Abstract
Aim
The aim of this study was to share our experience of clinical presentation and ultrasonographic findings in cases of ectopic pregnancy especially in the context of usage of unsupervised medical abortifacients.
Settings and Design
This is prospective study conducted over a period of 1 year extending from August 01, 2009 to July 31, 2010 in a tertiary care Armed Forces Hospital of India.
Materials and Methods
Clinically and or sonologically suspected cases of ectopic pregnancy formed the study group. Detailed clinical, menstrual, and treatment history was obtained for each patient. Ultrasonography (USG) was done with multifrequency convex (2.5–6 MHz) followed by transvaginal (6–10 MHz) probes. Operative findings were noted and recorded in each case.
Results
In the study period, a total of 1958 pregnant patients were admitted and treated, which included 1690 deliveries and 268 abortions. Based on USG findings, 16 cases (0.8 %) of ectopic pregnancy were diagnosed. While four patients were treated medically (with methotrexate), 12 cases underwent surgery. Out of 16 cases, 10 cases were suspected clinically as ectopic pregnancy. Features suggestive of menorrhagia, threatened abortion, and pelvic inflammatory disease were present in five, three, and three cases, respectively. History of intake of medical abortifacients (MA) (mifepristone followed by misoprostol) was present in 07 (43.75 %) cases. On USG, commonest abnormality was a complex adnexal mass seen in 12 (75 %) cases. Gestational sac with definite embryo within and surrounding echogenic rim was seen in five cases. Live ectopic pregnancy was diagnosed in two (12.5 %) cases. Endometrial thickness was less than 10 mm in all cases who had taken MA. Pseudo gestation sac was seen in 02 (12.5 %) cases. Significant hemoperitoneum was present in 10 out of 12 cases operated. Organized hematoma in pelvis masking the presence of adnexal mass was noted in three cases.
Conclusion
Over-the-counter availability, failure to strictly follow the guidelines, unsupervised usage of MA along with atypical clinical history have increased diagnostic dilemma in ectopic pregnancy. Sonographic findings are frequently atypical in such cases. Ectopic pregnancy may remain under-diagnosed with potentially serious consequences in patients who have taken MA without prior confirmation of intrauterine gestation.
Keywords: Medical abortifacients, Ectopic pregnancy, Ultrasonography
Introduction
Ectopic pregnancy (EP) is a leading cause of maternal morbidity and mortality in the first trimester. The incidence of EP has steadily risen since 1970s and now accounts for approximately 2 % of all pregnancies [1–3]. Timely diagnosis and appropriate management can reduce the maternal morbidity and mortality significantly. Transvaginal ultrasonography (TVS) coupled with quantitative serum βHCG estimation has increased the diagnostic accuracy manifolds although each modality has its own limitation. Despite tremendous advances in the medical science, diagnosis of EP is not always easy. The classic clinical triad of amenorrhea, lower abdominal pain, and bleeding per vaginum is present in less than 50 % of cases [4]. Diagnostic dilemma is further compounded when EP is not suspected clinically because of atypical clinical presentation. An example of such a scenario is when a woman reports for prolonged bleeding per vaginum and lower abdominal pain after taking medications (mifepristone followed by misoprostol) for medical abortion, the signs and symptoms may be attributed to be a part of abortion process. As per guidelines, mifepristone and misoprostol combination is supposed to be administered under strict supervision by an authorized medical practitioner in a center approved for medical termination of pregnancy, after taking into consideration several contraindications one of which is the suspected EP. Despite strict regulations in this aspect, over-the-counter sale of medical abortifacients (MA) with or without prescription is not uncommon in India. Suffice it to say that it is practically impossible to confirm or exclude an early intrauterine pregnancy without a sonographic examination. We share our experience of clinical presentation and ultrasonographic findings in cases of EP especially in the context of usage of unsupervised MA in a busy tertiary care Armed Forces Hospital of India. We also highlight the diagnostic difficulties encountered in those cases.
Materials and Methods
All our patients were families of Armed Forces personnel admitted and treated in our institution for various obstetric and gynecological conditions. The study group was selected from a total number of 1958 pregnant patients admitted during the study period (Aug 2009–Jul 2010). Besides, routine antenatal ultrasonography (USG), patients were also referred to the department of radiodiagnosis for the USG of pelvis with a variety of other clinical indications which included suspected EP, menorrhagia, threatened abortion, pelvic inflammatory disease, nonspecific lower abdominal pain, etc. All patients were referred for USG by the attending gynecologist or the medical officer in the family ward or out patient department. Two radiologists, having 12 and 8 years of experience of doing USG, carried out the sonographic studies. All patients were initially examined with multifrequency (2.5–6 MHz, Wipro GE LOGIQ P5) convex transabdominal probe with a moderately distended urinary bladder. Transvaginal sonography (TVS) (6–10MHZ, Wipro GE LOGIQ P5) was carried out in all cases of suspected EP. In addition, TVS was also carried out whenever there was a positive finding on transabdominal sonography (TAS) (e.g., suspected hemorrhagic cyst in ovary/endometrioma, etc.), when visualization of pelvic organs was suboptimal on TAS, and lastly whenever there was any clinico-radiological mismatch. The sonographic study assessed the presence or the absence of the following: (a) extrauterine gestation sac containing a yolk sac or fetal pole with or without cardiac motion, (b) complex adnexal mass, (c) endometrial thickness, (d) pseudo gestation sac, and (e) amount of fluid (anechoic/particulate) in the pelvis/abdomen. As a routine, representative positive images of all patients were archived in digital format. Sonographic findings of all patients were recorded for future reference. Cases of EP diagnosed on the basis of TVS formed the study group. Detailed sonographic findings of suspected cases of EP were recorded separately. Detailed history including menstrual history, history of intake of any previous medication, and treatment history was taken in each case. Clinical examination findings including per vaginum examination was noted for each patient. Whenever a diagnosis of EP was made on sonography, the attending gynecologist was informed immediately about the patient. Urgent serum βHCG estimation was done in all relevant cases at the discretion of the gynecologist. Wherever relevant, serum βHCG estimation was repeated after 48 h. Decision for expectant, medical, or surgical management was made by the treating gynecologist based on standard guidelines and overall merit of the case. Follow-up USG was carried out wherever deemed necessary. Medical treatment was carried out with methotrexate (1 mg per kg body weight, and IM on alternate day for 3 days). βHCG estimation was repeated weekly in patients who were treated with methotrexate. Details of operative findings were recorded for those who underwent surgery. At the end of the study period, patient-related data, sonographic and operative findings, were analyzed for all cases of EP treated in our hospital during the study period.
Results
Between Aug 01, 2009 and July 31, 2010, 1958 pregnant patients were admitted and treated in our hospital. This included 1690 deliveries and 268 abortions. All patients of abortions (spontaneous/induced, and medical/surgical) had at least one prior pelvic USG done. Based on sonographic (TVS) findings 16 (0.8 %) patients were diagnosed to have EP. Out of 16 patients of EP, 10 (62.5 %) were from Pathankot (Punjab) and adjoining areas of Himachal Pradesh; remaining 06 were from various other states of India, belonging to families of Armed Forces Personnel. Age group of the study group patients ranged from 20 to 40 years with a mean age of 27 years. Majority (14/16, 87 %) of the patients were second gravida or above. One patient was undergoing treatment for primary infertility. One patient had a history of previous EP.
Serum levels of βHCG in women with suspected EP were <700 mIU/ml in four patients (25 %), 700–1,500 mIU/ml in five patients (31.25 %) and >1,500 mIU/ml in seven patients (43.75 %), respectively. Out of 16 cases, 10 (62.5 %) cases were suspected clinically as EP. Clinical features suggestive of menorrhagia, threatened abortion, and pelvic inflammatory disease were present in five, three, and three cases, respectively. One patient had a clinical diagnosis of acute appendicitis. History of intake of MA (mifepristone followed by misoprostol) was present in 07 (43.75 %) cases. All of them did pregnancy test at home with commercially available kits. Five out of seven patients took the abortifacients (mifepristone followed by misoprostol) directly from the retail outlet without any prescription. Two patients did visit private doctor who prescribed them the MA. None of these patients was advised any pelvic USG for confirmation of intrauterine pregnancy before taking MA. While 4 out of 16 patients were treated medically (methotrexate), 12 cases underwent surgery. Out of 12 cases operated, 8 (66.6 %) had ruptured ectopic pregnancy, three tubal abortions, and one chronic ectopic.
USG Findings (Table 1): Complex adnexal mass was the commonest abnormality on TVS seen in 12 (75 %) cases (Fig. 1). Gestational sac with definite embryo and or yolk sac within was noted in 5 (31.2 %) cases. Embryonic cardiac activity suggesting live ectopic pregnancy was noted in 2 (12 %) cases (Figs. 2, 3a, b). Mean endometrial thickness was 12 mm (range 5–20 mm). Endometrial thickness was less than 10 mm (mean = 7 mm) in all cases who had taken MA. Pseudo gestation sac was seen in 02 (12.5 %) cases. Organized hematoma in pelvis masking the presence of adnexal mass was noted in three cases. Significant hemoperitoneum (particulate fluid in pelvis, both iliac fossae and both flanks) was present in 10 out 12 cases operated.
Table 1.
Sonographic findings in ectopic pregnancy (total patients = 16)
| Sonographic findings | Number | % |
|---|---|---|
| Extrauterine gestation sac seen | ||
| Yolk sac seen | 4 | 25 |
| Embryo with cardiac activity | 2 | 12.5 |
| Embryo without cardiac activity | 3 | 18.75 |
| Thick echogenic rim surrounding gestation sac | 4 | 25 |
| Indistinct echogenic rim surrounding gestation sac | 3 | 18.75 |
| Complex adnexal mass | 12 | 75 |
| Significant hemoperitoneum present (pelvis and both flanks) | 10 | 62.5 |
| Pseudogestation sac | 2 | 12.5 |
| Endometrial thickness | ||
| >10 mm | 6 | 37.5 |
| <10 mm | 8 | 50 |
Fig. 1.
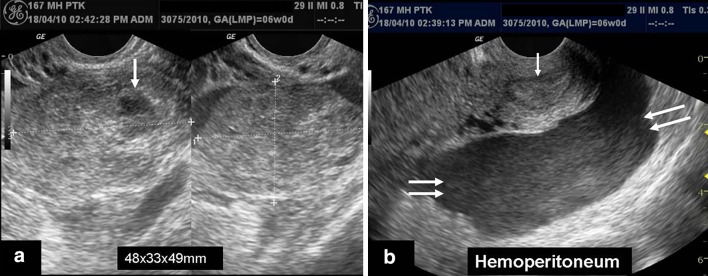
a, b Transvaginal sonogram in a patient who had taken medical abortifacients without prior confirmation of intrauterine gestation. a An ill-defined left adnexal mass with an irregular margined sac-like structure (single white arrow) within is noted. Note that the trophoblastic reaction surrounding the sac is indistinct. b Significant particulate fluid consistent with hemoperitoneum (double white arrow) is noted in the pelvis. Also note that the endometrial thickness and reaction are not very prominent
Fig. 2.

Transvaginal sonogram in a 26-year-old female who had taken medical abortifacients without prior confirmation of intrauterine gestation. A gestation sac with an embryo (7 weeks 2 days) within is clearly visible in the right adnexa. The inset picture shows the presence of cardiac activity confirming a diagnosis of live ectopic pregnancy
Fig. 3.
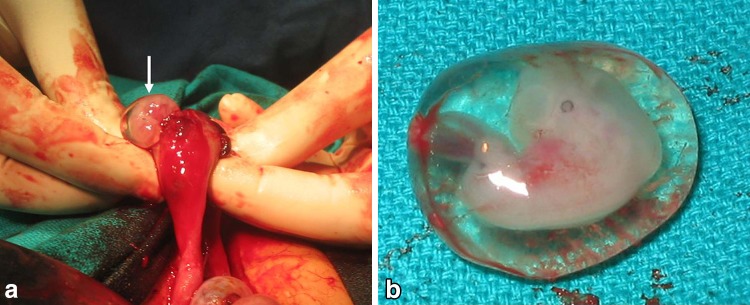
a, b Per operative finding and specimen of the same patient as in Fig. 2. a The ectopic gestation being delivered from the ampullary end of right Falopian tube with intact sac (white arrow). b Photograph of the specimen taken immediately after the ectopic gestation was delivered. Note that the embryo is contained within an intact gestation sac
Discussion
EP refers to implantation of a fertilized egg out side the uterine cavity, with the commonest (97 %) site being the fallopian tube. Other sites of EP are rare and include cornual (2 %), abdominal (1.4 %), and ovarian/cervical (0.2 %) pregnancy [1, 4]. As per the estimates of the Centre for Disease Control and Prevention (CDC), there has been a sixfold increase in the frequency of EP from 1970 to 1992. Owing to improvements in the diagnostic technology (e.g., TVS, serum βHCG estimation, etc.) and timely management, case fatality rates have declined drastically from 35.5 deaths per 10,000 cases in 1970 to 2.6 per 10,000 cases in 1992 [1–3]. Despite significant reduction in the mortality rate, EP continues to be the leading cause of pregnancy-related deaths during the first trimester. Ruptured EP accounts for 10–15 % of all maternal deaths [1]. The key to successful management of EP essentially lies in high index of clinical suspicion, appropriate risk stratification, early diagnosis (with TVS + serum βHCG estimation), and timely management. However, accurate diagnosis of EP is not always easy. No amount of symptoms and physical signs can make a diagnosis or exclude a diagnosis of EP with certainty [5, 6]. This happens primarily because of a significant clinical overlap with other related/unrelated conditions (e.g., ruptured follicle, ovarian torsion, various phases of abortion, pelvic inflammatory disease, acute appendicitis, calculus disease of the urinary tract, etc.).
About 30 million of abortions worldwide are performed every year. Although abortion has been legalized in India more than 3 decades ago, number of illegal abortions far outweighs the number of legal abortions in India. Various factors may be responsible for this like literacy, economic status, social customs, limited access/availability of suitable center for surgical abortions and last but not the least female feticide. Although the exact figure is not known, it is estimated that unsafe abortion accounts for 12–18 % of all maternal deaths in India. According to the Consortium on National Consensus for Medical Abortion in India, on an average about 11 million abortions take place annually and around 20,000 women die every year because of abortion-related complications mostly attributable to illegal abortions [7]. Over the last two decades, medical termination of pregnancy (mifepristone followed by misoprostol) has emerged as a reasonably safe and effective alternative to surgical abortion up to a certain limit of gestational age (49–63 days) [8–12].
Progesterone is vital for maintaining the developing embryo. Mifepristone blocks action of progesterone at the receptor label, alters the endometrial lining, and induces endometrial shedding. Misoprostol, an analog of prostaglandin E1, interacts with prostaglandin receptors and results in softening of cervix and uterine contractions leading to expulsion of the uterine contents. The clinical efficacy and relative safety of medical abortion has already been established worldwide. In the year 2000, the US Food and Drug Administration (FDA) has approved the use of mifepristone/misoprostol combination (mifepristone 600 mg orally followed 2 days later by 400 μg of misoprostol orally) for pregnancy up to 49 days of gestation. Mifepristone was approved for use in India in 2002. Medical termination of pregnancy rules 2003 of India clearly defines that Mifepristone (RU‐486) with Misoprostol may be prescribed for termination of early pregnancy not exceeding 7 weeks by a registered medical practitioner as prescribed under section 2 (d) and rule 3 (MTP Act) having access to a place approved by the Government under section 4 of the MTP act 1971 read with MTP Amendment Act 2002 for surgical and emergency back-up whenever required. In other words, Mifepristone was approved to be made available for medical termination of pregnancy (MTP) in India strictly under the provisions of the MTP Act, 1971 under which, pregnancy can be terminated (1) by approved physicians (2) at approved centers (3) for approved indications, and (4) for approved duration. In the year 2004, an important judgment was passed by Rajasthan State Human Rights Commission in response to a petition by Dr SG Kabra, to curb misuse, free sale/availability of mifepristone over the counter [13]. Despite all rules and regulations, mifepristone/misoprostol combination continues to be freely available over the counter with or without prescription in India. Random surveys from various parts of India confirm this. Our experience also bears similar trends. As per guideline, mifepristone/misoprostol combination should only be used under supervision in an approved center. A woman has to visit the center at least three times during the course of treatment. Before starting treatment with mifepristone/misoprostol combination, it is mandatory to ascertain suitability of the patient for medical abortion after going through the mandatory check list including the list of contraindications. Suspected/confirmed ectopic pregnancy/undiagnosed adnexal mass are among the important contraindications of medical abortion.
Pelvic sonography (TAS/TVS) is a well-established, easily available, highly accurate means of confirming and dating intrauterine gestation. A positive urine pregnancy test, however, does not guarantee an intrauterine gestation. Hence, patients who take MA purely on the basis of urine pregnancy test and without sonographic confirmation of intrauterine gestation will always run the risk of missing an EP with potential disastrous consequences. Diagnostic confusion is further accentuated because such patients often attribute the continued bleeding per vaginum and pain lower abdomen as a part of the abortion process which may have been communicated by the pharmacist/doctor at the time prescribing/dispensing the medicines. Therefore, these patients do not raise an alarm about such symptoms. As a result, they tend to report late to a gynecologist. Even when they report to a gynecologist, initially they tend to hide the history of unsupervised intake of MA, may be for the fear of facing criticism from the doctor or social reasons or else. Today’s practitioners of family medicine including sonologists need to have a high index of suspicion and elicit the history of intake of MA whenever present by asking leading questions if required. Sonographic diagnosis of EP in patients who had taken MA become slightly complicated unless one visualizes a clear cut extrauterine gestation sac with an yolk sac and or embryo within, with or without cardiac activity. As has been observed in our study, endometrial thickness is frequently low in such patients because of endometrial shedding likely secondary to antiprogesterone effect of mifepristone. Similarly, we have observed that the echogenic rim surrounding the gestation sac were mostly indistinct in patients who have taken MA supporting the antiprogesterone effect of mifepristone. The association of thin endometrium and indistinct decidual reaction, as observed in some of our patients who have taken MA, needs to be validated by larger case control/cohort studies. Thin endometrium and indistinct echogenic rim surrounding the gestation sac in such a patient certainly increases the diagnostic dilemma. In these settings, diagnostic dilemma is further compounded when the adnexal mass is surrounded by organized blood clots and fibrinous strands merging with the outline of adnexal mass. Based on USG findings alone, differentiation from pelvic inflammatory disease may be extremely difficult at times. Under these circumstances, one practical solution is to aspirate the fluid in the pelvis with a fine needle under direct USG guidance which would help immediate confirmation/exclusion of hemoperitoneum.
Use of sonography as the sole modality to establish the location of pregnancy in women before administration of mifepristone and misoprostol has been previously debated by Fielding et al. [14]. The authors, in their study, concluded that clinicians felt confident in most cases of not using sonography for diagnosis of intrauterine gestation. The authors also suggested that by monitoring βHCG levels to identify any ectopic or continuing pregnancies, medical abortion can be safely performed without sonography. However, in India, the scenario is slightly different. Here, USG facility is widely available compared with centers for βHCG estimation. A single USG test can document the presence of intrauterine gestation as well as accurately date the pregnancy which is not possible with βHCG estimation. Moreover, as of today, βHCG estimation is costlier than a USG test. Another advantage of USG study is that the results are available immediately to the treating physician for taking a quick decision, while it takes at least 24–48 h for βHCG estimation results to arrive depending on the place and center. USG not only identifies intra/extrauterine pregnancy with rapidity and accuracy, it also helps identifying various conditions that mimic ectopic pregnancy which is equally important. Considering the above issues, USG would possibly remain as the frontline modality of choice for diagnosis of intrauterine gestation before prescribing MA. However, serial βHCG estimation would continue to remain useful in cases where USG findings are inconclusive and also for monitoring success of medical management (e.g., methotrexate) of EP.
Despite our clientele being very limited, supposedly educated, we have observed cases of unsupervised usage of MA compounding the dilemma in the timely diagnosis of EP. This represents just the tip of the iceberg, and the actual situation in general population may be worse. What is urgently needed today is awareness among health care providers as well as patients, about the MA, their indications, contraindications, and correct/appropriate usage under supervision. Appropriate usage of MA will go a long way in reducing maternal morbidity and mortality of unsafe surgical abortions especially in developing countries like India. The pharmacists/chemists at the retail outlet have an important role to play in preventing/reducing misuse of MA.
Relatively small size of the study group is an important limitation of our study. A larger sample size and a case control/cohort study would be needed before any concrete conclusion can be drawn out of it. Our observations, although preliminary, seems logical, scientific, and clinically relevant. There is a need to undertake a prospective study with larger sample size in near future.
Conclusion
Over-the-counter availability, failure to strictly follow the guidelines, unsupervised usage of MA along with atypical clinical history have increased diagnostic dilemma in EP. Sonographic findings are frequently atypical in such cases. EP may remain under diagnosed with potentially serious consequences in patients who have taken MA without prior confirmation of intrauterine gestation. Clinicians and sonologists need to have high index of suspicion and be aware about the spectrum of sonographic findings in such cases to minimize/prevent any catastrophe. Mandatory sonographic confirmation of intrauterine pregnancy, as a protocol, before administration of MA would certainly help in preventing/minimizing the incidence of missed/delayed diagnosis of EP in such patients.
Conflict of interest
None.
Contributor Information
Jyotindu Debnath, Phone: +91-9216915034, Email: jyotindu_debnath@rediffmail.com.
Surendra Kumar Gulati, Email: skgorama@yahoo.co.in.
Ankit Mathur, Email: ankitmathur74@yahoo.com.
Ritu Gupta, Email: rohitdr2001@yahoo.co.in.
Nikhilesh Kumar, Email: nikhileshkumar16@gmail.com.
Sunil Arora, Email: arora.s915@yahoo.com.
R. Bala Murali Krishna, Email: rbm_krshna@rediffmail.com.
References
- 1.Lozeau AM, Potter B. Diagnosis and management of ectopic pregnancy. Am Fam Physician. 2005;72:1707–1714. [PubMed] [Google Scholar]
- 2.Goldner TE, Lawson HW, Xia Z, et al. Surveillance for ectopic pregnancy: United States, 1970–1989. CDC surveillance summaries (December) MMWR. 1993;42(SS-6):73–85. [PubMed] [Google Scholar]
- 3.CDC Ectopic pregnancy—United States, 1990–1992. MMWR. 1995;44(3):46–48. [PubMed] [Google Scholar]
- 4.Sepilian VP, Wood A. Ectopic Pregnancy. eMedicine, Obstetrics and Gynecology. May 2010.
- 5.Dart RG, Kaplan B, Varaklis K. Predictive value of history and physical examination in patients with suspected ectopic pregnancy. Ann Emerg Med. 1999;33:283–290. doi: 10.1016/S0196-0644(99)70364-1. [DOI] [PubMed] [Google Scholar]
- 6.Gutman SJ, Lindsay K. Suspected ectopic pregnancy: can it be predicted by history and examination? Can Fam Physician. 2000;46:1297–1298. [PMC free article] [PubMed] [Google Scholar]
- 7.Iyenger S. Current status of abortion in India. In: Consortium on national consensus for medical abortion in India: WHO–CCR in human reproduction. All India Institute of Medical Sciences, New Delhi.
- 8.Mittal S. Guidelines for medical abortion in India. In: Consortium on national consensus for medical abortion in India: WHO–CCR in human reproduction. All India Institute of Medical Sciences, New Delhi.
- 9.Spitz IM, Bardin CW, Benton L, et al. Early pregnancy termination with mifepristone and misoprostol in the United States. N Engl J Med. 1998;338:1241–1247. doi: 10.1056/NEJM199804303381801. [DOI] [PubMed] [Google Scholar]
- 10.Coyaji K. Early medical abortion in India: three studies and their implications for abortion services. J Am Med Womens Assoc. 2000;55(3 Suppl):191–194. [PubMed] [Google Scholar]
- 11.Coyaji K, Elul B, Krishna U, et al. Mifepristone-misoprostol abortion: a trial in rural and urban Maharashtra. India Contracept. 2002;66:33–40. doi: 10.1016/S0010-7824(02)00309-8. [DOI] [PubMed] [Google Scholar]
- 12.Tran NT, Jang MC, Choe YS, et al. Feasibility, efficacy, safety, and acceptability of mifepristone-misoprostol for medical abortion in the Democratic People’s Republic of Korea. Int J Gynaecol Obstet. 2010;109(3):209–212. doi: 10.1016/j.ijgo.2010.01.012. [DOI] [PubMed] [Google Scholar]
- 13.Mifepristone can be sold only to approved MTP Centres: Rajasthan State HRC. Indian Express Health Care Management. May 2004.
- 14.Fielding SL, Schaff EA, Nam NY. Clinicians’ perception of sonogram indication for mifepristone abortion up to 63 days. Contraception. 2002;66:27–31. doi: 10.1016/S0010-7824(02)00316-5. [DOI] [PubMed] [Google Scholar]


