Abstract
Background
Total knee arthroplasty (TKA) and related interventions such as revision TKA and the treatment of infected TKAs are commonly performed procedures. Hospital readmission rates are used to measure hospital performance, but risk factors (both medical and surgical) for readmission after TKA, revision TKA, and treatment for the infected TKA have not been well characterized.
Questions/purposes
We measured (1) the unplanned hospital readmission rate in primary TKA and revision TKA, including antibiotic-spacer staged revision TKA to treat infection. We also evaluated (2) the medical and surgical causes of readmission and (3) risk factors associated with unplanned hospital readmission.
Methods
This retrospective cohort study included a total of 1408 patients (1032 primary TKAs, 262 revision TKAs, 113 revision of infected TKAs) from one institution. All hospital readmissions within 90 days of discharge were evaluated for timing and cause. Diagnoses at readmission were categorized as surgical or medical. Readmission risk was assessed using a Cox proportional hazards model that incorporated patient demographics and medical comorbidities.
Results
The unplanned readmission rate for the entire cohort was 4% at 30 days and 8% at 90 days. At 90 days postoperatively, revision of an infected TKA had the highest readmission rate, followed by revision TKA, with primary TKA having the lowest rate. Approximately three-fourths of readmissions were the result of surgical causes, mostly infection, arthrofibrosis, and cellulitis, whereas the remainder of readmissions were the result of medical causes. Procedure type (primary TKA versus revision TKA or staged treatment for infected TKA), hospital stay more than 5 days, discharge destination, and a fluid/electrolyte abnormality were each associated with risk of unplanned readmission.
Conclusions
Patients having revision TKA, whether for infection or other causes, are more likely to have an unplanned readmission to the hospital than are patients having primary TKA. When assessing hospital performance for TKA, it is important to distinguish among these surgical procedures.
Level of Evidence
Level III, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
TKA is widely regarded as a beneficial and cost-effective treatment for osteoarthritis [15]. There were more than 600,000 TKAs performed in the United States in 2007 with costs exceeding USD 9 billion [21]. By 2009, the use of TKA had almost doubled from a decade earlier [3], and rates of both primary and revision TKA are expected to continue to increase exponentially during the next several decades [13]. Although considered a safe and effective procedure, complications associated with TKA can lead to poor outcomes [19]. As the population ages, more patients will have comorbid medical problems that may increase their risk of complications.
Unplanned hospital readmissions are expensive and an undesired outcome for the patient, the physician, and the healthcare system, yet have been found to occur in almost one in five Medicare patients [8]. Provisions in the Patient Protection and Affordable Care Act require reporting of hospital quality metrics along with financial accountability for underperforming hospitals [18]. Fully evaluating the cost-effectiveness of procedures requires measuring the cost over the continuum of care and must include readmissions related to an index event [17].
However, patients considering TKA may present with a wide range of age and comorbid medical conditions that may affect the likelihood of having an unplanned hospital readmission after surgery. Thus, it will be important for providers to identify patients at higher risk for such complications to minimize their occurrence and evaluate risk-stratified outcomes.
The primary objective of this study was to measure 90-day unplanned hospital readmission rates for patients undergoing TKA with the hypothesis that lower readmission rates would be seen for primary TKA, whereas higher readmission rates would be seen for revision TKA, with or without infection. Secondary objectives included characterizing the causes of and risk factors for unplanned readmission.
Patients and Methods
Patient Selection
All patients who underwent TKA between 2005 and 2011 at a single institution were identified using an administrative claims database with International Classification of Diseases, 9th Revision and Current Procedural Terminology codes for primary TKA (81.54, 27447), revision TKA (00.80–00.84, 81.55, 27486, 27487), and antibiotic spacer implantation/removal (84.56, 84.57, 27448). Patients were grouped by procedure type: (1) primary TKA; (2) revision TKA; and (3) infected TKA with staged implant removal, placement of cement-eluding antibiotic spacer, and finally revision TKA. There were no changes in indications or surgical or care pathways during the study time period. There were no uniform criteria for discharge timing and destination (eg, skilled nursing or inpatient rehabilitation requirements), and these decisions were made by the treating physician in consultation with our rehabilitation and case management departments.
Hospital Readmission
Hospital administrative claims data were used to identify any hospital readmission within 90 days of discharge from the initial TKA. All hospital readmissions underwent confirmatory medical record review and were categorized as planned if the readmission was predetermined at the time of the original procedure (eg, staged antibiotic spacer exchange for revision TKA) or unplanned. Causes of readmission were grouped as a surgical complication (infection, arthrofibrosis, cellulitis of extremity, venous thromboembolism, etc) or a medical complication (atrial fibrillation, myocardial infarction, pneumonia, etc). There were no uniform criteria for hospital readmission. Medical comorbidities were assessed using the Elixhauser comorbidity index as well as the All Payer Refined Diagnosis Related Group Severity of Illness scale (APR-SOI) [5, 7]. However, APR-SOI was not available for patients before 2007 and thus was not included in the multivariate analysis.
Patient Characteristics and Planned Readmissions
A total of 1408 patients met inclusion criteria for this study; 294 patients were excluded for insufficient followup (Table 1). There were 1032 patients who underwent primary TKA (912 unilateral, 120 bilateral), 262 who underwent revision TKA, and 113 who underwent revision for infected TKA. The average age was 63.2 ± 13.0 years and was similar between groups (Table 1). Patients in the primary TKA group were more often women than in the other two groups and were also more likely to require discharge to an inpatient rehabilitation center. Patients in the revision for infected TKA group had a longer hospital stay, more medical comorbidities, and were more likely to require discharge to a skilled nursing facility than were the primary or revision TKA groups. Patients who received revision TKA were less likely to have Medicaid insurance compared with patients receiving primary or revision for infected TKA, but otherwise there were no differences in payor source between groups.
Table 1.
Patient demographics
| Variable | Primary TKA | Revision TKA | Antibiotic spacer | p value |
|---|---|---|---|---|
| Total | 1032 | 262 | 113 | – |
| Age (years) | 63.6 ± 13.1 | 62.1 ± 12.9 | 62.9 ± 11.8 | 0.372 |
| Female | 653 (63.3%) | 147 (56.1%) | 61 (54.0%) | 0.027* |
| Insurance status | ||||
| Medicare | 427 (41.4%) | 114 (43.5%) | 49 (43.4%) | 0.781 |
| Private | 286 (27.7%) | 84 (32.1%) | 27 (23.9%) | 0.214 |
| Medicaid | 116 (11.2%) | 14 (5.3%) | 13 (11.5%) | 0.017* |
| Length of stay (days) | 4.2 ± 2.4 | 4.6 ± 2.5 | 8.3 ± 6.3 | 0.000* |
| Discharge to inpatient rehabilitation | 183 (17.7%) | 33 (12.6%) | 7 (6.2%) | 0.002* |
| Discharge to skilled nursing facility | 168 (16.3%) | 46 (17.6%) | 34 (30.1%) | 0.001* |
| All Payer Refined Severity of Illness | 1.55 ± 1.0 | 1.58 ± 1.0 | 2.04 ± 1.2 | 0.005* |
| Total comorbidities | 2.51 ± 2.0 | 2.78 ± 2.2 | 3.55 ± 2.7 | 0.000* |
Values are mean ± SD or numbers with percentages in parentheses; * statistical significance with p < 0.05.
The all-cause 90-day readmission rate was 13% (n = 176 of 1408) (Table 2). Six patients in the primary TKA group (0.6%) had a planned readmission for a contralateral primary TKA. There were 51 patients in the revision for infected TKA group (45%) who had planned readmissions for antibiotic spacer removal and revision TKA.
Table 2.
Demographics of readmitted and not readmitted patients
| Variable | Readmitted | Not readmitted | Odds ratio | SE | p value |
|---|---|---|---|---|---|
| Demographics | |||||
| Number | 118 | 1290 | – | – | – |
| Age (years) | 62.8 ± 12.4 | 63.3 ± 13.0 | 1.00 | 0.0 [1.0–1.0] | 0.656 |
| Female | 65 (55.1%) | 796 (61.7%) | 0.76 | 0.1 [0.5–1.1] | 0.159 |
| Insurance status | |||||
| Medicare | 54 (45.8%) | 536 (41.6%) | 1.19 | 0.2 [0.8–1.7] | 0.375 |
| Private | 25 (21.2%) | 372 (28.8%) | 0.66 | 0.2 [0.4–1.0] | 0.079 |
| Medicaid | 16 (13.6%) | 127 (9.8%) | 1.44 | 0.4 [0.8–2.5] | 0.203 |
| Surgical characteristics | |||||
| TKA group | |||||
| Primary TKA | 64 (6.2%) | 968 (93.8%) | – | – | – |
| Revision TKA (versus primary TKA) | 34 (13.0%) | 228 (87.0%) | 2.26 | 0.5 [1.5–3.5] | < 0.001* |
| Antibiotic spacer (versus primary TKA) | 20 (17.7%) | 93 (82.3%) | 3.25 | 0.9 [1.9–5.6] | < 0.001* |
| Length of stay over 5 days | 42 (35.6%) | 221 (17.1%) | 2.67 | 0.6 [1.8–4.0] | < 0.001* |
| Discharged to rehabilitation | 18 (15.3%) | 205 (15.9%) | 0.95 | 0.3 [0.6–1.6] | 0.856 |
| Discharged to skilled nursing facility | 34 (28.8%) | 214 (16.6%) | 2.04 | 0.4 [1.3–3.1] | 0.001* |
| Patient medical comorbidities | |||||
| All Payer Refined Severity of Illness (1–4) | 1.76 ± 1.1 | 1.58 ± 1.0 | 1.20 | 0.1 [1.0–1.4] | 0.061 |
| Osteoporosis | 7 (5.9%) | 41 (3.2%) | 1.92 | 0.8 [0.8–4.4] | 0.121 |
| Tobacco use | 36 (30.5%) | 344 (26.7%) | 1.21 | 0.3 [0.8–1.8] | 0.371 |
| Morbid obesity | 11 (9.3%) | 78 (6.1%) | 1.60 | 0.5 [0.8–3.1] | 0.166 |
| Total comorbidities | 3.21 ± 2.3 | 2.59 ± 2.1 | 1.14 | 0.0 [1.0–1.2] | 0.002* |
Values are mean ± SD or number with percentage in parentheses or range in brackets; * statistical significance at p < 0.05.
Statistical Analysis
Categorical variables were compared across groups using a chi-square test, whereas continuous variables were compared with a t-test with a p value < 0.05 considered statistically significant. Readmission within 90 days was measured using a Kaplan-Meier failure analysis and groups compared using a log-rank test with a p value < 0.05 deemed significant. Patients were censored after one hospital readmission to ensure that patients with multiple hospital readmissions did not excessively weight the results. Risk factors with a univariate p value of < 0.2 were included in a Cox proportional hazards model. Variables were removed stepwise if the p value in the multivariate model was > 0.1. Risk was reported with hazard ratios.
Results
Unplanned Readmission Rate
The overall unplanned readmission rate was 4% (n = 57 of 1408) at 30 days and 8% (n = 118 of 1408) at 90 days. Patients were readmitted from the emergency department (39.8%, n = 47 of 118), from the clinic or other direct admission (51.7%, n = 61 of 118), or transferred from an outside hospital (8.5%, n = 10 of 118). Unplanned readmissions required a surgical procedure in 42% of cases.
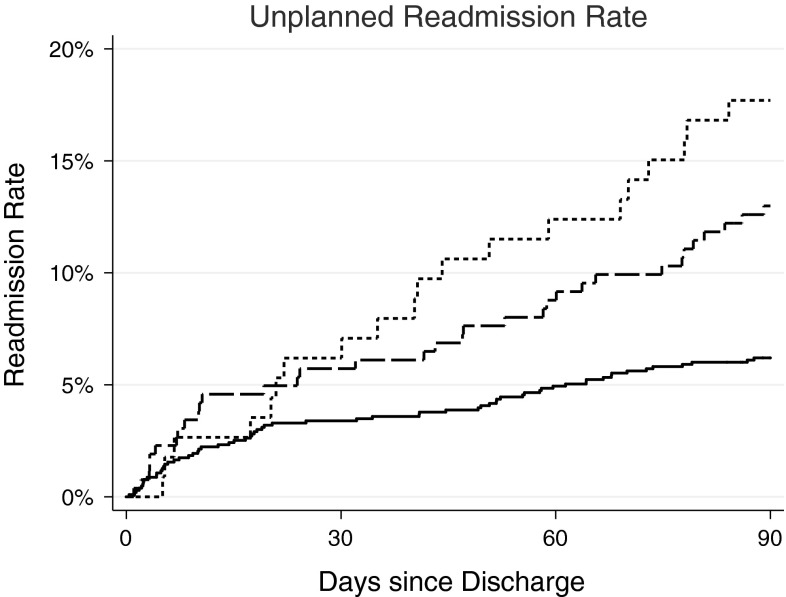
The 30-day readmission rate showed significant (p = 0.047) differences across groups for primary TKA (3.4%), revision TKA (5.7%), and revision for infected TKA (6.2%). A similar result was also seen at 90 days (primary TKA 6%, revision TKA 13%, revision for infected TKA 18%; p < 0.001) (Fig. 1). There were no differences in age, sex, or insurance type between patients who were readmitted and those who were not, but readmitted patients were more likely to have had a hospital stay over 5 days (p < 0.001), have been discharged to a skilled nursing facility (p = 0.001), and have more medical comorbidities (p = 0.002). All Payer Refined Severity of Illness (APR-SOI), graded from 1 (low) to 4 (high), was significantly associated with hospital readmission. Compared with Grade 1, Grade 2 (hazard ratio [HR], 1.82; p = 0.041), Grade 3 (2.17; p = 0.019), and Grade 4 (HR = 3.39; p = 0.030) showed increased risk of readmission. After adjusting for procedure type, APR-SOI still showed elevated risk of readmission of 33% for each additional grade (p = 0.041).
Fig. 1.
Ninety-day unplanned readmission rates were significantly higher at 90 days for revision TKA (dashed line) and staged antibiotic-spacer revision TKA (dotted line) when compared with primary TKA (solid line).
Causes of Readmission
The cause of readmission was surgical in 75% (n = 88 of 118) of patients, whereas 25% (n = 30 of 118) of readmissions were the result of medical causes (Table 3). The majority of surgical causes were the result of arthrofibrosis (28% [n = 25 of 88]), surgical site infection (SSI) (18% [n = 16 of 88]), and cellulitis (16% [n = 14 of 88]). SSI occurred more often in revision TKA (2.3%, p = 0.067) and revision for infected TKA (2.7%, p = 0.031) than in primary TKA (0.9%) (p = 0.020), whereas rates of cellulitis (0.9% primary TKA, 1.9% revision TKA, 0.9% revision for infected TKA) and arthrofibrosis (1.7% primary TKA, 2.7% revision TKA, 0.9% revision for infected TKA) were similar across groups (p > 0.05). Medical causes of readmission were varied, as seen in detail in Table 3.
Table 3.
Causes of readmission
| Cause of readmission | 0–90 days | 0–30 days | 31–60 days | 61–90 days |
|---|---|---|---|---|
| Medical | 27 (22.9%) | 23 (39.7%) | 1 (3.2%) | 3 (10.3%) |
| Clostridium difficile infection | 3 (11.1%) | 3 (13.0%) | – | – |
| Renal failure | 2 (7.4%) | 2 (8.7%) | – | – |
| Arthritis flare | 1 (3.7%) | 1 (4.3%) | – | – |
| Bacteremia | 1 (3.7%) | 1 (4.3%) | – | – |
| Constipation | 1 (3.7%) | 1 (4.3%) | – | – |
| Encephalopathy | 1 (3.7%) | 1 (4.3%) | – | – |
| Gastroenteritis | 1 (3.7%) | 1 (4.3%) | – | – |
| Hyponatremia | 1 (3.7%) | 1 (4.3%) | – | – |
| Back pain after fall | 1 (3.7%) | 1 (4.3%) | – | – |
| Melena | 1 (3.7%) | 1 (4.3%) | – | – |
| Myocardial infarction and pulmonary embolus | 1 (3.7%) | 1 (4.3%) | – | – |
| Percutaneous inserted central catheter line sepsis | 1 (3.7%) | 1 (4.3%) | – | – |
| Pulmonary edema | 1 (3.7%) | 1 (4.3%) | – | – |
| Small bowel obstruction | 1 (3.7%) | 1 (4.3%) | – | – |
| Myocardial infarction | 1 (3.7%) | 1 (4.3%) | – | – |
| Supraglottitis and mediastinitis | 1 (3.7%) | 1 (4.3%) | – | – |
| Symptomatic anemia | 1 (3.7%) | 1 (4.3%) | – | – |
| Syncope | 1 (3.7%) | 1 (4.3%) | – | – |
| Urosepsis | 1 (3.7%) | 1 (4.3%) | – | – |
| Vancomycin allergy | 1 (3.7%) | 1 (4.3%) | – | – |
| Pulmonary hypertension | 1 (3.7%) | – | 1 (100.0%) | – |
| Cellulitis (away from surgical site) | 1 (3.7%) | – | – | 1 (33.3%) |
| Pacemaker adjustment | 1 (3.7%) | – | – | 1 (33.3%) |
| Pressure ulcers, thigh pyomyositis | 1 (3.7%) | – | – | 1 (33.3%) |
| Surgical | 91 (77.1%) | 35 (60.3%) | 30 (96.8%) | 26 (89.7%) |
| Arthrofibrosis | 25 (27.5%) | 1 (2.9%) | 11 (36.7%) | 13 (50.0%) |
| Surgical site infection | 17 (18.7%) | 8 (22.9%) | 6 (20.0%) | 3 (11.5%) |
| Cellulitis | 14 (15.4%) | 10 (28.6%) | 4 (13.3%) | – |
| Hematoma | 7 (7.7%) | 3 (8.6%) | – | 4 (15.4%) |
| Dehiscence | 7 (7.7%) | 2 (5.7%) | 3 (10.0%) | 2 (7.7%) |
| Noninfected wound discharge | 3 (3.3%) | 3 (8.6%) | – | – |
| Periprosthetic fracture | 3 (3.3%) | 2 (5.7%) | – | 1 (3.8%) |
| Dislodged polyethylene insert | 3 (3.3%) | – | 2 (6.7%) | 1 (3.8%) |
| Pulmonary embolus | 2 (2.2%) | 1 (2.9%) | 1 (3.3%) | – |
| Patellar tendon rupture | 2 (2.2%) | 1 (2.9%) | – | 1 (3.8%) |
| Compartment syndrome | 1 (1.1%) | 1 (2.9%) | – | – |
| Knee effusion | 1 (1.1%) | 1 (2.9%) | – | – |
| Knee pain | 1 (1.1%) | 1 (2.9%) | – | – |
| Knee swelling | 1 (1.1%) | 1 (2.9%) | – | – |
| Dislodged antibiotic cement spacer | 1 (1.1%) | – | 1 (3.3%) | – |
| Dislocation | 1 (1.1%) | – | 1 (3.3%) | – |
| Instability | 1 (1.1%) | – | 1 (3.3%) | – |
| Patellar fracture and tendon rupture | 1 (1.1%) | – | – | 1 (3.8%) |
Early (0–30 days) readmissions were the result of medical causes in 40% of cases and surgical causes in 60% of cases. The most common surgical-related reasons for readmission were SSI and cellulitis. Late readmissions (61–90 days) were predominantly surgical-related with the majority of readmissions being for treatment of arthrofibrosis.
Risk of Readmission
Multivariate analysis showed that, compared with primary TKA, there was an increased risk of unplanned readmission for both revision TKA (HR, 2.00; p < 0.001) and revision for infected TKA (HR, 1.79; p = 0.037) (Table 4). A hospital length of stay over 5 days requiring discharge to a skilled nursing facility (versus home or an acute rehabilitation facility) and a fluid or electrolyte disorder (eg, hyponatremia, hypovolemia, acid-base disturbance, etc) also were associated with an increased likelihood of readmission.
Table 4.
Independent risk factors for readmission
| Risk factor | Hazard ratio | SE (95% CI) | p value |
|---|---|---|---|
| Revision TKA (versus primary TKA) | 2.00 | 0.4 (1.3–3.0) | 0.001 |
| Antibiotic cement spacer (versus primary TKA) | 1.79 | 0.5 (1.0–3.1) | 0.037 |
| Hospital stay over 5 days | 1.94 | 0.4 (1.3–2.9) | 0.002 |
| Discharge to skilled nursing facility | 1.62 | 0.3 (1.1–2.4) | 0.021 |
| Fluid electrolyte disorder | 1.80 | 0.4 (1.2–2.7) | 0.004 |
CI = confidence interval.
Discussion
Hospital readmissions are unfortunately not uncommon in the elderly population. With the increasing cost of health care, there will be increased scrutiny surrounding the complications causing potentially unnecessary hospital readmissions after high-volume, elective procedures such as TKA. To contain the total cost associated with TKA, it is important to evaluate the rates, timing, and causes of hospital readmissions so that we can implement cost-effective measures to address common complications. The results of this study show that patients undergoing revision TKAs or staged treatment for infected TKAs have higher unplanned readmission rates than patients undergoing primary TKAs. Additionally, approximately three-fourths of unplanned hospital readmissions are for surgical (as opposed to medical) complications. Finally, in addition to the type of procedure (primary versus revision or treatment for infection), we observed that an index hospital stay more than 5 days, discharge to a skilled nursing facility, and a fluid or electrolyte disorder each were associated with increased risk of unplanned hospital readmission.
There are limitations to consider for this study. As a retrospective study, we could not control for differing criteria for discharge destination or criteria for hospital readmission. Although there were no specific changes in surgical pathways during this study period, decisions regarding discharge and hospital readmission were clinical decisions made by the surgeon on a per-patient basis (or the admitting hospitalist physician in the case of medical readmissions). Additionally, we only evaluated complications that resulted in hospital readmission within 90 days, and thus it is important to recognize that overall complication rates are likely higher. We could only evaluate hospital visits at our institution and thus may have underestimated the rate of readmissions if patients were readmitted to an outside facility. This may be especially significant for tertiary care hospitals because patients often travel further distances to receive care, and thus our results represent a best case scenario assuming that all patients returned to our institution for treatment of all complications. Finally, as a referral center that treats patients with complex surgical problems and numerous medical comorbidities, these overall readmission rates may have limited applicability to other practice settings.
Although we could find no reports in the literature that specifically addressed a 90-day readmission rate for TKA, our 30-day unplanned readmission rate of 4% is similar to other reports in the literature. Brown et al. found an all-cause 30-day readmission rate of 4.2% in patients undergoing primary TKA [2]. Huddleston et al. [6] evaluated adverse events in Medicare beneficiaries after TKA and found a 30-day all-cause readmission rate of 5.5%. Additionally, they found that an adverse event during the index hospitalization was not associated with a higher risk of readmission. However, Mahomed et al. [16] reported a readmission rate of only 0.9% in a similar Medicare cohort. Huddleston et al. suggested that their higher readmission rate might be the result of earlier discharge after TKA, although this explanation remains controversial [4, 9, 22]. The low readmission rate reported by Mahomed et al. may also be the result of how they defined readmission, which was limited to a specific list of diagnoses rather than a true all-cause readmission rate.
Of the few studies that have reported on hospital readmission rates in patients undergoing TKA, we could only find one report that described the complications leading to readmission. In their large study on readmissions in Medicare patients, Jencks et al. [8] reported a 30-day readmission rate of 9.9% for combined major hip or knee surgery, although the procedures that made up this group were not defined. The most frequent cause was “aftercare” (10.3% of readmissions and not included in our definition of readmission for this study) followed by “major hip or knee problems” (6.0%) and pneumonia (4.2%). Infection was the cause of 3.1% of readmissions at 30 days, whereas the other measured causes were medically related (gastrointestinal, cardiac, etc). If this grouped infection rate of 3.1% includes superficial and deep infections, including cellulitis of the surrounding surgical site, then it may be comparable to our findings for SSI (1.2%, n = 17 of 1408) and cellulitis (1.0%, n = 14 of 1408). Kim et al. reported that arthrofibrosis after primary TKA occurred in 1.3% of patients [12], which is similar to the rate in our overall cohort of 1.8%. They found that all patients with arthrofibrosis underwent manipulation under anesthesia within 3 months of the original procedure but that half of patients required a revision procedure for continued stiffness. Thus, in addition to hospital readmissions, patients with arthrofibrosis are at risk for a continued high cost of treatment. Our results suggest that strategies to target specific complications could have a substantial effect on readmission rates in patients undergoing TKA. These complications (arthrofibrosis, SSI, and cellulitis) accounted for nearly half of all unplanned readmissions. Efforts to reduce these three complications may result in both significant cost savings and improved patient outcomes.
Medical comorbidities are an important predictor of complications and hospital readmissions [11, 20]. We found that increased APR severity of illness significantly elevated the risk of readmission by 82% for Grade 2, 117% for Grade 3, and 239% for Grade 4, and remained significant even when controlling for primary or revision procedure. Multivariate analysis showed that revision procedures were independently associated with risk for readmission. A long hospitalization or discharge to a skilled nursing facility was also associated with a high risk; however, we did not evaluate this cohort for complications during the primary hospitalization, and thus both of these factors are likely a proxy representing the initial state of health and possible complications. Although public health insurance has been associated with higher rates of hospital readmissions [14, 23], we did not see this trend in our data. Thus, there are many risk factors to consider when evaluating a patient for TKA. Failure to adjust for both procedure complexity and patient severity of illness will likely penalize large tertiary care referral centers that often care for patients with medical comorbidities undergoing more complicated procedures [10].
In summary, readmissions after primary, revision, and staged revision TKAs were found to be 6%, 13%, and 18% within 90 days of discharge, respectively. Risk of readmission is higher among patients undergoing revision TKA (with or without infection) when compared with patients undergoing primary TKA. This information will assist with shared decision-making between physicians and patients by better informing all parties of the possible outcomes [1]. As public reporting of provider performance becomes more common, it will be important for quality measures to distinguish among different types of knee arthroplasties to provide fair and accurate information for patients. Additionally, arthrofibrosis and infection-related complications were responsible for almost half of unplanned readmissions, making them appealing targets for cost-effective interventions to reduce readmissions.
Acknowledgments
We thank Vanessa Chan MPH, for her help in preparing this manuscript.
Footnotes
One of the authors (TPV) certifies that he has received or may receive payments or benefits, during the study period, an amount in excess of USD 10,000 from DePuy Orthopaedics, Inc (Warsaw, IN, USA). The institution of one or more of the authors (KJB) has received, during the study period, funding from the Orthopaedic Research and Education Foundation (Rosemont, IL, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that institution where the work was performed approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Bozic KJ, Chiu V. Emerging ideas: shared decision making in patients with osteoarthritis of the hip and knee. Clin Orthop Relat Res. 2011;469:2081–2085. doi: 10.1007/s11999-010-1740-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brown NM, Sheth NP, Davis K, Berend ME, Lombardi AV, Berend KR, Della Valle CJ. Total knee arthroplasty has higher postoperative morbidity than unicompartmental knee arthroplasty: a multicenter analysis. J Arthroplasty. 2012;27(Suppl):86–90. doi: 10.1016/j.arth.2012.03.022. [DOI] [PubMed] [Google Scholar]
- 3.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991–2010. JAMA. 2012;308:1227–1236. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crowe J, Henderson J. Pre-arthroplasty rehabilitation is effective in reducing hospital stay. Can J Occup Ther. 2003;70:88–96. doi: 10.1177/000841740307000204. [DOI] [PubMed] [Google Scholar]
- 5.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Huddleston JI, Maloney WJ, Wang Y, Verzier N, Hunt DR, Herndon JH. Adverse events after total knee arthroplasty: a national Medicare study. J Arthroplasty. 2009;24:95–100. doi: 10.1016/j.arth.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 7.Iezzoni LI, Ash AS, Shwartz M, Landon BE, Mackiernan YD. Predicting in-hospital deaths from coronary artery bypass graft surgery. Do different severity measures give different predictions? Med Care. 1998;36:28–39. doi: 10.1097/00005650-199801000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 9.Jones S, Alnaib M, Kokkinakis M, Wilkinson M, St Clair Gibson A, Kader D. Pre-operative patient education reduces length of stay after knee joint arthroplasty. Ann R Coll Surg Engl. 2011;93:71–75. doi: 10.1308/003588410X12771863936765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Joynt KE, Jha AK. Characteristics of hospitals receiving penalties under the Hospital Readmissions Reduction Program. JAMA. 2013;309:342–343. doi: 10.1001/jama.2012.94856. [DOI] [PubMed] [Google Scholar]
- 11.Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. JAMA. 2011;305:675–681. doi: 10.1001/jama.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim J, Nelson CL, Lotke PA. Stiffness after total knee arthroplasty. Prevalence of the complication and outcomes of revision. J Bone Joint Surg Am. 2004;86:1479–1484. [PubMed] [Google Scholar]
- 13.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467:2606–2612. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lavernia CJ, Villa JM, Iacobelli DA. Readmission rates in the state of Florida: a reflection of quality? Clin Orthop Relat Res. 2013 Feb 20 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 15.Losina E, Walensky RP, Kessler CL, Emrani PS, Reichmann WM, Wright EA, Holt HL, Solomon DH, Yelin E, Paltiel AD, Katz JN. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169:1113–1121. doi: 10.1001/archinternmed.2009.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahomed NN, Barrett JA, Katz JN, Phillips CB, Losina E, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Joint Surg Am. 2003;85:27–32. doi: 10.2106/00004623-200301000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Marshall DA, Wasylak T, Khong H, Parker RD, Faris PD, Frank C. Measuring the value of total hip and knee arthroplasty: considering costs over the continuum of care. Clin Orthop Relat Res. 2012;470:1065–1072. doi: 10.1007/s11999-011-2026-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Medicare Payment Advisory Commission (MedPAC). Medicare Payment Policy. Washington, DC, USA: Medicare Payment Advisory Commission (MedPAC); 2012.
- 19.Pulido L, Parvizi J, Macgibeny M, Sharkey PF, Purtill JJ, Rothman RH, Hozack WJ. In hospital complications after total joint arthroplasty. J Arthroplasty. 2008;23:139–145. doi: 10.1016/j.arth.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 20.Rathore SS, Foody JM, Wang Y, Smith GL, Herrin J, Masoudi FA, Wolfe P, Havranek EP, Ordin DL, Krumholz HM. Race, quality of care, and outcomes of elderly patients hospitalized with heart failure. JAMA. 2003;289:2517–2524. doi: 10.1001/jama.289.19.2517. [DOI] [PubMed] [Google Scholar]
- 21.Stranges E, Russo CA, Friedman B. Procedures With the Most Rapidly Increasing Hospital Costs, 2004–2007. Rockville, MD, USA: Agency for Healthcare Research and Quality; 2009. [PubMed] [Google Scholar]
- 22.Weingarten S, Riedinger MS, Sandhu M, Bowers C, Ellrodt AG, Nunn C, Hobson P, Greengold N. Can practice guidelines safely reduce hospital length of stay? Results from a multicenter interventional study. Am J Med. 1998;105:33–40. doi: 10.1016/S0002-9343(98)00129-6. [DOI] [PubMed] [Google Scholar]
- 23.Wier LM, Barrett M, Steiner C, Jiang HJ. All-cause Readmissions by Payer and Age, 2008: Statistical Brief #115.Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD, USA: Healthcare Cost and Utilization Project (HCUP); 2006. [PubMed]