Abstract
Background
Kinematics vary, sometimes in important ways, among the different types of total knee arthroplasty (TKA) designs, yet differences between the in vivo mechanisms of cam-post engagement in rotating-platform posterior-stabilized (PS) TKA, bicruciate-stabilized TKA, and fixed-bearing PS TKA designs remain largely uncharacterized.
Questions/purposes
The objective of this study was to determine the cam-post mechanism interaction for subjects implanted with three different TKA designs.
Methods
In vivo, analysis was conducted for patients implanted with nine rotating-platform PS TKAs, five knees with a fixed-bearing PS TKA, and 10 knees with a bicruciate-stabilized TKA while performing a deep knee bend. Three-dimensional kinematics of the implant components were determined by analysis of fluoroscopic images during flexion. The distances between the interacting surfaces were measured throughout flexion and instances and locations of contact were identified.
Results
Seven of the 10 bicruciate-stabilized knees analyzed had the femoral component engaged with the anterior aspect of the tibial post at full extension. Posterior cam-post engagement occurred at 34° for the bicruciate-stabilized (range, 17°–68°), 93° for the fixed-bearing PS (range, 88°–100°), and at 97° (range, 90°–104°) for rotating-platform PS TKA. In bicruciate-stabilized and fixed-bearing PS knees, the contact initially occurred on the medial aspect of the posterior surface of the tibial post and then moved centrally and superiorly with increasing flexion. For rotating-platform PS TKA, it was located centrally on the posterior surface of the post at all times.
Conclusions
This study suggests that mobility of the polyethylene might play an important role in ensuring central cam-post interaction in PS TKA. The polyethylene insert rotates axially in accordance with the rotating femur, maintaining central cam-post contact. This phenomenon was not observed in the fixed-bearing PS TKAs analyzed in this study.
Clinical Relevance
We speculate that this centralized symmetrical contact between the cam and posterior surface of the post could be beneficial clinically in terms of reducing wear of the posterior surface and particularly at the medial extremes of it.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
TKAs in general have provided good mid- to long-term survivability. However, the question on which type of implant configuration provides the best postsurgery outcomes is still a cause for debate [7]. One area of contention is whether the posterior cruciate ligament should be retained or substituted. Proponents of the cruciate-retaining design have suggested that the posterior femoral rollback seen in posterior-stabilized (PS) TKAs is the result of the “guided motion” provided by the cam-post engaging. During gait, fixed-bearing and rotating-platform/mobile-bearing PS TKA designs have experienced similar kinematic patterns as those designs that lacked a cam and post mechanism [5]. This has been attributed to the fact that the cam and post mechanism of most PS TKA designs do not engage during lesser flexion activities such as gait. During a deep knee bend, however, PS TKA designs typically show greater posterior femoral rollback than designs without a cam and post mechanism [5, 6, 17].
Few studies have been conducted that quantify the function of the cam-post engagement mechanism in PS TKAs [2, 3, 24]. Banks et al. [2] reported the minimum distance between the cam and post as a function of flexion in five knees with a primary fixed-bearing PS TKA. That study estimated cam-post engagement to occur at 40° of flexion during a stepup maneuver. Suggs et al. [24] investigated the flexion range at which cam-post engagement occurred during a lunge activity for 24 patients undergoing fixed-bearing PS TKA in vivo. They reported average contact angle of 91.1° with a range from 69° to 114°. Both of these studies were conducted on fixed-bearing TKAs and the effect of a mobile polyethylene insert on cam-post engagement has not yet been analyzed.
Another area of contention has been bearing mobility. The rotating-platform implant was designed to reduce contact stress, thereby reducing wear, and recreate more normal-like knee kinematics. In vitro studies have shown reduced wear with the use of a rotating-platform implant [9, 10]. However, kinematics, clinical outcomes, and survivability between fixed- and mobile-bearing implants have produced similar results in some studies [13, 19, 21].
Hence, the objective of this study was to analyze the in vivo cam-post engagement mechanism in three different types of PS TKA designs. The analysis was conducted to determine four aspects of cam-post interaction during deep knee bend activity: (1) the flexion angle at which cam-post contact first occurs; (2) the cam-post distance throughout flexion; (3) the location on the posterior surface of the tibial post where contact occurs through flexion; and (4) the height of the contact of the femoral cam on the tibial post.
Patients and Methods
The patients selected for this study were part of three different kinematic studies conducted at The University of Tennessee–Knoxville. All subjects had well-functioning TKAs and were judged clinically successful (Hospital for Special Surgery knee scores > 90) with no ligamentous laxity or pain. Internal review board approval was obtained from each institution involved in the data collection process, and informed consents were obtained for all the patients in the three studies.
Eight patients (nine TKAs) implanted with a PFC Sigma rotating-platform PS TKA (DePuy Inc, Warsaw, IN, USA) (rotating-platform PS group), five patients (five TKAs) implanted with a NexGen LPS-Flex fixed-bearing PS TKA (Zimmer Inc, Warsaw, IN, USA) (fixed-bearing PS group), and nine patients (10 TKAs) implanted with the Journey bicruciate-stabilized TKA (Smith & Nephew Inc, Memphis, TN, USA) (bicruciate-stabilized group) were selected. The bicruciate-stabilized implant is designed to resect the ACL and PCL and provide both anterior (anterior femoral cam/tibial post interaction) as well as posterior (posterior femoral cam/tibial post interaction) stabilization. All three TKA groups were implanted by different surgeons with each set of TKAs being implanted by the same surgeon. The age of the patients and postoperative times were kept as close to equal as possible (Table 1). This was done to create a more controlled data set during analysis.
Table 1.
Demographic information for all subjects in the three groups
| Group | Number of subjects | Number of TKAs | Age (years) |
|---|---|---|---|
| RP-PS group | 8 | 9 | 68.0 (SD = 6.9) |
| FB-PS group | 5 | 5 | 69.2 (SD = 10.5) |
| BCS group | 9 | 10 | 67.1 (SD = 8.9) |
RP-PS = rotating-platform posterior-stabilized; FB-PS = fixed-bearing posterior-stabilized; BCS = bicruciate-stabilized.
Each patient was asked to perform a series of successive weightbearing deep knee bend cycles on the implanted knee while under fluoroscopic surveillance. The fluoroscopic images were stored on videotape for subsequent redigitization and analysis using a frame grabber. For each patient, images from full extension to maximum flexion at increments of 10° of flexion were used for the analysis.
In the case of the rotating-platform PS polyethylene inserts, the three-dimensional (3-D) orientation of the radiolucent bearing was determined by identification of four metallic beads that had been embedded in the component at specified locations during the manufacturing process. Because three noncollinear points are needed to define a rigid body’s spatial orientation, the four beads were inserted out of plane and as far away from one another as possible without compromising the integrity of the insert. This increases the probability that at least three of the beads are visualized during fluoroscopy.
The 3-D solid models for all the implant components were obtained from the respective manufacturers. Subsequent 3-D solid models of the polyethylene component having the strategically positioned beads were also created. Using a previously published three-dimensional-to-two-dimensional (2-D) registration technique [16], 3-D implant orientations of the TKA implant components were determined for the individual fluoroscopic frames at specified degrees of flexion for the deep knee bend activity. The images were projected onto the image plane with the corresponding implant models added to the scene. Initially, the 3-D orientations of the femoral and tibial components are positioned by the operator manipulating the 3-D solid models into a position closely corresponding with their respective silhouettes in the digitized fluoroscopic image. Then the automated computer algorithm used a simulated annealing technique to determine the best orientation of the models. To determine the 3-D orientation of the polyethylene component, the polyethylene insert was made transparent, which resulted in only the embedded beads within the 3-D solid model being visible. The bead portion of the polyethylene insert was then matched to the fluoroscopic silhouettes of the embedded beads (Fig. 1). Once complete, the full orientation of the polyethylene insert could be determined.
Fig. 1.

Fluoroscopy image shown with femoral and tibial 3-D solid models of rotating-platform PS TKA and four visible bead silhouettes that allow for proper positioning of polyethylene bearing when silhouettes match.
In the case of the fixed-bearing PS and bicruciate-stabilized TKAs, the polyethylene insert was fixed to the metallic tibial tray and no relative motion was assumed to occur between the tibial tray and the insert. To achieve the correct 3-D orientation, the polyethylene 3-D solid model was centered to the tibial 3-D solid model in both the AP and mediolateral directions before the overlay process.
The correct fit for each of the models was achieved when the silhouettes of the femoral and tibial components and the beads embedded (only for rotating-platform PS group) in the polyethylene bearing best matched their corresponding components in the fluoroscopic image. Once the 3-D-to-2D registration technique was completed, the 3-D implant orientations were imported into an in-house-developed analysis software. This package developed in MATLAB (Mathworks©, Natick, MA, USA) enabled further determination of kinematic parameters of interest at the tibiofemoral and cam-post interface of the TKA implant components. Using this package, the analysis to determine the cam-post contact was carried out.
Initially, the mesh size of the femoral cam and the tibial post was imported into a meshing software (HyperMesh, Troy, MI, USA) and the mesh size pertaining to those areas was refined to contain approximately 10,000 tetrahedral elements. The refined models were then reintroduced into the analysis software and the contact between the cam and the post was determined. This was done by designating the femoral cam and the tibial post parts of the models as separate surfaces. The contact algorithm of the analysis software package was executed to determine the distance between the corresponding polyethylene and femoral surfaces. This analysis was conducted for every degree of flexion from full extension to maximum knee flexion. This was achieved by interpolating the 3-D kinematic data using a 6° spline interpolation technique to determine the kinematics for flexion angles not included in the fluoroscopic analysis. A distance of less than 0.5 mm was considered to signify contact between the femoral condyle and the polyethylene insert. The center of this area was assigned as the contact location (on both the surfaces) and the flexion angle at which contact was first determined was assigned as the cam-post contact angle (Fig. 2).
Fig. 2.
Cam-post contact determination for a sample patient in the rotating-platform PS group exhibits a typical result of the contact analysis conducted to determine cam-post contact.
Once this analysis was completed, four parameters are determined: (1) cam-post contact angle; (2) distance between the femoral cam and the tibial post throughout the deep knee bend activity (Fig. 3); (3) height of the contact point on the tibial post with respect to the medial tibiofemoral contact point; and (4) height of the contact point on the tibial post with respect to the lateral tibiofemoral contact point (Fig. 4).
Fig. 3.

Cam-post distance determination for a sample patient in the rotating-platform PS group exhibits a typical result for distance calculation between the femoral cam and the posterior surface of the tibial post.
Fig. 4.
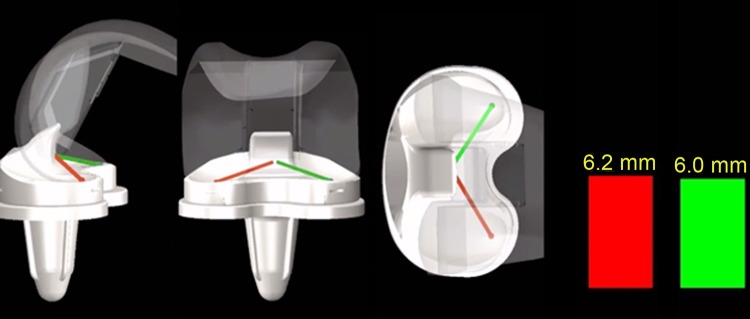
Cam-post height of contact determination for a sample patient in the rotating-platform PS group exhibits a typical result for contact height calculation on the posterior surface of the tibial post.
A post hoc power analysis conducted on the chosen sample size revealed 0.81 power for determining difference in distances of 2 mm and 0.76 power for angles for determining a difference of 5° for flexion angle measurements using a significance criteria of 0.05. Statistical significance of 95% was determined using a nonparametric Tukey-Kramer honestly significant difference pairwise comparison test.
Results
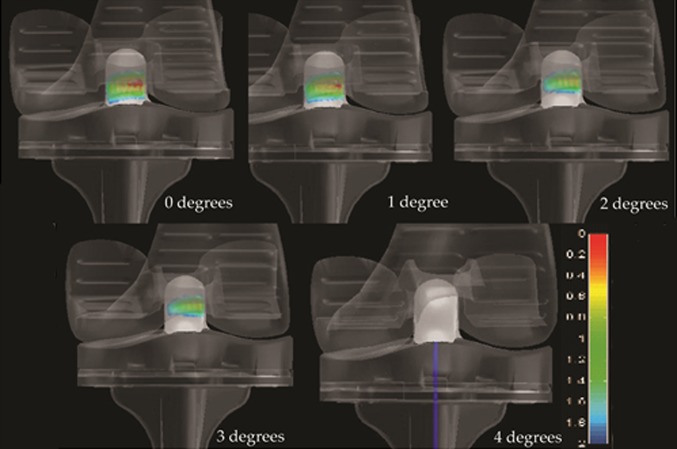
Cam-post contact occurred at a lower flexion angle for the bicruciate-stabilized group when compared with the fixed-bearing PS group (p < 0.001) as well as the rotating-platform PS group (p < 0.001), which was found to be statistically significant. There was no difference between patients in the fixed-bearing PS and rotating-platform PS groups (p = 0.765). There were two knees in the bicruciate-stabilized group and one knee in the rotating-platform PS group that did not exhibit cam-post engagement through their ROM. For the patients in the bicruciate-stabilized group, seven of 10 knees analyzed had the femoral component engaged with the anterior aspect of the tibial post at full extension (Fig. 5). However, the contact between them was lost in very early flexion (average, 4.9°; range, 0.0°–9.9°). When the posterior cam-post mechanism was analyzed for the three groups, it was seen that the engagement occurred at 34° for the bicruciate-stabilized (range, 17°–68°), 93° for the fixed-bearing PS (range, 88°–100°), and 97° (range, 90°–104°) for rotating-platform PS TKA.
Fig. 5.
Anterior cam-post contact was evaluated for a sample patient in the bicruciate-stabilized group depicting loss of contact at early flexion.
The effect of the initial dwell point of the femur on the polyethylene insert played a major role in determining when cam-post contact occurred. The subjects in the bicruciate-stabilized group experienced a lower cam-post distance than their fixed-bearing PS (p < 0.001) and rotating-platform PS (p = 0.003) counterparts, which was found to be statistically significant. There was no significant difference between the fixed-bearing PS and rotating-platform PS TKA groups (p = 0.693). The average distance between the cam and the posterior aspect of the post at full extension was 9.3 mm (range, 5.5–11 mm) for the bicruciate-stabilized group, 19.1 mm (range, 13–23 mm) for the fixed-bearing PS group, and 17.3 (range, 14–21 mm) for the rotating-platform PS group.
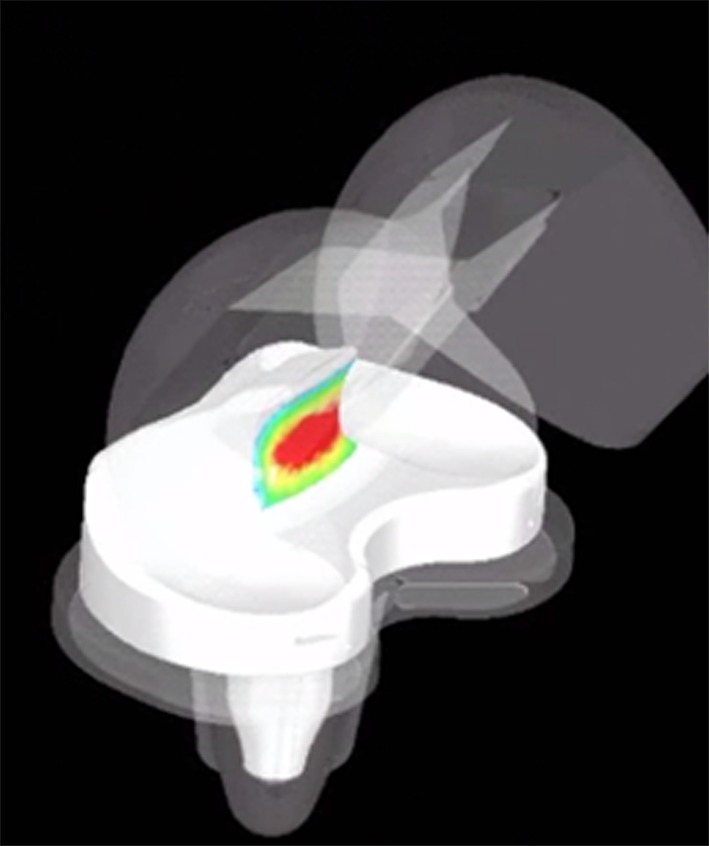
The anterior contact in the bicruciate-stabilized group was always located centrally on the anterior aspect of the tibial post. As far as the posterior contact was concerned, in the bicruciate-stabilized (Fig. 6) and fixed-bearing PS knees, the contact initially occurred toward the medial aspect of the posterior surface of the tibial post and then gradually moved centrally and superiorly with increasing flexion, whereas for the rotating-platform PS TKA, it was located centrally on the post at all times (Fig. 7). The amount of medialization of the contact in the bicruciate-stabilized and fixed-bearing PS groups was found to correlate with the amount of tibiofemoral axial rotation experienced by the patient with patients experiencing higher axial rotation having a higher tendency to demonstrate medial contact at the tibial post interface.
Fig. 6.
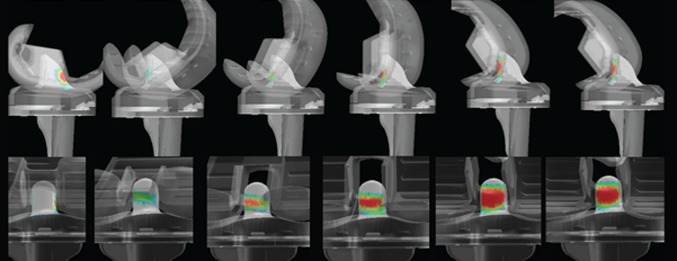
Evaluation of posterior cam-post contact for a sample patient in the bicruciate-stabilized group depicts a medialized contact point, which then moves posteriorly and superiorly with increasing flexion.
Fig. 7.

Evaluation of the cam-post interaction for a sample patient in the rotating-platform PS group exhibits central contact on the tibial post through flexion.
The height at which the contact occurred on the posterior aspect of the post was variable among the three groups. The bicruciate-stabilized group experienced contact higher on the tibial post from either the medial tibiofemoral contact point or the lateral tibiofemoral contact point (average, 12.5 mm; range, 7.0–18.5 mm) than their fixed-bearing PS (average, 7.2 mm; range, 6.1–10.0 mm) (p = 0.02) and rotating-platform PS (average, 6.2; range, 3.0–11 mm) (p = 0.009) counterparts. There was no statistical difference on the cam-post contact height between the fixed-bearing PS and rotating-platform PS groups (p = 0.792).
Discussion
Multiple studies [4–6, 12, 14, 22, 23, 26] have demonstrated the kinematic performance of cruciate-retaining and PS-type TKA designs. Also, other studies [11, 17, 18, 20, 25, 27] have investigated the kinematic efficacy of a mobile polyethylene when compared with a fixed-bearing device. However, limited data exist investigating the various aspects pertaining to the cam-post interaction and the role bearing mobility plays in terms of cam-post mechanics. The present study investigates the cam-post mechanism in three different types of PS TKA and demonstrates the differences in terms of contact angle, location of the contact on the tibial post, and height of cam-post contact between the devices. In the three types of TKAs analyzed, we found that the bicruciate-stabilized TKA experienced lower contact angles, lower cam-post distance through flexion, and higher height of contact on the tibial post when compared with the fixed-bearing PS and rotating-platform PS TKAs. Also, the location of contact on the tibial post was located centrally on the post for the rotating-platform TKA while moved from the medial aspect of the tibial post to the center of the tibial post with increasing flexion in both of the fixed-bearing TKA designs.
Although this study is the first to our knowledge to compare cam-post interaction between fixed- and mobile-bearing TKAs, it does have some limitations. First, the sample size of the study is small. Despite the small sample size, the findings of this study clearly demonstrate the differences in the three groups of TKAs and are a good first indicator of trends among the groups. Second, the patients chosen were operated on by different surgeons and does not account for surgeon variability. Third, the effect of knee side of implantation, the differences between the femoral box and tibial post designs among the three TKA designs, differently sized implants within each TKA design, and mismatched tibial and femoral sizes for certain patients on cam-post engagement was not conducted in this study. Also, this study was conducted on a single TKA design for each of the rotating-platform PS, fixed-bearing PS, and bicruciate-stabilized designs. Lastly, the cam-post engagement mechanism was estimated by using a single-plane fluoroscopy unit with a 3-D-to-2-D registration technique and 3-D solid models provided by the device manufacturers. The single-plane fluoroscopy technique, although accurate, does have an inherent error in the submillimeter range. The implant components (especially the polyethylene insert) do not take into account wear patients may have experienced postsurgery.
Numerous kinematic evaluations have found larger magnitudes of posterior femoral rollback in native knees when compared with TKAs [5, 8, 15]. To replicate normal knee kinematics in TKAs, and to facilitate higher ROM postsurgery, implant manufacturers have used various philosophies. One of the commonly used configurations of TKA in the market today uses a cam-post mechanism to engage in midflexion and facilitate posterior femoral rollback to achieve higher flexion. Early cam-post engagement is not ideal, because it would mean that engagement would occur during every cycle of common-day activities (eg, walking) not requiring high flexion and increase the possibility of early tibial post wear. The present study found that the average cam-post contact for the bicruciate-stabilized TKA was 34°. This may increase the possibility for cam-post engagement to occur frequently during daily activities for this TKA design.
Studies conducted to evaluate the cam-post interaction in fixed-bearing PS TKA designs during common daily activities have exhibited cam-post engagement angles ranging from 40° during a stepup maneuver to 91° during lunge activities [2, 24]. A study conducted by Catani et al. [3] on five bicruciate-stabilized TKAs revealed anterior cam-post engagement to occur only in early flexion, whereas posterior cam-post engagement occurred at approximately 63°, 58°, and 50° during the chair-rise, stepup, and stepdown activities, respectively. The current study suggests similar results for the two PS-type designs with cam-post engagement occurring at 93° and 97° for the fixed-bearing PS and rotating-platform PS groups, respectively. However, the bicruciate-stabilized group experienced an average of 34° during the deep knee bend activity, which is contrary to that reported by Catani et al. The difference between the two studies is crucial because early cam-post interaction reported in this study could give rise higher tibial post wear.
Polyethylene design also plays an important role in determining the cam-post engagement. Designs that incorporate an anteriorized dwell point at full extension reduce the initial cam-post distance, thereby increasing the possibility of early cam-post engagement. This seems to explain the early engagement angle experienced by the subjects in the bicruciate-stabilized group. Among all three groups analyzed, the bicruciate-stabilized group experienced the most anterior tibiofemoral contact points at full extension (Table 2). The fixed-bearing PS and rotating-platform PS groups experienced a contact point that was posterior to the midline of the tibial component. This ensured a larger distance between the femoral cam and tibial post, thereby ensuring late cam-post interaction. Although the anterior location of the tibiofemoral contact point is desirable, because it mimics the normal knee, this study suggests that it could have a negative impact on cam-post interaction by forcing early cam-post interaction. This in turn may lead to abnormal tibial post wear. One subject in the rotating-platform PS group did not experience cam-post engagement. However, this patient exhibited a lower maximum knee flexion (86°) than the average cam-post contact angle (97°) for this group.
Table 2.
Tibiofemoral contact point location at full extension for patients in the three groups
| Group | Full extension (mm) | |||||
|---|---|---|---|---|---|---|
| Lateral AP contact | Medial AP contact | |||||
| Average | Range | SD | Average | Range | SD | |
| RP-PS group | −5.7 | −8.7 to −2.2 | 2.0 | −5.3 | −7.2 to −3.0 | 1.4 |
| FB-PS group | −2.1 | −5.4 to 0.8 | 2.1 | −3.9 | −8.7 to −0.2 | 2.3 |
| BCS group | 4.6 | −3.0 to 18.4 | 8.0 | 6.6 | 3.9 to 9.4 | 1.6 |
RP = rotating-platform; PS = posterior-stabilized; FB = fixed-bearing; BCS = bicruciate-stabilized.
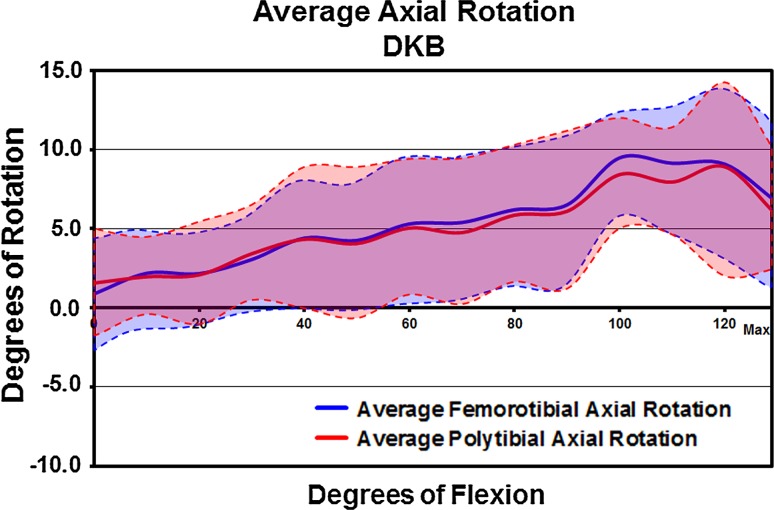
On the posterior cam-post interaction site, for the bicruciate-stabilized and fixed-bearing PS groups, the initial contact with the tibial post was achieved on the medial aspect of its posterior surface, before the contact area tended to move centrally and superiorly with increasing flexion. In the rotating-platform group, contact with the cam was located centrally rather than medially or laterally on the posterior surface of post during flexion. The polyethylene bearing did rotate axially with the femoral component (Fig. 8) consistent with design intent, and this probably helped keep the axis of the posterior cam and the posterior surface of the bearing post nearly parallel throughout flexion. We speculate that this centralized symmetrical contact between the cam and posterior surface of the post could be beneficial clinically in terms of reducing wear of the posterior surface and particularly at the medial extremes of it. This phenomenon was not observed in the fixed-bearing TKAs and may increase the chances of edge loading on the polyethylene, resulting in wear patterns on the post in the fixed-bearing group. However, there are no data in the present study to suggest a direct correlation between cam-post wear and edge contact seen in the fixed-bearing TKAs. Also, the potential benefit of the rotating-platform TKA must be weighed against the additional adverse consequences that could be encountered with use of a rotating-platform tibial component.
Fig. 8.
Tibiofemoral and polyfemoral rotation comparison for the patients in the rotating-platform PS group exhibits consistent rotation of the femoral component with polyethylene rotation. DKB = deep knee bend.
Another consideration in designing the cam-post interaction is the ability of the cam-post contact point to remain low on the tibial spine with increasing flexion. This provides greater stability by increasing the jump height and also reduces stress in the tibial post by introducing the cam-post force at a location of maximum material [1]. In the current study, the cam-post contact height for the bicruciate-stabilized TKA was statistically higher than the other two groups. For the fixed-bearing PS and rotating-platform PS groups, the contact occurred midspine and remained in the lower part of the tibial post. This finding suggests that the cam-post design for fixed-bearing PS and rotating-platform PS TKAs could result in lower cam-post stresses, thus reducing the chances for failure of the tibial post.
This is the first study to our knowledge to compare the cam-post interaction mechanics in three different types of PS-type TKAs. It suggests that the mobility of the polyethylene insert in the rotating-platform PS TKA ensures central contact on the tibial post during flexion. Also, the polyethylene design pertaining to the tibiofemoral interaction in the rotating-platform PS TKA as well as the fixed-bearing PS TKA ensures late cam-post contact, which is desirable to prevent excessive cam-post interaction. However, more research needs to be conducted to determine if the early contact seen in the bicruciate-stabilized TKA and the edge contact seen in the bi cruciate as well as the fixed-bearing PS TKA have any direct correlation with excessive polyethylene post wear.
Footnotes
One of the authors (RDK) certifies that he or a member of his immediate family has or may receive payments or benefits during this study period of an amount of USD 100,001 to USD 1,000,000 from DePuy Synthese Inc (Warsaw, IN, USA). One of the authors (FL) certifies that he or a member of his immediate family has or may receive payments or benefits during this study period of an amount of USD 10,001 to USD 100,000 from DePuy Synthese Inc. One of the authors (DAD) certifies that he or a member of his immediate family has or may receive payments or benefits during this study period of an amount of more than USD 100,001 from DePuy Synthese Inc.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocols for these previous studies, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation was also obtained.
This work was performed at the University of Tennessee, Knoxville, TN, USA.
References
- 1.Argenson JN, Scuderi GR, Komistek RD, Scott WN, Kelly MA, Aubaniac JM. In vivo kinematic evaluation and design considerations related to high flexion in total knee arthroplasty. J Biomech. 2005;38:277–284. doi: 10.1016/j.jbiomech.2004.02.027. [DOI] [PubMed] [Google Scholar]
- 2.Banks SA, Markovich GD, Hodge WA. In vivo kinematics of cruciate-retaining and -substituting knee arthroplasties. J Arthroplasty. 1997;12:297–304. doi: 10.1016/S0883-5403(97)90026-7. [DOI] [PubMed] [Google Scholar]
- 3.Catani F, Innocenti B, Belvedere C, Labey L, Ensini A, Leardini A. Articular contact estimation in TKA using in vivo kinematics and finite element analysis. Clin Orthop Relat Res. 2010;468:19–28. doi: 10.1007/s11999-009-0941-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cates HE, Komistek RD, Mahfouz MR, Schmidt MA, Anderle M. In vivo comparison of knee kinematics for subjects having either a posterior stabilized or cruciate retaining high-flexion total knee arthroplasty. J Arthroplasty. 2008;23:1057–1067. doi: 10.1016/j.arth.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 5.Dennis DA, Komistek RD, Colwell CE, Jr, Ranawat CS, Scott RD, Thornhill TS, Lapp MA. In vivo anteroposterior femorotibial translation: a multi-center analysis. Clin Orthop Relat Res. 1998;356:47–57. doi: 10.1097/00003086-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Dennis DA, Komistek RD, Mahfouz MR, Haas BD, Stiehl JB. Multicenter determination of in vivo kinematics after total knee arthroplasty. Clin Orthop Relat Res. 2003;416:37–57. doi: 10.1097/01.blo.0000092986.12414.b5. [DOI] [PubMed] [Google Scholar]
- 7.Dennis DA, Komistek RD, Scuderi GR, Zingde S. Factors affecting flexion after total knee arthroplasty. Clin Orthop Relat Res. 2007;464:53–60. doi: 10.1097/BLO.0b013e31812f785d. [DOI] [PubMed] [Google Scholar]
- 8.Dennis DA, Mahfouz MR, Komistek RD, Hoff W. In vivo determination of normal and anterior cruciate ligament-deficient knee kinematics. J Biomech. 2005;38:241–253. doi: 10.1016/j.jbiomech.2004.02.042. [DOI] [PubMed] [Google Scholar]
- 9.Fisher J, McEwen H, Tipper J, Jennings L, Farrar R, Stone M, Ingham E. Wear-simulation analysis of rotating-platform mobile-bearing knees. Orthopedics. 2006;29:S36–S41. [PubMed] [Google Scholar]
- 10.Fisher J, McEwen HM, Tipper JL, Galvin AL, Ingram J, Kamali A, Stone MH, Ingham E. Wear, debris, and biologic activity of cross-linked polyethylene in the knee: benefits and potential concerns. Clin Orthop Relat Res. 2004;428:114–119. doi: 10.1097/01.blo.0000148783.20469.4c. [DOI] [PubMed] [Google Scholar]
- 11.Haas BD, Komistek RD, Stiehl JB, Anderson DT, Northcut EJ. Kinematic comparison of posterior cruciate sacrifice versus substitution in a mobile bearing total knee arthroplasty. J Arthroplasty. 2002;17:685–692. doi: 10.1054/arth.2002.33550. [DOI] [PubMed] [Google Scholar]
- 12.Kanekasu K, Banks SA, Honjo S, Nakata O, Kato H. Fluoroscopic analysis of knee arthroplasty kinematics during deep flexion kneeling. J Arthroplasty. 2004;19:998–1003. doi: 10.1016/j.arth.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 13.Kim YH, Yoon SH, Kim JS. The long-term results of simultaneous fixed-bearing and mobile-bearing total knee replacements performed in the same patient. J Bone Joint Surg Br. 2007;89:1317–1323. doi: 10.1302/0301-620X.89B10.19223. [DOI] [PubMed] [Google Scholar]
- 14.Komistek RD, Mahfouz MR, Bertin KC, Rosenberg A, Kennedy W. In vivo determination of total knee arthroplasty kinematics: a multicenter analysis of an asymmetrical posterior cruciate retaining total knee arthroplasty. J Arthroplasty. 2008;23:41–50. doi: 10.1016/j.arth.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 15.Leszko F, Hovinga KR, Lerner AL, Komistek RD, Mahfouz MR. In vivo normal knee kinematics: is ethnicity or gender an influencing factor? Clin Orthop Relat Res. 2011;469:95–106. doi: 10.1007/s11999-010-1517-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahfouz MR, Hoff W, Komistek RD, Dennis DA. A robust method for registration of three-dimensional knee implant models to two-dimensional fluoroscopy images. IEEE Trans Med Imaging. 2003;22:1561–1574. doi: 10.1109/TMI.2003.820027. [DOI] [PubMed] [Google Scholar]
- 17.Mueller J, Komistek RD, Dennis DA. Kinematics of the implanted and non-implanted knee. In: Scott WN, editor. Insall & Scott Surgery of the Knee. 5. Philadelphia, PA, USA: Churchill Livingstone; 2012. [Google Scholar]
- 18.Pagnano MW, Trousdale RT, Stuart MJ, Hanssen AD, Jacofsky DJ. Rotating platform knees did not improve patellar tracking: a prospective, randomized study of 240 primary total knee arthroplasties. Clin Orthop Relat Res. 2004;428:221–227. doi: 10.1097/01.blo.0000148892.31464.81. [DOI] [PubMed] [Google Scholar]
- 19.Post ZD, Matar WY, van de Leur T, Grossman EL, Austin MS. Mobile-bearing total knee arthroplasty: better than a fixed-bearing? J Arthroplasty. 2010;25:998–1003. doi: 10.1016/j.arth.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 20.Ranawat AS, Rossi R, Loreti I, Rasquinha VJ, Rodriguez JA, Ranawat CS. Comparison of the PFC Sigma fixed-bearing and rotating-platform total knee arthroplasty in the same patient: short-term results. J Arthroplasty. 2004;19:35–39. doi: 10.1016/j.arth.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 21.Ranawat CS, Komistek RD, Rodriguez JA, Dennis DA, Anderle M. In vivo kinematics for fixed and mobile-bearing posterior stabilized knee prostheses. Clin Orthop Relat Res. 2004;418:184–190. doi: 10.1097/00003086-200401000-00030. [DOI] [PubMed] [Google Scholar]
- 22.Schmidt R, Komistek RD, Blaha JD, Penenberg BL, Maloney WJ. Fluoroscopic analyses of cruciate-retaining and medial pivot knee implants. Clin Orthop Relat Res. 2003;410:139–147. doi: 10.1097/01.blo.0000063565.90853.a4. [DOI] [PubMed] [Google Scholar]
- 23.Stiehl JB, Komistek RD, Dennis DA, Paxson RD, Hoff WA. Fluoroscopic analysis of kinematic after posterior-cruciate-retaining knee arthroplasty. J Bone Joint Surg Br. 1995;77:884–889. [PubMed] [Google Scholar]
- 24.Suggs JF, Hanson GR, Park SE, Moynihan AL, Li G. Patient function after a posterior stabilized total knee arthroplasty: cam-post engagement and knee kinematics. Knee Surg Sports Traumatol Arthrosc. 2008;16:290–296. doi: 10.1007/s00167-007-0467-9. [DOI] [PubMed] [Google Scholar]
- 25.Tamaki M, Tomita T, Watanabe T, Yamazaki T, Yoshikawa H, Sugamoto K. In vivo kinematic analysis of a high-flexion, posterior-stabilized, mobile-bearing knee prosthesis in deep knee bending motion. J Arthroplasty. 2009;24:972–978. doi: 10.1016/j.arth.2008.06.012. [DOI] [PubMed] [Google Scholar]
- 26.Victor J, Mueller JK, Komistek RD, Sharma A, Nadaud MC, Bellemans J. In vivo kinematics after a cruciate-substituting TKA. Clin Orthop Relat Res. 2010;468:807–814. doi: 10.1007/s11999-009-1072-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wasielewski RC, Komistek RD, Zingde SM, Sheridan KC, Mahfouz MR. Lack of axial rotation in mobile-bearing knee designs. Clin Orthop Relat Res. 2008;466:2662–2668. doi: 10.1007/s11999-008-0354-9. [DOI] [PMC free article] [PubMed] [Google Scholar]