTSD Emotional Numbing symptoms (PDS: Emotional Numbing)
PTSD—Hyperarousal
The proposed model accounted for 31.8 % of variance, F(4, 185)=21.65, p<.001. Step one of the model (i.e., ASI—total score) accounted for a significant 13.5 % of variance (p<.001), with greater ASI scores being related to greater PTSD—Hyperarousal symptoms. Step two of the model accounted for an additional 17 % of unique variance (p<.001), with DTS—total score and AIM—Negative Item total score emerging as significant incremental predictors in the expected directions. The interaction at step three of the model was not statistically significant (p=.057).
Discussion
The present investigation examined the main and interactive effects of distress tolerance and negative affect intensity with regard to PTSD symptom severity and symptom cluster severity within a sample of trauma-exposed adults from the general community. As predicted, the main effect of distress tolerance was significantly and inversely related to total PTSD symptom severity, as well as Re-Experiencing and Emotional Numbing symptom severity. Specifically, lower levels of distress tolerance were related to higher levels of PTSD symptoms (and vice versa). Notably, although distress tolerance and PTSD—Effortful Avoidance symptom severity were significantly related at the zero-order level, that association was not significant after accounting for variance explained by anxiety sensitivity. This finding is consistent with past work using the DTS (Marshall-Berenz et al. 2011; Vujanovic, Bonn-Miller et al. 2011) but inconsistent with studies employing behavioral indices of distress tolerance which documented a significant incremental association between distress tolerance, as indexed by breath-holding duration, and PTSD—Effortful Avoidance symptom severity (Berenz et al. 2012). The present findings may be an artifact of measurement or may reflect the possibility that perceived abilities to withstand distress do not incrementally relate to avoidance among trauma-exposed, nonclinical samples; further multi-method and longitudinal investigation is needed.
Also consistent with hypotheses and past work (Tull et al. 2007), negative affect intensity demonstrated incremental, positive associations with each of the PTSD outcomes. Thus, higher levels of negative affect intensity were associated with higher levels of PTSD symptoms, even after controlling for the effects of anxiety sensitivity, a well-established risk and maintenance factor for PTSD (Olatunji and Wolitzky-Taylor 2009). Trauma-exposed individuals who tend to experience negative affective states intensely also tend to report higher levels of PTSD symptoms. Notably, the present data do not indicate whether distress tolerance and negative affect intensity convey risk for the onset or maintenance of PTSD symptoms following trauma exposure, or whether the experience of more significant PTSD symptoms influences individuals’ experience of negative emotions; these pathways are not necessarily mutually exclusive (Vujanovic, Bonn-Miller et al. 2011).
The interactive effect of distress tolerance and negative affect intensity was significantly associated with total PTSD symptom severity and PTSD—Emotional Numbing symptom severity, contributing small but statistically significant 1.5 % and 2.3 % of variance to the respective models above and beyond the large main effect terms. Post hoc probing analyses of the simple slopes and interactions supported a moderating role of negative affect intensity in the association between distress tolerance and PTSD symptom severity as well as PTSD—Emotional Numbing severity (Please see Figs. 1 and 2). That is, the association between distress tolerance and PTSD symptom severity and PTSD—Emotional Numbing severity was significant only among those with high negative affect intensity, with individuals high in negative affect intensity and low in distress tolerance reporting the greatest levels of symptoms. Notably, no interactive effect was observed with respect to Re-Experiencing, Avoidance, or Hyperarousal symptoms, as consistent with some past work in this domain (Marshall-Berenz et al. 2011), but partially inconsistent with hypotheses. The lack of effects with respect to these symptom clusters may be, in part, a result of the nonclinical composition of the sample. Alternatively, these results may be due to the utilization of a self-report index of distress tolerance, measuring individuals’ perceptions of their ability to withstand negative emotional states, and work employing behavioral indices of the construct may find different effects. Indeed, past work with trauma-exposed, community samples also failed to document incremental associations between distress tolerance and the Re-Experiencing cluster (e.g., Vujanovic, Bonn-Miller et al. 2011). It is important for future work to extend this line of inquiry with clinical samples.
Trauma-exposed individuals with low levels of perceived tolerance to withstand negative emotional states may be especially likely to experience PTSD symptoms, especially when also manifesting the trait-like tendency to experience negative affect intensely, particularly symptoms of Emotional Numbing. This finding is consistent with hyper-emotionality theories of PTSD and past work suggesting that the intensity of anxiety and arousal symptoms influences the extent of emotional numbing among individuals with PTSD (Flack et al. 2000; Litz and Keane 1989). Understanding the nature and direction of the observed relations using experimental and longitudinal designs can inform the future development of secondary prevention and early intervention treatments. These findings suggest that targeting distress tolerance and/or negative affect intensity in the context of treatment for PTSD symptoms may be indicated, pending replication and extension of this work with clinical samples and experimental designs.
There are several limitations worthy of note in the present study. First, the sample was comprised of relatively young, Caucasian, trauma-exposed individuals, only 12.6 % of whom met criteria for current Axis I psychopathology. Future studies would benefit from including older, more diverse, clinical samples with PTSD and co-occurring disorders. Second, the overall sample endorsed low mean levels of PTSD symptoms on the PDS (M=8.30, SD=9.88), limiting our ability to readily extrapolate from the present findings to PTSD in clinical samples. Third, this study relied exclusively on self-report, which may be subject to report biases. It is important to extend this work, using behavioral indices of distress tolerance and negative affect intensity as well as interview-based assessments of the frequency and intensity of PTSD symptoms. Fourth, given the cross-sectional study design, the direction of the observed associations is not known. As noted previously, it is important to extend this line of work using controlled experimental, longitudinal/prospective, and intervention-based designs to examine potential causal links among these variables.
Overall, both distress tolerance and negative affect intensity are candidate risk factors worthy of further study with respect to PTSD onset, maintenance, and recovery. This study provides a conceptual model for better understanding the individual, additive, and synergistic relations of these variables with regard to PTSD. Future work, using more rigorous methodologies, is needed to more conclusively establish the clinical and theoretical significance of these constructs for PTSD.
Table 2.
Main and Interactive Effects of Distress Tolerance and Negative Affect Intensity in Relation to PTSD Symptoms
| Δ R2 | t | β | sr2 | p | |
|---|---|---|---|---|---|
| Criterion Variable: PDS—Total Score | |||||
| Step 1 | 0.149 | <.001 | |||
| ASI | 5.74 | 0.39 | 0.15 | <.001 | |
| Step 2 | .152 | <.001 | |||
| DTS | –2.73 | –0.21 | 0.04 | .007 | |
| AIM | 4.06 | 0.30 | 0.08 | <.001 | |
| Step 3 | 0.015 | 0.044 | |||
| DTS × AIM | –2.03 | –0.48 | 0.02 | 0.044 | |
| Criterion Variable: PDS—Re-Experiencing | |||||
| Step 1 | 0.134 | <.001 | |||
| ASI | 5.39 | 0.37 | 0.13 | <.001 | |
| Step 2 | 0.142 | <.001 | |||
| DTS | –2.00 | –0.16 | 0.02 | .047 | |
| AIM | 4.33 | 0.33 | 0.09 | <.001 | |
| Step 3 | 0.012 | .081 | |||
| DTS × AIM | –1.75 | –0.43 | 0.02 | .081 | |
| Criterion Variable: PDS—Effortful Avoidance | |||||
| Step 1 | 0.039 | .006 | |||
| ASI | 2.78 | 0.20 | 0.04 | .006 | |
| Step 2 | 0.075 | .001 | |||
| DTS | –1.27 | –0.11 | 0.01 | .204 | |
| AIM | 2.86 | 0.24 | 0.04 | .005 | |
| Step 3 | 0.000 | .806 | |||
| DTS × AIM | –0.25 | –0.07 | 0.00 | .806 | |
| Criterion Variable: PDS—Emotional Numbing | |||||
| Step 1 | 0.130 | <.001 | |||
| ASI | 5.30 | 0.36 | 0.13 | <.001 | |
| Step 2 | 0.075 | <.001 | |||
| DTS | –2.33 | –0.19 | 0.03 | .021 | |
| AIM | 2.18 | 0.17 | 0.02 | .031 | |
| Step 3 | 0.023 | .021 | |||
| DTS × AIM | –2.33 | –0.59 | 0.03 | .021 | |
| Criterion Variable: PDS—Hyperarousal | |||||
| Step 1 | 0.135 | <.001 | |||
| ASI | 5.42 | 0.37 | 0.13 | <.001 | |
| Step 2 | 0.170 | <.001 | |||
| DTS | –3.10 | –0.24 | 0.05 | .002 | |
| AIM | 4.14 | 0.31 | 0.08 | <.001 | |
| Step 3 | 0.013 | .057 | |||
| DTS × AIM | –1.91 | –0.45 | 0.02 | .057 | |
PDS Posttraumatic Diagnostic Scale; ASI Anxiety Sensitivity Index (total score); DTS Distress Tolerance Scale (total score); AIM Affect Intensity Measure (Negative Item total score)
Acknowledgements
This work was supported, in part, by grants awarded to Anka A. Vujanovic (1F31 DA021006-02), Erin C. Berenz (1F31 MH080453-01A1), and Amit Bernstein (1 F31MH73205-2). Amit Bernstein also recognizes the funding support from the Israeli Council for Higher Education Yigal Alon Fellowship, the European Union FP-7 Marie Curie Fellowship International Reintegration Grant, Psychology Beyond Borders Mission Award, Israel Science Foundation, the University of Haifa Research Authority Exploratory Grant, and the Rothschild-Caesarea Foundation’s Returning Scientists Project at the University of Haifa. The views expressed here are those of the authors and do not necessarily represent those of the Department of Veterans Affairs.
Footnotes
The pattern of results did not change when gender was included as a covariate in regression analyses.
Contributor Information
Anka A. Vujanovic, Department of Psychiatry and Behavioral Sciences, University of Texas Health Science Center at Houston, 2800 South MacGregor Way, Houston, TX 77021, USA
Ashley S. Hart, Rhode Island Hospital and The Warren Alpert Medical School of Brown University, Providence, RI, USA
Carrie M. Potter, Temple University, Philadelphia, PA, USA
Erin C. Berenz, Virginia Institute for Psychiatric and Behavioral Genetics, Virginia Commonwealth University, Richmond, VA, USA
Barbara Niles, National Center for PTSD, VA Boston Healthcare System and Boston University School of Medicine, Boston, MA, USA.
Amit Bernstein, University of Haifa, Haifa, Israel.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 1994. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 2000. text rev. [Google Scholar]
- Basco MR, Bostic JQ, Davies D, Rush J, Witte B, Hendrickse W, Barnett V. Methods to improve diagnostic accuracy in a community mental health setting. The American Journal of Psychiatry. 2000;157:1599–1605. doi: 10.1176/appi.ajp.157.10.1599. doi:10.1176/appi.ajp.157.10.1599. [DOI] [PubMed] [Google Scholar]
- Berenz EC, Vujanovic AA, Coffey SF, Zvolensky MJ. Anxiety sensitivity and breath-holding duration in relation to PTSD symptom severity among trauma exposed adults. Journal of Anxiety Disorders. 2012;26:134–139. doi: 10.1016/j.janxdis.2011.10.004. doi:10.1016/j.janxdis.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. 2nd ed. Erlbaum; Hillsdale, NJ: 1983. [Google Scholar]
- Fedoroff IC, Taylor S, Asmundson GJG, Koch WJ. Cognitive factors in traumatic stress reactions: predicting PTSD symptoms from anxiety sensitivity and beliefs about harmful events. Behavioural and Cognitive Psychotherapy. 2000;28:5–15. [Google Scholar]
- First M, Spitzer R, Williams J, Gibbon M. Structured clinical interview for DSM-IV-Non-patient edition (SCID-NP, version 1.0) American Psychiatric Press; Washington, DC: 1995. [Google Scholar]
- Flack WF, Litz BT, Hsieh FY, Kaloupek DG, Keane TM. Predictors of emotional numbing, revisited: a replication and extension. Journal of Traumatic Stress. 2000;13:611–618. doi: 10.1023/A:1007806132319. doi:10.1023/A:1007806132319. [DOI] [PubMed] [Google Scholar]
- Flett GL, Boase P, McAndrews MP, Pliner P, Blankstein KR. Affect intensity and the appraisal of emotion. Journal of Research in Personality. 1986;20:447–459. doi:10.1016/0092-6566(86)90125-X. [Google Scholar]
- Foa EB. Posttraumatic stress diagnostic scale manual. National Computer Systems; Minneapolis: 1995. [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress. 1993;6:459–473. doi:10.1002/jts.2490060405. [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: the posttraumatic diagnostic scale. Psychological Assessment. 1997;9:445–451. doi:10.1037//1040-3590.9.4.445. [Google Scholar]
- Hajek P, Belcher M, Stapleton J. Breath-holding endurance as a predictor of success in smoking cessation. Addictive Behaviors. 1987;12:285–288. doi: 10.1016/0306-4603(87)90041-4. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. doi:10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Keane TM, Barlow DH. Posttraumatic stress disorder. In: Barlow DH, editor. Anxiety and its disorders. 2nd ed. Guilford; New York: 2002. pp. 418–453. [Google Scholar]
- King DW, Leskin GA, King LA, Weathers FW. Confirmatory factor analysis of the clinician-administered PTSD scale: evidence for dimensionality of posttraumatic stress disorder. Psychological Assessment. 1998;10:90–96. doi:10.1037//1040-3590.10.2.90. [Google Scholar]
- Larsen RJ, Diener E. Affect intensity as an individual difference characteristic: a review. Journal of Research in Personality. 1987;21:1–39. [Google Scholar]
- Leyro TM, Zvolensky MJ, Bernstein A. Distress tolerance and psychopathological symptoms and disorders: a review of the empirical literature among adults. Psychological Bulletin. 2010;136:576–600. doi: 10.1037/a0019712. doi:10.1177/0963721410388642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litz BT, Keane TM. Information processing in anxiety disorders: application to the understanding of post-traumatic stress disorder. Clinical Psychology Review. 1989;9:243–257. doi:10.1016/0272-7358(89)90030-5. [Google Scholar]
- Lynch TR, Robins CJ, Morse JQ, Krause ED. A mediational model relating affect intensity, emotion inhibition, and psychological distress. Behavior Therapy. 2001;32:519–536. doi:10.1016/S0005-7894(01)80034-4. [Google Scholar]
- Marshall-Berenz EC, Vujanovic AA, Bonn-Miller MO, Bernstein A, Zvolensky MJ. Multimethod study of distress tolerance and PTSD symptom severity in a trauma-exposed community sample. Journal of Traumatic Stress. 2010;23:623–630. doi: 10.1002/jts.20568. doi:10.1002/jts.20568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall-Berenz EC, Vujanovic AA, Zvolensky MJ. Main and interactive effects of a nonclinical panic attack history and distress tolerance in relation to PTSD symptom severity. Journal of Anxiety Disorders. 2011;25:185–191. doi: 10.1016/j.janxdis.2010.09.001. doi:10.1016/j.janxdis.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally RJ. Anxiety sensitivity and panic disorder. Biological Psychiatry. 2002;52:938–946. doi: 10.1016/s0006-3223(02)01475-0. doi:10.1016/S0006-3223 (02)01475-0. [DOI] [PubMed] [Google Scholar]
- Norman SB, Stein MB, Davidson JR. Profiling posttraumatic functional impairment. The Journal of Nervous and Mental Disease. 2007;195:48–53. doi: 10.1097/01.nmd.0000252135.25114.02. doi:10.1097/01.nmd.0000252135.25114.02. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Wolitzky-Taylor KB. Anxiety sensitivity and the anxiety disorders: a meta-analytic review and synthesis. Psychological Bulletin. 2009;135:974–999. doi: 10.1037/a0017428. [DOI] [PubMed] [Google Scholar]
- Peterson RA, Reiss S. The anxiety sensitivity index manual. 2nd ed. International Diagnostic Systems; Worthington: 1992. [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the predictions of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. doi:10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Shea MT, Vujanovic AA, Mansfield AK, Sevin E, Liu F. Functional impairment among OEF/OIF veterans: associations with PTSD symptoms. Journal of Traumatic Stress. 2010;23:100–107. doi: 10.1002/jts.20497. doi:10.1002/jts.20497. [DOI] [PubMed] [Google Scholar]
- Simons JS, Gaher RM. The distress tolerance scale: development and validation of a self-report measure. Motivation and Emotion. 2005;29:83–102. doi:10.1007/s11031-005-7955-3. [Google Scholar]
- State of Vermont, Department of Health [November 3, 2011]; from http://www.healthyvermonters.info/
- Tull MT, Jakupcak M, McFadden ME, Roemer L. The role of negative affect intensity and the fear of emotions in posttraumatic stress symptom severity among victims of childhood interpersonal violence. The Journal of Nervous and Mental Disease. 2007;195:580–587. doi: 10.1097/NMD.0b013e318093ed5f. doi:10.1097/NMD.0b013e318093ed5f. [DOI] [PubMed] [Google Scholar]
- Vujanovic AA, Zvolensky MJ, Gibson LE, Lynch TR, Leen-Feldner EW, Feldner MT, Bernstein A. Affect intensity: association with anxious and fearful responding to bodily sensations. Journal of Anxiety Disorders. 2006;20:192–206. doi: 10.1016/j.janxdis.2004.12.002. doi:10.1016/j.janxdis.2004.12.002. [DOI] [PubMed] [Google Scholar]
- Vujanovic AA, Bernstein A, Litz BT. Traumatic stress. In: Zvolensky MJ, Bernstein A, Vujanovic AA, editors. Distress tolerance: theory, research, and clinical applications. Guilford; New York: 2011. pp. 126–148. [Google Scholar]
- Vujanovic AA, Bonn-Miller MO, Potter CM, Marshall EC, Zvolensky MJ. An evaluation of the relation between distress tolerance and posttraumatic stress within a trauma-exposed sample. Psychopathology and Behavioral Assessment. 2011;33:129–135. doi: 10.1007/s10862-010-9209-2. doi:10.1007/s10862-010-9209-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, Gunderson JG. The collaborative longitudinal personality disorders study: reliability of axis I and II diagnoses. Journal of Personality Disorders. 2000;14:291–299. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Vujanovic AA, Bernstein A, Leyro T. Distress tolerance: theory, measurement, and relations to psycho-pathology. Current Directions in Psychological Science. 2010;19:406–410. doi: 10.1177/0963721410388642. doi:10.1177/0963721410388642. [DOI] [PMC free article] [PubMed] [Google Scholar]