Abstract
The aim of this study is to evaluate the results of closure of subtotal perforation by tympanoplasty using underlay technique with the perichondrium/temporalis fascia graft supported by single cartilage slice anteriorly. Our hypothesis was that the cartilage support, single slice, offers an extremely reliable method for reconstruction of the tympanic membrane in cases of advanced middle ear pathology and Eustachian tube dysfunction. Retrospective and prospective study of patient undergoing tympanoplasty in subtotal perforation with graft supported by a slice of cartilage between March 2000 and October 2005. Intact perichondrium/temporalis fascia was placed as graft in subtotal perforation, supported by a slice of cartilage. Slice was placed anteriorly from hypotympanum to anterior part of attic. It does not obstruct Eustachian tube opening, as it is curved with concavity facing towards medial wall and lined by perichondrium without any raw area, which prevents adhesion formation. Hearing results were reported using four frequency (500, 1,000, 2,000 and 3,000) pure tone average air-bone gap. During the study period, perichondrium/temporalis fascia graft with support of cartilage slice was used for tympanic membrane reconstruction in 94 patients. Overall graft take rate was 98.94 %. In 95.74 % of patients of different types of tympanoplasty achieved hearing level of 30 dB or less. Complications included residual perforation in (1.06 %), infection or gaping of wound in 2 (2.13 %). Cartilage slice support offers an extremely reliable method for reconstruction of tympanic membrane in cases of high-risk perforation (subtotal perforation, retraction pocket, cholesteatoma, anterior perforation of tympanic membrane).
Keywords: Tympanoplasty, Subtotal perforation, Cartilage slice, High-risk perforation
Introduction
Repair of subtotal perforations are difficult because very little support is there for the graft particularly along the anterior rim of perforation, also there are chances of recurrence of pathology due to Eustachian tube dysfunction. Chances of failure are very high in anterior–superior quadrant, since the graft may fall around the Eustachian tube orifice leading to the medialization of graft and blocking the Eustachian tube [1]. During post operative period shrinkage of graft can occur leading to residual perforation, especially near the anterior annular region. The underlay technique with fascia or perichondrium is an uncertain method. The soft material, which is only fixed by adhesion, can easily be displaced during wound healing. Temporalis fascia and perichondrium are the most popular and commonly used graft material. They contain collagen and mucopolysaccharides. These two components give it a high tensile strength and low metabolic rate. For this reason it does not get autolysed in the presence of infection. Cartilage being a bradytrophic tissue allows stable and functionally reliable reconstruction of the ear drum. Subtotal reconstruction of tympanic membrane with graft supported by cartilage anteriorly counteracts tendency to reconstruction of soft autologous materials like temporalis fascia or perichondrium. Because of its low turnover rate, cartilage is more resistant to infection.
Heerman [2] showed in cartilage tunnel at Eustachian tube Entrance that it has been very useful in all tympanoplasty types in maintaining the patency of the tubal entrance and in reconstructing the antero-inferior aspect of the tympanic membrane. The proper direction of this tunnel and cartilage bridge will lead to an easy construction of the remainder of the tympanic membrane by use of multiple pieces of fascia or cartilage.
The purpose of this study is to evaluate the results of closure of subtotal perforation of tympanic membrane by tympanoplasty using underlay technique with supporting the graft by single cartilage piece anteriorly. It gives support to the graft anteriorly and prevents it from falling and also residual perforation.
Materials and Methods
Operative Technique
The general technique of reconstruction of subtotal perforation (Fig. 1) using perichondrium or temporalis fascia graft with single piece of cartilage begins with harvest of temporalis fascia. Post-auricular incision is given. Temporalis fascia is obtained from lateral surface of temporalis muscle. To obtain tragal cartilage, incision is made slightly posterior to the free edge of the tragus to expose the cartilage. Dissection is first taken to free the cartilage on its ventral surface from the overlying muscle and then carefully on its dorsal surface from the thin canal skin. The cartilage is then cut depending on the size of the graft required.
Fig. 1.

Pre-operative photograph showing subtotal perforation of tympanic membrane
Subsequently, a T shaped incision is made. A Farabeuf’s periosteum elevator is used to mobilize the periosteum to the level of the ear canal. Horizontal incision is then made on skin of the posterior canal wall. Edges excised with sickle knife and undersurface of the perforation is freshened.
Under operating microscope tympanomeatal flap elevated up to the annulus. Middle ear entered by piercing the middle ear mucosa from the posterior-superior quadrant. Middle ear is examined, handle of malleus is denuded and ossicular chain is checked for continuity and mobility.
First a slice of cartilage, slightly curved, covered with perichondrium placed from hypotympanum to anterior part of attic. Anteriorly slice of tragal cartilage with intact perichondrium/temporalis fascia placed as graft (Figs. 2, 3). It does not obstruct Eustachian tube opening, as it is curved with concavity facing towards medial wall and lined by perichondrium without any raw area, which prevents adhesion formation.
Fig. 2.
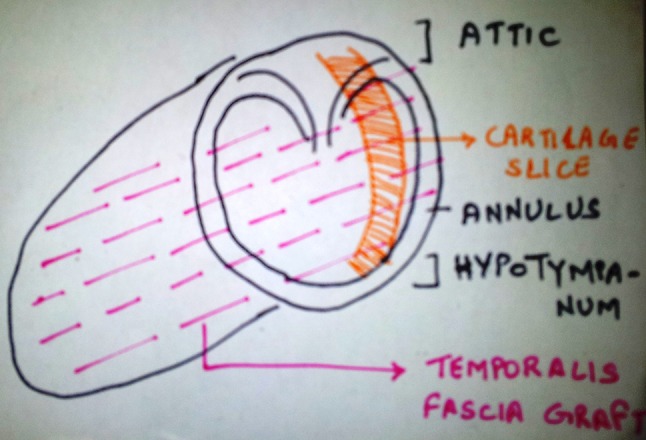
Line diagram demonstrating proper placement of temporalis fascia graft on cartilage slice support
Fig. 3.

Post-operative photograph after placement of temporalis fascia graft and cartilage slice
If required ossicular reconstruction is done using tragal cartilage with intact perichondrium. Gel foam soaked antibiotic solution is packed in middle ear. Tympanomeatal flap replaced. Canal is packed with antibiotic impregnated with gelfoam. Post-operative pure tone audiometry was done after 3 months.
Results
During the study period, cartilage slice was used for tympanic membrane reconstruction in more than 100 patient, of which 94 had the hospital charts and full follow-up record.
Of these 63 (66.67 %) were female cases and 31 (33.33 %) were male cases, most of the patients belongs to age group of 11–20 years (40.42 %). 19.74 % of patient belong to age group of 21–30 years. Deafness was the chief complaint in 94.68 % cases and it was mainly conductive type with that of moderate degree in 55.32 % cases. Severe degree of conductive deafness is present in 36.17 % cases. Tympanoplasty was done using both post-aural (91.49 %) as well as end-aural (8.51 %) approach. Subtotal perforation was seen in all cases. Granulation was present in 26.60 % cases and cholesteatoma in 21.28 % cases. Incus was the most common ossicles found necrosed in 34.04 % cases followed by malleus.
Type I tympanoplasty was done in 62.77 % cases followed by Type II in 31.91 % cases. Type III and IV tympanoplasty was done in 3.19 and 2.13 % cases. The average duration of follow up was 6 months ranging from 3 months to 4 years.
Overall graft take rate was 98.94 %. Only one patient had partial take-up due to development of postoperative infection. 95.74 % of patients of different types of tympanoplasty achieved hearing level of 30 dB or less i.e. socially acceptable hearing. Good result was found in type I tympanoplasty 84.75 % of cases air bone closure up to 20 dB. Postoperative complications were minimal. 2.13 % had infection and gaping of wound, which was managed conservatively. Only 1.06 % cases had residual perforation.
Discussion
Hearing is one of the most important and visible functions of the ear. Impairment of hearing, results in substantial disability. Perforation of tympanic membrane causes conductive hearing loss. This is a serious health concern worldwide, not only because of the distress it causes to the patients and relatives, but also the associated hearing impairment imposes substantial economic burden on the patient and health care system.
Permanent restoration of hearing is the goal of functional reconstruction of the perforations of tympanic membrane by tympanoplasty. Otologists to repair subtotal perforation now practice various techniques.
Problems with Closure of Subtotal Perforation
Very little support is provided by the remnant of tympanic membrane anteriorly.
Graft may fall around the Eustachian tube orifice.
Medialization of graft and blocking of Eustachian tube opening.
Residual perforation in anterior quadrant.
Perforation fails to close in approximately 10 % of tympanoplasty surgeries [3]. Reason for failure are graft displacement, improper placement, autolysis, infection, haemorrhage, Eustachian tube dysfunction etc.
The use of cartilage support is experiencing a renaissance in ear surgery because it appears to offer an extremely reliable method for reconstruction of tympanic membrane in cases of middle ear pathology and Eustachian dysfunction. Conceptually, one might anticipate a significant conductive hearing loss with a tympanic membrane that is rigid and thick, a fact that has hampered the routine acceptance of cartilage as a grafting material. But single slice support has changed that, resulting greater acceptance.
Heerman showed in cartilage tunnel at the Eustachian Tube Entrance that it has been very useful in all types of tympanoplasty in maintaining the patency of the tubal entrance and in reconstructing the antero-inferior aspect of the tympanic membrane. The proper direction of this tunnel and cartilage bridge will lead to an easy construction of the remainder of the tympanic membrane by use of multiple pieces of fascia or cartilage [2].
Heerman also used small cartilaginous chips for reconstruction of the eardrum and introduced it as Palisade Cartilage Tympanoplasty. Reconstruction of subtotal perforation of tympanic membrane with cartilage palisades counteracts the tendency of retraction of soft autologous materials like temporalis fascia or perichondrium. Cartilage is more resistant to the prolonged absence of neovascularisation from the periphery in large central and subtotal perforation making it more resistant to infection [2].
Borkowski et al. [4] introduce a perichondrium–cartilage composite graft for closure of total perforations of the tympanic membrane. An oval shaped piece of cartilage with perichondrium on one side was harvested from cavum conchae. The cartilage was cut in the shape of U without removing the inner layer of perichondrium. The inner diameter of the cartilage ring should be nearly the same as the diameter of the tympanic ring. This cartilage framework stabilizes and fixes the perichondrium and prevents the perichondrium from subsiding into the middle ear cavity. The cartilage ring also reduces shrinking of the perichondrium. In all patients, the tympanic membrane was closed and no residual perforation occurred (27 patients). The hearing results in tympanoplasty were the same as in other techniques with a residual air-bone gap of 20 dB [4].
Dornhoffer [5] compared the hearing results of patients with cartilage tympanoplasty with results of patients who underwent revision tympanoplasty using perichondrium. He showed 100 % take up rate of cartilage tympanoplasty compared to 85 % of perichondrium with no difference in hearing improvement [5].
Indorewala [6] introduced approach to middle ear by lifting the anterior annulus tympanicus and anchorage the graft underneath the anterior tympanomeatal flap and named the technique as anterior tympanotomy, author did 1,113 tympanoplasties by this technique and his failure rate was only 0.09 %.
Dornhoffer [7] showed good anatomical and audiologic results in cartilage tympanoplasty. In cases of high-risk perforation, reconstruction with cartilage yielded anatomical and functional results that compared favourably to primary tympanoplasty using traditional techniques, which have showed high rates of retraction and failure. He classified high-risk cases as those, which are of revision surgery, a perforation near to anterior annulus and larger than larger than 50 % or bilateral perforations. Significant hearing improvement was realized in all pathological groups (subtotal perforation, atelectatic ear, cholesteatoma) and chances of recurrence or displacement are minimal [7].
Indorewala showed that in repair of subtotal perforation, temporalis fascia result in 83 % primary closure with only 67 % had no recurrent perforation as compared to fascia lata, which has resulted in 95 % closure and 89 % had no recurrence. Temporal fascia has been shown to shrink and thicken more. In subtotal perforation with very small margin of remnant tympanic membrane, shrinkage of graft causes a high failure rate [3].
In our study, tympanoplasty is done with intact perichondrium/temporalis fascia placed as graft supported by cartilage slice. Slice of cartilage, slightly curved, and covered with perichondrium placed from hypotympanum to anterior part of attic. It does not obstruct Eustachian tube opening, as it is curved with concavity facing towards medial wall and lined by perichondrium without any raw area, which prevents adhesion formation. Reconstruction of subtotal perforation of tympanic membrane with cartilage support counteracts the tendency to retraction of soft autologous materials like temporalis fascia and perichondrium. Because of its low metabolic rate cartilage is more resistant to the prolong absence of neovascularisation from the periphery in subtotal perforation making it more resistant to infection. Anatomical and audiological results are then evaluated.
Graft Take Up Rate and Hearing Improvement
In our study, graft take rate is 98.94 %. Only 1 out of 94 cases had residual perforation of tympanic membrane. That patient has not come for follow-up for initial 1 month, during which he had develop URI and otomycosis. This has resulted in small residual perforation that gets healed on conservative treatment. So taken this in consideration our results were almost 100 %. 95.74 % has closed air bone gap within 0–30 dB (social hearing), 21.28 % within 10 dB and 56.38 % within 20 dB in this series was obtained. 4.26 % cases has >30 dB hearing, they are cases of unsafe variety.
Dornhoffer [5] reported success rate of 85 % with perichondrium. He achieved air bone gap <20 dB by cartilage palisade technique.
Borkowski et al. [4] and Dornhoffer [7] reported 100 % results with cartilage palisade tympanoplasty and cartilage-perichondrium grafting.
Singh et al. [8] reported a graft-take up rate of 93.3 % for large central and subtotal perforation. They reported an overall hearing gain in 92.8 % cases.
Indorewala [3] reported 83 % success rate with temporalis fascia and 95 % success rate with fascia lata.
Brandtlow reported 48 % cases closing air bone gap to 15 dB in Wullstein series [9] (Table 1).
Table 1.
Take up and hearing results of various authors in cases of subtotal perforation
| Author | Type | Take up in % | Hearing |
|---|---|---|---|
| Dornhoffer [5] | Perichondrium | 85 | Air bone-gap < 10 dB |
| Borkowski et al. [4] | Cartilage–perichondrium | 100 | Air bone-gap < 20 dB |
| Singh et al. [8] | Temporalis fascia | 93.3 | Air bone-gap < 30 dB |
| Neumann et al. [11] | Cartilage palisade | 100 | Air bone-gap < 30 dB |
| Dornhoffer [7] | Cartilage palisade | 100 | Air bone-gap < 20 dB |
| Indorewala [3] | (a) Temporalis fascia | 66 | Air bone-gap < 10 dB |
| (b) Fascia lata | 95 | Air bone-gap < 20 dB | |
| Present series | Temporalis fascia/perichondrium graft with cartilage slice support | 98.94 | Air bone-gap < 30 dB |
Postoperative Complications
In this series incidence of postoperative complications was very low. In one patient i.e. 1.06 % of cases residual perforation was present. In 2.13 % cases, minimal post aural wound gaping was noted which responded to conservative management.
Medialization of graft and blockage of Eustachian tube are common problems associated with closure of subtotal perforation of tympanic membrane did not occur in this series. None of the cases developed facial nerve palsy, labyrinthitis or sensorineural deafness post operatively.
Glasscock et al. [10] reported sensorineural hearing loss in >1 % cases post operatively.
Dornhoffer reported post-operative perforation in 4.2 % cases, revision surgery for conductive deafness in 1.9 % cases and delayed facial weakness (temporary) in 0.5 %. He also had secondary cholesteatoma in 1.3 % cases [7].
Neuman et al. [11] reported post operative recurrence in 1.6 % cases with no facial weakness and otorrhea.
Hence, it was found that closure of subtotal perforation of tympanic membrane can be done effectively with near 100 % success rate by underlay technique of tympanoplasty by temporalis fascia/perichondrium with supporting the graft anteriorly by cartilage.
Conclusion
Results in our patients series indicate that this tympanoplasty technique i.e. graft supported by cartilage slice, achieve good anatomical and audiological results. Cartilage slice in spite of being rigid and thick, a fact that has hampered the routine acceptance of it, does not significantly affect post operative hearing results. With this technique, whole of tympanic membrane does not become opaque. Middle ear structure can be seen through semi transparent graft in post operative period. Any recurrence of cholesteatoma can be detected early, which will not be visible in cases of opaque tympanic membrane due to palisade or island cartilage perichondrium graft. Cartilage support offers an extremely reliable method for reconstruction of the tympanic membrane in cases of advance middle ear pathology and Eustachian tube dysfunction. Single slice prevent falling of graft in middle ear and prevent failure of graft as residual perforation. It is somewhat difficult to keep asymptomatic patient on follow up, especially in developing countries. In them cartilage support is useful in preventing recurrence due to its tensile strength as well as low rate of absorption. Cartilage slice support gives a very high success rate in cases of high-risk perforation (subtotal perforation, retraction pocket, cholesteatoma, anterior perforation of tympanic membrane). Tympanoplasty using temporalis fascia/perichondrium with graft supported by slice of cartilage anteriorly is safe and reliable procedure.
Footnotes
Richi Sinha and Richa Agrawal have contributed equally to this study.
Contributor Information
R. K. Mundra, Email: mundra.rk@gmail.com
Richi Sinha, Email: rich1.ost@gmail.com.
Richa Agrawal, Email: agrawal23richa@gmail.com.
References
- 1.Schuknecht HF, Kerr AG. Pathology of Eustachian tube. Arch Otolaryngol. 1967;86:497. doi: 10.1001/archotol.1967.00760050499007. [DOI] [PubMed] [Google Scholar]
- 2.Heerman J. Autograft tragal and conchal palisade cartilage and perichondrium in tympanomastoid reconstruction. Ear Nose Throat J. 1992;71(8):344–349. [PubMed] [Google Scholar]
- 3.Indorewala S. Dimensional stability of free fascia grafts: clinical application. Laryngoscope. 2005;115:278–282. doi: 10.1097/01.mlg.0000154733.54152.54. [DOI] [PubMed] [Google Scholar]
- 4.Borkowski G, Sudhoff H, Luckhaupt H. Autologous perichondrium–cartilage graft in the treatment of total and subtotal perforations of the tympanic membrane. Laryngorhino-otologic. 1999;78(2):68–72. doi: 10.1055/s-2007-996833. [DOI] [PubMed] [Google Scholar]
- 5.Dornhoffer JL. Hearing results with cartilage tympanoplasty. Laryngoscope. 1997;107:1094–1099. doi: 10.1097/00005537-199708000-00016. [DOI] [PubMed] [Google Scholar]
- 6.Indorewala S. The anterior tympanotomy. Indian J Otolaryngol Head Neck Surg. 1997;49:122–124. doi: 10.1007/BF03023787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dornhoffer JL. Cartilage tympanoplasty: indications, techniques, and outcomes in a 1000 patient series. Laryngoscope. 2003;113:1844–1856. doi: 10.1097/00005537-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Singh M, Rai A, Bandyopadhyay S, Gupta SC. Comparative study of underlay and overlay techniques of myringoplasty in large and subtotal perforations of the tympanic membrane. J Laryngol Otol. 2003;117:444–448. doi: 10.1258/002221503321892262. [DOI] [PubMed] [Google Scholar]
- 9.Wullstein HL. Past and future of tympanoplasty. Arch Otolaryngol. 1963;78:371. doi: 10.1001/archotol.1963.00750020381021. [DOI] [PubMed] [Google Scholar]
- 10.Glasscock ME, Jackson CG, Schwaber MK, et al. Post auricular undersurface tympanic membrane grafting: a follow up report. Laryngoscope. 1982;92:718–727. doi: 10.1288/00005537-198207000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Neumann A, Schultz-Coulon HJ, Jahnke K. Type III tympanoplasty applying the palisade cartilage technique: a study of 61 cases. Otol Neurotol. 2003;24(1):33–37. doi: 10.1097/00129492-200301000-00008. [DOI] [PubMed] [Google Scholar]


