Abstract
Objective
To study the impact of Training of Traditional Birth Attendants (TBAs) on maternal health care in a rural area.
Methods
An interventional study in the Primary Health Center area was conducted over 1-year period between March 2006 and February 2007, which included all the 50 Traditional Birth Attendants (30 previously trained and 20 untrained), as study participants. Pretest evaluation regarding knowledge, attitude, and practices about maternal care was done. Post-test evaluation was done at the first month (early) and at the fifth month (late) after the training. Analysis was done by using Mc. Nemer’s test, Chi-square test with Yates’s correction and Fischer’s exact test.
Results
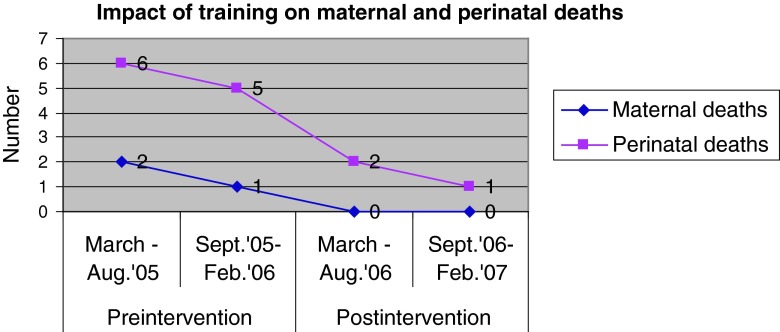
Early and late post-test evaluation showed that there was a progressive improvement in the maternal health care provided by both the groups. Significant reduction in the maternal and perinatal deaths among the deliveries conducted by TBAs after the training was noted.
Conclusion
Training programme for TBAs with regular follow-ups in the resource-poor setting will not only improve the quality of maternal care but also reduce perinatal deaths.
Keywords: Traditional birth attendants, Maternal health care, Maternal mortality, Training
Introduction
Women are crucial to social and economic development. Their health and well being matters not only to themselves, but also to their families and to the community. They are facing constraints not only in obtaining health services but also in expressing health needs. Though various programmes have been launched to provide primary health care to women and children, the impact of these programmes has not been significant particularly in rural areas [1].
Globally, 61 % of births are assisted by skilled birth attendants, while in some low income countries the average is as low as 34 % [2]. The current level of home deliveries in India is 59 %. Out of these 53 % are conducted by Traditional Birth Attendants [3]. Although there is a provision of Trained Birth Attendant in every village in the national programme since 1977, most of the deliveries in rural areas are still conducted at home by untrained TBAs [4]. Lack of awareness about utilization of health services, inappropriate transport facilities, health ignorance, poverty and traditional beliefs are the factors which make the rural pregnant women go to untrained TBAs who are easily available. Training programme regarding maternal and child health (MCH) care has resulted in better knowledge, attitude, and practices amongst TBAs in Nigeria [5].
According to the Primary Health Centre statistics, 58.7 % of deliveries occur at home. Out of these 63.3 % of deliveries are conducted by untrained TBAs. The present study was an attempt to assess the impact of training programme on the knowledge, attitude, and practice regarding maternal health care among TBAs in a rural area.
Objective
To study the impact of Training of Traditional Birth Attendants (TBAs) on maternal health care in a rural area.
Materials and Methods
This is an interventional study undertaken in the Primary Health Centre (PHC) area of Vantamuri, Belgaum Dist., Karnataka, India between March 2006 and February 2007. All the existing TBAs (n = 50) in the area were contacted and pretest evaluation of their knowledge, attitude, and practices regarding MCH care was done by using a predesigned and pretested questionnaire. Forty-five TBAs attended 2 days intensive training programme held at the PHC on the third and fourth March, 2006. Training sessions included topics on antenatal care, safe delivery practices, postnatal care and family planning practices. It was conducted by a team of Obstetricians, Public health specialists and trainers from perinatal health centre, JN Medical College, Belgaum. Different teaching techniques like lectures, demonstrations and interactive sessions were used with the help of audiovisual aids like LCD, flip charts, video clippings and models. Evaluation regarding gain in knowledge and change in attitude and practices regarding maternal health care was noted periodically at 1-month interval till 5 months. The periodic monthly post-tests evaluation was followed by personal individual contact with TBAs for explaining regarding maternal health care and clarification of their doubts. The early post-test impact of training was noted at the first month wherein only 45 TBAs participated and the late impact was noted at the fifth month for which only 40 TBAs participated. Others were lost to follow-up. Statistical analysis was done by using Mc. Nemer test, Chi-square test with Yate’s correction and Fischer’s exact test.
Results
In our study, 40 % of TBAs were trained before the training programme. Majority were illiterates. Most of them were in the age group of 40 and 60 years. (Tables 1, 2, 3, 4 and 5). Most of the TBAs were conducting deliveries since more than 5 years. Out of 20 previously trained TBAs, only 17 and 15 TBAs were evaluated at early and late post-test period, respectively. Out of 30 untrained TBAs, only 28 and 25 TBAs were evaluated at early and late post-test period, respectively. Others were lost to follow-up.
Table 1.
Impact of training on knowledge about maternal health care
| Knowledge about maternal health care | Trained TBA | Untrained TBA | ||||
|---|---|---|---|---|---|---|
| Pretest (n = 20) (%) | Post-test | Pretest (n = 30) (%) | Post-test | |||
| Early (n = 17) (%) | Late (n = 15) (%) | Early (n = 28) (%) | Late (n = 25) (%) | |||
| Antenatal care | ||||||
| Regular antenatal care (Min. 3) | 50 | 88.2* | 93.3** | 10 | 60.7* | 75** |
| Danger signals during antenatal period | 50 | 88.2* | 86.6** | 3.3 | 17.8 | 44** |
| Referral if complications | 85 | 100 | 100 | 53.3 | 89.3 | 100** |
| Intranatal care | ||||||
| All five cleans | 30 | 52.9 | 80** | 0 | 78.6* | 88** |
| Complications during labour | 50 | 70.5 | 80 | 10 | 46.4* | 60** |
| Immediate newborn care | 75 | 82.3 | 93.3 | 43.3 | 53.6 | 60** |
| Referral if complications | 80 | 88.2 | 100 | 23.3 | 82.1* | 96** |
| Postnatal care | ||||||
| PNC visits (min.3) | 60 | 82.3 | 100 | 15 | 42.8* | 68** |
| Complications | 45 | 64.7 | 80 | 0 | 17.8 | 44** |
| Referral if complications | 80 | 100 | 100 | 26.6 | 85.7* | 100** |
| Know family planning methods | 55 | 82.3 | 100** | 20 | 78.6* | 96** |
* Indicates the statistically significant (p < 0.05) improvement in the percentage of TBAs at early post-test evaluation compared to pretest
** Indicates the statistically significant (p < 0.05) improvement in the percentage of TBAs at late post-test evaluation compared to pretest
Table 2.
Impact of training on the attitude towards MCH care
| Attitude towards maternal health care | Trained TBA | Untrained TBA | ||||
|---|---|---|---|---|---|---|
| Pretest (n = 20) (%) | Post-test | Pretest (n = 30) (%) | Post-test | |||
| Early (n = 17) (%) | Late (n = 15) (%) | Early (n = 28) (%) | Late (n = 25) (%) | |||
| Regular antenatal care needed | 40 | 70.5* | 100** | 0 | 39.3* | 64** |
| Safe delivery practices reduce maternal and newborn deaths | 35 | 70.5* | 80** | 10 | 42.8* | 60** |
| Regular postnatal care needed | 55 | 76.5* | 100** | 6.6 | 25* | 60** |
* Indicates the statistically significant (p < 0.05) improvement in the percentage of TBAs at early post-test evaluation compared to pretest
** Indicates the statistically significant (p < 0.05) improvement in the percentage of TBAs at late post-test evaluation compared to pretest
Table 3.
Impact on the antenatal care provided
| Antenatal care | Trained TBA | Untrained TBA | ||||
|---|---|---|---|---|---|---|
| Pretest (n = 20) (%) | Post-test | Pretest (n = 30) (%) | Post-test | |||
| Early (n = 17) (%) | Late (n = 15) (%) | Early (n = 28) (%) | Late (n = 25) (%) | |||
| Advice regular ANC visits to health centre | 40 | 70.6 | 86.6** | 10 | 42.8* | 48** |
| Advice IFA and Calcium tablets | 40 | 64.7 | 73.3** | 10 | 35.7 | 44** |
| Advice to take Inj. TT | 35 | 64.7 | 73.3** | 3.3 | 28.6 | 36** |
* Indicates the statistically significant (p < 0.05) improvement in the percentage of TBAs at early post-test evaluation compared to pretest
** Indicates the statistically significant (p < 0.05) improvement in the percentage of TBAs at late post-test evaluation compared to pretest
Table 4.
Impact on delivery practices
| Delivery practices | Trained TBA | Untrained TBA | ||||
|---|---|---|---|---|---|---|
| Pretest (n = 20) | Post-test | Pretest (n = 30) | Post-test | |||
| Early (n = 17) | Late (n = 15) | Early (n = 28) | Late (n = 25) | |||
| Advice hygienic preparation before delivery | 75 | 100 | 100 | 60 | 92.8* | 100** |
| Use disposable delivery kit | 35 | 100* | 93.3** | 0 | 92.8* | 92** |
| Practice all five cleans | 30 | 88.2 | 93.3** | 0 | 64.3* | 88** |
| Referral if complications | 70 | 100 | 100 | 13.3 | 85.7* | 88** |
* Indicates the statistically significant (p < 0.05) improvement in the percentage of TBAs at early post-test evaluation compared to pretest
** Indicates the statistically significant (p < 0.05) improvement in the percentage of TBAs at late post-test evaluation compared to pretest
Table 5.
Impact on postnatal care
| Postnatal care | Trained TBA | Untrained TBA | ||||
|---|---|---|---|---|---|---|
| Pretest (n = 20) | Post-test | Pretest (n = 30) | Post-test | |||
| Early (n = 17) | Late (n = 15) | Early (n = 28) | Late (n = 25) | |||
| Provide postnatal care | 50 | 70.5 | 93.3** | 0 | 28.6* | 60** |
| Referral if complications | 60 | 88.2 | 100** | 23.3 | 78.6* | 100** |
| Advice on family planning services | 40 | 70.5* | 93.3** | 0 | 57.1* | 80** |
* Indicates the statistically significant (p < 0.05) improvement in the percentage of TBAs at early post-test evaluation compared to pretest
** Indicates the statistically significant (p < 0.05) improvement in the percentage of TBAs at late post-test evaluation compared to pretest
Pretest evaluation showed that there was a difference in the depth of knowledge regarding maternal health care between trained and untrained TBAs. There was a progressive improvement in the percentage of TBAs who gained knowledge regarding maternal health care. Late post-test evaluation showed that the improvement in the percentage of previously trained TBAs was statistically significant (p < 0.05) with respect to gain in knowledge regarding ANC care, identification of danger signals during antenatal period, maintenance of all the five cleans and their knowledge regarding any one of family planning methods. Also there was a statistically significant improvement in the percentage of untrained TBAs who gained knowledge regarding maternal health care except for the immediate newborn care.
At the time of pretest evaluation, all untrained TBAs believed that regular antenatal care is not needed as it will not influence the outcome of delivery. The change in the attitude towards maternal health care at late post-test evaluation showed a statistically significant (p < 0.05) improvement in the percentage of TBAs.
There was a progressive improvement in the quality of antenatal care provided by both the groups of TBAs. Early and late impact showed that the improvement in the percentage of TBAs who provided correct antenatal care practices was statistically significant (p < 0.05).
There was a progressive improvement in the quality of safe delivery practices provided. This improvement was statistically significant (p < 0.05) among untrained TBAs and among trained TBAs with respect to use of disposable delivery kit and maintenance of all the five cleans. The practice of using disposable delivery kit and maintaining all five cleans among untrained TBAs was zero during pretest evaluation. This has gradually progressed to 93.3 and 88 %, respectively, among trained and untrained TBAs.
The progressive improvement in the percentage of TBAs who provided correct postnatal care, referral if there was any complication for the mother or newborn and advice family planning services was statistically significant (p < 0.05).
It was significant to find that 1 year after the training programme, there was no reported maternal death among the deliveries conducted by TBAs in the whole PHC area as compared to three deaths, 1 year prior to the training programme. Also the number of perinatal deaths which occurred for the deliveries conducted at home by the TBAs has reduced from eleven to three deaths (Fig. 1).
Fig. 1.
Impact of training on maternal and perinatal deaths
Discussion
The assessment of quality of antenatal, intranatal and postnatal care provided suggests that trained TBAs provide better services as compared to untrained. However, there was also a progressive improvement in the knowledge, attitude, and practices among untrained TBAs regarding maternal health care. Majority of TBAs were unaware of the pregnant women in the community, but they were called by the family only at the time of delivery. Pretest evaluation showed a statistically significant difference in the depth of knowledge among the two groups. Late post-test evaluation showed that 100 % of TBAs came to knew about the referral if complications occur during antenatal, intranatal and postnatal period. Also 100 % of them know regarding postnatal visits and advice regarding immunization to baby.
Overall improvement in the positive attitude towards MCH care was the important finding. All the trained TBAs and 64 % of untrained TBAs stressed on the need for antenatal care. Over 80 % of trained and 60 % of untrained TBAs are of the opinion that safe delivery practices will reduce maternal and infant deaths. In a similar study conducted in Rajasthan 57.89 % of TBAs had a favourable attitudes towards MCH care [6]. At the end of evaluation, 73.3 % of trained TBAs and 36 % of untrained TBAs were able to advice on immunization of antenatal mothers. In contrast, the study conducted in Nigeria showed that 91 % of them were able to advice on immunization after the training [5]. Pretest evaluation among untrained TBAs showed that they neither practiced all the five cleans nor used disposable delivery kit for conducting deliveries. Inspite of revised reproductive and child health programmes, there had been incidences where unsterilized sickle was used to cut the umbilical cord (2 untrained TBAs). Post-test evaluation showed that 92 and 88 % of trained and untrained TBAs, respectively, practiced all the five cleans. The practice of maintaining all the five cleans was gradually increased from 30 to 93.3 % among trained TBAs and from 0 to 88 % among untrained TBAs. In a study conducted in a rural area of Bangaldesh 45 % of trained TBAs were practicing hygienic delivery when compared to 19.3 % among untrained TBAs. More rigorous evaluation is needed, not only of TBA training programmes as a whole, but also of the effectiveness of the individual components of the training [7].
It was surprising during pretest evaluation that majority of TBAs do not interfere with the family planning practices utilized by the women before the training programme. The important finding was that there was a progressive improvement in the advice given regarding tubectomy after the third child birth. It has improved from 40 to 93.3 % and 0 to 80 % among trained and untrained TBAs, respectively. There was a significant reduction in the maternal and perinatal deaths among the home deliveries conducted by these TBAs as compared to 1 year prior to training. A WHO-supported study in Pune used identification of high risk neonates in rural community by home visiting by a village heath worker, providing supportive care at home and referral to the health center. The study like ours did not have a control group. It reported a 25 % reduction in the neonatal mortality rate [8]. Another study in Gadchiroli documented reduced maternal and perinatal death after the training [9].
Conclusion
Training programmes for TBAs with regular follow-ups is the need of the hour especially in resource-poor settings where immediate MCH care is not available. The Government should adopt steps to recognize the importance of TBAs, adequately compensate them, train them and improve their skills until the rural health infrastructure replaces the TBAs. It should also integrate them into Maternal and child health programmes as a first-level contact person. They should undergo continuing education sessions which will enhance their knowledge regarding MCH care and help to practice safe deliveries.
References
- 1.Bharadwaj N, Yunus M, Hasan SB, et al. Role of traditional birth attendants in maternal care services- a rural study. Indian J Matern Child Health. 1990;1(1):29–30. [PubMed] [Google Scholar]
- 2.WHO. Make every mother and child count-A tool kit for organizers of activities, 2005.
- 3.www.rch.india.org. Current fact files on Maternal Newborn and Child health situation in India.
- 4.Jeffery R, Jeffery P, Lyon A. Only cord cutters? Midwifery and child birth in rural north India. Soc Act. 1984;34(3):229–250. www.pubmed.com. [PubMed]
- 5.Akpala CO. An evaluation of the knowledge and practices of trained traditional birth attendants in Bodinga, Sokoto State, Nigeria. J Trop Med Hyg. 1994;97(1):46–50. www.pubmed.com. [PubMed]
- 6.Chaturvedi SK, Dudani IV. Knowledge and attitude of dais towards family planning. Rajasthan Med J. 1997;16(4):237–239. www.pubmed.com. [PubMed]
- 7.Goodburn EA, Chowdhury M, Gazi R, Marshal T, Graham W. Training traditional birth attendants in clean delivery does not prevent postpartum infection. Health Policy Plan. 2000;15(4):394–399. doi: 10.1093/heapol/15.4.394. [DOI] [PubMed] [Google Scholar]
- 8.Manandhar DS, Osrin D, Shrestha BP, et al. Effect of a participatory intervention with women’s groups on birth outcomes in Nepal: cluster-randomised controlled trial. The Lancet. 2004;364:970–979. doi: 10.1016/S0140-6736(04)17021-9. [DOI] [PubMed] [Google Scholar]
- 9.Bang AT, Reddy HM, Deshmukh MD, et al. Neonatal and infant mortality in the 10 years (1993–2003) of the gadchiroli field trial: effect of homebased neonatal care. J Perinatol. 2005;25(suppl. 1):S92–S107. doi: 10.1038/sj.jp.7211277. [DOI] [PubMed] [Google Scholar]