Abstract
Background
The use of a highly conforming, anterior-stabilized bearing has been associated with clinical success in a limited number of studies.
Questions/purposes
We compared Knee Society scores, radiographic results, complication rates, and revision rates with the use of anterior-stabilized bearings compared with cruciate-retaining (CR) bearings.
Methods
A series of 382 patients with 468 primary total knee arthroplasties (TKAs) between 2003 and 2008 with minimum 2-year followup were reviewed. Anterior-stabilized bearings comprised 49% (n = 228) of the sample and CR bearings consisted of 51% (n = 240). The decision to use an anterior-stabilized bearing was based on integrity of the posterior cruciate ligament (PCL) intraoperatively or after sacrifice of the PCL to achieve soft tissue balance. The tibial and femoral component designs were the same regardless of bearing choice. Outcomes were measured with Knee Society scores, complications, revision TKA, and survival. Radiographs were analyzed for component alignment and evidence of loosening.
Results
There was no difference in Knee Society knee scores, radiographic alignment, component loosening, manipulation rate, major complications, or time to revision for patients between the two groups. However, the CR group had significantly more revisions than the anterior-stabilized group (21 CR [1.5%] versus seven anterior-stabilized [4.6%], p = 0.03) at a minimum followup of 5 months (mean, 42 months; range, 5–181 months).
Conclusions
The use of a highly congruent anterior-stabilized bearing for PCL substitution has comparable clinical and radiographic results to traditional CR TKA. These results suggest that this approach is an effective method to achieve stability without the PCL in primary TKA.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
TKA is a reliable operation for reducing pain and improving function. This has largely remained true even in the face of multiple surgical approaches, a dizzying array of implant choices, and a multitude of perioperative care regimens. One of the ongoing debates concerns the management of the posterior cruciate ligament (PCL). The PCL is the primary restraint to posterior translation of the tibia throughout the full range of knee flexion, and it is believed to be the primary stabilizer of the knee [7]. There are a number of possible strategies for managing the PCL in TKA, including retention of the PCL or PCL substitution. Arguments have been advanced in support of retention or substitution based on theoretical, in vivo and in vitro kinematic analyses, and clinical outcome data with very little consensus [20].
Proponents of PCL retention (cruciate-retaining [CR]) assert that PCL retention preserves more normal knee kinematics, is associated with fewer patellar complications, reduces shear forces at the bone-tibial implant interface, and that the PCL has an important proprioceptive function [3, 6, 9, 15]. Despite these proposed benefits, retention is not always an option and substitution of the PCL may be either required or preferred. PCL substitution in primary TKA has traditionally relied on a cam and post (cam-post) mechanism in the form of a posterior-stabilized (PS) design. Short- and long-term evaluations of PS and CR knees have failed to show clinically significant differences in their outcomes [2, 11, 12, 17–21].
In the past 20 years, the use of a highly conforming TKA bearing with an elevated anterior lip (anterior-stabilized) has emerged as an innovation for PCL substitution with favorable results in relatively few published reports compared with the existing body of literature on CR or PS designs [1, 8, 10, 14, 16]. Reported advantages for the use of the anterior-stabilized design include ease and speed of conversion to substitute for the PCL deemed incompetent or poorly balanced during the placement of a modular CR knee design, bone preservation resulting from the lack of need to resect intercondylar notch bone from the femur to accommodate the box of the PS design, eliminating cam-post impingement and the potential wear sequelae of that mechanism, further reducing the potential for patellar clunk, and potentially decreasing wear related to the high contact forces over small contact areas seen in flat-on-flat designs [8, 14]. Given these advantages and favorable published results, for nearly 7 years, we have used anterior-stabilized bearings exclusively when the PCL is deemed intraoperatively incompetent or unable to be balanced. Our anecdotal clinical observations have revealed no difference in CR knees and anterior-stabilized knees during this time period.
To more fully investigate the clinical performance of anterior-stabilized bearings as compared with CR bearings, we compared the Knee Society scores, radiographic results, complication rates, revision rates, and survival with the use of anterior-stabilized bearings compared with CR bearings.
Patients and Methods
After receiving exemption from the institutional review board, we reviewed a consecutive series of 914 TKAs in 741 patients. Four hundred thirty-two knees had less than 2-year minimum followup and were not included in this analysis; however, those who underwent revision TKA before the 2-year followup (n = 14 knees; 10 CR, four anterior-stabilized) were included in the analysis. Given that failure was determined after the variables were collected, we chose a cohort study design. Thirteen patients (14 knees) died before 2-year followup, maintaining the original TKA, and were excluded. Two patients (three knees) died after at least 2 years of followup, maintaining the original TKA, and were included in the analysis. No patients died as a result of their index TKA. This resulted in 382 patients with 468 knees for review. The data were analyzed at a minimum followup of 5 months (mean, 42 months; range, 5–181 months); followup periods of less than 2 years were permitted, again, only to allow us to capture early failures in both groups. No patients in the study group were lost to followup. All patients had undergone primary TKA with either an anterior-stabilized bearing (49%, n = 228) or a CR bearing (51%, n = 240) between 2003 and 2008. There were significantly more (p = 0.005) females (n = 305) than males (n = 163). The groups were comparable in regard to age, body mass index, and primary diagnosis (Table 1).
Table 1.
Patient characteristics
| Patient characteristic | AS group (n = 228) | CR group (n = 240) | p value |
|---|---|---|---|
| Age (years) | |||
| Mean ± SD | 62 ± 11 | 62 ± 10 | 0.89 |
| Range | 23–82 | 23–86 | |
| BMI (kg/m2) | |||
| Mean ± SD | 31.7 ± 7.9 | 33.3 ± 8.8 | |
| Range | 17.7–87.9 | 17.7–79.5 | 0.94 |
| Primary diagnosis | |||
| Osteoarthritis, number (%) | 201 (88%) | 215 (90%) | 0.91 |
AS = anterior-stabilized; CR = cruciate-retaining; BMI = body mass index.
All TKAs were performed through a medial parapatellar approach with a single FDA-approved implant type (Biomet, Warsaw, IN, USA). The goal for coronal alignment was 5° valgus (anatomic axis) and 0° mechanical axis. The tibia cut was neutral to the mechanical axis in the coronal plane and with 3° to 5° of posterior slope using an extramedullary guide. An initial medial release of the deep medial collateral ligament to the midsagittal line of the tibia was performed as part of the initial exposure. After bone preparation with measured resection bone cuts (posterior referencing), the symmetry of the flexion and extension gaps was investigated with trial components in place. Further medial, lateral, and PCL selective soft tissue release was performed to achieve balanced rectangular gaps [13]. Once trial implants were placed, the PCL was evaluated for both competence and balance. With the knee at 90° of flexion and the appropriate thickness modular trial CR polyethylene component in place, the PCL was deemed intact and balanced with a negative posterior drawer test and a tibiofemoral contact point at the middle of the tibial bearing. If these conditions were not satisfied, the PCL was deemed either incompetent or excessively tight. If the PCL was deemed competent and balanced, a CR tibial bearing with inherent 3° slope was chosen as the bearing surface. If the PCL was deemed incompetent or overly tight (requiring subsequent PCL recession or release), an anterior-stabilized bearing with 0° inherent posterior slope and 9 to 11 mm anterior lip (size-dependent) was chosen as the bearing surface. All patients had the same postoperative regimen and followup schedule.
Clinical outcomes were graded using the Knee Society Score (KSS), measured by clinicians other than the operating surgeon preoperatively, at 6 months and 1 year postoperatively and yearly thereafter. The last available KSS was used as the postoperative score for analysis. Radiographs were reviewed by the authors for assessment of the postoperative mechanical axis and radiolucent lines, according to the Knee Society Roentgenographic Evaluation System, at last followup. All 468 knees had preoperative, postoperative, and followup (6-week, 6-month, and yearly) radiographs including standing AP, longstanding AP, lateral, and sunrise views. Records were reviewed for both surgical and nonsurgical complications.
Complications were identified by chart review, which was performed by an individual not directly involved in the care of the patients (MA). The indications for manipulation under anesthesia during the period in question included failure to achieve 90° of flexion by 6 to 8 weeks postoperatively as evaluated and measured by the senior author (CLP).
Indications for revision for instability during the period in question included well-fixed, well-aligned TKA components on radiographs with symptomatic instability plus a positive posterior drawer sign on examination by the senior author (CLP) with the knee at 85° to 95° of flexion.
Statistical Methods
Because more than one knee was used from the same patient for 86 patients, the assumption of independence between the observations on knees was questionable. To check this assumption, a mixed effects logistic regression was fitted with TKA revision as the outcome and treatment group (anterior-stabilized bearings versus CR bearings) as the predictor with knees nested within patients as the random effect. In this model, the intraclass correlation coefficient (ICC) was quite large (ICC = 0.75), and the likelihood ratio test for the ICC was statistically significant (p = 0.009), demonstrating that the independence between observations was not met. Therefore, a mixed effects modeling approach was used for all statistical comparisons, which correctly accounted for the lack of independence. Additionally, Kaplan-Meier survival analysis was performed with failures defined as revision TKA (including polyethylene exchange). A log-rank analysis test was performed to assess for differences in survival between the groups. Data were analyzed using commercially available statistical software (STATA®; Statacorp, LP, College Station, TX, USA).
Results
Knee Society scores were comparable in the two groups (p = 0.29), and both groups improved after surgery. The mean improvement in KSS was 58 ± 53 in the anterior-stabilized group and 68 ± 50 in the CR group (Table 2).
Table 2.
Knee Society scores
| Knee Society Score | AS | CR | p value |
|---|---|---|---|
| Preoperative total, mean ± SD | 110 ± 32 | 108 ± 33 | 0.84 |
| Preoperative clinical | 52 ± 12 | 53 ± 18 | 0.60 |
| Preoperative functional | 58 ± 23 | 56 ± 22 | 0.51 |
| Postoperative total, mean ± SD | 168 ± 41 | 177 ± 31 | 0.19 |
| Postoperative clinical | 88 ± 19 | 92 ± 10 | 0.13 |
| Postoperative functional | 81 ± 27 | 85 ± 23 | 0.33 |
| Mean improvement, mean ± SD | 58 ± 53 | 68 ± 50 | 0.29 |
AS = anterior-stabilized; CR = cruciate-retaining.
Radiographic review showed no difference between the groups with postoperative mechanical axis (p = 0.30) or postoperative anatomical axis (p = 0.98). The mechanical axis was 0° ± 3° in the anterior-stabilized group and 0° ± 3° in the CR group (p = 0.30). The anatomical axis was −3° ± 3° in the anterior-stabilized group and −4° ± 3° in the CR group (p = 0.98). We also found no difference in progressive radiolucent lines (p = 0.99) or loosening (p = 0.36) between the groups.
There were no differences in nonsurgical complications between the groups (p = 0.92) or in manipulations under anesthesia to treat knee stiffness (p = 0.76) (Table 3). There was one reoperation in the anterior-stabilized group for arthroscopic débridement of a loose body and one in the CR group (p = 0.21), which was irrigation and débridement for infection.
Table 3.
Complications and revisions
| Variable | AS group | CR group | p value |
|---|---|---|---|
| Nonsurgical complications,* number (%) | 11 (4.58%) | 11 (4.82%) | 0.92 |
| Deaths | 2 (0.83%) | 1 (0.44%) | 0.75 |
| Manipulations, number (%) | 3 (1.32%) | 4 (1.67%) | 0.76 |
| Reoperations, number (%) | 1 (0.44%) | 1 (0.42%) | 0.97 |
| Revision TKA, number (%) | 7 (3.07%) | 21 (8.75%) | 0.03 |
| Septic | 5 (2.19%) | 7 (2.92%) | 0.67 |
| Aseptic | 2 (0.88%) | 14 (5.83%) | 0.01 |
| Instability | 0 | 6 | N/A |
| Loosening | 1 | 3 | |
| Patellofemoral problems | 1 | 1 | |
| Possible metal allergy | 0 | 1 | |
| Fracture | 0 | 1 | |
| Revised elsewhere | 0 | 2 |
* Nonsurgical complications include pulmonary embolism, deep vein thrombosis, cellulitis, cerebrovascular accident, aspiration pneumonia, death; AS = anterior-stabilized; CR = cruciate-retaining; N/A = not available.
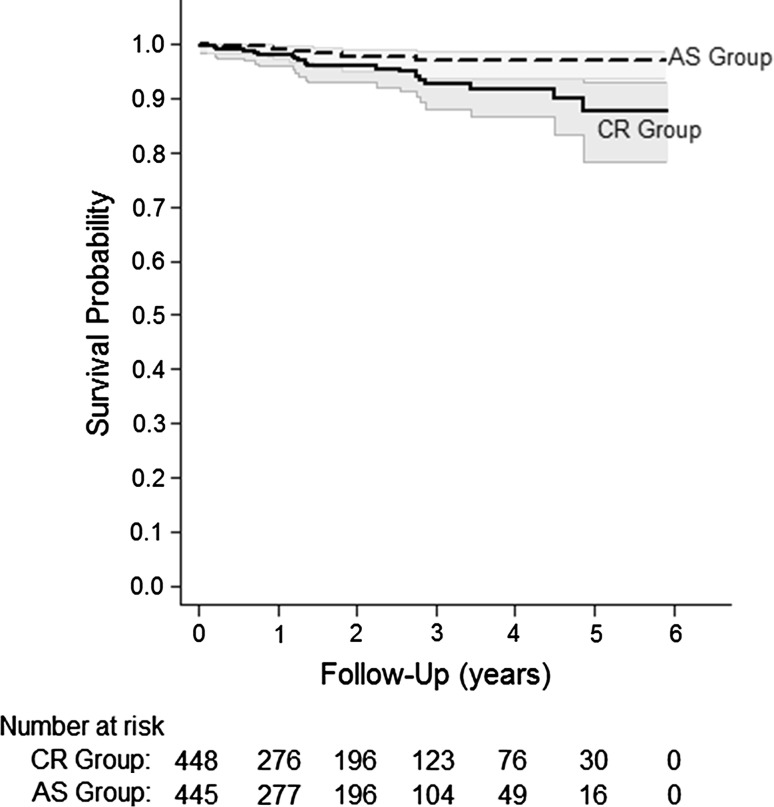
The log-rank analysis demonstrated significantly better survival at 5 years in the anterior-stabilized group (97% = anterior-stabilized, 88% = CR, p = 0.01) (Fig. 1). There were significantly more revisions in the CR group (n = 21) than the anterior-stabilized group (n = 7) (p = 0.03). There was no difference in septic failures between the groups (anterior-stabilized = 5, CR = 7, p = 0.67). However, there were significantly more aseptic failures in the CR group (n = 14) versus the anterior-stabilized group (n = 2) (p = 0.01). Instability (n = 6) was the primary reason for aseptic failure in the CR group, two of which were the result of PCL insufficiency at > 2.5 years (Table 3).
Fig. 1.
The Kaplan-Meier graph demonstrates the survival of the bearings in each group. AS = anterior-stabilized.
Discussion
The hypothesis of this article was an anterior-stabilized bearing performs comparably to a CR bearing using a single femoral component.
The debate regarding the optimal management of the PCL during primary TKA continues with options including cruciate retention, posterior substitution, or a deep-dished, highly conforming, ultracongruent anterior-stabilized design. Reported advantages of the anterior-stabilized design include ease of conversion from CR to PCL substitution, bone preservation, and the potential for improved wear characteristics resulting from the increased surface contact area and potentially decreased surface contact forces [8, 14]. Critics of anterior-stabilized bearings report their inability to restore normal knee kinematics and the potential to create a kinematic conflict [4, 5]. Few, although generally favorable, clinical outcomes have been reported in the literature with the use of the anterior-stabilized bearing designs [1, 8, 10, 14, 16]. We sought to compare anterior-stabilized TKAs with the cruciate-retaining approach, in terms of KSS, radiographic results, the frequency of complications (in particular manipulations for knee stiffness), revisions, and survival. We found comparable knee scores between the groups but better survival in the anterior-stabilized TKAs than in the CR knees.
This study has limitations inherent to a retrospective review. First is the issue of selection bias. The decision to use a CR versus anterior-stabilized bearing was made during surgery by the senior author (CLP), and although the assignment of patients into groups was made based on subjective evaluation of the competence of the PCL, there could potentially be other criteria used during the intraoperative decision-making process. The second limitation is the nonquantifiable nature of the soft tissue balancing protocol used for all knees in this study. The bearing choice was dependent on the senior surgeon’s interpretation of PCL integrity. If the PCL was found to be too lax, allowing subluxation with posterior stress, the anterior-stabilized bearing would be selected. Alternatively, if the PCL is found to be too tight/scarred and causing excessive femoral rollback during flexion, then it was sacrificed to ensure a better flexion profile. Although this was not a randomized selection of patients, we did review a consecutive series of all patients with greater than 2-year followup. It would not be possible to randomize this surgical procedure because the decision is based on the individual patient’s anatomy and stability. Even given this limitation, we had a remarkably even distribution between the two groups (49% versus 51%).
The third limitation is that although we included failures before minimum 2-year followup, we did not fully analyze the other patients with less than 2-year followup. However, our sample of patients with greater than 2-year followup provided a balanced sample of knees with anterior-stabilized and CR bearings. A post hoc power analysis (set at 80% power, alpha = 0.05) demonstrated 55% power for improvement in KSS (80% power would have required 417 knees in each group) and 5% power for complications (80% power would have required 9875 knees in each group to detect a difference of 0.2%). However, we had 100% power to detect a difference in radiographic loosening and revision rates between the two groups.
We found comparable knee scores and radiographic results between anterior-stabilized and CR TKAs. Hofmann et al. [8] retrospectively reviewed 53 primary and 47 revision PCL-substituting TKAs using an anterior-stabilized polyethylene insert with a mean 60-month followup period and compared their results with 100 age- and sex-matched patients who received TKA with a CR design. They found no significant difference between the two groups in regard to the modified Hospital for Special Surgery score or ROM. Laskin et al. [10] found favorable outcomes with the use of an anterior-stabilized bearing design in a prospectively randomized trial of 176 patients with osteoarthritis using either a posterior-stabilized bearing or a deep-dished, anterior-stabilized tibial bearing after PCL sacrifice and found no statistically significant difference in ROM, ascending or descending stairs, pain, KSS, or stability. Additionally, Sathappan et al. [14] retrospectively reviewed 114 TKAs using an anterior-stabilized bearing with a mean 8.3-year followup and demonstrated significantly improved ROM, WOMAC scores, and KSS [14]. Scott et al. reported similar clinical outcomes and no differences in the incidence of radiolucent lines when comparing anterior-stabilized inserts with posterior-lipped inserts. The fluoroscopic and kinematic arguments may in fact be moot as a result of the excellent clinical and radiographic outcomes achieved using anterior-stabilized bearings. At the present time, the literature suggests comparable clinical outcomes scores in patients receiving anterior-stabilized bearings during TKA [1, 8, 10, 14, 16].
We found no differences in the frequency of complications between the two groups, but we did identify that CR knees underwent revisions more frequently than did the anterior-stabilized TKAs, mainly related to instability. Hofmann et al. [8] found a similar higher incidence of revisions related to instability (five knees) in the CR group compared with no revisions resulting from instability in the anterior-stabilized group (zero knees). Sathappan et al. [14] similarly demonstrated good implant survival of 95% at 10 years with the use of an anterior-stabilized bearing design. In our study, revision TKA in the CR group was performed at a rate three times as often compared with the anterior-stabilized group (p = 0.03), and instability was the most common cause of revision in the CR group. Although this may illustrate a concern with the use of a CR bearing, it also suggests that the anterior-stabilized bearing affords adequate clinical stability in the setting of a deficient or absent PCL.
Although the debate over the optimal method of management of the PCL continues, we found comparable knee scores, radiographic findings, and fewer revisions with the use of an anterior-stabilized bearing when compared with a CR design. Because our study did not investigate potential longer-term issues such as polyethylene wear and detailed kinematic or functional analyses such as quadriceps force during stairclimbing, we are uncomfortable recommending the sole use of anterior-stabilized bearings based only on the results of this study. Anterior-stabilized bearings are attractive because they can be used with a CR femoral component design, enabling intraoperative flexibility to balance the knee without the need to make additional cuts or change the femoral component. Additionally, there is no need to cut a box in the femur to accept a PCL-substituting post, thus preserving femoral bone stock.
Acknowledgments
We thank David Evans for his contribution to this study.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Aigner C, Windhager R, Pechmann M, Rehak P, Engeleke K. The influence of an anterior-posterior gliding mobile bearing on range of motion after total knee arthroplasty. A prospective, randomized, double-blinded study. J Bone Joint Surg Am. 2004;86:2257–2262. doi: 10.2106/00004623-200410000-00018. [DOI] [PubMed] [Google Scholar]
- 2.Andriacchi TP, Galante JO. Retention of the posterior cruciate in total knee arthroplasty. J Arthroplasty. 1988;3:S13–S19. doi: 10.1016/S0883-5403(88)80003-2. [DOI] [PubMed] [Google Scholar]
- 3.Andriacchi TP, Galante JO, Fermier RW. The influence of total knee-replacement design on walking and stair-climbing. J Bone Joint Surg Am. 1982;64:1328–1335. [PubMed] [Google Scholar]
- 4.Daniilidis K, Skwara A, Vieth V, Fuchs-Winkelmann S, Heindel W, Stuckmann V, Tibesku CO. Highly conforming polyethylene inlays reduce the in vivo variability of knee joint kinematics after total knee arthroplasty. Knee. 2012;19:260–265. doi: 10.1016/j.knee.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 5.Dennis DA, Komistek RD, Colwell CE, Jr, Ranawat CS, Scott RD, Thornhill TS, Lapp MA. In vivo anteroposterior femorotibial translation of total knee arthroplasty: a multicenter analysis. Clin Orthop Relat Res. 1998;356:47–57. doi: 10.1097/00003086-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Ewald FC, Jacobs MA, Miegel RE, Walker PS, Poss R, Sledge CB. Kinematic total knee replacement. J Bone Joint Surg Am. 1984;66:1032–1040. [PubMed] [Google Scholar]
- 7.Harner CD, Xerogeanes JW, Livesay GA, Carlin GJ, Smith BA, Kusayama T, Kashiwaguchi S, Woo SL. The human posterior cruciate ligament complex: an interdisciplinary study. Ligament morphology and biomechanical evaluation. Am J Sports Med. 1995;23:736–745. doi: 10.1177/036354659502300617. [DOI] [PubMed] [Google Scholar]
- 8.Hofmann AA, Tkach TK, Evanich CJ, Camargo MP. Posterior stabilization in total knee arthroplasty with use of an ultracongruent polyethylene insert. J Arthroplasty. 2000;15:576–583. doi: 10.1054/arth.2000.6633. [DOI] [PubMed] [Google Scholar]
- 9.Kelman GJ, Biden EN, Wyatt MP, Ritter MA, Colwell CW Jr. Gait laboratory analysis of a posterior cruciate-sparing total knee arthroplasty in stair ascent and descent. Clin Orthop Relat Res. 1989;248:21–25; discussion 25–26. [DOI] [PubMed]
- 10.Laskin RS, Maruyama Y, Villaneuva M, Bourne R. Deep-dish congruent tibial component use in total knee arthroplasty: a randomized prospective study. Clin Orthop Relat Res. 2000;380:36–44. doi: 10.1097/00003086-200011000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Lozano-Calderon SA, Shen J, Doumato DF, Greene DA, Zelicof SB. Cruciate-Retaining vs posterior-substituting inserts in total knee arthroplasty: functional outcome comparison. J Arthroplasty. 2013;28:234–242.e1. [DOI] [PubMed]
- 12.Parsley BS, Conditt MA, Bertolusso R, Noble PC. Posterior cruciate ligament substitution is not essential for excellent postoperative outcomes in total knee arthroplasty. J Arthroplasty. 2006;21:127–131. doi: 10.1016/j.arth.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 13.Peters CL. Soft-tissue balancing in primary total knee arthroplasty. Instr Course Lect. 2006;55:413–417. [PubMed] [Google Scholar]
- 14.Sathappan SS, Wasserman B, Jaffe WL, Bong M, Walsh M, Di Cesare PE. Midterm results of primary total knee arthroplasty using a dished polyethylene insert with a recessed or resected posterior cruciate ligament. J Arthroplasty. 2006;21:1012–1016. doi: 10.1016/j.arth.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 15.Schultz RA, Miller DC, Kerr CS, Micheli L. Mechanoreceptors in human cruciate ligaments. A histological study. J Bone Joint Surg Am. 1984;66:1072–1076. [PubMed] [Google Scholar]
- 16.Scott RD, Thornhill TS. Posterior cruciate supplementing total knee replacement using conforming inserts and cruciate recession: effect on range of motion and radiolucent lines. Clin Orthop Relat Res. 1994;309:146. [PubMed] [Google Scholar]
- 17.Shoji H, Wolf A, Packard S, Yoshino S. Cruciate retained and excised total knee arthroplasty: a comparative study in patients with bilateral total knee arthroplasty. Clin Orthop Relat Res. 1994;305:218–222. [PubMed] [Google Scholar]
- 18.Tanzer M, Smith K, Burnett S. Posterior-stabilized versus cruciate-retaining total knee arthroplasty. J Arthroplasty. 2002;17:813–819. doi: 10.1054/arth.2002.34814. [DOI] [PubMed] [Google Scholar]
- 19.Udomkiat P, Meng B, Dorr LD, Wan Z. Functional comparison of posterior cruciate retention and substitution knee replacement. Clin Orthop Relat Res. 2000;378:192. doi: 10.1097/00003086-200009000-00029. [DOI] [PubMed] [Google Scholar]
- 20.Victor J, Banks S, Bellemans J. Kinematics of posterior cruciate ligament-retaining and -substituting total knee arthroplasty: a prospective randomised outcome study. J Bone Joint Surg Br. 2005;87:646–655. doi: 10.1302/0301-620X.87B5.15602. [DOI] [PubMed] [Google Scholar]
- 21.Wing CK, Kwok-Hing C. Sixteen years’ result of posterior-stabilized TKA. J Knee Surg. 2012;25:245–248. doi: 10.1055/s-0031-1299655. [DOI] [PubMed] [Google Scholar]